Improved Anti-Washout Property of Calcium Sulfate/Tri-Calcium Phosphate Premixed Bone Substitute with Glycerin and Hydroxypropyl Methylcellulose
Abstract
1. Introduction
2. Materials and Methods
2.1. Preparation of Premixed Putty
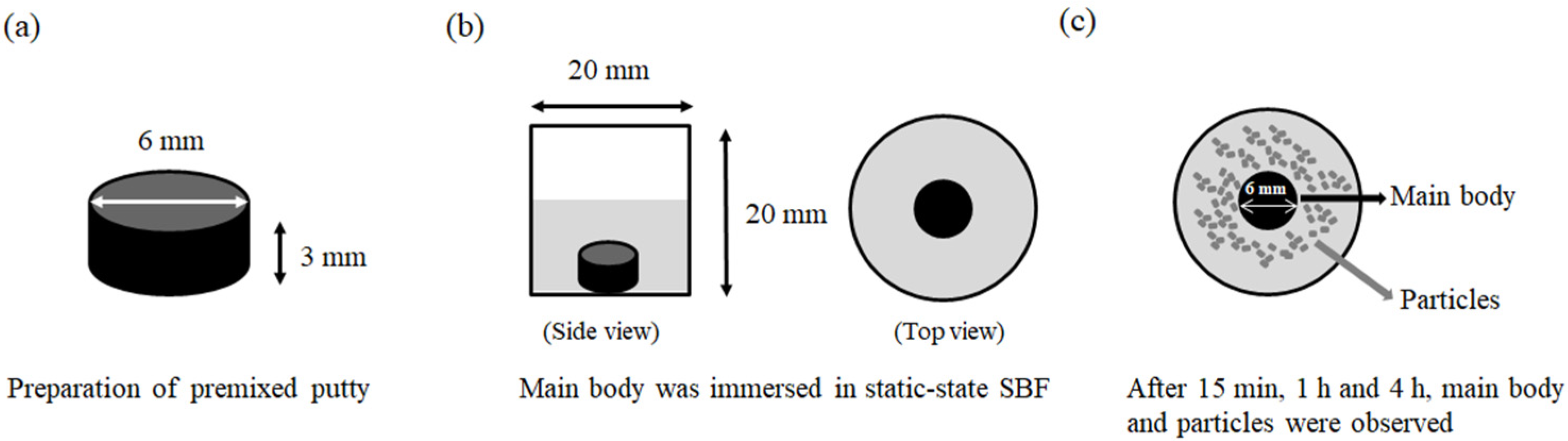
2.2. Washout Resistance Test
2.3. Analysis of the Particles
2.4. Microstructure and Phase Composition
2.5. Statistical Analysis
3. Results
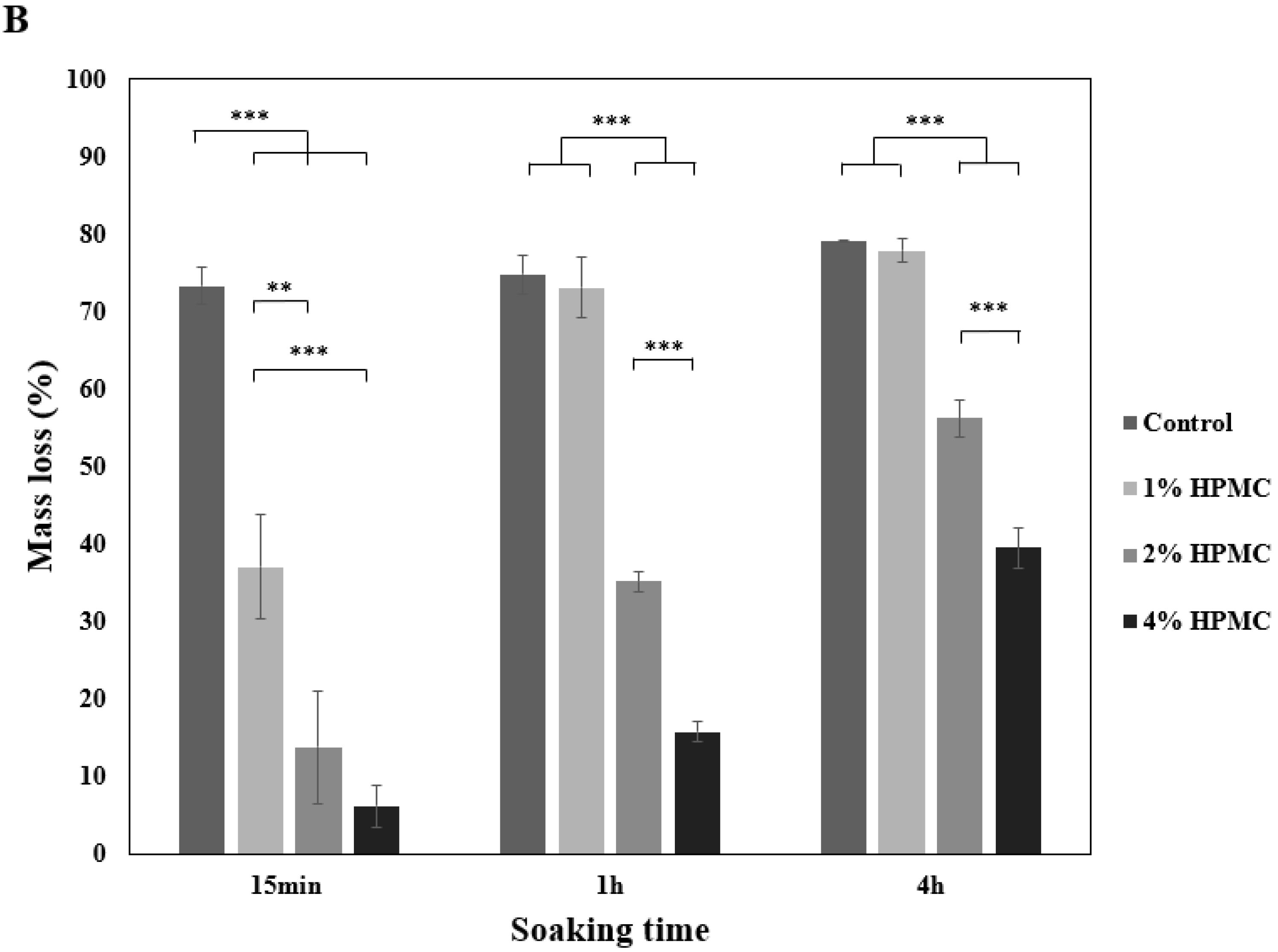
3.1. Washout Resistance of Premixed Putty at Different Ratios
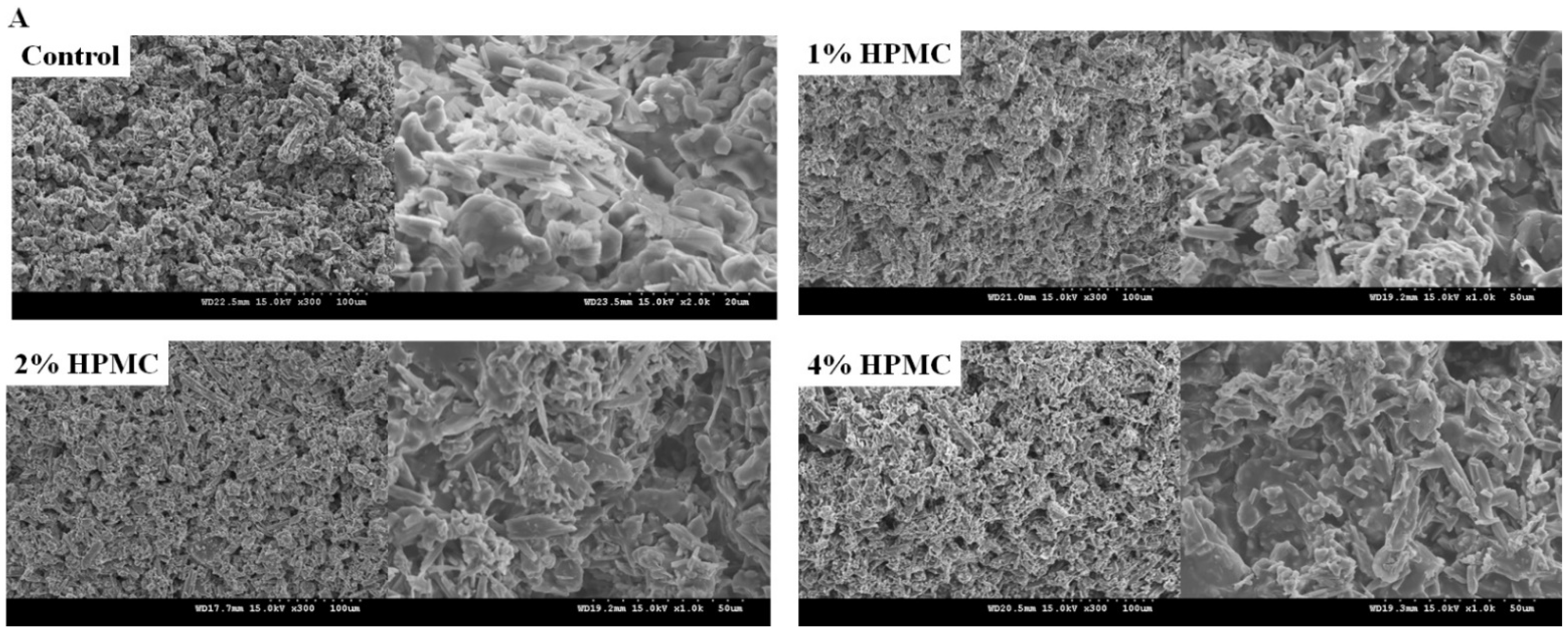
3.2. Surface Morphology Analysis
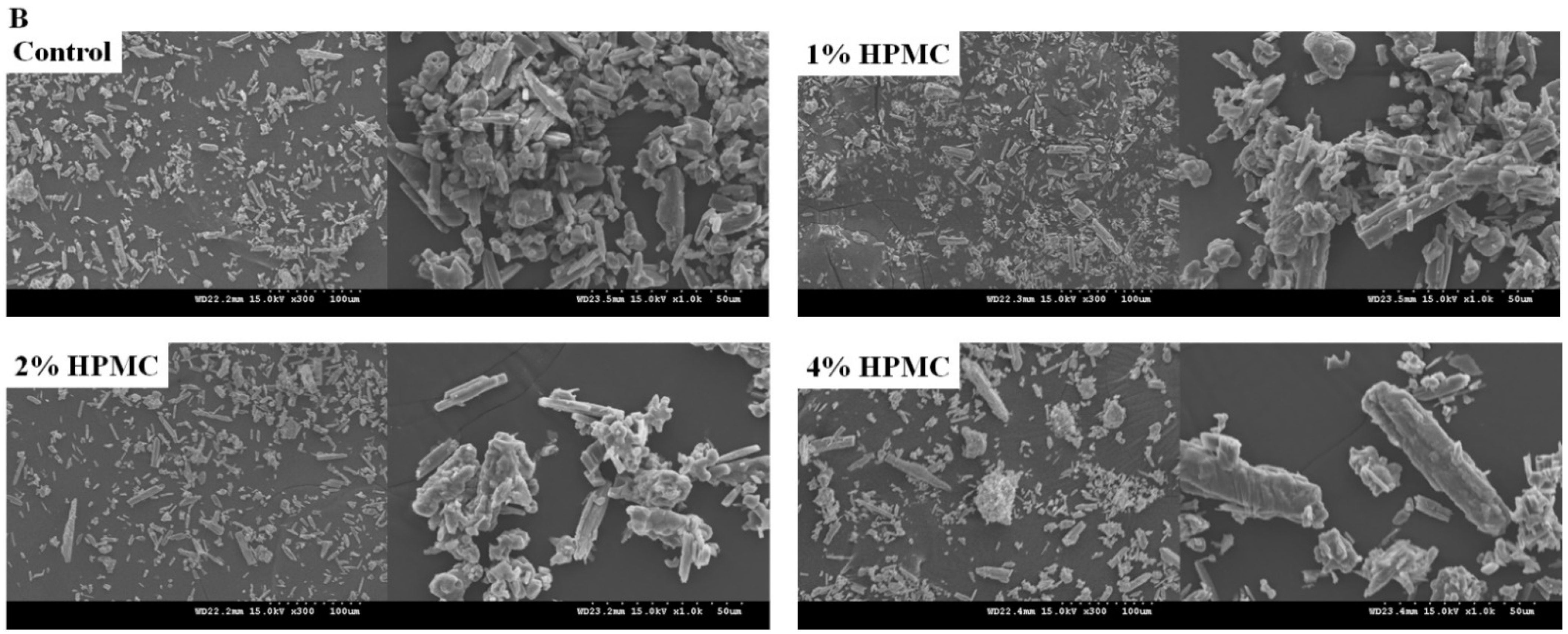
3.3. Morphology of Premixed Putty with Collapsed Particle Structures
3.4. X-ray Diffractometer Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Jia, P.; Tang, H.; Chen, H.; Bao, L.; Feng, F.; Yang, H.; Li, J. Prophylactic vertebroplasty procedure applied with a resorbable bone cement can decrease the fracture risk of sandwich vertebrae: Long-term evaluation of clinical outcomes. Regen. Biomater. 2017, 4, 47–53. [Google Scholar] [CrossRef] [PubMed]
- Liao, J.-C.; Fan, K.-F.; Keorochana, G.; Chen, W.-J.; Chen, L.-H. Transpedicular grafting after short-segment pedicle instrumentation for thoracolumbar burst fracture: Calcium sulfate cement versus autogenous iliac bone graft. Spine 2010, 35, 1482–1488. [Google Scholar] [CrossRef] [PubMed]
- Sinjab, Y.H.; Sinjab, K.H.; Navarrete-Bedoya, C.; Gutmann, J.L. Calcium sulfate applications in dentistry: A literature review. Endodontology 2020, 32, 167. [Google Scholar]
- Scarano, A.; Carinci, F.; Cimorelli, E.; Quaranta, M.; Piattelli, A. Application of calcium sulfate in surgical-orthodontic treatment of impacted teeth: A new procedure to control hemostasis. J. Oral Maxillofac. Surg. 2010, 68, 964–968. [Google Scholar] [CrossRef]
- Strocchi, R.; Orsini, G.; Iezzi, G.; Scarano, A.; Rubini, C.; Pecora, G.; Piattelli, A. Bone regeneration with calcium sulfate: Evidence for increased angiogenesis in rabbits. J. Oral Implantol. 2002, 28, 273–278. [Google Scholar] [CrossRef]
- Wang, W.; Yeung, K.W. Bone grafts and biomaterials substitutes for bone defect repair: A review. Bioact. Mater. 2017, 2, 224–247. [Google Scholar] [CrossRef]
- Ginebra, M.-P.; Espanol, M.; Montufar, E.B.; Perez, R.A.; Mestres, G. New processing approaches in calcium phosphate cements and their applications in regenerative medicine. Acta Biomater. 2010, 6, 2863–2873. [Google Scholar] [CrossRef]
- Urban, R.M.; Turner, T.M.; Hall, D.J.; Inoue, N.; Gitelis, S. Increased bone formation using calcium sulfate-calcium phosphate composite graft. Clin. Orthop. Relat. Res.® 2007, 459, 110–117. [Google Scholar] [CrossRef]
- Landgraeber, S.; Warwas, S.; Claßen, T.; Jäger, M. Modifications to advanced Core decompression for treatment of Avascular necrosis of the femoral head. BMC Musculoskelet. Disord. 2017, 18, 1–8. [Google Scholar] [CrossRef]
- Bohner, M. Resorbable biomaterials as bone graft substitutes. Mater. Today 2010, 13, 24–30. [Google Scholar] [CrossRef]
- Sandiford, N.A. Complication rates are low with the use of Stimulan calcium sulphate based antibiotic delivery system in the management of patients with hip-related PJI: Early results of a consecutive case series. HIP Int. 2020, 30, 3–6. [Google Scholar] [CrossRef]
- Wang, J.-Y.; Cheng, C.-Y.; Chen, A.C.-Y.; Chan, Y.-S. Arthroscopy-assisted corrective osteotomy, reduction, internal fixation and strut allograft augmentation for tibial plateau malunion or nonunion. J. Clin. Med. 2020, 9, 973. [Google Scholar] [CrossRef]
- Peersman, G.; Laskin, R.; Davis, J.; Peterson, M.; Richart, T. Prolonged operative time correlates with increased infection rate after total knee arthroplasty. HSS J.® 2006, 2, 70–72. [Google Scholar] [CrossRef]
- Friesenbichler, J.; Maurer-Ertl, W.; Sadoghi, P.; Pirker-Fruehauf, U.; Bodo, K.; Leithner, A. Adverse reactions of artificial bone graft substitutes: Lessons learned from using tricalcium phosphate geneX®. Clin. Orthop. Relat. Res.® 2014, 472, 976–982. [Google Scholar] [CrossRef]
- Park, J.-H.; Suh, S.-J.; Lee, Y.-S.; Lee, J.-H.; Ryu, K.-Y.; Kang, D.-G. Lytic Complications after Skull Reconstruction Using GeneX®. Korean J. Neurotrauma 2015, 11, 135. [Google Scholar] [CrossRef][Green Version]
- Wang, X.; Chen, L.; Xiang, H.; Ye, J. Influence of anti-washout agents on the rheological properties and injectability of a calcium phosphate cement. J. Biomed. Mater. Res. Part B Appl. Biomater. 2007, 81, 410–418. [Google Scholar] [CrossRef]
- Sato, T.; Kikuchi, M.; Aizawa, M. Preparation of hydroxyapatite/collagen injectable bone paste with an anti-washout property utilizing sodium alginate. Part 1: Influences of excess supplementation of calcium compounds. J. Mater. Sci. Mater. Med. 2017, 28, 49. [Google Scholar] [CrossRef]
- Yokoyama, A.; Yamamoto, S.; Kawasaki, T.; Kohgo, T.; Nakasu, M. Development of calcium phosphate cement using chitosan and citric acid for bone substitute materials. Biomaterials 2002, 23, 1091–1101. [Google Scholar] [CrossRef]
- Li, X.; He, F.; Ye, J. Preparation, characterization and in vitro cell performance of anti-washout calcium phosphate cement modified by sodium polyacrylate. RSC Adv. 2017, 7, 32842–32849. [Google Scholar] [CrossRef]
- Tamimi, F.; Kumarasami, B.; Doillon, C.; Gbureck, U.; Le Nihouannen, D.; Cabarcos, E.L.; Barralet, J.E. Brushite–collagen composites for bone regeneration. Acta Biomater. 2008, 4, 1315–1321. [Google Scholar] [CrossRef]
- Alkhraisat, M.; Rueda, C.; Marino, F.; Torres, J.; Jerez, L.; Gbureck, U.; Cabarcos, E. The effect of hyaluronic acid on brushite cement cohesion. Acta Biomater. 2009, 5, 3150–3156. [Google Scholar] [CrossRef]
- Liu, W.; Zhang, J.; Rethore, G.; Khairoun, K.; Pilet, P.; Tancret, F.; Bouler, J.-M.; Weiss, P. A novel injectable, cohesive and toughened Si-HPMC (silanized-hydroxypropyl methylcellulose) composite calcium phosphate cement for bone substitution. Acta Biomater. 2014, 10, 3335–3345. [Google Scholar] [CrossRef] [PubMed]
- Bigi, A.; Bracci, B.; Panzavolta, S. Effect of added gelatin on the properties of calcium phosphate cement. Biomaterials 2004, 25, 2893–2899. [Google Scholar] [CrossRef]
- Qian, G.; Li, X.; He, F.; Ye, J. Improving the anti-washout property of calcium phosphate cement by introducing konjac glucomannan/κ-carrageenan blend. J. Biomater. Appl. 2019, 33, 1094–1104. [Google Scholar] [CrossRef]
- Xie, Y.; Liu, J.; Cai, S.; Bao, X.; Li, Q.; Xu, G. Setting Characteristics and High Compressive Strength of an Anti-washout, Injectable Calcium Phosphate Cement Combined with Thermosensitive Hydrogel. Materials 2020, 13, 5779. [Google Scholar] [CrossRef] [PubMed]
- Bohner, M. Design of ceramic-based cements and putties for bone graft substitution. Eur. Cell Mater. 2010, 20, 3–10. [Google Scholar] [CrossRef]
- Takagi, S.; Chow, L.C.; Hirayama, S.; Sugawara, A. Premixed calcium–phosphate cement pastes. J. Biomed. Mater. Res. Part B Appl. Biomater. 2003, 67, 689–696. [Google Scholar] [CrossRef]
- Carey, L.E.; Xu, H.H.; Simon Jr, C.G.; Takagi, S.; Chow, L.C. Premixed rapid-setting calcium phosphate composites for bone repair. Biomaterials 2005, 26, 5002–5014. [Google Scholar] [CrossRef]
- Xu, H.H.; Carey, L.E.; Simon, C.G., Jr.; Takagi, S.; Chow, L.C. Premixed calcium phosphate cements: Synthesis, physical properties, and cell cytotoxicity. Dent. Mater. 2007, 23, 433–441. [Google Scholar] [CrossRef]
- Jyoti, M.A.; Min, Y.K.; Lee, B.-T.; Song, H.-Y. In vitro bioactivity and biocompatibility of calcium phosphate cements using Hydroxy-propyl-methyl-Cellulose (HPMC). Appl. Surf. Sci. 2010, 257, 1533–1539. [Google Scholar] [CrossRef]
- Yao, Q.; Ye, J.; Xu, Q.; Mo, A.; Gong, P. Composite scaffolds of dicalcium phosphate anhydrate/multi-(amino acid) copolymer: In vitro degradability and osteoblast biocompatibility. J. Biomater. Sci. Polymer Ed. 2015, 26, 211–223. [Google Scholar] [CrossRef] [PubMed]
- Pandey, A.; Kuo, C.-L.; Liang, C.-J.; Chang, L.-Y.; Hsu, C.-Y.; Lee, S.-Y.; Teng, N.-C.; Yang, J.-C. 3D pore-interconnected calcium phosphate bone blocks for bone tissue engineering. Ceram. Int. 2020, 46, 16465–16471. [Google Scholar] [CrossRef]
- Iqbal, H.; Ali, M.; Zeeshan, R.; Mutahir, Z.; Iqbal, F.; Nawaz, M.A.H.; Shahzadi, L.; Chaudhry, A.A.; Yar, M.; Luan, S. Chitosan/hydroxyapatite (HA)/hydroxypropylmethyl cellulose (HPMC) spongy scaffolds-synthesis and evaluation as potential alveolar bone substitutes. Colloids Surf. B Biointerfaces 2017, 160, 553–563. [Google Scholar] [CrossRef]
- Struillou, X.; Rakic, M.; Badran, Z.; Macquigneau, L.; Colombeix, C.; Pilet, P.; Verner, C.; Gauthier, O.; Weiss, P.; Soueidan, A. The association of hydrogel and biphasic calcium phosphate in the treatment of dehiscence-type peri-implant defects: An experimental study in dogs. J. Mater. Sci. Mater. Med. 2013, 24, 2749–2760. [Google Scholar] [CrossRef]
- Woo, K.M.; Yu, B.; Jung, H.M.; Lee, Y.K. Comparative evaluation of different crystal-structured calcium sulfates as bone-filling materials. J. Biomed. Mater. Res. Part B Appl. Biomater. 2009, 91, 545–554. [Google Scholar] [CrossRef]
- Urban, R.M.; Turner, T.M.; Hall, D.J.; Infanger, S.I.; Cheema, N.; Lim, T.H.; Richelsoph, K. An injectable calcium sulfate-based bone graft putty using hydroxypropylmethylcellulose as the plasticizer. Orthopedics 2004, 27, S155–S159. [Google Scholar] [CrossRef]
- Wang, X.; Ye, J.; Wang, H. Effects of additives on the rheological properties and injectability of a calcium phosphate bone substitute material. J. Biomed. Mater. Res. Part B Appl. Biomater. 2006, 78, 259–264. [Google Scholar] [CrossRef] [PubMed]
- Wang, P.; Lee, E.J.; Park, C.S.; Yoon, B.H.; Shin, D.S.; Kim, H.E.; Koh, Y.H.; Park, S.H. Calcium sulfate hemihydrate powders with a controlled morphology for use as bone cement. J. Am. Ceram. Soc. 2008, 91, 2039–2042. [Google Scholar] [CrossRef]
- Kokubo, T.; Takadama, H. How useful is SBF in predicting in vivo bone bioactivity? Biomaterials 2006, 27, 2907–2915. [Google Scholar] [CrossRef] [PubMed]
- Zhou, H.; Yang, M.; Ni, X.; Yang, L.; Kutty, M.G. Using calcium sulfate cement—Hydroxypropyl methyl cellulose/sodium alginate composites as substitutes of bone wax. Int. J. Appl. Ceram. Technol. 2018, 15, 903–909. [Google Scholar] [CrossRef]
- Nokhodchi, A.; Ford, J.L.; Rubinstein, M.H. Studies on the interaction between water and (hydroxypropyl) methylcellulose. J. Pharm. Sci. 1997, 86, 608–615. [Google Scholar] [CrossRef]
- Pioletti, D.P.; Takei, H.; Lin, T.; Van Landuyt, P.; Ma, Q.J.; Kwon, S.Y.; Sung, K.-L.P. The effects of calcium phosphate cement particles on osteoblast functions. Biomaterials 2000, 21, 1103–1114. [Google Scholar] [CrossRef]
- Lebre, F.; Sridharan, R.; Sawkins, M.J.; Kelly, D.J.; O’Brien, F.J.; Lavelle, E.C. The shape and size of hydroxyapatite particles dictate inflammatory responses following implantation. Sci. Rep. 2017, 7, 2922. [Google Scholar] [CrossRef] [PubMed]
- Gallo, J.; Slouf, M.; Goodman, S.B. The relationship of polyethylene wear to particle size, distribution, and number: A possible factor explaining the risk of osteolysis after hip arthroplasty. J. Biomed. Mater. Res. Part B Appl. Biomater. 2010, 94, 171–177. [Google Scholar] [CrossRef]
- Goodman, S.B.; Gibon, E.; Yao, Z. The basic science of periprosthetic osteolysis. Instr. Course Lect. 2013, 62, 201. [Google Scholar]


| CSH (wt%) | β-TCP (wt%) | HPMC (wt%) | |
|---|---|---|---|
| Control | 50 | 50 | 0 |
| 1% HPMC | 49.5 | 49.5 | 1 |
| 2% HPMC | 49 | 49 | 2 |
| 4% HPMC | 48 | 48 | 4 |
| Control | 1% HPMC | 2% HPMC | 4% HPMC | |
|---|---|---|---|---|
| Particle length (μm) | 10.07 (7.73) [2.67–47.24] | 9.658 (6.7) [2.27–44.11] | 11.73 (7.953) [7.94–68.63] | 24.6 (18.67) *** [5.5–124.95] |
| Aspect ratio | 2.23 (1.75) [0.84–10.58] | 2.97 (2.11) [1–9.97] | 2.55 (2.19) [1.01–10.78] | 2.13 (1.67) [1–9.69] |
| Control (%) | 1% HPMC (%) | 2% HPMC (%) | 4% HPMC (%) | |
|---|---|---|---|---|
| <10 μm | 49.6 | 49.2 | 39.2 | 6.4 |
| 11–30 μm | 47.6 | 47.2 | 58.4 | 58.8 |
| >30 μm | 2.8 | 3.6 | 2.4 | 34.8 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chiang, H.-H.; Su, C.-Y.; Hsu, L.-H.; Yang, M.-H.; Fang, H.-W. Improved Anti-Washout Property of Calcium Sulfate/Tri-Calcium Phosphate Premixed Bone Substitute with Glycerin and Hydroxypropyl Methylcellulose. Appl. Sci. 2021, 11, 8136. https://doi.org/10.3390/app11178136
Chiang H-H, Su C-Y, Hsu L-H, Yang M-H, Fang H-W. Improved Anti-Washout Property of Calcium Sulfate/Tri-Calcium Phosphate Premixed Bone Substitute with Glycerin and Hydroxypropyl Methylcellulose. Applied Sciences. 2021; 11(17):8136. https://doi.org/10.3390/app11178136
Chicago/Turabian StyleChiang, Hsiao-Hung, Chen-Ying Su, Ling-Hsiang Hsu, Min-Hsuan Yang, and Hsu-Wei Fang. 2021. "Improved Anti-Washout Property of Calcium Sulfate/Tri-Calcium Phosphate Premixed Bone Substitute with Glycerin and Hydroxypropyl Methylcellulose" Applied Sciences 11, no. 17: 8136. https://doi.org/10.3390/app11178136
APA StyleChiang, H.-H., Su, C.-Y., Hsu, L.-H., Yang, M.-H., & Fang, H.-W. (2021). Improved Anti-Washout Property of Calcium Sulfate/Tri-Calcium Phosphate Premixed Bone Substitute with Glycerin and Hydroxypropyl Methylcellulose. Applied Sciences, 11(17), 8136. https://doi.org/10.3390/app11178136






