Development of a MyData Platform Based on the Personal Health Record Data Sharing System in Korea
Abstract
:1. Introduction
2. Related Work
3. Proposed System
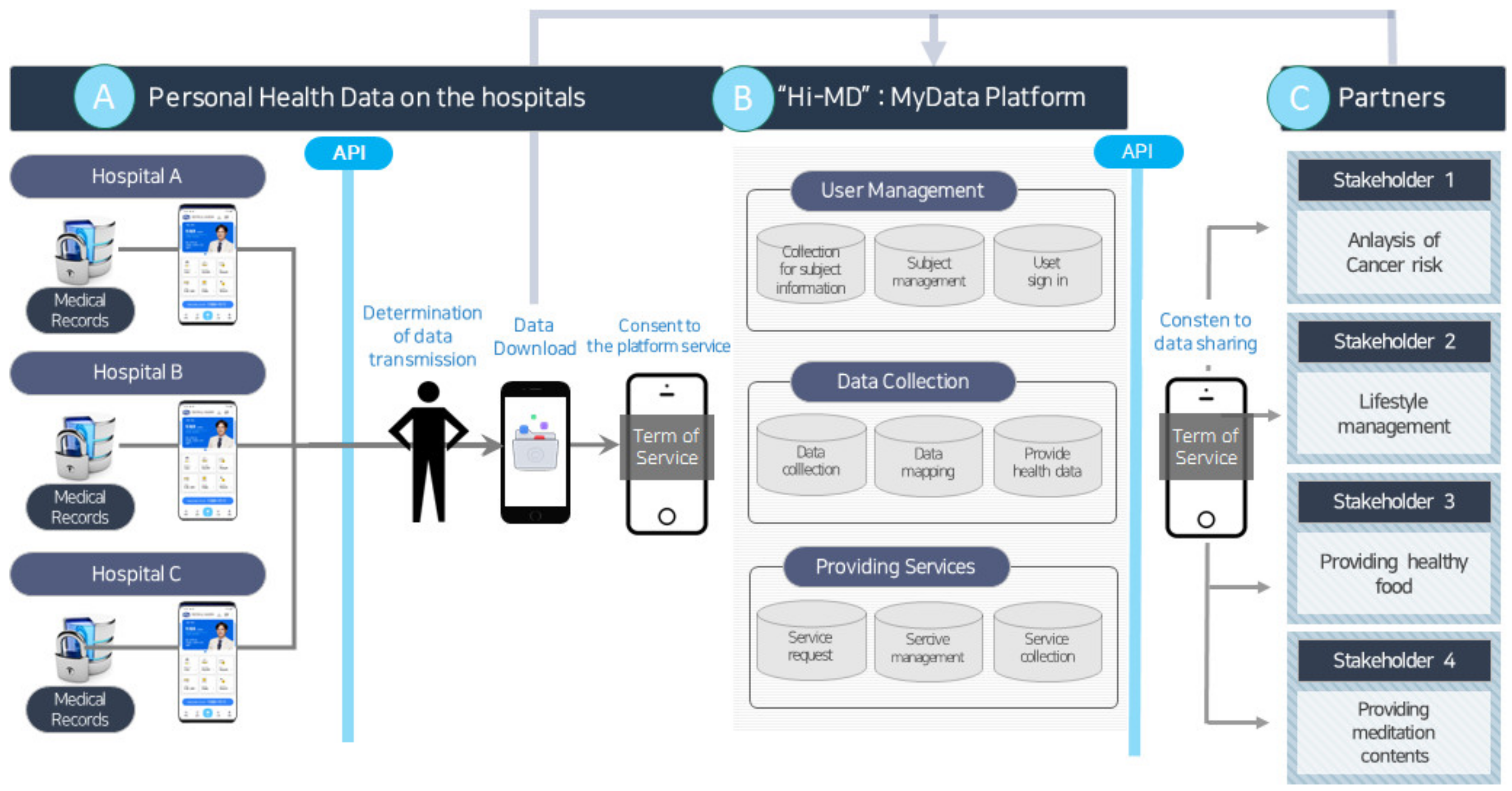
3.1. Overall System Architecture
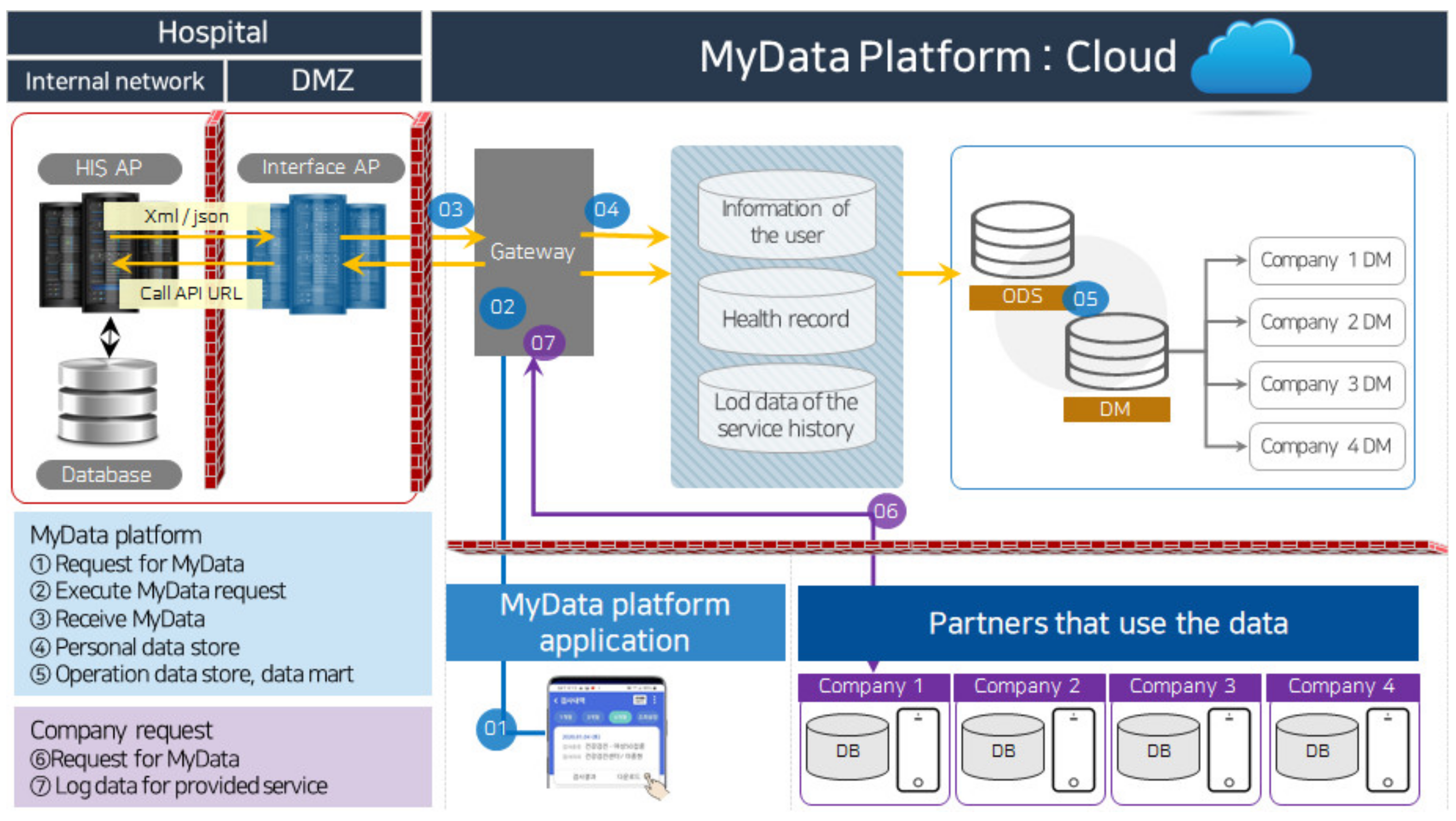
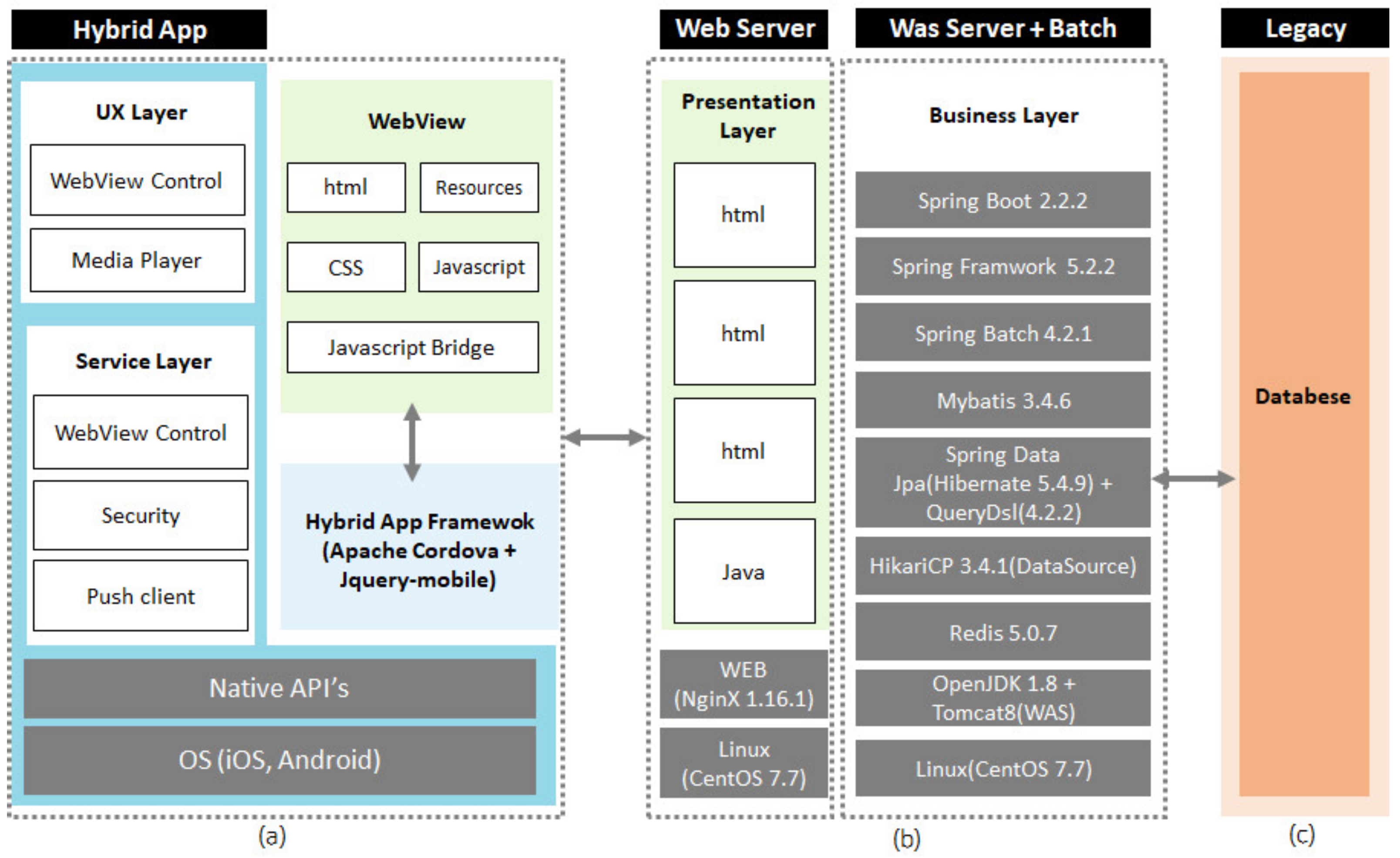
3.2. System Specifications
4. Evaluation
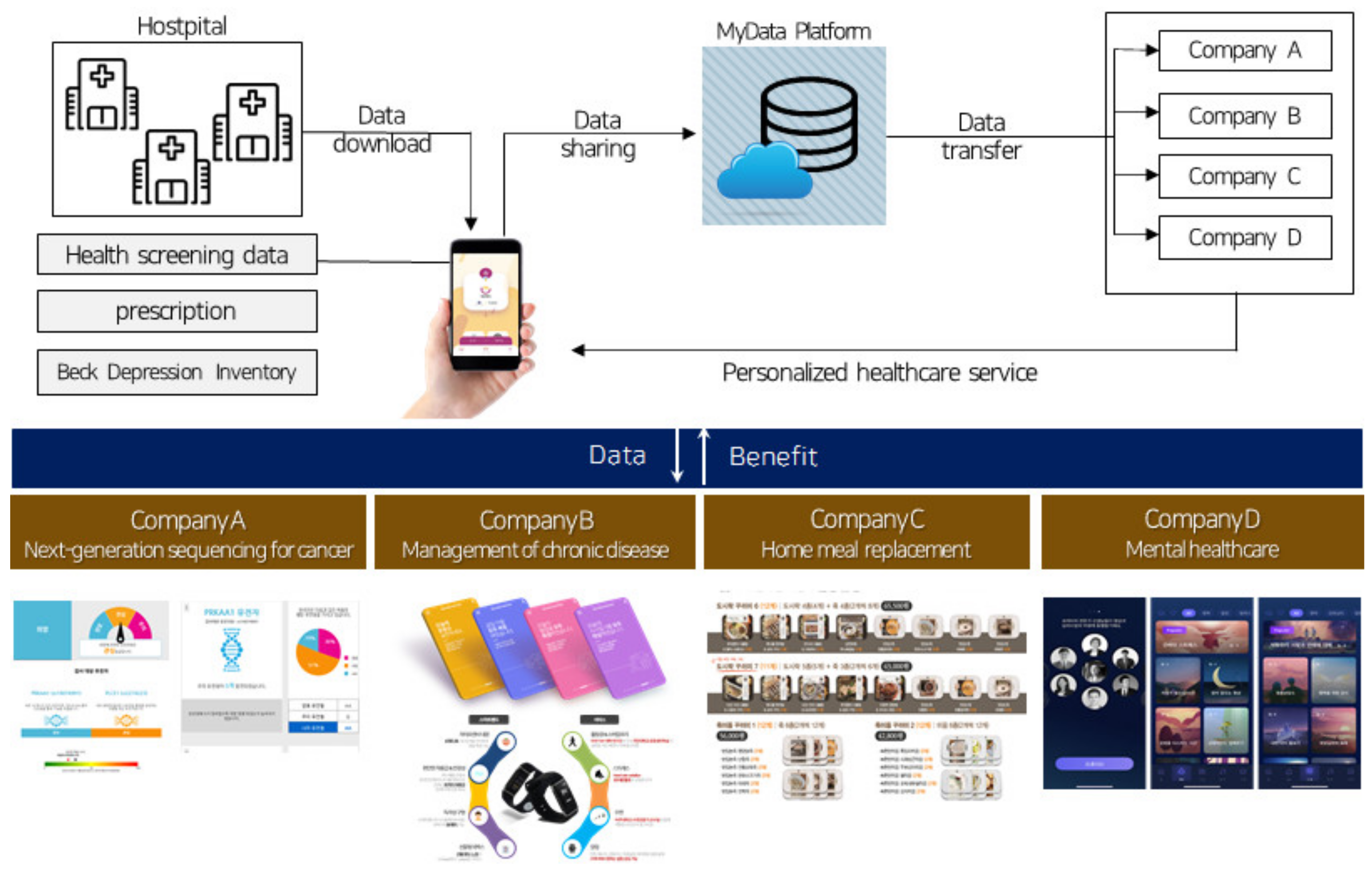
4.1. Implementation
4.2. Usage Results
5. Discussion and Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Shadbolt, N. Midata: Towards a Personal Information Revolution. In Digital Enlightenment Forum Yearbook; IOS Press: Amsterdam, The Netherlands, 2013. [Google Scholar]
- Michel, A.; Nguyen, B.; Pucheral, P. Managing distributed queries under personalized anonymity constraints. In Proceedings of the 6th International Conference on Data Science, Technology and Applications-DATA 2017, Madrid, Spain, 24–26 July 2017. [Google Scholar]
- Huang, S.K.; Pan, Y.T.; Chen, M.S. My Health Bank 2.0-making a patron saint for people’s health. J. Formos. Med. Assoc. 2017, 116, 69–71. [Google Scholar] [CrossRef]
- De Hert, P.; Papakonstantinou, V.; Malgieri, G.; Beslay, L.; Sanchez, I. The right to data portability in the GDPR: Towards user-centric interoperability of digital services. Comput. Law Secur. Rev. 2018, 34, 193–203. [Google Scholar] [CrossRef]
- Wong, J.; Henderson, T. The right to data portability in practice: Exploring the implications of the technologically neutral GDPR. Int. Data Priv. Law 2019, 9, 173–191. [Google Scholar] [CrossRef]
- Colorafi, K.; Bailey, B. It’s time for innovation in the health insurance portability and accountability act (hipaa). JMIR Med. Inform. 2016, 4, 1–5. [Google Scholar] [CrossRef]
- Lee, H.Y. My Data from the Perspective of the Nordic Model: Issues and Lessons. Korea Inf. Soc. Dev. Inst. 2020, 27, 33–64. [Google Scholar] [CrossRef]
- Harrington, E. Midata initiative update. J. Direct Data Digit. Mark. Pract. 2014, 15, 350–351. [Google Scholar] [CrossRef]
- Mitchell, A. From data hoarding to data sharing. J. Direct Data Digit. Mark. Pract. 2012, 13, 325–334. [Google Scholar] [CrossRef] [Green Version]
- Midata Innovation Lab. The Midata Innovation Opportunity. 2013. Available online: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/262271/bis-13-1314-the_midata-innovation-opportunity-v2.pdf (accessed on 19 April 2021).
- Moll, J.; Rexhepi, H.; Cajander, Å.; Grünloh, C.; Huvila, I.; Hägglund, M.; Myreteg, G.; Scandurra, I.; Åhlfeldt, R.M. Patients’ experiences of accessing their electronic health records: National patient survey in Sweden. J. Med. Internet Res. 2018, 20, 1–13. [Google Scholar] [CrossRef] [PubMed]
- PCEHR. Available online: https://www.privatehealthcareaustralia.org.au/resources/fund-resources/364-2/personally-controlled-electronic-health-record-pcehr-system/ (accessed on 20 May 2021).
- Almond, H.; Cummings, E.; Turner, P. Australia’s personally controlled electronic health record and primary healthcare: Generating a framework for implementation and evaluation. In Proceedings of the HIC, Adelaide, Australia, 15–18 July 2013; pp. 1–6. [Google Scholar]
- Basic Plan Establishment Research for Utilization of Health Care Big Data; Ministry of Health and Welfare: Taipei, Taiwan, 2015.
- Win, K.T.; Susilo, W.; Mu, Y. Personal health record systems and their security protection. J. Med. Syst. 2006, 30, 309–315. [Google Scholar] [CrossRef]
- Goldzweig, C.L.; Orshansky, G.; Paige, N.M.; Towfigh, A.A.; Haggstrom, D.A.; Miake-Lye, I.; Beroes, J.M.; Shekelle, P.G. Electronic Patient Portals: Evidence on Health Outcomes, Satisfaction, Efficiency and Attitudes. Ann. Intern. Med. 2013, 159, 677–687. [Google Scholar] [CrossRef]
- Park, Y.R.; Lee, Y.; Kim, J.Y.; Kim, J.; Kim, H.R.; Kim, Y.H.; Kim, W.S.; Lee, J.H. Managing patient-generated health data through mobile personal health records: Analysis of usage data. JMIR mHealth uHealth 2018, 6, e9620. [Google Scholar] [CrossRef] [PubMed]
- Davis, S.; Roudsari, A.; Raworth, R.; Courtney, K.L.; Mackay, L. Shared decision-making using personal health record technology: A scoping review at the crossroads. J. Am. Med. Inform. Assoc. 2017, 24, 857–866. [Google Scholar] [CrossRef] [PubMed]
- Wells, S.; Rozenblum, R.; Park, A.; Dunn, M.; Bates, D.W. Personal health records for patients with chronic disease: A major opportunity. Appl. Clin. Inform. 2014, 5, 416–429. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dash, S.; Shakyawar, S.K.; Sharma, M.; Kaushik, S. Big data in healthcare: Management, analysis and future prospects. J. Big Data 2019, 6, 54. [Google Scholar] [CrossRef] [Green Version]
- Flavián, C.; Guinalíu, M.; Gurrea, R. The role played by perceived usability, satisfaction and consumer trust on website loyalty. Inf. Manag. 2006, 43, 1–14. [Google Scholar] [CrossRef]
- Delgado-Ballester, E.; Munuera-Alemán, J.L. Brand trust in the context of consumer loyalty. Eur. J. Mark. 2001, 35, 1238–1258. [Google Scholar] [CrossRef]
- Esteves, J.; Curto, J. A risk and benefits behavioral model to assess intentions to adopt big data. J. Intell. Stud. Bus. 2013, 3, 37–46. [Google Scholar] [CrossRef] [Green Version]
- Venkatesh, V.; Morris, M.G.; Davis, G.B.; Davis, F.D. User acceptance of information technology: Toward a unified view. MIS Q. 2003, 27, 425–478. [Google Scholar] [CrossRef] [Green Version]
- Shahbaz, M.; Gao, C.; Zhai, L.L.; Shahzad, F.; Hu, Y. Investigating the adoption of big data analytics in healthcare: The moderating role of resistance to change. J. Big Data 2019, 6, 6. [Google Scholar] [CrossRef] [Green Version]
- Ball, M.P.; Chung, S.; de Zegher, I.; Fabianek, C.; Grundstrom, C.; Knowles, P.; Lähteenoja, V.; Langford, J.; Lindén, F.; Perälä-Heape, M.; et al. Mydata: Applying human-centric principles to health data. Med. Writ. 2020, 29, 64–69. [Google Scholar]
- Pinkhasov, R.M.; Wong, J.; Kashanian, J.; Lee, M.; Samadi, D.B.; Pinkhasov, M.M.; Shabsigh, R. Are men shortchanged on health? Perspective on health care utilization and health risk behavior in men and women in the United States. Int. J. Clin. Pract. 2010, 64, 475–487. [Google Scholar] [CrossRef] [PubMed]
- Morris, A.; Goodman, J.; Brading, H. Internet use and non-use: Views of older users. Univers. Access Inf. Soc. 2007, 6, 43–57. [Google Scholar] [CrossRef]
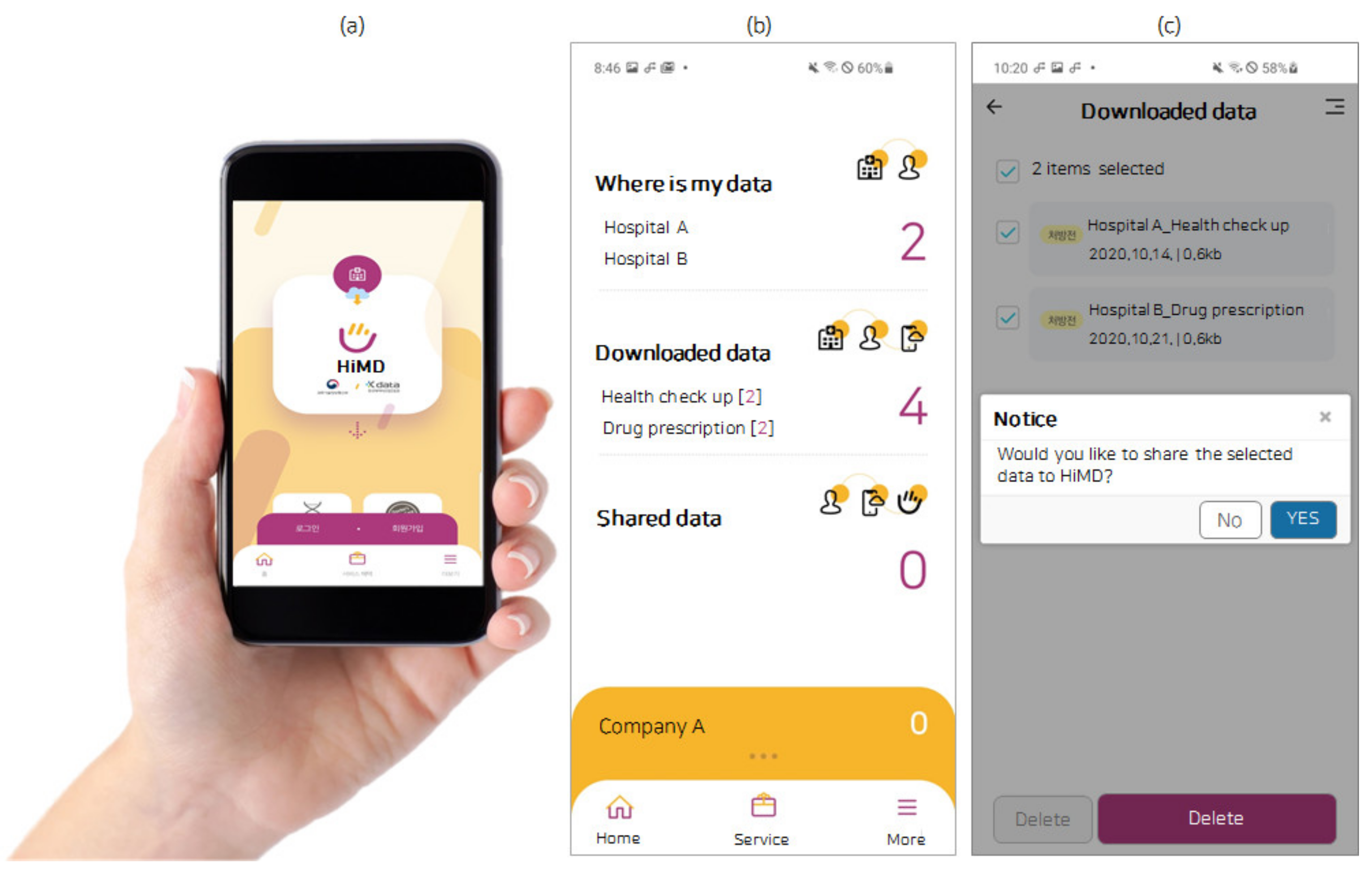
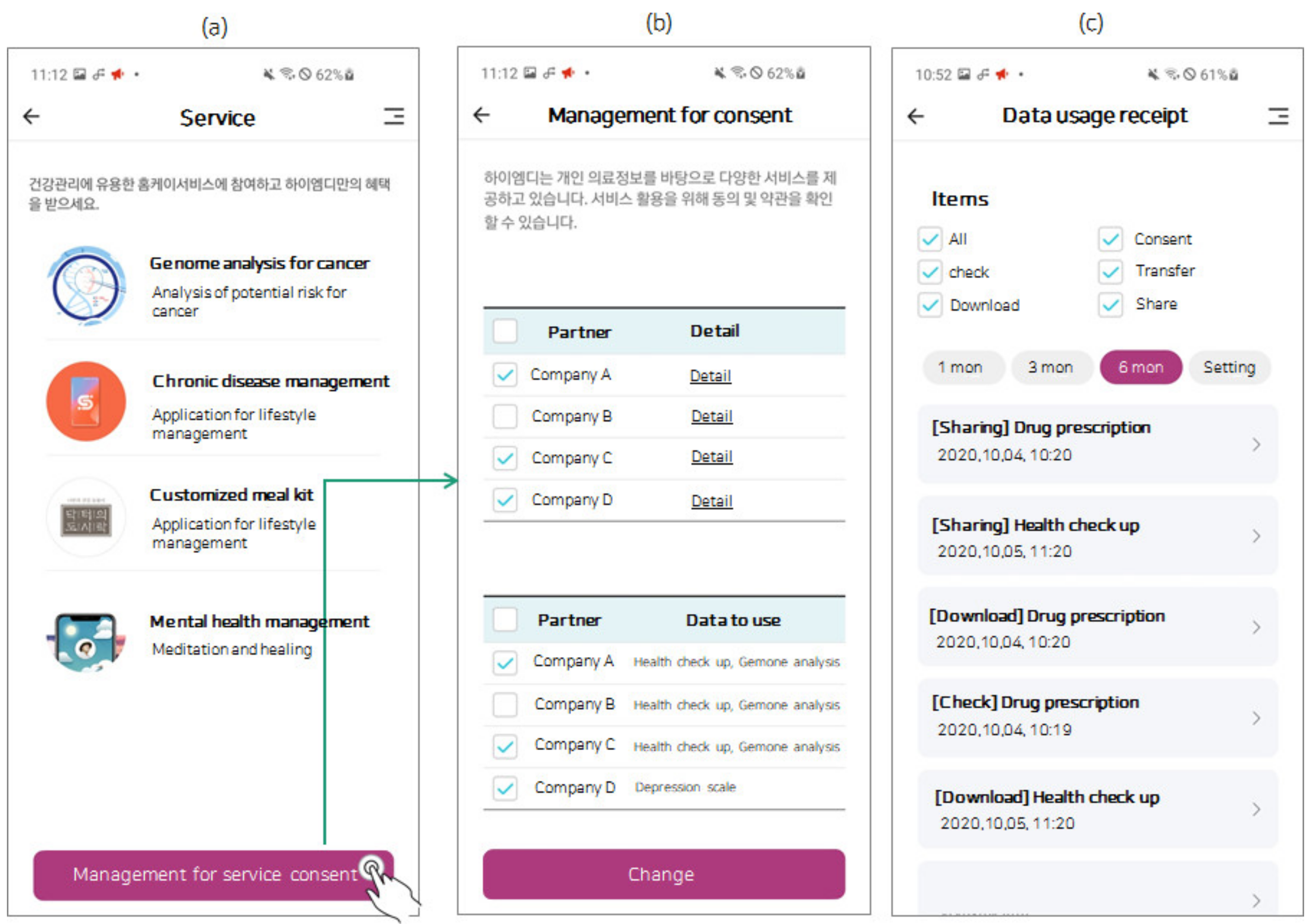

| Function | Detail |
|---|---|
| Consent | Consent to the terms of use of the platform service (users select hospitals to grant permission to use personal health records) |
| Consent to the terms of use regarding other partners that wish to use data | |
| Consent to share data, transfer data, as well as usage consent regarding third parties | |
| Data check | Searching user data among selected hospitals |
| (health check-up data, drug prescription data and depression scale testing data) | |
| Data download | Downloading data searched by users |
| Data sharing | Sharing data selected by users |
| Data transfer | Confirmation action that gives permission to a partner’s request for data transfer |
| Demographic | Category | Participants (=n) | Percent (%) | Cumulative Percent (%) |
|---|---|---|---|---|
| Total | 1269 | 100.0 | 100.0 | |
| Gender | Male | 278 | 21.9 | 21.9 |
| Female | 991 | 78.1 | 100.0 | |
| Age | 20–29 | 359 | 28.3 | 28.3 |
| 30–39 | 465 | 36.6 | 64.9 | |
| 40–49 | 267 | 21.0 | 85.9 | |
| ≥50 | 178 | 14.0 | 100.0 | |
| Hospital | Hospital A | 835 | 65.8 | 65.8 |
| Hospital B | 318 | 25.1 | 90.9 | |
| Hospital C | 116 | 9.1 | 100.0 | |
| Searching | Downloading | Data Sharing | Data Transferring | Total | |
|---|---|---|---|---|---|
| n | 1204 | 1161 | 1066 | 1007 | 1269 |
| (%) | (94.9%) | (91.5%) | (84.0%) | (79.4%) | (100%) |
| Provided Service | Person (n) | Percent (%) | |
|---|---|---|---|
| Total | 1007 | 100.0 | |
| Company A | Gene sequencing for cancer | 888 | 81.2 |
| Company B | Management of chronic disease | 707 | 70.2 |
| Company C | Home meal replacement | 357 | 35.5 |
| Company D | Mental healthcare | 240 | 23.8 |
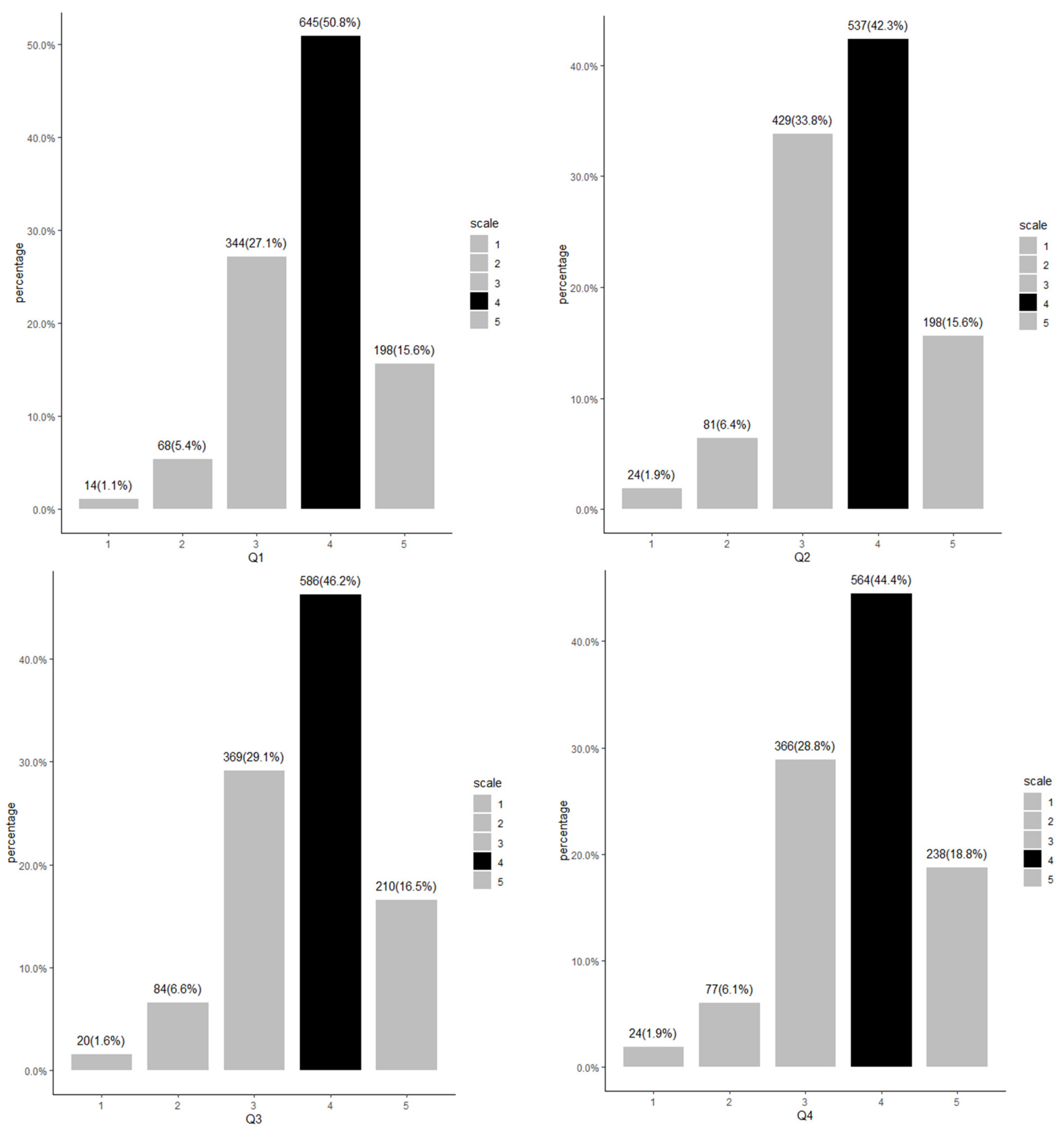
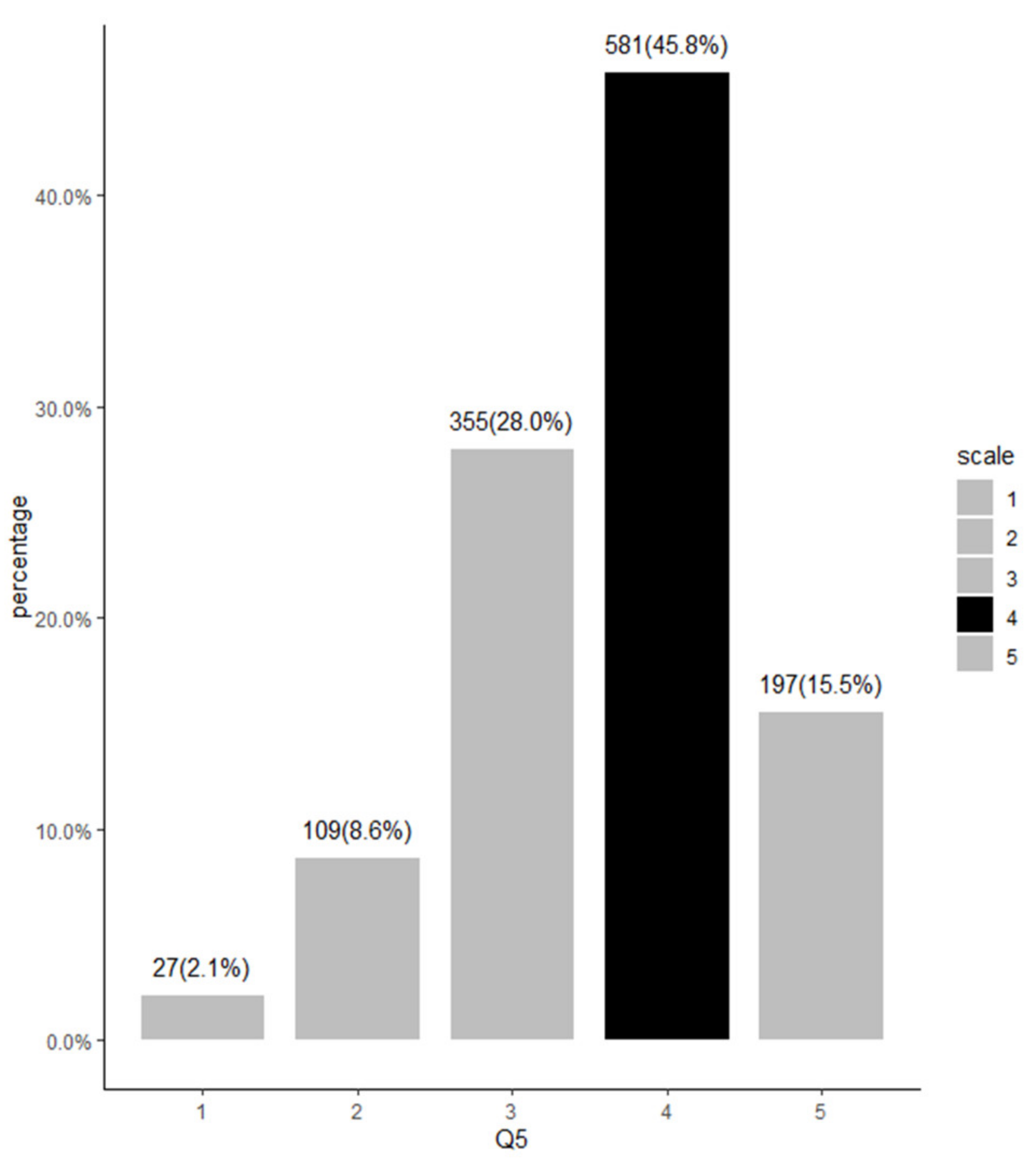
| Questionnaire | |
|---|---|
| Q 1 | I think this system is a good tool for health management |
| Q 2 | I am satisfied with the beta testing experience gained from using this system |
| Q 3 | I am satisfied with the way this system handles my medical data |
| Q 4 | I am satisfied with the services provided by this system |
| Q 5 | I intend to use this system in the future for my health management |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Choi, W.; Chun, J.-W.; Lee, S.-J.; Chang, S.-H.; Kim, D.-J.; Choi, I.Y. Development of a MyData Platform Based on the Personal Health Record Data Sharing System in Korea. Appl. Sci. 2021, 11, 8208. https://doi.org/10.3390/app11178208
Choi W, Chun J-W, Lee S-J, Chang S-H, Kim D-J, Choi IY. Development of a MyData Platform Based on the Personal Health Record Data Sharing System in Korea. Applied Sciences. 2021; 11(17):8208. https://doi.org/10.3390/app11178208
Chicago/Turabian StyleChoi, Wona, Ji-Won Chun, Seo-Joon Lee, Se-Hyun Chang, Dai-Jin Kim, and In Young Choi. 2021. "Development of a MyData Platform Based on the Personal Health Record Data Sharing System in Korea" Applied Sciences 11, no. 17: 8208. https://doi.org/10.3390/app11178208
APA StyleChoi, W., Chun, J.-W., Lee, S.-J., Chang, S.-H., Kim, D.-J., & Choi, I. Y. (2021). Development of a MyData Platform Based on the Personal Health Record Data Sharing System in Korea. Applied Sciences, 11(17), 8208. https://doi.org/10.3390/app11178208






