Predictive Ability of Fahrenheit, a Hand Motion Recording System for Assessing Hand Motor Function in Patients with Hemiplegia Post-Cerebrovascular Disease—A Pilot Study
Abstract
:Featured Application
Abstract
1. Introduction
2. Materials and Methods
2.1. Participant Selection
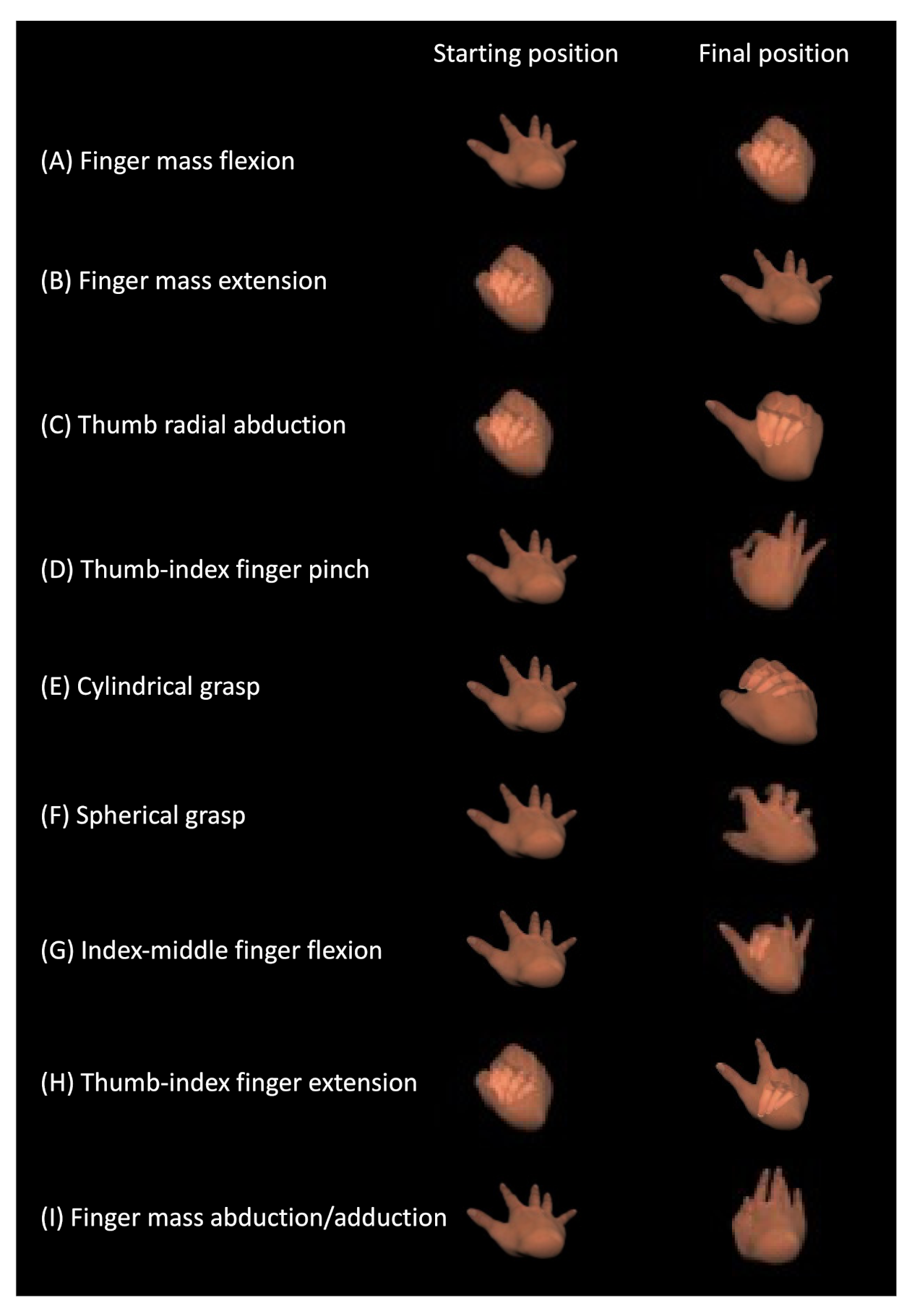
2.2. Fahrenheit Procedures
2.3. Therapist’s Assessment of Hand Function
2.4. Statistical Analysis
3. Results
3.1. BRS Assessment
3.2. Analysis Using Fahrenheit
3.3. Therapists’ Assessment of Hand Functions
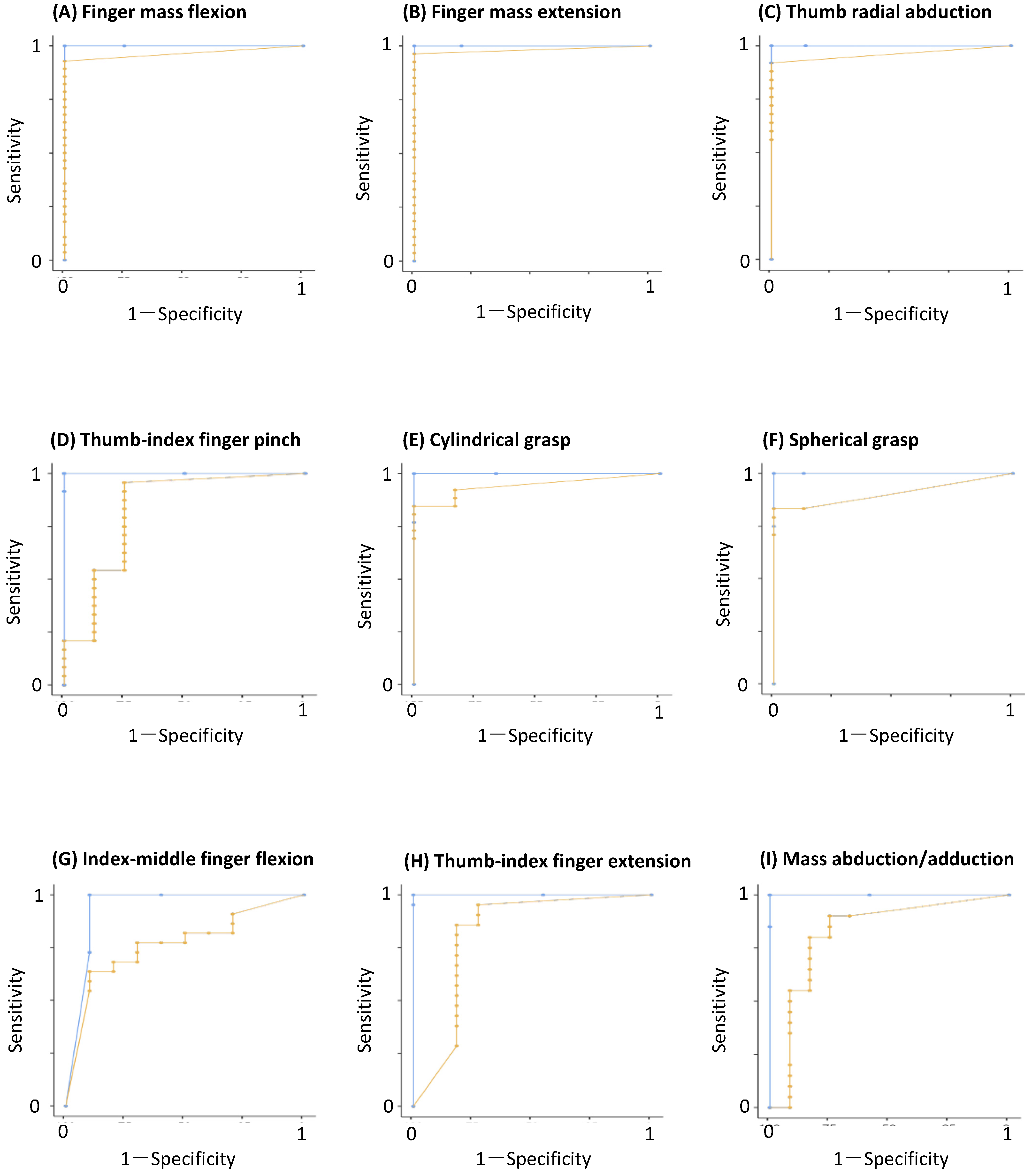
3.4. ROC Curves
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| CeVD | cerebrovascular disease |
| BRS | Brunnstrom recovery stage |
| ROC | receiver operating characteristic |
| UE | upper extremity |
| FMA | Fugl-Meyer assessment |
| 3D | three-dimensional |
| IR | infrared |
| LMC | leap motion controller |
| MCP | metacarpophalangeal |
| PIP | proximal interphalangeal |
| DIP | distal interphalangeal |
| Fps | frames per second |
| FDP | flexor digitorum profondus muscle |
| CDE | common digital extensor muscle |
References
- Mackay, J.; Mensah, G.A. The Atlas of Heart Disease and Stroke; World Health Organization: Geneva, Switzerland, 2004; pp. 50–51. [Google Scholar]
- Feydy, A.; Carlier, R.; Roby-Brami, A.; Bussel, B.; Cazalis, F.; Pierot, L.; Burnod, Y.; Maier, M.A. Longitudinal study of motor recovery after stroke: Recruitment and focusing of brain activation. Stroke 2002, 33, 1610–1617. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sawner, K.A.; LaVigne, J.M. Brunnstrom’s Movement Therapy in Hemiplegia, 2nd ed.; J. B. Lippincott Company: Philadelphia, PA, USA, 1992. [Google Scholar]
- Naghdi, S.; Ansari, N.N.; Mansouri, K.; Hasson, S. A neurophysiological and clinical study of Brunnstrom recovery stages in the upper limb following stroke. Brain Inj. 2010, 24, 1372–1378. [Google Scholar] [CrossRef] [PubMed]
- Fugl-Meyer, A.; Jääskö, L.; Leyman, I.; Olsson, S.; Steglind, S. The post-stroke hemiplegic patient. 1. a method for evaluation of physical performance. Scand. J. Rehabil. Med. 1975, 7, 13–31. [Google Scholar] [PubMed]
- Woytowicz, E.J.; Rietschel, J.C.; Goodman, R.N.; Conroy, S.S.; Sorkin, J.D.; Whitall, J.; McCombe-Waller, S. Determining levels of upper extremity movement impairment by applying a cluster analysis to the fugl-meyer assessment of the upper extremity in chronic stroke. Arch. Phys. Med. Rehabil. 2016, 98, 456–462. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gladstone, D.J.; Danells, C.J.; Black, S.E. The fugl-meyer assessment of motor recovery after stroke: A critical review of its measurement properties. Neurorehabilit. Neural Repair 2002, 16, 232–240. [Google Scholar] [CrossRef] [PubMed]
- Hondori, H.M.; Khademi, M. A review on technical and clinical impact of microsoft Kinect on physical therapy and rehabilitation. J. Med. Eng. 2014, 2014, 846514. [Google Scholar] [CrossRef] [Green Version]
- Ultraleap. Available online: http://www.ultraleap.com (accessed on 30 May 2021).
- Weichert, F.; Bachmann, D.; Rudak, B.; Fisseler, D. Analysis of the accuracy and robustness of the leap motion controller. Sensors 2013, 13, 6380–6393. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Smeragliuolo, A.H.; Hill, N.J.; Disla, L.; Putrino, D. Validation of the leap motion controller using markered motion capture technology. J. Biomech. 2016, 49, 1742–1750. [Google Scholar] [CrossRef] [PubMed]
- Unity. Available online: http://japan.unity3d.com (accessed on 1 April 2019).
- Hsu, A.T.; Chang, J.H.; Chang, C.H. Determining the resting position of the glenohumeral joint: A cadaver study. J. Orthop. Sports Phys. Ther. 2002, 32, 605–612. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Youden, W.J. Index for rating diagnostic tests. Cancer 1950, 3, 32–35. [Google Scholar] [CrossRef]
- DeLong, E.R.; DeLong, D.M.; Clarke-Pearson, D.L. Comparing the areas under two or more correlated receiver operating characteristic curves: A nonparametric approach. Biometrics 1988, 44, 837–845. [Google Scholar] [CrossRef] [PubMed]
- Jamovi. Available online: https://www.jamovi.org (accessed on 10 October 2020).
- Del Din, S.; Patel, S.; Cobelli, C.; Bonato, P. Estimating fugl-meyer clinical scores in stroke survivors using wearable sensors. In Proceedings of the Annual International Conference of the IEEE Engineering in Medicine and Biology Society, Boston, MA, USA, 30 August–3 September 2011. [Google Scholar]
- Lee, S.; Lee, Y.S.; Kim, J. Automated evaluation of upper-limb motor function impairment using fugl-meyer assessment. IEEE Trans. Neural Syst. Rehabil. Eng. 2018, 26, 125–134. [Google Scholar] [CrossRef] [PubMed]
- Kim, W.S.; Cho, S.; Baek, D.; Bang, H.; Paik, N.J. Upper extremity functional evaluation by Fugl-Meyer assessment scoring using depth-sensing camera in hemiplegic stroke patients. PLoS ONE 2016, 11, e0158640. [Google Scholar] [CrossRef] [PubMed]
- Butt, A.H.; Rovini, E.; Dolciotti, C.; Bongioanni, P.; De Petris, G.; Cavallo, F. Leap motion evaluation for assessment of upper limb motor skills in Parkinson’s disease. In Proceedings of the 2017 IEEE International Conference on Rehabilitation Robotics, London, UK, 17–20 July 2017; pp. 116–121. [Google Scholar] [CrossRef]
- Lugo, G.; Ibarra-Manzano, M.; Ba, F.; Cheng, I. Virtual reality and hand tracking system as a medical tool to evaluate patients with Parkinson’s. In Virtual Reality and Hand Tracking System as a Medical Tool to Evaluate Patients with Parkinson’s, Proceedings of the 11th EAI International Conference on Pervasive Computing Technologies for Healthcare, Barcelona, Spain, 23–26 May 2017; Association for Computing Machinery: New York, NY, USA, 2017; pp. 405–408. [Google Scholar] [CrossRef]
- Nordin, N.; Xie, S.Q.; Wünsche, B. Assessment of movement quality in robot-Assisted upper limb rehabilitation after stroke: A review. J. Neuroeng. Rehabil. 2014, 11, 1–23. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, Y.-W.; Liao, W.-W.; Chen, C.-L.; Wu, C.-Y. Kinematic descriptions of upper limb function using simulated tasks in activities of daily living after stroke. Hum. Mov. Sci. 2021, 79, 102834. [Google Scholar] [CrossRef] [PubMed]


| Characteristics | Statistics |
|---|---|
| Mean age: mean years (range) | 67 (39–87) |
| Sex: female/male | 8/24 |
| Hand dominance: right/left | 31/1/0 |
| Mean time since CeVD onset: mean days (range) | 13 (2–37) |
| CeVD lesion side: right/left | 13/19 |
| Type of CeVD: ischemic/hemorrhagic | 25/7 |
| Brunnstrom recovery stage (hand): I/II/III/IV/V/VI | 1/3/5/7/7/9 |
| Tasks | Number of Patients Allocated Each BRS Score (0/1) | Mean Values ± SD Recorded with Fahrenheit (BRS Score Assigned as 0/1) | T Value | p Value | |
|---|---|---|---|---|---|
| (A) Finger mass flexion | 4/28 | 0.00 ± 0.00/0.58 ± 0.18 | 11.46 | <0.001 | |
| (B) Finger mass extension | 5/27 | 0.00 ± 0.00/0.74 ± 0.17 | 19.00 | <0.001 | |
| (C) Thumb radial abduction | 7/25 | 0.00 ± 0.00/0.81 ± 0.32 | 10.80 | <0.001 | |
| (D) Thumb-index finger pinch | 8/24 | 0.22 ± 0.40/0.77 ± 0.22 | 2.73 | 0.005 | |
| (E) Cylindrical grasp | 6/26 | 0.27 ± 0.11/0.87 ± 0.31 | 3.91 | <0.001 | |
| (F) Spherical grasp | 8/24 | 0.10 ± 0.29/0.83 ± 0.38 | 4.58 | <0.001 | |
| (G) Index-middle finger flexion | 22/10 | 0.33 ± 0.45/0.80 ± 0.31 | 2.64 | 0.007 | |
| (H) Thumb-index finger extension | 11/21 | 0.23 ± 0.42/0.85 ± 0.26 | 3.67 | <0.001 | |
| (I) Finger mass abduction/adduction | 12/20 | 0.27 ± 0.42/0.84 ± 0.30 | 3.56 | <0.001 | |
| Tasks | Cut-Off Value | Predictive Measures | Youden’s Index | Goodness-of-Fit | |||||
|---|---|---|---|---|---|---|---|---|---|
| Accuracy | Specificity | Sensitivity | AUC | AIC | R2 | p | |||
| (A) Finger mass flexion | 0.407 | 0.938 | 1.000 | 0.929 | 0.964 | 0.929 | 11.6 | 0.683 | <0.001 |
| (B) Finger mass extension | 0.524 | 0.969 | 1.000 | 0.963 | 0.981 | 0.963 | 9.41 | 0.805 | <0.001 |
| (C) Thumb radial abduction | 0.299 | 0.938 | 1.000 | 0.920 | 0.960 | 0.920 | 13.5 | 0.716 | <0.001 |
| (D) Thumb-index finger pinch | 0.336 | 0.719 | 0.750 | 0.958 | 0.828 | 0.708 | 26.1 | 0.387 | <0.001 |
| (E) Cylindrical grasp | 0.913 | 0.844 | 1.000 | 0.846 | 0.942 | 0.846 | 19.6 | 0.495 | <0.001 |
| (F) Spherical grasp | 0.983 | 0.844 | 1.000 | 0.833 | 0.906 | 0.833 | 25.2 | 0.410 | 0.005 |
| (G) Index-middle finger flexion | 0.005 | 0.719 | 0.900 | 0.636 | 0.764 | 0.536 | 35.7 | 0.202 | 0.021 |
| (H) Thumb-index finger extension | 0.363 | 0.813 | 0.727 | 0.952 | 0.814 | 0.680 | 29.1 | 0.391 | <0.001 |
| (I) Finger mass abduction/adduction | 0.570 | 0.813 | 0.750 | 0.900 | 0.821 | 0.650 | 32.9 | 0.318 | 0.003 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Saito, T.; Ishioka, T.; Yoshimura, S.; Hamaguchi, T. Predictive Ability of Fahrenheit, a Hand Motion Recording System for Assessing Hand Motor Function in Patients with Hemiplegia Post-Cerebrovascular Disease—A Pilot Study. Appl. Sci. 2021, 11, 8153. https://doi.org/10.3390/app11178153
Saito T, Ishioka T, Yoshimura S, Hamaguchi T. Predictive Ability of Fahrenheit, a Hand Motion Recording System for Assessing Hand Motor Function in Patients with Hemiplegia Post-Cerebrovascular Disease—A Pilot Study. Applied Sciences. 2021; 11(17):8153. https://doi.org/10.3390/app11178153
Chicago/Turabian StyleSaito, Takeshi, Toshiyuki Ishioka, Sho Yoshimura, and Toyohiro Hamaguchi. 2021. "Predictive Ability of Fahrenheit, a Hand Motion Recording System for Assessing Hand Motor Function in Patients with Hemiplegia Post-Cerebrovascular Disease—A Pilot Study" Applied Sciences 11, no. 17: 8153. https://doi.org/10.3390/app11178153
APA StyleSaito, T., Ishioka, T., Yoshimura, S., & Hamaguchi, T. (2021). Predictive Ability of Fahrenheit, a Hand Motion Recording System for Assessing Hand Motor Function in Patients with Hemiplegia Post-Cerebrovascular Disease—A Pilot Study. Applied Sciences, 11(17), 8153. https://doi.org/10.3390/app11178153






