Abstract
The aim of this study was to review the literature and evaluate the failure rates and factors that affect the stability and success of temporary anchorage devices (TADs) used as orthodontic anchorage. Data was collected from electronic databases: MEDLINE database and Google Scholar. Four combinations of term were used as keywords: “micro-implant”, “mini-implant”, “mini-screw”, and “orthodontics”. The following selection criteria were used to select appropriate articles: articles on implants and screws used as orthodontic anchorage, published in English, with both prospective and retrospective clinical and experimental investigations. The search provided 209 abstracts about TADs used as anchorage. After reading and applying the selection criteria, 66 articles were included in the study. The data obtained were divided into two topics: which factors affected TAD success rate and to what degree and in how many articles they were quoted. Clinical factors were divided into three main groups: patient-related, implant related, and management-related factors. Although all articles included in this meta-analysis reported success rates of greater than 80 percent, the factors determining success rates were inconsistent between the studies analyzed and this made conclusions difficult.
Keywords:
micro-implants; orthodontics; success rate; insertion; loading; biocompatibility; compliance 1. Introduction
Anchorage is one of the most important elements for successful orthodontic treatment. Traditionally, orthodontics employed teeth and extraoral or intraoral appliances for anchorage, often relying on the patient compliance for its effectiveness. Micro-implants (OMIs), also known in orthodontics as temporary anchorage devices (TAD) or mini-implants or mini-screws have been used to realize difficult orthodontic movements. Orthodontic mini-implants can be a powerful aid in resolving challenging malocclusions that require increased anchorage potential. Their use is versatile, minimally invasive, and proves a good ratio between costs and benefits of orthodontic treatments. They can help orthopedic dentofacial treatments by supporting distraction procedures, maxillary protractions, cleft segment expansion, stabilization, and tooth movements into narrow alveolar sites. Anchorage control is essential for an orthodontic treatment’s success. The anchorage on micro-implants prevents undesirable movements of tooth elements that were used in classic orthodontic procedures, offers an alternative to orthognathic surgery. As temporary anchorage devices, the use of micro-implants solves difficult problems such as guiding osteo-distractions, fixing maxillary cants after the vertical distraction of a ramus, stabilizing an edentulous premaxilla, moving teeth into atrophic alveolar sites [1]. The skeletal anchorage on micro-implants is a solution to treat adult orthodontic patients with a lack of quantity or quality of dental elements when conventional dental or mobile anchorage is not possible or cases with poor patients’ compliance where the wear of mobile devices or elastics is compromised [2]. Their use is the ideal solution in cases where dental anchorage may result in undesirable side effects such as vertical dimension changes produced by the use of conventional inter-maxillary forces [1]. Micro-implants as skeletal anchorage lead to a more effective orthopedic growth modification, and their use helps camouflage orthodontic treatment for those patients who were not eligible for orthognathic surgery [3,4].
Surgical atraumatic techniques, regeneration and osseointegration, an environment favorable for the primary healing, and biocompatible materials are necessary for micro-implants success. Other important issues in using micro-implants as anchorage elements are patients’ cooperation and the perception of the pain and trauma produced by surgical insertion and retraction procedures [4].
Many orthodontists avoid using micro-implants as anchorage elements because they are unfamiliar with the surgical procedures required for their insertion or because of fear of failure. Another cause could be a lack of interest in approaching new techniques compared to treatments that are already routine. These limitations should disappear, and orthodontists should also acquire the surgical skills necessary to use micro-implants, The present paper is intended to be a small guide in the practical activity of orthodontists and not only, which can help them in terms of the use of micro-implants by showing the existing types, how to apply them, the clinical situations in which they can be used, and the difficulties that may occur during treatments that use this type of anchorage.
The aim of this study was to review the literature and evaluate the failure rates and factors that affect the stability and success of temporary anchorage devices used as orthodontic anchorage.
2. Materials and Methods
2.1. Eligibility Criteria
Inclusion criteria:
- Scientific articles published from January 2006 to June 2021 (the last 15 years);
- Scientific articles published in the English language;
- Case series, original research, review;
- Mention of the following words in each possible combination: mini-implant; mini-screw; micro-implant; orthodontics.
Exclusion criteria:
- Papers with no clear report of clinical cases;
- Articles published before January 2006;
- Case reports;
- Book chapters, thesis;
- Mini-plates articles.
2.2. Literature Search Strategy
A systematic search of the literature was performed using PubMed and Google Scholar databases. Search strategies are highlighted in Table 1.

Table 1.
Literature search strategy.
Titles and abstracts of retrieved studies were screened and all the studies that included one or more of the exclusion criteria were excluded from the study. The articles selected for full text reading were examined by two authors and those that were lacking relevant informations for the purpose of this review were excluded. Any controversy was resolved with the aid of a third reviewer, selected among the authors.
2.3. Risk of Bias
In order to evaluate the methodological quality of included studies, reviewers used the JBI Critical Appraisal Checklist for Case Reports Studies (Table 2) [5].

Table 2.
JBI Critical Appraisal Checklist for Case Reports Studies.
An initial search of PubMed and Google Scholar databases identified a total of 209 documents. Of these 114 records were found on PubMed database and 95 on Google Scholar database. The full-texts of 209 articles were then screened and 8 articles were excluded cause the main topic was not relevant for the purpose of this review and 1 record was excluded because the full-text was not in English language. After applying the inclusion criteria when reading titles and abstracts due to type of publication (book or thesis), main topic, language and incapability to retrieve the abstract and/or the full-text we found 50 manuscripts that were not relevant to the purpose of the manuscript.
Furthermore, a manual search of the reference lists of all selected studies was performed and three studies were additionally included after full-text reading. Ultimately, 66 studies were included in the systematic review and processed for data extraction (Figure 1).
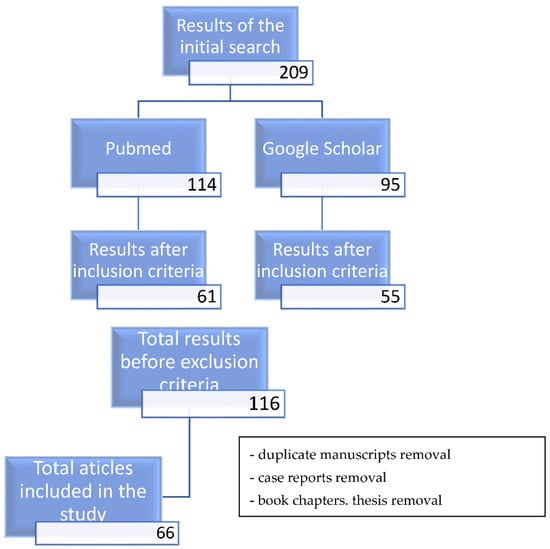
Figure 1.
Results of the study selection.
3. Results
3.1. The Success Rate of Micro-Implants
The overall success rate of skeletal anchorage using micro-implants was ranged from 79% to 98.2% [4], described by other studies as being 85.0% [6]. A systematic review published in 2010 [7] included fourteen clinical trials and described the mean overall success rate of 83.8 ± 7.4%, with no significant differences regarding the patient’s sex. Little diameters of the mini-screws from 1 to 1.1 mm had lower success rates than the greater ones from 1.5 to 2.3 mm; screws less than 8 mm in length and 1.2 mm in diameter should be avoided [7]. One study reported significantly lower success rates for 6-mm vs. 8-mm long mini-screws (72% vs. 90%) [7]. The recommended diameter and length for a micro-implant placed in the alveolar bone were 1.2 to 1.6 mm respectively 6–7 mm in another study [8]. Other authors [9] concluded that the success rate did not depend on sex, age, and side of placement but significantly increased as total bone density and cancellous bone density increased. The OMIs’ success rate was not significantly correlated with the cortical bone density.
3.2. Design
The researchers tried to improve the design of the orthodontic micro-implants to increase torsional strength, stability and reduce bone damage during insertion. An objective function stability quotient (SQ) was built and solved by Korean researchers [10] started from the thread height and pitch of AbsoAnchor SH1312-7 micro-implant (Dentos Inc., Daegu, Korea) as parameters. 3D finite element simulation, torque test, and clinical test led to the creation of four models with optimized thread design and better performance, which indicated that their optimization methodology could be used when designing OMI threads.
The peak insertion torque value is another parameter that influences the OMI’s stability. This depends on the manufacturer [11]; the study showed no correlation between the diameter of six different types of self-drilling micro-implants and torque values. Insertion speed did not affect significantly the peak torque values, but the 6 mm OMIs proved to have significantly higher torque values than the 8 and 10 mm ones. Using a screwdriver for limiting the torque or pre-drilling the cortical bone to reduce insertion torque could be a good choice.
3.3. Anatomical and Surgical Details
Over time, several methods have been devised and developed to avoid accidents using micro-implants, the most important being damage to the roots of the neighboring teeth. A precise surgical plan before OMIs’ insertion is crucial. Some researchers described the use of radiographic templates and film holders to make a surgical template for guiding OMIs’ insertion [12]. The success rate of OMIs was tested by using panoramic radiographs that showed the position and angulation of the screws [6]. The overall success rate was higher for people more than 20 years old and screws on the left side, for the women than for the men, for extraction than for non-extraction group, for OMIs placed on the interradicular midline. OMI success rate significantly increased with an increase in the OMI length and placement height, and with a lesser angulation [6].
Other authors claimed that compared with panoramic radiographs, cone beam computed tomography (CBCT) images can provide more accurate information regarding tooth position, root resorption, and various pathologies; the radiation exposure is less and the cost is lower using panoramic radiographs, which provides acceptable reliability [9].
The efficacy of optical coherence tomography (OCT) was tested comparatively with that of micro-computed tomography (μCT) [13] to detect and analyze cortical bone micro-damage immediately after insertion. The visualization of individual microcracks was highly correlated. Even if the depth penetration of OCT was more limited, it has been able to give high-resolution images of the bone microdamage occurring around the micro-implant. Image quality at the surface of the cortical bone is better when compared with μCT imaging, because of the high contrast and the high-resolution quality of OCT systems [13].
The surgical insertion procedure showed contradictory results between flap or without flap techniques on mandibular mini-implants. Loading and healing periods were not significant in the mini-screws success rates [7].
When using micro-implants is important to evaluate the cortical bone thickness and the interradicular spaces to create enough stability for the application of orthodontic forces. Park and Cho [8] found using cone-beam 3D images that in the posterior dentition area the buccal cortical bone is 1 mm or thicker, 1.12 to 1.33 mm for maxilla, and 1.25 to 2.98 mm for mandibula. The cortical bone becomes thicker progressively from the cement-enamel junction to the apical zone. The interradicular distances varied from 1.6 to 3.46 mm in the maxilla with a maximum between the second premolar and the first molar. In mandibula, the interradicular distances were greater than in maxilla and ranged between 1.99 and 4.25 mm. The retromolar zones showed cortical bone from 1.96 to 2.06 mm thicker. The widths of alveolar processes were 3.74–5.78 mm for the maxilla and 3.11–7.84 mm for the mandibula. The mid-palatal area at 20–25 mm posterior than foramen incisivum ranged from 7.04 to 6.99 mm. They concluded that a better location for placing micro-implants was buccal between the second premolar and the first molar for maxilla, buccal from the first premolar to the second molar for mandibula, palatal between molars for maxilla, the mid-palatal and retromolar areas [8].
The cortical bone thickness of the inter-dental area of maxilla and mandible for orthodontic micro-implants placement was investigated by cone-beam computerized tomography [14] by a study that was performed on 32 non-orthodontic adults with normal occlusion. Buccal cortical bone was thicker in the mandible. In the maxilla, the cortical bone was thicker buccal than palatal. In the mandible, the buccal cortical bone vas thickest distal to the first molar, and in the maxilla, it was thickest mesial to the first molar; in the palatal side of maxilla, the cortical bone was thickest mesial to the second premolar. The thinnest cortical bone was found in the buccal side of the maxilla at 4 mm from the alveolar crest and the thickest was at 10 mm, except for the site mesial to the first premolar. The buccal cortical bone thickness mesial or distal to the first inferior molar and palatal cortical bone tended to increase with increasing distance from the alveolar bone [14].
These buccal ideal locations for placing micro-implants were also used in another study that comparatively investigates the anchorage loss in canine retraction with conventional molar anchorage versus titanium micro-implants [15]. In adult patients with a mean age of 19.6 years, the first premolars were extracted to create space for canine retraction. Titanium micro-implants of 1.3 mm in diameter and 9 mm in length were placed between the second premolars and the first molars. The orthodontic mechanics were performed by using closed-coil springs which performed the canine retraction by having on one quadrant a molar anchorage and on the other an anchorage on micro-implants. The results showed no anchorage loss on the micro-implant side and 1.60–1.70 anchorage loss on the molar anchorage side. Other similar studies have aimed to investigate the effectiveness of using mini-implants in canine retraction [16]. The authors used mini-implants of 1.3 mm in diameter and 8 mm in length and their placement was also between the second premolars and the first molars, for each patient in the same quadrants (on the right side), placed at an angle of 30–40° in the maxilla and of 10–20° in the mandible to the long axis of the teeth to increase the contact between the implant and the bone. On the left quadrants, the retraction of the canines was done by using the first molars as anchorage. Orthodontic forces of 100 g were immediately applied; coil springs were used for canine retraction. Results showed that the rates of canine retraction were higher on the implant sides, 0.95 and 0.81 mm/month in maxilla respectively in the mandible and lower on the molar sides, 0.82 and 0.76 mm/month in the maxilla respectively in mandible. The loss of anchorage was less on the implant sides, 0.1 in the maxilla and 0.06 in the mandible and greater on the molar sides, 1.3 mm on the molar side of the maxilla and mandible. There were statistically significant differences between changes in anchorage inclination on the implant side and molar side in both maxilla and mandible: 0.3° on the implant side and 2.45° on the molar side in the maxilla and 0.19° on the implant side and 2.69° on the molar side in mandible. Studies [15,16] demonstrated that micro-implant anchorage is a better alternative to molar anchorage.
Many other studies investigated the ideal insertion angle of orthodontic micro-implants for biomechanical control and cortical anchorage. A study on finite models of maxilla and mandible [17] which used D2 and D3 types of bone and micro-implants of 1.3 mm diameter and 7–8 mm length inserted in different angles on bone’s surface shows that the maximum von Mises stress in the implants and the cortical bone decreases as the insertion angle increases. The stress generated at the application of horizontal orthodontic forces was distributed mainly to the cortical bone and less to the cancellous bone. The stress was higher in type D3 bone quality than in type D2. The study demonstrated that the 90° insertion angle is ideal for orthodontic micro-implants’ stabilization [17]. The shortcoming of the investigation’s method was that the ideal angle for insertion of the screw was not determined in all three spatial planes but only in the horizontal one because the direction of application of the orthodontic force was horizontal. Other studies that investigate only micro-implants placed in the upper jaw demonstrated the opposite, namely that the insertion angle of micro-implants, the cortical bone thickness is not important for the success rate of using orthodontic micro-implants [18,19]. The authors measured horizontal and vertical placement angles using cone-beam computed tomography images. The micro-implants’ success rates significantly increased with the distance to the root surface. Cortical bone thickness was affected by placement angles but root proximity was not affected by insertion angles. Other interesting results were that success rates were higher for screws put on the left side, for adult patients than for teenagers, in women than in men. The success rate increased by increasing the horizontal placement angle but the difference was not statistically significant [18].
Contact between orthodontic mini-implants and dental roots during the insertion process is a common problem because inter-radicular spaces are narrow [20]. Such contacts have been associated with root damage and increased implant failure rates. An accurate test to diagnose implant–root contact is therefore indicated. Using specific insertion torque values (the index test) as a diagnostic test of OMIs with root contact could be more accurate less adverse compared with radiographic images. Torque levels of OMIs inserted with root contact were higher than those without. The highest torque differences were identified in the self-drilling compared with the pre-drilling. It is important to record constantly the torque values during the insertion process.
The stress in the cortical bone during and after insertion of self-tapping orthodontic micro-implants using predrilled holes was simulated with a 3-dimensional finite element method [21]. Results showed stresses during insertion that could fracture the cortical bone; hoop stresses of the ultimate tensile strength and radial stresses of the ultimate compressive strength of cortical bone were developed. After insertion, residual radial stresses that could cause bone resorptions were observed. The high insertion-related stresses showed that the bone’s response and the micro-implant prognosis depend on the insertion conditions not on the orthodontic force or the timing of its application.
The primary stability of OMIs is influenced by various insertion angles and the direction of the applied orthodontic force. An opinion is that the highest primary stability values were get at an insertion angle of 45° when the mini-implants were loaded by shear force and at 90° when pullout forces were used [22].
Different OMIs proved a wide range of torque at fracture that depended on the manufacturer and the correlation between the diameter of the screw and fracture resistance was poor. The torque is to be considered at the insertion phase to minimize the risk of screw fracture and much care should be for the areas with high-density bone without predrilling [23].
By sequential fluorochrome staining combined with laser confocal microscopy were visualized the damage of cortical bone at insertion and removal of orthodontic micro-implants (OMI) [24]. The presence of a pilot hole demonstrated a minimal effect on microdamage bone characteristics and a minimal effect on maximum insertion torque. The micro-damages increased with the bone thickness; there was a positive correlation between the bone thickness and the increase in maximum insertion torque. The maximum insertion torque was correlated with the total and diffused bone damaged area. The study concluded that the choice of making pilot holes for orthodontic micro-implants’ insertion should depend on the thickness of cortical bone. The bone damages evaluated with two different types of OMI, non-drilling, and self-drilling and pilot holes showed that fractional damaged area, fractional microcracked area, and fractional diffuse damaged area were greater with the self-drilling ones and as the thickness of cortical bone increased [25].
The self-drilling micro-implants create better anchorage than self-tapping ones [26]. Self-drilling micro-implants had higher peak insertion torque and peak removal torque than self-tapping ones. Self-drilling screws demonstrate a higher fracture tendency and better contact between the implant and bone [24,25]; their use is indicated in the maxilla and thin cortical mandibular areas. Negative correlations between Periotest values were mostly demonstrated by the self-drilling micro-implants [27]. The differences between insertion torque values and corresponding assessments of stability scores were higher self-drilling screws.
3.4. Immediate Loading
In the literature, there has been much discussion about the possibility of immediate loading of mini-implants and how it affects the stability of the screw and bone structure.
Immediate loading doesn’t affect the osseointegration of OMIs but the anchorage is not always absolutely stationary, extrusion and tipping were observed in areas with thin cortical bone [28]. Immediately loading with orthodontic forces of 200 g does not influence significantly the stability [7] and seemed to accelerate the shaping of periosteal bone after the surgical intervention; there were no statistically significant differences in bone and implant contact values between the loaded OMIs and the unloaded ones [28].
Another study [29] found by histological analysis good osseointegration, bone apposition, and new bone formation in loaded and unloaded OMIs. The contact between bone and micro-implant was higher in the loaded ones. The study concluded that small diameters (1.2–1.3) OMIs made from Titanium alloy are strong enough for immediate loading even in thin cortical bone areas; in this situation drilling a pilot hole reduces the possibility of micro-implants’ breakage.
Comparing immediate loading with one-week post-insertion loading of orthodontic micro-implants showed a statistically higher torque loss in delayed insertion; a significant stability loss was seen in both situations in the first week of investigation [30].
Investigating the biomechanical properties of bone around OMIs under immediate loading using nanoindentation testing [31] showed that the trabecular area on the compression site near the implant was significantly harder than in other bone locations.
Another study based on histological, histological-morphometric, and cone beam computed tomography (CBCT) analysis were performed on autoclave-sterilized OMIs and proved that an immediate, light orthodontic load did not influence the bone healing around mini-screws [32]. The osseointegration and the cortical bone thickness increased with the time passed from the insertion of the implants. The absence of infections during the healing showed that OMIs can be autoclaved in the dental practice before insertion time, with no effect on subsequent osseointegration. The predrilling of thick cortical bone reduced the microfractures. The displacement of the periosteum stimulated the healing of the cortical bone [32].
A review article showed the efficiency of using mini-implants as anchorage and concluded that their success depends on proper initial stability and the quality and quantity of loading [16]. Other factors that could compromise the success of using OMIs are the patient’s oral hygiene, coexisting pathologies, smoking, the condition of the mucosa, the timing, quantity, and direction of the loading force direction [2,7]. Thus, the micro-implants’ success involves factors related to the patient, the orthodontist, and the OMI’s design [2,7].
3.5. Microbial Aggregation around Micro-Implants, Biocompatibility
The possibility of microbial aggregation and biofilm formation on micro-implants has been intensively investigated; surface roughness and chemical composition play an important role in this issue. An in-vitro study [33] which uses X-ray photoelectron spectroscopy detected high-carbon contamination and other inorganic elements like Pb, Zn, P, Cu, Cr, Ca on the oxide surfaces of five different types of micro-implants. Those chemical impurities disappeared after Ar(+) ion sputtering. The surface roughness was greater for titanium micro-implants (182 nm) than for the stainless-steel ones. Through scanning electron microscopy, structural defects were observed [34]. These retention sites favored the biofilm’s formation when the micro-implants were immersed in human saliva; the microbial flora of the biofilm was reduced when the micro-implants were pretreated with chlorhexidine and fluoride mouth rinses.
Various other methods have been tried to decrease microbial aggregation around micro-implants to prevent their loss. By using silver nanoparticles (AgNPs) were manufactured AgNP-modified titanium micro-implants (Ti-nAg) by coating OMIs with AgNPs or with a AgNP-coated biopolymer (Ti-BP-AgNP) [35]. Comparative data showed that OMIs coated with BP-AgNP had remarkable antibacterial properties by creating inhibition zones for Aggregatibacter actinomycetemcomitans, Streptococcus mutans, and Streptococcus sanguinis, whereas no antibacterial effects were seen on those coated with AgNPs. Scanning electron microscopy showed a silver atomic percent of 1.05 in the group of OMIs coated with regular AgNPs and much greater, 21.2%, in the group coated with BP-AgNP. Ti-BP-AgNP proved to be an excellent implantable biomaterial, with very good antibacterial properties [34].
The heat treatment (APH treatment) increases the hydrophilicity and the roughness of Ti6Al4V micro-implants subjected to anodization and cyclic calcification. APH treatment created a surface of the nanotubular TiO2 layer which was covered with a compact apatite-like film. APH-treated micro-implants showed better bioactivity and biocompatibility, better bone regenerative characteristics, higher removable torque, and greater contact with bone, compared with untreated (UT) and anodized and heat-treated (AH) ones [36].
Self-drilling orthodontic micro-implants were surface-treated with acid (etched), resorbable blasting media (RBM), partially resorbable blasting media (hybrid) to increase, study and compare the bone-cutting capacity and osseointegration [37]. The hybrid type gave the most stable self-drilling OMIs, without reduction of bone-cutting capacity.
Chitosan modification of the surface of micro-implants might be an approach to enhance the bioactive- and antibacterial properties of orthodontic micro-implants. Chitosan-modified titanium alloy micro-implants showed better biocompatibility with pre-osteoblastic cells which was confirmed by their improved adhesion, proliferation, and cell viability analysis [38]. Biofilm formation of Streptococcus mutans and Streptococcus sobrinus was reduced by 53% and 31%, respectively, on the surface of OMIs.
Nanotechnology is the study, production, and controlled manipulation of materials with a grain size less than 100 nm. As grain size decreases, the interaction between OMIs and the surrounding cellular environment increases. Treating the micro-implants surface with nanophase materials improved their osteo-integration due to a more closely match with the architecture of native trabecular bone [39].
Zirconia micro-implants proved excellent biocompatibility; they were tested and showed initial stability and clinical applicability for orthodontic treatments comparable to that of titanium micro-implants under various compressive and tensile forces [40]. Compressive and tensile forces were recorded at 0.01, 0.02, and 0.03 mm displacement of the implants of zirconia and titanium at various angles of 0°, 10°, 20°, 30°, and 40°; there were no statistically significant differences between the two types of implants made of different materials regarding the maximum insertion torque, maximum removal torque or the amount of movement at displacement test.
3.6. Use in Orthodontic Clinical Practice and Dento-Facial Orthopedics
Micro-implants could help orthopedic and skeletal modifications. Micro-implant-assisted rapid palatal expanders variable as design and using protocols were used for the treatments of Class III [3]. By fixing with micro-implants transversal screws to the hard palate the rapid palatal expansion prevents the tipping of the anchorage teeth, tooth mobility, and resorption of roots and bone which are accidents in using conventional rapid palatal expenders (RPE) [41,42,43].
Computer tomography and Mimics modeling software, ANSYS simulation software showed that compression and tension forces are directed to the palate bone and produced less rotation or tipping of the maxillary complex in case of using micro-implant-assisted rapid palatal expansion (MARPE) compared to use of conventional rapid palatal expander (RPE) [44]. MARPE made the maxilla bend laterally and prevented unwanted rotation of the maxillary complex, the vertical maxillary dropping [44].
The MARPE was described as efficient in adolescents and an adult-case patient (19 years old) where the palatal anchorage was performed by using four micro-implants. The palatal bones were expanded by 5.41 ± 2.18 mm and 10 mm, respectively [45]. The cross-sectional CT showed the expansion of maxillofacial structures, zygoma, and nasal floor, and the widening of circum-maxillary sutures; the alveolar bone maintained its integrity even the teeth tipped in vestibular direction. The dentoalveolar side effects were minimum: the first molars exhibited buccal tipping of 2.56 ± 2.64° [46].
Another study [47] contradicted these results by finding 41% skeletal enlargement, 12% alveolar bone bending, and 48% dental tipping after MARPE. The mid-palatal suture opening was parallel in both axial and coronal planes. The dental tipping was 4.17° to 4.96° and the buccal bone thickness was reduced by an average of 39% measured at the molars and the premolars [46]. MARPE appears to be an alternative to surgical treatment in the correction of moderate transverse deficiencies in skeletally mature adult patients [43,44,45,46,47].
Micro-implant-supported midfacial skeletal expanders that had been used as anchorage four OMIs (1.8 mm in diameter, 11 mm or 13 mm in length) inserted through the palatal bone, bi-cortically, produced almost pure skeletal rotational movement of the mid cranial structures [48]. Alveolar bone bending and dental tipping were not statistically significant. The localization of the rotational fulcrum of the zygomaticomaxillary complex should be the first step to differentiate the expansion pattern, than angular measurements should be performed. The angular measurements for fulcrums gave very different results than the conventional linear measurement system that can falsely exaggerate the alveolar and dental components of midfacial skeletal expansion [48].
Micro-implant-assisted expanders have proved significant effects on the mid-face, with a degree of asymmetry [49]. On non-growing patients, CBCT images showed a statistically significant difference between the average magnitude of the total expansion of 4.98 mm at the anterior nasal spine and the average of 4.77 mm at the posterior nasal spine. Among the asymmetric patients, one-half of the anterior nasal spine moved more than the contralateral one by 2.22 mm. The expansion achieved was 96% parallel in the antero-posterior direction.
The palatal bone and soft tissue thicknesses were investigated by cone-beam computerized tomography, using a micro-implant-supported maxillary skeletal expander in Class III malocclusion on 58 patients [50]. The antero-posterior reference that has been used was the line connecting the central fossae of the first molars (Level 0). The anterior palatal bone was significantly thicker in males than females in the anterior palate, whilst in the posterior palate there was no significant sex-related difference. The thickness tended to decrease in the posterior direction, except in women at 2 mm lateral from the reference line. In all investigated areas the palatal soft tissue was significantly thicker in males than females. The bone thickness decreased and the soft tissue thickness increased as the lateral distance from the reference line increased. Another similar study [51] showed that the palatal bone was thinner in cases with class III malocclusion than in those with class I malocclusion, with significant differences in some areas. Palatal bone was thicker in the middle region of the midline area. The palatal bone was significantly thinner in area 9.0 mm before the transverse palatine suture in the midline area, 9.0 mm before and after the transverse palatine suture in the middle area, and 9.0 mm after the transverse palatine suture in the lateral area. The study concluded that anterior and middle palatal areas are safer for putting micro-implants, while the thinness of the posterior palatal bone increases the risk of failure and perforations.
Micro-implants can be used as orthodontic anchorage in infra-zygomatic areas. A research study was performed to investigate the insertion torque and pull-out strength of three brands of infra-zygomatic mini-implants. Their mechanical strength proved to depend on their design [52].
Cleft lip and palate is the most common craniofacial malformation clinical characterized by underdeveloped maxilla in transverse and sagittal dimension; it can be corrected by surgical repair of the cleft followed by orthodontic treatment [53]. Bone-anchored rapid palatal expanders had the advantage of directly anchoring the expansion appliance to the palatal bone with less dental secondary effects. The greatest stress caused by the bone expander which used OMIs as anchor system was observed in the mid-palatal suture area at the implant insertion site on the cleft side along the palatal slopes and was equally distributed superiorly to the alveolar and basal bone [53]. In conventional expanders the greatest stress was observed at tooth level both on the cleft side and on the opposite side. The zygomaticomaxillary suture experienced maximum stress, followed by the zygomaticotemporal and nasomaxillary sutures. Displacement in the transverse plane was highest on the cleft side, and in the antero-posterior plane was highest in the posterior region [53].
The OMIs can be used as direct or indirect anchorage elements for molar up-righting in all three spatial planes [54]. The direct method is simpler because it requires one OMI and a single bracket or button, reducing the patient’s discomfort and chair time compared to the indirect anchorage. It eliminates the unwanted movement of the anchorage unit. Direct anchorage has limitations in cases of rotated or lingually tipped molars because they need more than a single force to upright their position. OMIs are a reliable solution in the treatment of tipped or impacted molars.
Micro-implant assisted molar intrusion in maxillary helped the prosthetic rehabilitation in mandible [55]. The maxillary molars extruded in time after opposite molar extractions in mandible could be easily intruded by using OMIs placed palatal or both buccal and palatal and placing on them intrusive forces. These procedures created a minimum of 5–8 mm for rehabilitation on implants of the posterior sector of the mandible, in adult patients [55].
The distalization with micro-implant-aided sliding mechanics proved less distal tipping of the posterior teeth and the method seemed efficient for patients with mild arch length discrepancies even without making therapeutic extractions, except the third molars [56]. In the maxilla, the posterior teeth were distalized with 1.4 to 2.0 mm, a media of 3.5° of distal tipping, and 1 mm intrusion; in the mandible, the posterior teeth were distalized with 1.6 to 2.5 mm and 6.6° to 8.3° of distal tipping. The maxillary posterior teeth showed intrusion by 1 mm. There were increases in arch widths at the premolars and molars. The micro-implants’ success rate was 89.7% and the mean treatment time was 20 ± 4.9 months. Inter-premolar and intermolar distances have increased. In the adult group, the Frankfort horizontal to mandibular plane angle has decreased. Profile changes were determined by distal repositioning of the upper and lower lips [57].
In cases with maxillary dentoalveolar protrusion, the anchorage on micro-implants was more efficient in retracting the anterior group than the traditional anchorage [57]. The use of micro-implants produced less anchorage loss, and had a better effect for the high-angle patients than had traditional anchorage. Both systems proved their efficiency in reducing dental and alveolar protrusion.
In skeletal Class III, orthognathic surgery the maxillary intervention could be avoided by using OMIs placed in the palatal bone between the upper first and second molars to intrude the posterior teeth. The maxillary occlusal plane rotated clockwise and increased the surgical mandibular setback; the vertical dimension was reduced. The distal movement of the chin was greater than the alternative surgical prediction with no change in the occlusal plane. The intrusion of the maxillary posterior teeth with OMIs prevented the need for upper jaw surgery in adult skeletal Class III patients [58].
The micro-implants as anchorage can be successfully used for the treatment of Class II malocclusions [59]. OMIs were included in a novel en masse distalization concept used for patients with canine sagittal distalizations of half of a cusp or more. One palatal micro-implant on each maxillary side was introduced in the interradicular region. The objective of the study was to get a complete en-masse distalization of the whole upper arch in one step. By maxillary tooth movements and dentoalveolar compensations, the canine neutral relationship and the overjet correction were achieved [59].
OMIs can be used in lingual straight wire appliances for retraction of the frontal maxillary group [60]. The study used 3D finite element models and analysis software ANSYSnsys Workbench 15 (ANSYS, USA). The OMIs were positioned at 8 mm from the alveolar crest. On the OMIs positioned between the two central incisors was applied a vertical traction force for the simulation of the intrusion anterior from the bonded threads. The retraction hooks were positioned between the lateral incisor and the canine at a height of 6 mm. A retraction force of 1.5 N from the retraction hooks to OMIs was applied; the additional intrusive force of 50 g from the two incisors was combined to simulate the effect on labial crown torque. The double wire was more efficient in torque control compared with the single round or rectangular wire or in lingual orthodontics [60]. En-masse bodily movement of anterior teeth seemed to be difficult although the vertical intrusion force increases by using OMIs increased.
En-masse distalization in the maxilla requires antibiotics or a placebo before the micro-implant’s placement. However, a study on 38 participants [61] proved that antibiotics provided no benefit in terms of OMIs stability, inflammation of soft tissues, and postinterventional pain. Measurements of inflammatory markers in serum were inefficient in demonstrating soft tissue inflammations. Antibiotic prophylaxis slightly decreased the levels of the biomarkers.
Regardless of the severity of obstructive sleep apnea (OSA), the use of oral appliances is preferred when nasal continuous positive airway pressure (CPAP) is not efficient [62]. Micro-implant assisted rapid maxillary expansion is effective in treating children with OSA and maxillary constriction. The maxillary expansion enlarges the nasal cavity and increases the air quantity that passes through the nasal pathway. In adult patients, the side effects are unwanted teeth movements. Micro-implant assisted rapid maxillary expansion (MARME) could reduce even eliminate the dental side effects. MARME produces skeletal effects that enable a larger mid-palatal suture separation and a larger increase of the nasal cavity volume. The maxillary skeletal expander (MSE) is a special MARME appliance of four mini-screws inserted in the posterior palate with bi-cortical engagements in the palatal and nasal cortical bone. MSE expands the superior and posterior areas of the nasal cavity [62].
The pterygopalatine suture can be split without surgery, by using midfacial skeletal expanders [63]. The device used had a jackscrew unit with four parallel holes for the micro-implant insertion, with two soft supporting arms on each side which are soldered to the molar bands for increasing stability. The jackscrew was seated on the hard palate between the zygomatic buttress bones. After the treatment, the mean palatal suture opening angle was 0.57°. There was no significant difference between males and females regarding the palatal suture opening pattern and 84% of cases had openings between the medial and lateral pterygoid plates on both right and left sides.
Micro-implants are indicated as anchorage elements in cases of periodontal patients who need orthodontic treatment [64]. For the advantages like a simple surgical procedure, low cost, immediate loading, the placement’s possibilities the OMIs are indicated for molar intrusion, molar up-righting, and other minor tooth movements [54].
Rupture of the intermaxillary suture with a micro-implant-supported screw was experimentally achieved with an expansion force of 86 N. A high tensile stress concentration was exerted and opened the fused intermaxillary suture [65].
Experimentally on dogs, the bi-cortical micro-implants with two anchorage units demonstrated their efficiency for the difficult movement that is the posterior teeth protraction, in the mandible [66].
3.7. Patients’ and Practitioners’ Compliance
Another important issue besides investigating the efficiency of the use of micro-implants was the determination of patients’ compliance with their use and the perception of pain while performing the insertion procedures. An article from 2008 [67] showed by using a visual analog scale (VAS) that the patients who underwent micro-implant surgery were expected to experience significantly greater pain than they endured. The postinterventional pain decreased continuously from the first to day seven after the surgical procedure. Pain experienced in the initial tooth alignment phase was significantly greater than in extraction procedures, micro-implants’ insertion, or tooth or the insertion of separators. Patients’ expectations of pain were greater in the case of micro-implants’ insertion than in insertion of separators and tooth alignment but not statistically different than in extractions. Patients’ pain significantly decreased seven days after the insertion of the micro-implants. Most patients reported little or no pain during micro-implant’s insertion and overestimated first overestimated before the intervention the pain and trauma that would have been endured. The only problems caused by micro-implants were the accumulation of food waste around the screws (86%) and minor speech disturbances (37%). A large percentage of patients were satisfied with the implant surgery (76%) and said they would recommend it to others (78%).
Another similar article that investigated pain perception on maxillary OMIs insertion found that VAS score 1 day after placement was significantly less than that 1 day after first premolar extraction for orthodontic purpose or that one day after the fixed appliance was bonded. The results indicated that interdental micro-implants did not produce greater pain than other orthodontic interventions [68].
A questionnaire-based study from 2010 [69] evaluated the pain experienced by orthodontic patients during tooth extractions, maxillary OMIs insertions, and gingival tissue removal before placing the maxillary implants. The pain felt during extractions was significantly greater than during tissue removal or micro-implant placement. The micro-implant placement caused no pain in 30% of patients and was the least painful procedure; the transgingival placement was significantly preferred.
Orthodontic mini implants (OMIs) provide anchorage without depending on the collaboration of patients, they are effective and can be used for various treatment objectives; still, surveys have shown that many orthodontists never or rarely use them [70]. The barriers to implement OMIs in clinical practice are: the need to perform surgical procedures for their placement and risk factors associated, implant failure, costs, numerous implementation issues. Conducting surgical interventions in orthodontic offices is still very uncommon and can be conditioned by variables such as the lack of knowledge and skills of clinicians; the lack of knowledge-management skills of pertinent stakeholders, lack of organization, lack of time and resources, attitudes towards new knowledge, and resistance from the patient. Limitations depend more on the medical staff than on patients [70].
Retrieved OMIs exhibited different degrees of chemical changes on surface characteristics and mechanical behavior. The thread edges and tips were worn out and thin deposits were seen on their surfaces. Traces of foreign elements like iron, sulfur, and calcium, were detected on their surfaces. The maximum insertion torque and the insertion time of retrieved OMIs were increased compared to the initial use. The maximum insertion torque was increased in all OMIs put with the insertion angle of 45° compared with 90°. The reuse for immediate relocation in the same patient may be acceptable; postponed relocation and allogeneic reuse of OMIs are not recommended in clinical practice [71].
For future practice, we can try the mini-implant anchorage in the mechanics of reducing the displacements of the temporomandibular discs [72], in the reposition of the mandible [73], in solving complicated problems such as cranial asymmetries with dentofacial and occlusal effects [74], in orofaciodigital syndrome treatments [75], and as a non-surgical alternative in progressive ankylosis of the temporomandibular joint when patients do not accept the surgical treatment [76].
A great advantage of using micro-implants is the possibility of maintaining better oral hygiene than with the use of conventional anchoring systems, due to the smaller size and lower ability to retain food debris [77]. In the last decade, oral hygiene has been greatly improved by using web media as a means of investigation and education for patients and their parents in cases of pediatric patients [78,79]. The possible side effects of mini-implants as oral mucosa trauma, inflammation, and eventually chronic lesions can be easily treated by photodynamic therapy that is minimally invasive and showed promising results [80].
4. Conclusions
Considering the results of our study we can conclude that the micro-implants’ success involves factors related to the patient, the orthodontist, the design and material of these devices and due to the multiple advantages that micro-implants have, they would have been indicated to be commonly used in orthodontic practices.
Author Contributions
Conceptualization, S.-M.B., C.D.O.; methodology, L.L.V., S.-M.B.; supervision, V.C.; writing—original draft, S.-M.B.; writing—review and editing, L.L.V., C.D.O., V.C. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare that they have no conflict of interest regarding this manuscript and did not receive any financial support from any organizations or a research grant.
References
- Vachiramon, A.; Urata, M.; Kyung, H.M.; Yamashita, D.-D.; Yen, S.L.-K. Clinical Applications of Orthodontic Microimplant Anchorage in Craniofacial Patients. Cleft Palate-Craniofacial J. 2009, 46, 136–146. [Google Scholar] [CrossRef] [PubMed]
- Leo, M.; Cerroni, L.; Pasquantonio, G. Temporary anchorage devices (TADs) in orthodontics: Review of the factors that influence the clinical success rate of the mini-implants. Clin. Ter. 2016, 167, e70–e77. [Google Scholar] [CrossRef] [PubMed]
- Ngan, P.; Moon, W. Evolution of Class III treatment in orthodontics. Am. J. Orthod. Dentofac. Orthop. 2015, 148, 22–36. [Google Scholar] [CrossRef] [PubMed]
- Kyung, H.; Ly, N.; Hong, M. Orthodontic skeletal anchorage: Up-to-date review. Orthod. Waves 2017, 76, 123–132. [Google Scholar] [CrossRef]
- The Joanna Briggs Institute Critical Appraisal Tools for Use in JBI Systematic Reviews Checklist for Case Reports. Available online: http://joannabriggs.org/research/critical-appraisal-tools.html (accessed on 6 October 2021).
- Park, J.H.; Chae, J.-M.; Bay, R.C.; Kim, M.-J.; Lee, K.-Y.; Chang, N.-Y. Evaluation of factors influencing the success rate of orthodontic microimplants using panoramic radiographs. Korean J. Orthod. 2018, 48, 30–38. [Google Scholar] [CrossRef]
- Crismani, A.G.; Bertl, M.; Čelar, A.G.; Bantleon, H.-P.; Burstone, C.J. Miniscrews in orthodontic treatment: Review and analysis of published clinical trials. Am. J. Orthod. Dentofac. Orthop. 2010, 137, 108–113. [Google Scholar] [CrossRef]
- Park, J.; Cho, H.J. Three-dimensional evaluation of interradicular spaces and cortical bone thickness for the placement and initial stability of microimplants in adults. Am. J. Orthod. Dentofac. Orthop. 2009, 136, 314.e1–314.e12, discussion 314–315. [Google Scholar] [CrossRef]
- Lee, M.-Y.; Park, J.H.; Kim, S.-C.; Kang, K.-H.; Cho, J.-H.; Chang, N.-Y.; Chae, J.-M. Bone density effects on the success rate of orthodontic microimplants evaluated with cone-beam computed tomography. Am. J. Orthod. Dentofac. Orthop. 2016, 149, 217–224. [Google Scholar] [CrossRef]
- Kim, K.-D.; Yu, W.-J.; Park, H.-S.; Kyung, H.-M.; Kwon, O.-W. Optimization of orthodontic microimplant thread design. Korean J. Orthod. 2011, 41, 25–35. [Google Scholar] [CrossRef]
- Whang, C.Z.Y.; Bister, D.; Sherriff, M. An in vitro investigation of peak insertion torque values of six commercially available mini-implants. Eur. J. Orthod. 2011, 33, 660–666. [Google Scholar] [CrossRef]
- Wu, J.C.; Huang, J.-N.; Zhao, S.-F.; Xu, X.-J.; Xie, Z.-J. Radiographic and surgical template for placement of orthodontic microimplants in interradicular areas: A technical note. Int. J. Oral Maxillofac. Implant. 2006, 21, 629–634. [Google Scholar]
- Lakshmikantha, H.T.; Ravichandran, N.K.; Jeon, M.; Kim, J.; Park, H.-S. Assessment of cortical bone microdamage following insertion of microimplants using optical coherence tomography: A preliminary study. J. Zhejiang Univ. Sci. B 2018, 19, 818–828. [Google Scholar] [CrossRef]
- Zhao, H.; Gu, X.-M.; Liu, H.-C.; Wang, Z.-W.; Xun, C.-L. Measurement of cortical bone thickness in adults by cone-beam computerized tomography for orthodontic miniscrews placement. J. Huazhong Univ. Sci. Technolog. Med. Sci. 2013, 33, 303–308. [Google Scholar] [CrossRef]
- Thiruvenkatachari, B.; Pavithranand, A.; Rajasigamani, K.; Kyung, H.M. Comparison and measurement of the amount of anchorage loss of the molars with and without the use of implant anchorage during canine retraction. Am. J. Orthod. Dentofac. Orthop. 2006, 129, 551–554. [Google Scholar] [CrossRef]
- Davis, D.; Krishnaraj, R.; Duraisamy, S.; Ravi, K.; Dilip, S.; Charles, A.; Sushil, N. Comparison of Rate of Canine Retraction and Anchorage Potential between Mini-implant and Conventional Molar Anchorage: An In vivo Study. Contemp. Clin. Dent. 2018, 9, 337–342. [Google Scholar] [CrossRef] [PubMed]
- Jasmine, M.I.F.; Yezdani, A.A.; Tajir, F.; Venu, R.M. Analysis of stress in bone and microimplants during en-masse retraction of maxillary and mandibular anterior teeth with different insertion angulations: A 3-dimensional finite element analysis study. Am. J. Orthod. Dentofac. Orthop. 2012, 141, 71–80. [Google Scholar] [CrossRef]
- Chen, Y.; Kyung, H.M.; Zhao, W.T.; Yu, W.J. Critical factors for the success of orthodontic mini-implants: A systematic review. Am. J. Orthod. Dentofac. Orthop. 2009, 135, 284–291. [Google Scholar] [CrossRef] [PubMed]
- Park, H.-S.; Hwangbo, E.-S.; Kwon, T.-G. Proper mesiodistal angles for microimplant placement assessed with 3-dimensional computed tomography images. Am. J. Orthod. Dentofac. Orthop. 2010, 137, 200–206. [Google Scholar] [CrossRef] [PubMed]
- Reynders, R.M.; Ladu, L.; Ronchi, L.; Di Girolamo, N.; De Lange, J.; Roberts, N.; Plüddemann, A. Insertion torque recordings for the diagnosis of contact between orthodontic mini-implants and dental roots: A systematic review. Syst. Rev. 2016, 5, 50. [Google Scholar] [CrossRef] [PubMed]
- Yu, W.; Park, H.-S.; Kyung, H.-M.; Kwon, O.-W. Dynamic simulation of the self-tapping insertion process of orthodontic microimplants into cortical bone with a 3-dimensional finite element method. Am. J. Orthod. Dentofac. Orthop. 2012, 142, 834–841. [Google Scholar] [CrossRef]
- Araghbidikashani, M.; Golshah, A.; Nikkerdar, N.; Rezaei, M. In-vitro impact of insertion angle on primary stability of miniscrews. Am. J. Orthod. Dentofac. Orthop. 2016, 150, 436–443. [Google Scholar] [CrossRef] [PubMed]
- Smith, A.; Hosein, Y.K.; Dunning, C.E.; Tassi, A. Fracture resistance of commonly used self-drilling orthodontic mini-implants. Angle Orthod. 2015, 85, 26–32. [Google Scholar] [CrossRef] [PubMed]
- Jensen, S.; Jensen, E.; Sampson, W.; Dreyer, C. Torque Requirements and the Influence of Pilot Holes on Orthodontic Miniscrew Microdamage. Appl. Sci. 2021, 11, 3564. [Google Scholar] [CrossRef]
- Shank, S.B.; Beck, F.M.; D’Atri, A.M.; Huja, S.S. Bone damage associated with orthodontic placement of miniscrew implants in an animal model. Am. J. Orthod. Dentofac. Orthop. 2012, 141, 412–418. [Google Scholar] [CrossRef]
- Chen, Y.; Shin, H.-I.; Kyung, H.-M. Biomechanical and histological comparison of self-drilling and self-tapping orthodontic microimplants in dogs. Am. J. Orthod. Dentofac. Orthop. 2008, 133, 44–50. [Google Scholar] [CrossRef]
- Çehreli, S.; Özçirpici, A.A. Primary stability and histomorphometric bone-implant contact of self-drilling and self-tapping orthodontic microimplants. Am. J. Orthod. Dentofac. Orthop. 2012, 141, 187–195. [Google Scholar] [CrossRef]
- Chen, Y.; Kang, S.T.; Bae, S.-M.; Kyung, H.-M. Clinical and histologic analysis of the stability of microimplants with immediate orthodontic loading in dogs. Am. J. Orthod. Dentofac. Orthop. 2009, 136, 260–267. [Google Scholar] [CrossRef]
- Chen, Y.; Lee, J.-W.; Cho, W.-H.; Kyung, H.-M. Potential of self-drilling orthodontic microimplants under immediate loading. Am. J. Orthod. Dentofac. Orthop. 2010, 137, 496–502. [Google Scholar] [CrossRef]
- Migliorati, M.; Drago, S.; Gallo, F.; Amorfini, L.; Dalessandri, D.; Calzolari, C.; Benedicenti, S.; Silvestrini-Biavati, A. Immediate versus delayed loading: Comparison of primary stability loss after miniscrew placement in orthodontic patients—a single-centre blinded randomized clinical trial. Eur. J. Orthod. 2016, 38, 652–659. [Google Scholar] [CrossRef]
- Iijima, M.; Nakagaki, S.; Yasuda, Y.; Handa, K.; Koike, T.; Muguruma, T.; Saito, T.; Mizoguchi, I. Effect of immediate loading on the biomechanical properties of bone surrounding the miniscrew implants. Eur. J. Orthod. 2013, 35, 577–582. [Google Scholar] [CrossRef][Green Version]
- Catharino, P.C.; Dominguez, G.C.; Dos Santos, P., Jr.; Morea, C. Histologic, Histomorphometric, and Radiographic Monitoring of Bone Healing Around In-Office–Sterilized Orthodontic Mini-implants With or Without Immediate Load: Study in Rabbit Tibiae. Int. J. Oral Maxillofac. Implant. 2014, 29, 321–330. [Google Scholar] [CrossRef] [PubMed]
- Chin, M.Y.; Sandham, A.; de Vries, J.; van der Mei, H.C.; Busscher, H.J. Biofilm formation on surface characterized micro-implants for skeletal anchorage in orthodontics. Biomaterials 2007, 28, 2032–2040. [Google Scholar] [CrossRef] [PubMed]
- Vlasa, A.; Biris, C.; Lazar, L.; Bud, A.; Bud, E.; Varlam, C.M.; Maris, M.; Pacurar, M. Scanning Electron Microscope Analysis of Titanium Alloy Orthodontic Implants. Mater. Plast. 2017, 54, 345–347. [Google Scholar] [CrossRef]
- Venugopal, A.; Muthuchamy, N.; Tejani, H.; Gopalan, A.-I.; Lee, K.-P.; Lee, H.-J.; Kyung, H.M. Incorporation of silver nanoparticles on the surface of orthodontic microimplants to achieve antimicrobial properties. Korean J. Orthod. 2017, 47, 3–10. [Google Scholar] [CrossRef]
- Oh, E.-J.; Nguyen, T.-D.T.; Lee, S.-Y.; Jeon, Y.-M.; Bae, T.-S.; Kim, J.-G. Enhanced compatibility and initial stability of Ti6Al4V alloy orthodontic miniscrews subjected to anodization, cyclic precalcification, and heat treatment. Korean J. Orthod. 2014, 44, 246–253. [Google Scholar] [CrossRef]
- Kim, H.-Y.; Kim, S.-C. Bone cutting capacity and osseointegration of surface-treated orthodontic mini-implants. Korean J. Orthod. 2016, 46, 386–394. [Google Scholar] [CrossRef]
- Ly, N.T.K.; Shin, H.; Gupta, K.C.; Kang, I.K.; Yu, W. Bioactive Antibacterial Modification of Orthodontic Microimplants Using Chitosan Biopolymer. Macromol. Res. 2019, 27, 504–510. [Google Scholar] [CrossRef]
- De Stefani, A.; Bruno, G.; Preo, G.; Gracco, A. Application of Nanotechnology in Orthodontic Materials: A State-of-the-Art Review. Dent. J. 2020, 8, 126. [Google Scholar] [CrossRef]
- Choi, H.W.; Park, Y.S.; Chung, S.H.; Jung, M.H.; Moon, W.; Rhee, S.H. Comparison of mechanical and biological properties of zirconia and titanium alloy orthodontic micro-implants. Korean J. Orthod. 2017, 47, 229–237. [Google Scholar] [CrossRef]
- Harzer, W.; Schneider, M.; Gedrange, T. Rapid Maxillary Expansion with Palatal Anchorage of the Hyrax Expansion Screw?Pilot Study with Case Presentation. J. Orofac. Orthop. 2004, 65, 419–424. [Google Scholar] [CrossRef]
- Bud, E.; Bică, C.; Păcurar, M.; Vaida, P.; Vlasa, A.; Martha, K.; Bud, A. Observational Study Regarding Possible Side Effects of Miniscrew-Assisted Rapid Palatal Expander (MARPE) with or without the Use of Corticopuncture Therapy. Biology 2021, 10, 187. [Google Scholar] [CrossRef] [PubMed]
- Tausche, E.; Hansen, L.; Schneider, M.; Harzer, W. Bone-supported rapid maxillary expansion with an implant-borne Hyrax screw: The Dresden Distractor. L’Orthodontie Française 2008, 79, 127–135. [Google Scholar] [CrossRef] [PubMed]
- MacGinnis, M.; Chu, H.; Youssef, G.; Wu, K.W.; Machado, A.W.; Moon, W. The effects of micro-implant assisted rapid palatal expansion (MARPE) on the nasomaxillary complex—A finite element method (FEM) analysis. Prog. Orthod. 2014, 15, 52. [Google Scholar] [CrossRef] [PubMed]
- Carlson, C.; Sung, J.; McComb, R.W.; Machado, A.W.; Moon, W. Microimplant-assisted rapid palatal expansion appliance to orthopedically correct transverse maxillary deficiency in an adult. Am. J. Orthod. Dentofac. Orthop. 2016, 149, 716–728. [Google Scholar] [CrossRef]
- Zong, C.; Tang, B.; Hua, F.; He, H.; Ngan, P. Skeletal and dentoalveolar changes in the transverse dimension using microimplant-assisted rapid palatal expansion (MARPE) appliances. Semin. Orthod. 2019, 25, 46–59. [Google Scholar] [CrossRef]
- Ngan, P.; Nguyen, U.K.; Nguyen, T.; Tremont, T.; Martin, C. Skeletal, Dentoalveolar, and Periodontal Changes of Skeletally Matured Patients with Maxillary Deficiency Treated with Microimplant-assisted Rapid Palatal Expansion Appliances: A Pilot Study. APOS Trends Orthod. 2018, 8, 71. [Google Scholar] [CrossRef]
- Paredes, N.; Colak, O.; Sfogliano, L.; Elkenawy, I.; Fijany, L.; Fraser, A.; Zhang, B.; Moon, W. Differential assessment of skeletal, alveolar, and dental components induced by microimplant-supported midfacial skeletal expander (MSE), utilizing novel angular measurements from the fulcrum. Prog. Orthod. 2020, 21, 18. [Google Scholar] [CrossRef]
- Elkenawy, I.; Fijany, L.; Colak, O.; Paredes, N.A.; Gargoum, A.; Abedini, S.; Cantarella, D.; Dominguez-Mompell, R.; Sfogliano, L.; Moon, W. An assessment of the magnitude, parallelism, and asymmetry of micro-implant-assisted rapid maxillary expansion in non-growing patients. Prog. Orthod. 2020, 21, 42. [Google Scholar] [CrossRef]
- Yu, S.-K.; Cho, Y.; Seo, Y.-S.; Kim, J.-S.; Kim, D.K.; Kim, H.-J. Radiological evaluation of the bone and soft tissue thicknesses of the palate for using a miniscrew-supported maxillary skeletal expander. Surg. Radiol. Anat. 2021, 43, 1001–1008. [Google Scholar] [CrossRef]
- Chen, W.; Zhang, K.; Liu, D. Palatal bone thickness at the implantation area of maxillary skeletal expander in adult patients with skeletal Class III malocclusion: A cone-beam computed tomography study. BMC Oral Health 2021, 21, 144. [Google Scholar] [CrossRef]
- Wang, C.-H.; Wu, J.-H.; Lee, K.-T.; Hsu, K.-R.; Wang, H.C.; Chen, C.-M. Mechanical strength of orthodontic infrazygomatic mini-implants. Odontology 2011, 99, 98–100. [Google Scholar] [CrossRef] [PubMed]
- Mathew, A.; Nagachandran, K.S.; Vijayalakshmi, D. Stress and displacement pattern evaluation using two different palatal expanders in unilateral cleft lip and palate: A three-dimensional finite element analysis. Prog. Orthod. 2016, 17, 38. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Magkavali-Trikka, P.; Emmanouilidis, G.; Papadopoulos, M.A. Mandibular molar uprighting using orthodontic miniscrew implants: A systematic review. Prog. Orthod. 2018, 19, 1. [Google Scholar] [CrossRef] [PubMed]
- Rai, D.; Bhasin, S.S.; Rai, S. Orthodontic Microimplants Assisted Intrusion of Supra-erupted Maxillary Molar Enabling Osseointegrated Implant Supported Mandibular Prosthesis: Case Reports. J. Indian Prosthodont. Soc. 2014, 14 (Suppl. 1), 238–242. [Google Scholar] [CrossRef]
- Oh, Y.-H.; Park, H.-S.; Kwon, T.-G. Treatment effects of microimplant-aided sliding mechanics on distal retraction of posterior teeth. Am. J. Orthod. Dentofac. Orthop. 2011, 139, 470–481. [Google Scholar] [CrossRef]
- Xu, Y.; Xie, J. Comparison of the effects of mini-implant and traditional anchorage on patients with maxillary dentoalveolar protrusion. Angle Orthod. 2017, 87, 320–327. [Google Scholar] [CrossRef]
- Park, H.-S.; Kim, J.-Y.; Kwon, T.-G. Occlusal plane change after intrusion of maxillary posterior teeth by microimplants to avoid maxillary surgery with skeletal Class III orthognathic surgery. Am. J. Orthod. Dentofac. Orthop. 2010, 138, 631–640. [Google Scholar] [CrossRef] [PubMed]
- Beyling, F.; Klang, E.; Niehoff, E.; Schwestka-Polly, R.; Helms, H.-J.; Wiechmann, D. Class II correction by maxillary en masse distalization using a completely customized lingual appliance and a novel mini-screw anchorage concept—Preliminary results. Head Face Med. 2021, 17, 23. [Google Scholar] [CrossRef]
- Long, H.-Q.; Xuan, J.; Kyung, H.-M.; Bing, L.; Wu, X.-P. Biomechanical Analysis of Micro-implants Lingual Straight Wire Appliance during Retracting Maxillary Anterior Teeth. Int. J. Morphol. 2018, 36, 1386–1393. [Google Scholar] [CrossRef]
- Łyczek, J.; Kawala, B.; Antoszewska-Smith, J. Influence of antibiotic prophylaxis on the stability of orthodontic microimplants: A pilot randomized controlled trial. Am. J. Orthod. Dentofac. Orthop. 2018, 153, 621–631. [Google Scholar] [CrossRef] [PubMed]
- Chang, H.; Chen, Y.; Du, J. Obstructive sleep apnea treatment in adults. Med. Sci. 2020, 36, 7–12. [Google Scholar] [CrossRef]
- Colak, O.; Paredes, N.A.; Elkenawy, I.; Torres, M.; Bui, J.; Jahangiri, S.; Moon, W. Tomographic assessment of palatal suture opening pattern and pterygopalatine suture disarticulation in the axial plane after midfacial skeletal expansion. Prog. Orthod. 2020, 21, 21. [Google Scholar] [CrossRef] [PubMed]
- Zasčiurinskienė, E.; Lund, H.; Lindsten, R.; Jansson, H.; Bjerklin, K. Outcome of periodontal–orthodontic treatment in subjects with periodontal disease. Part II: A CBCT study of alveolar bone level changes. Eur. J. Orthod. 2019, 41, 565–574. [Google Scholar] [CrossRef] [PubMed]
- Boryor, A.; Hohmann, A.; Wunderlich, A.; Geiger, M.; Kilic, F.; Kim, K.B.; Sander, M.; Böckers, T.; Sander, C. Use of a modified expander during rapid maxillary expansion in adults: An in vitro and finite element study. Int. J. Oral Maxillofac. Implant. 2013, 28, e11–e16. [Google Scholar] [CrossRef][Green Version]
- Wu, J.-C.; Huang, J.-N.; Zhao, S.-F. Bicortical microimplant with 2 anchorage heads for mesial movement of posterior tooth in the beagle dog. Am. J. Orthod. Dentofac. Orthop. 2007, 132, 353–359. [Google Scholar] [CrossRef]
- Lee, T.C.K.; McGrath, C.P.J.; Wong, R.W.K.; Rabie, A.B.M. Patients’ Perceptions Regarding Microimplant as Anchorage in Orthodontics. Angle Orthod. 2008, 78, 228–233. [Google Scholar] [CrossRef]
- Chen, C.-M.; Chang, C.-S.; Tseng, Y.-C.; Hsu, K.-R.; Lee, K.-T.; Lee, H.-E. The perception of pain following interdental microimplant treatment for skeletal anchorage: A retrospective study. Odontology 2011, 99, 88–91. [Google Scholar] [CrossRef]
- Baxmann, M.; McDonald, F.; Bourauel, C.; Jäger, A. Expectations, acceptance, and preferences regarding microimplant treatment in orthodontic patients: A randomized controlled trial. Am. J. Orthod. Dentofac. Orthop. 2010, 138, 250.e1–250.e10, discussion 250–251. [Google Scholar] [CrossRef]
- Reynders, R.M.; Ronchi, L.; Ladu, L.; Di Girolamo, N.; De Lange, J.; Roberts, N.; Mickan, S. Barriers and facilitators to the implementation of orthodontic mini-implants in clinical practice: A protocol for a systematic review and meta-analysis. Syst. Rev. 2016, 5, 22. [Google Scholar] [CrossRef]
- Lu, L.; Park, H.-S. Surface characteristics and mechanical behavior of retrieved orthodontic microimplants. J. Zhejiang Univ. Sci. B 2018, 19, 372–382. [Google Scholar] [CrossRef] [PubMed]
- Supplement, D.; Minervini, G.; Nucci, L.; Lanza, A.; Femiano, F.; Contaldo, M.; Grassia, V. Temporomandibular disc displacement with reduction treated with anterior repositioning splint: A 2-year clinical and magnetic resonance imaging (MRI) follow-up. J. Biol. Regul. Homeost. Agents 2020, 34 (Suppl. 1), 151–160, DENTAL SUPPLEMENT. [Google Scholar]
- Minervini, G.; Lucchese, A.; Perillo, L.; Serpico, R.; Minervini, G. Unilateral superior condylar neck fracture with dislocation in a child treated with an acrylic splint in the upper arch for functional repositioning of the mandible. CRANIO® 2017, 35, 337–341. [Google Scholar] [CrossRef]
- Deshayes, M.-J. Les déformations crâniennes asymétriques et leur retentissement dento-facial et occlusal [Cranial asymmetries and their dento-facial and occlusal effects]. L’Orthodontie Française 2006, 77, 87–99. [Google Scholar] [CrossRef] [PubMed]
- Minervini, G.; Romano, A.; Petruzzi, M.; Maio, C.; Serpico, R.; Lucchese, A.; Candotto, V.; Di Stasio, D. Telescopic overdenture on natural teeth: Prosthetic rehabilitation on (OFD) syndromic patient and a review on available literature. J. Boil. Regul. Homeost. Agents 2018, 32 (Suppl. 1), 131–134. [Google Scholar]
- D’Apuzzo, F.; Minervini, G.; Grassia, V.; Rotolo, R.; Perillo, L.; Nucci, L. Mandibular Coronoid Process Hypertrophy: Diagnosis and 20-Year Follow-Up with CBCT, MRI and EMG Evaluations. Appl. Sci. 2021, 11, 4504. [Google Scholar] [CrossRef]
- Akbulut, Y. The effects of different antiseptic mouthwash on microbiota around orthodontic mini-screw. Niger. J. Clin. Pract. 2020, 23, 1507–1513. [Google Scholar] [CrossRef]
- Di Stasio, D.; Romano, A.N.; Paparella, R.S.; Gentile, C.; Minervini, G.; Serpico, R.; Candotto, V.; Laino, L. How social media meet patients questions: YouTube review for children oral thrush. J. Biol. Regul. Homeost. Agents 2018, 32 (Suppl. 1), 101–106. [Google Scholar]
- Di Stasio, D.; Romano, A.; Paparella, R.S.; Gentile, C.; Serpico, R.; Minervini, G.; Candotto, V.; Laino, L. How social media meet patients questions: YouTube review for mouth sores in children. J. Biol. Regul. Homeost. Agents 2018, 32 (Suppl. 1), 117–121. [Google Scholar] [PubMed]
- Di Stasio, D.; Romano, A.; Gentile, C.; Maio, C.; Lucchese, A.; Serpico, R.; Paparella, R.; Minervini, G.; Candotto, V.; Laino, L. Systemic and topical photodynamic therapy (PDT) on oral mucosa lesions: An overview. J. Biol. Regul. Homeost. Agents 2018, 32 (Suppl. 1), 123–126. [Google Scholar] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).