Abstract
The COVID-19 pandemic changed the management of emergency medicine and those complications that needed interventional procedures, such as endoscopy or other radiological procedures. At the beginning of the outbreak, there were no exploitable recommendations regarding the proper policy to apply for limiting the virus spread during endoscopy. Between the first and the second wave, the approach regarding interventional procedures changed, due to higher awareness and newly defined protocols, even if different among the health centers. Patients with severe COVID-19 may develop major gastrointestinal complications or require nutritional support, so interventional procedures are required at bedside, even if patients are in isolated rooms. Our tertiary center admitted 95 patients with severe COVID-19 at our ICU-dedicated department until May 2021, and 56% of them died. Among them, 61 endoscopic procedures were performed, mainly gastroscopies (81.96%) followed by colonoscopies (11.47%) and other more advanced procedures (6.55%). Our approach aimed to adapt and create COVID-related protocols, dedicated itineraries, and rooms in a separate department with the prospect to easily organize complete and safe endoscopic theaters at the COVID-ICU department.
1. Introduction
The COVID-19 pandemic has increased the fear of viral spread through both patients/healthcare workers and aerosol-generating procedures, as in endoscopy. At the beginning of the outbreak of severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2), there were no exploitable recommendations regarding the proper policy to apply for limiting the virus spread during endoscopy. That is why, initially, healthcare workers cancelled or postponed endoscopic procedures that were not clinically relevant in order to avoid potentially dangerous viral exposure of both sides, healthcare workers and patients. [1] During the first wave, this approach was reasonable, but during and after the second wave, it was not ethically allowed to postpone procedures due to the risk of missing pre-cancerous lesions or gastrointestinal (GI) cancers on time [2,3].
Patients with severe COVID-19 may develop major GI complications, such as GI bleeding or tracheoesophageal fistula (TEF), or require nutritional support (percutaneous endoscopic gastrostomy (PEG/PEG-jejunal) or feeding tube insertion).
Where and how to perform endoscopy for these patients has been a tricky issue since the beginning of the pandemic for many reasons, from adequate personal protections to appropriate instrument reprocessing. Furthermore, before the outbreak of SARS-CoV 2, a patient in isolation for any multi-resistant microorganism was accurately and safely transported to the endoscopic theater at the endoscopic service while taking proper precautions. This strategy was initially not applicable to SARS-CoV 2-positive patients, so when the pandemic globally spread, many departments changed their management strategies, and most of the hospitals adapted their facilities to the ongoing condition [4,5].
A major concern regards appropriate personal protections, which may minimize the risk of viral transmission during endoscopic procedures. A prospective study examined the extent of viral contamination present in the local environment before and after endoscopic procedures on COVID-19 patients, showing a relatively low risk of contamination compared with many other settings in hospital units during the first wave [6,7].
The endoscopic theater is an ergonomic room with easy visualization of monitors, protective radiation shielding, and chairs for sitting during long cases. These comforts help to prevent work-related fatigue and injury. When a complex procedure needs to be performed at bedside in an intensive care unit (ICU) or COVID unit, there is an increased risk of viral contamination and a decrease in healthcare comfort, which leads to more challenging endoscopic procedures. The aim of our study was to evaluate the current evidence regarding endoscopic procedures performed at the patient’s bedside and to provide our experience in endoscopy for COVID patients.
2. Research in Context
We also searched PubMed, Embase, and the Cochrane Library for studies published in English up to May 19, 2021, with the terms “endoscopy” and “bedside” and “COVID,” in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statements [8]. Our inclusion criteria were the English language, full-text paper, and including the text recommendations regarding endoscopic management of SARS-CoV-2 positive patients in endoscopy. The papers that did not fulfill these criteria were excluded. At the end of our research, 11 papers were eligible, but only 2 fulfilled our inclusion criteria (Figure 1) [9,10]. The few findings from this systematic review suggested that endoscopy at bedside did not reduce endoscopy-related mortality but seemed to be related to overall mortality in severe COVID-19 patients. However, these studies had substantial shortcomings, such as heterogeneous patient populations, mainly single-center experience, lack of well-defined protocols, and use of various endpoint definitions.
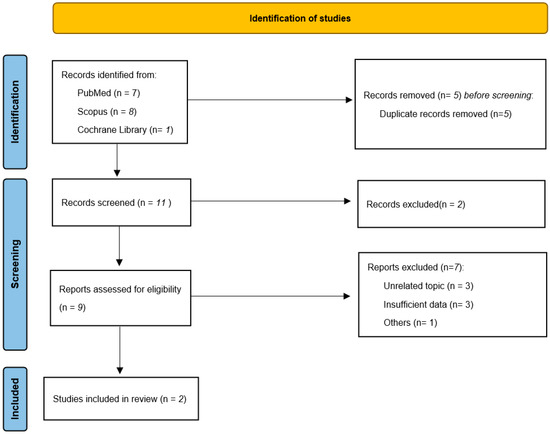
Figure 1.
Flow-chart systematic review.
3. Our Experience
Our institute is a tertiary referral center for severe COVID-19 patients thanks to our innovative instrumentation, including an extracorporeal membrane oxygenation (ECMO) system. During the outbreak of SARS-CoV 2, we admitted 95 patients with severe COVID-19 at our ICU-dedicated department (ICU-COVID area). We apply a multidisciplinary approach to these patients when they need an invasive procedure, which is usually performed in a dedicated room with radiological instrumentation and lead-shielded walls, such as operating or endoscopic theaters. When possible, it was decided to perform a less traumatic and invasive procedure at bedside in order to avoid patient transportation, so reducing, as much as possible, any unnecessary insults and risk of contamination out of the COVID-department. Specific personal protective equipment (PPE) for COVID-19, including masks and complete medical overalls, was assigned to those who took part in the endoscopic procedures at bedside. Furthermore, they had the chance to get dressed and undressed in separated and dedicated rooms in order not to spread the virus by contamination.
Among the 25 patients needing endoscopy—and for some, the procedures were performed more than once—we performed a total of 61 procedures at bedside in the ICU-COVID area. Fifty of them were gastroscopies (EGDS), performed mostly after clinical suspicion of trachea-esophageal fistula (40%) and gastrointestinal (GI) bleeding (30%). One case of EGDS showed a gastric perforation, which was treated with endoscopic sutures. Colonoscopies were performed mainly for GI bleeding (85.71%). We also performed more advanced and technically complex endoscopic procedures at bedside: three (4.81% of total procedures) endoscopic retrograde cholangiopancreatography (ERCP), all of them for complications of biliary lithiasis. One patient developed a walled-off pancreatic necrosis (WOPN), which needed an endoscopic ultrasound (EUS)-guided drainage through apposition of a luminal apposing metal stent (LAMS). Patients and procedures characteristics are summarized in Table 1. Our findings reflect similar results from the literature, even if other approaches were not well described. Nevertheless, we observed that our procedures at bedside were safe, and patients’ mortality was mainly due to SARS-CoV2 infection and its systemic complications.

Table 1.
Patient and endoscopic procedure characteristics performed at COVID-ICU department.
4. Conclusions
The COVID-19 pandemic changed the management of emergency medicine and those complications that needed interventional procedures, such as endoscopy [11] or other radiological procedures. Adaptation and creation of COVID-related protocols and novel systems were immediately prompted [12,13]. Focus on disinfection and appropriate reprocessing was intensified [14,15]. On the one hand, we supported the organization of departments in order to more easily give assistance to SARS-CoV-2-positive patients, creating dedicated itineraries and rooms in a separate department. On the other hand, we focused attention on those hospitals all over the world that do not have a structure making it possible to adapt to different itineraries (COVID and not-COVID), or simply those hospitals or institutions that cannot reorganize their employees in different sections of the hospital. Our approach to performing endoscopy for severe SARS-CoV-2 patients at bedside, even when radiological instrumentation is requested, may help guide other institutions to apply a reasonable choice. Our attitude, indeed, permitted us to transport endoscopic and radiological instrumentation to the COVID-ICU patients’ rooms according to a well-defined protocol of sanitization, reprocessing of instrumentation, and personal protection. Our approach allowed us to organize complete and safe endoscopic theaters at the COVID-ICU department on-demand, permitting the safe performance of the endoscopic and radiological procedures at the patients’ beds.
Author Contributions
A.G.: conceptualization, methodology, resources, and comments; G.M.: resources, comments, and data analysis; G.E.M.R.: manuscript writing, design, methodology, video editing, and images; D.L. comments and data analysis; C.S.: comments and data analysis; G.P. comments and data analysis; A.A.: supervision, comments, and data analysis. M.T.: supervision, comments, and data analysis. All the authors revised the manuscript and agreed on its conclusions. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study, when possible. When patients were unconscious, it was obtained from a guardian ad litem if assigned, otherwise the attending physician acted as a guarantor.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Hunt, R.H.; East, J.E.; Lanas, A.; Malfertheiner, P.; Satsangi, J.; Scarpignato, C.; Webb, G.J. COVID-19 and Gastrointestinal Disease: Implications for the Gastroenterologist. Dig. Dis. 2021, 39, 119–139. [Google Scholar] [CrossRef] [PubMed]
- Maida, M. Screening of gastrointestinal cancers during COVID-19: A new emergency. Lancet Oncol. 2020, 21, e338. [Google Scholar] [CrossRef]
- Aparicio, T.; Layese, R.; Hemery, F.; Tournigand, C.; Paillaud, E.; De Angelis, N.; Quero, L.; Ganne, N.; Prat, F.; Pachev, A.; et al. Effect of lockdown on digestive system cancer care among older patients during the first wave of COVID-19: The cadigcovage multicentre cohort study. Dig. Liver Dis. 2021. [Google Scholar] [CrossRef]
- Zhang, S.; Wu, X.; Feng, Y.; Wang, Q.; Jiang, Q.; Guo, T.; Wu, D.; Xu, T.; Li, R.; Yang, A. GI endoscopy infection control strategy after COVID-19 peak: Changing strategy for a changing epidemic. Gastrointest. Endosc. 2021, 93, 530–532.e1. [Google Scholar] [CrossRef] [PubMed]
- Petrocelli, G.; Dioscoridi, L.; Forti, E.; Pugliese, F.; Cintolo, M.; Bonato, G.; Rosa, R.; Mutignani, M. The first “exclusive COVID-19” endoscopy project. Endoscopy 2021, 53, 453–454. [Google Scholar] [CrossRef] [PubMed]
- Somerville, C.C.; Shoaib, M.; Kuschner, C.E.; Brune, Z.; Trindade, A.J.; Benias, P.C.; Becker, L.B. Prospective analysis of SARS-CoV-2 dissemination to environmental surfaces during endoscopic procedures. Endosc. Int. Open 2021, 9, E701–E705. [Google Scholar] [CrossRef] [PubMed]
- Guo, Z.-D.; Wang, Z.-Y.; Zhang, S.-F.; Li, X.; Li, L.; Li, C.; Cui, Y.; Fu, R.B.; Dong, Y.-Z.; Chi, X.-Y.; et al. Aerosol and surface distribution of severe acute respiratory syndrome coronavirus 2 in hospital wards, Wuhan, China, 2020. Emerg. Infect. Dis. J. 2020, 26, 1583. [Google Scholar]
- Page, M.J.; Moher, D.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. PRISMA 2020 explanation and elaboration: Updated guidance and exemplars for reporting systematic reviews. BMJ 2021, 372, n160. [Google Scholar] [CrossRef] [PubMed]
- Gu, Q.; Wang, H.-F.; Fang, Y.; Lu, Y.; Shen, Z.; Wang, Y.; Wu, X.; Cen, L.; Chen, Y.-S. Analysis of an improved workflow of endoscope reprocessing for bedside endoscopic diagnosis and treatment on COVID-19 patients. J. Zhejiang Univ. Sci. B 2020, 21, 416–422. [Google Scholar] [CrossRef]
- Tian, Q.; Yan, X.; Shi, R.; Wang, G.; Xu, X.; Wang, H.; Wang, Q.; Yang, L.; Liu, Z.; Wang, L.; et al. Endoscopic mask innovation and protective measures changes during the coronavirus disease-2019 pandemic: Experience from a Chinese hepato-biliary-pancreatic unit. Dig. Endosc. 2020, 32, 1105–1110. [Google Scholar] [CrossRef]
- Lisotti, A.; Bacchilega, I.; Linguerri, R.; Fusaroli, P. Endoscopic ultrasound-guided gallbladder drainage as a strategy to overcome shortage of operating rooms and intensive care unit beds during COVID-19 crisis. Endoscopy 2020, 52, E263–E264. [Google Scholar] [CrossRef] [PubMed]
- Franzini, T.A.P.; Kotinda, A.P.S.T.; Moura, D.; Badana, M.L.V.; De Medeiros, M.S.; Lima, P.G.R.; De Mello, B.F.; Kayano, R.P.; Carmona, M.J.C.; Rocha, M.C.; et al. Approach to endoscopic procedures: A routine protocol from a quaternary university referral center exclusively for coronavirus disease 2019 patients. Clinics 2020, 75, e1989. [Google Scholar] [CrossRef] [PubMed]
- Traina, M.; Amata, M.; Granata, A.; Ligresti, D.; Gaetano, B. The C-Cube: An endoscopic solution in the time of COVID-19. Endoscopy 2020, 52, E351–E352. [Google Scholar] [CrossRef] [PubMed]
- Rerknimitr, R.; Soetikno, R.; Ratanachu-Ek, T.; Tiankanon, K.; Kongkam, P.; Ridtitid, W. Additional measures for bedside endoscope cleaning to prevent contaminated splash during COVID-19 pandemic. Endoscopy 2020, 52, 706–707. [Google Scholar] [CrossRef] [PubMed]
- Lin, X.; Zhang, Z.; Gao, M.; Zhang, Z.; Lin, Z.; Huang, S.; Ren, J.; Luo, M.; Xu, X.; Chen, G.; et al. Practical experience of endoscope reprocessing and working-platform disinfection in COVID-19 patients: A report from Guangdong China during the pandemic. Gastroenterol. Res. Pract. 2020, 2020, 1–4. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).