Prevention of Mandible Fractures in Medication-Related Osteonecrosis of the Jaws: The Role of Virtual Surgical Planning and Computer-Aided Design and Manufacturing in Two Clinical Case Reports
Abstract
Featured Application
Abstract
1. Introduction
2. Case Descriptions
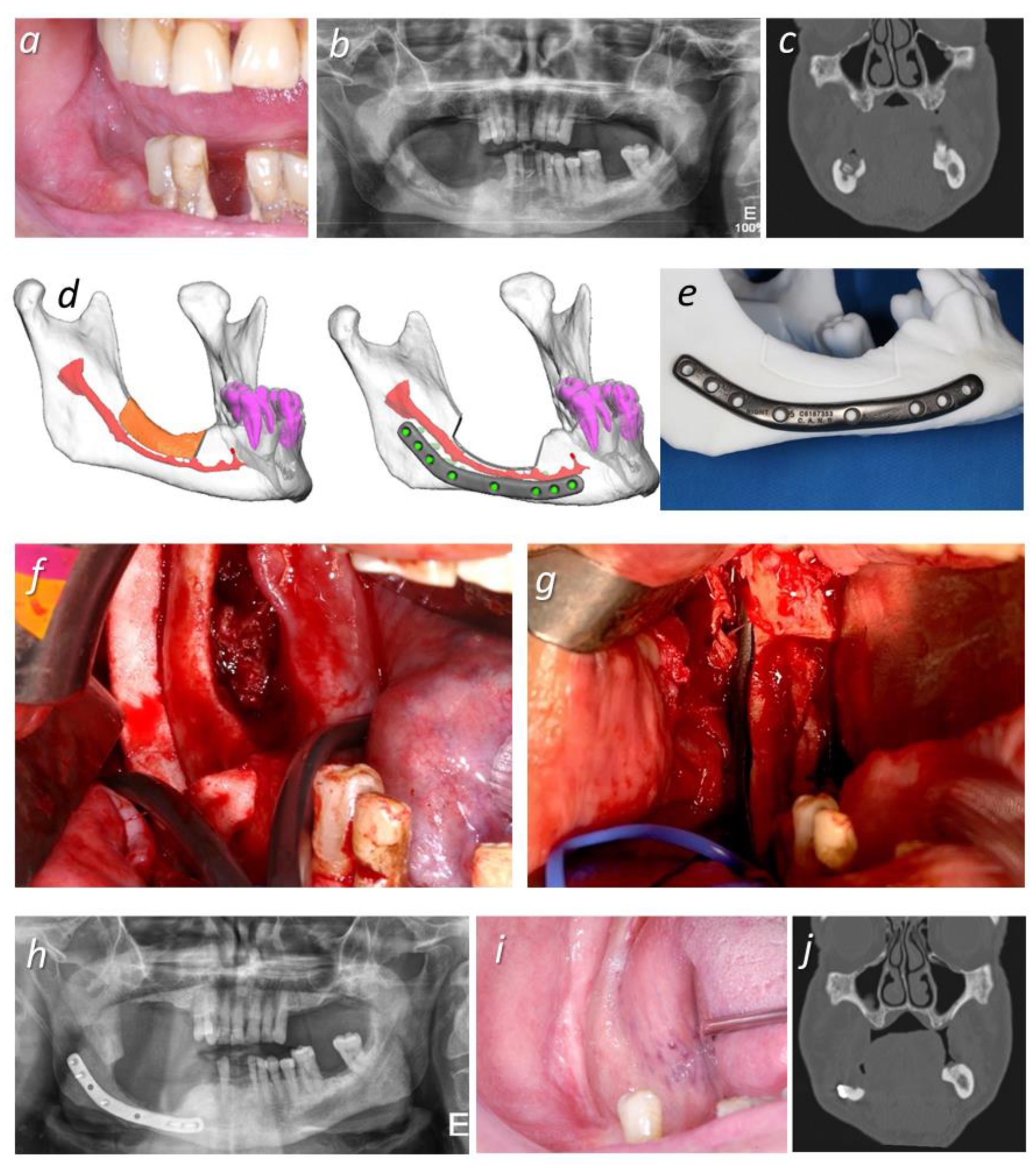
2.1. Case 1
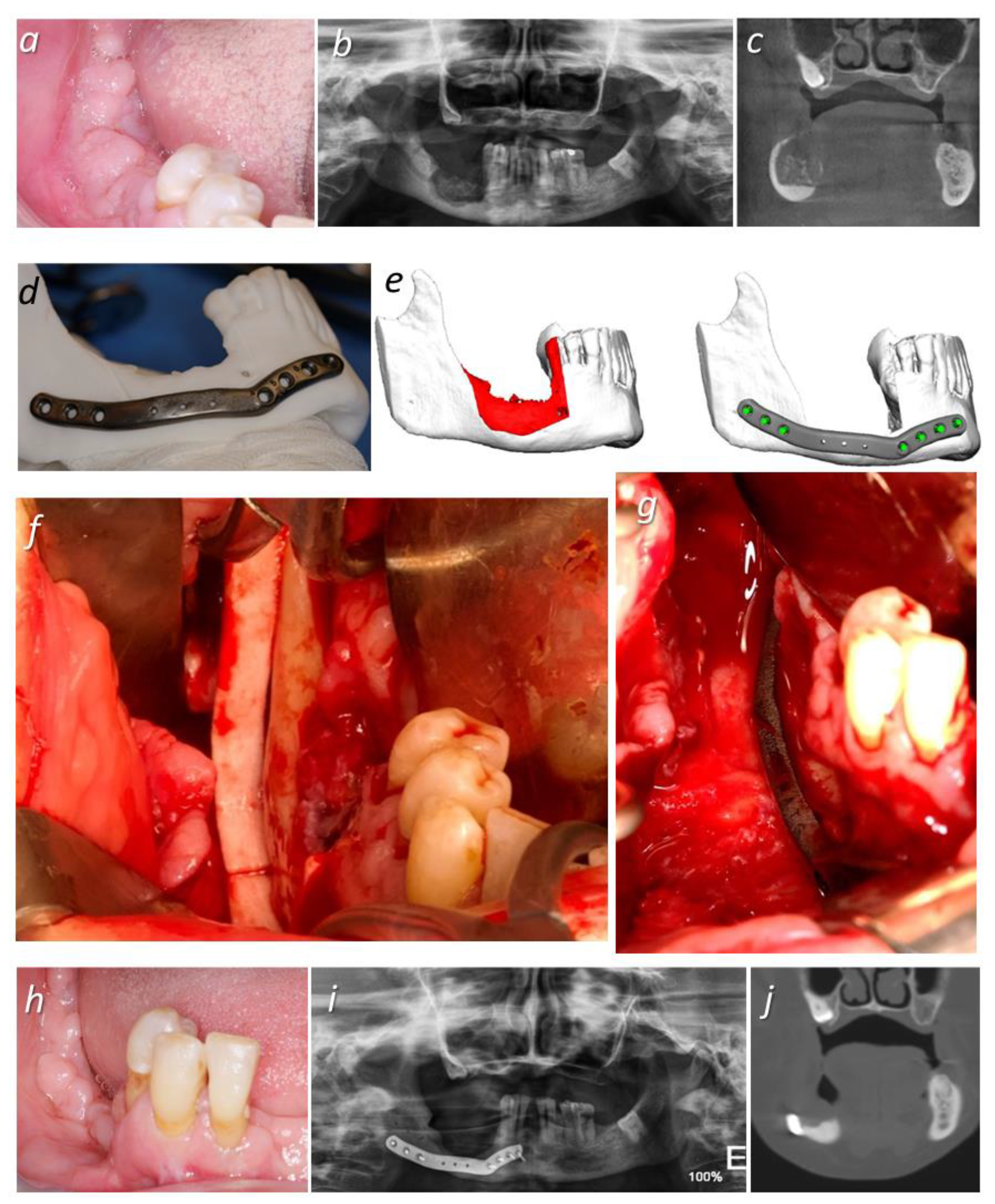
2.2. Case 2
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ruggiero, S.L.; Dodson, T.B.; Fantasia, J.; Goodday, R.; Aghaloo, T.; Mehrotra, B.; O’Ryan, F. American association of oral and maxillofacial surgeons position paper on medication-related osteonecrosis of the jaw—2014 update. J. Oral Maxillofac. Surg. 2014, 72, 1938–1956. [Google Scholar] [CrossRef]
- Akkawi, I.; Zmerly, H. Osteoporosis: Current Concepts. Joints 2018, 6, 122–127. [Google Scholar] [CrossRef] [PubMed]
- Otto, S.; Aljohani, S.; Fliefel, R.; Ecke, S.; Ristow, O.; Burian, E.; Troeltzsch, M.; Pautke, C.; Ehrenfeld, M. Infection as an Important Factor in Medication-Related Osteonecrosis of the Jaw (MRONJ). Medicina 2021, 57, 463. [Google Scholar] [CrossRef] [PubMed]
- Di Vito, A.; Chiarella, E.; Baudi, F.; Scardamaglia, P.; Antonelli, A.; Giudice, D.; Barni, T.; Fortunato, L.; Giudice, A. Dose-Dependent Effects of Zoledronic Acid on Human Periodontal Ligament Stem Cells: An In Vitro Pilot Study. Cell Transplant. 2020, 29, 963689720948497. [Google Scholar] [CrossRef] [PubMed]
- Schiodt, M.; Otto, S.; Fedele, S.; Bedogni, A.; Nicolatou-Galitis, O.; Guggenberger, R.; Herlofson, B.B.; Ristow, O.; Kofod, T. Workshop of European task force on medication-related osteonecrosis of the jaw-Current challenges. Oral Dis. 2019, 25, 1815–1821. [Google Scholar] [CrossRef]
- Chang, J.; Hakam, A.E.; McCauley, L.K. Current Understanding of the Pathophysiology of Osteonecrosis of the Jaw. Curr. Osteoporos Rep. 2018, 16, 584–595. [Google Scholar] [CrossRef] [PubMed]
- Aljohani, S.; Troeltzsch, M.; Hafner, S.; Kaeppler, G.; Mast, G.; Otto, S. Surgical treatment of medication-related osteonecrosis of the upper jaw: Case series. Oral Dis. 2019, 25, 497–597. [Google Scholar] [CrossRef]
- Otto, S.; Pautke, C.; Van den Wyngaert, T.; Niepel, D.; Schiødt, M. Medication-related osteonecrosis of the jaw: Prevention, diagnosis and management in patients with cancer and bone metastases. Cancer Treat. Rev. 2018, 69, 177–187. [Google Scholar] [CrossRef] [PubMed]
- Ristow, O.; Rückschloß, T.; Müller, M.; Berger, M.; Kargus, S.; Pautke, C.; Engel, M.; Hoffmann, J.; Freudlsperger, C. Is the conservative non-surgical management of medication-related osteonecrosis of the jaw an appropriate treatment option for early stages? A long-term single-center cohort study. J. Cranio-Maxillofac. Surg. 2019, 47, 491–499. [Google Scholar] [CrossRef] [PubMed]
- Hauer, L.; Jambura, J.; Hrusak, D.; Chalupova, M.; Posta, P.; Rusnak, S.; Vyskocil, V. Surgical therapy for medication-related osteonecrosis of the jaw in osteoporotic patients treated with antiresorptive agents. Biomed. Pap. Med. Fac. Univ. Palacky Olomouc. Czech Repub. 2020, 164, 100–107. [Google Scholar] [CrossRef] [PubMed]
- Yamada, S.H.; Kurita, H.; Kondo, E.M. Treatment outcomes and prognostic factors of medication-related osteonecrosis of the jaw: A case- and literature-based review. Clin. Oral Investig. 2019, 23, 3203–3211. [Google Scholar] [CrossRef]
- Giudice, A.; Barone, S.; Diodati, F.; Antonelli, A.; Nocini, R.; Cristofaro, M.G. Can Surgical Management Improve Resolution of Medication-Related Osteonecrosis of the Jaw at Early Stages? A Prospective Cohort Study. J. Oral Maxillofac. Surg. 2020, 78, 1986–1999. [Google Scholar] [CrossRef] [PubMed]
- Pedrazzoli, M.; Autelitano, L.; Biglioli, F. Prevention of bisphosphonate-related mandibular fractures. Acta Otorhinolaryngol. Ital. 2016, 36, 317–320. [Google Scholar] [CrossRef] [PubMed]
- Werning, J.W.; Downey, N.M.; Brinker, R.A.; Khuder, S.A.; Davis, W.J.; Rubin, A.M.; Elsamaloty, H.M. The Impact of Osteoporosis on Patients with Maxillofacial Trauma. Arch. Otolaryngol. Head Neck Surg. 2004, 130, 353–356. [Google Scholar] [CrossRef][Green Version]
- Probst, F.A.; Metzger, M.; Ehrenfeld, M.; Cornelius, C.P. Computer-Assisted Designed and Manufactured Procedures Facilitate the Lingual Application of Mandible Reconstruction Plates. J. Oral Maxillofac. Surg. 2016, 74, 1879–1895. [Google Scholar] [CrossRef]
- Kraeima, J.; Glas, H.H.; Witjes, M.J.H.; Schepman, K.P. Patient-specific pre-contouring of osteosynthesis plates for mandibular reconstruction: Using a three-dimensional key printed solution. J. Cranio-Maxillofac. Surg. 2018, 46, 1037–1040. [Google Scholar] [CrossRef] [PubMed]
- Dahake, S.; Kuthe, A.; Kulkarni, S.; Mawale, M. Finite element analysis of customized implant in mandibular reconstruction after tumor resection with and without using customized surgical osteotomy guide. Int. J. Med. Robot Comput. Assist. Surg. 2018, 14, e1854. [Google Scholar] [CrossRef]
- Rendenbach, C.; Sellenschloh, K.; Gerbig, L.; Morlock, M.M.; Beck-Broichsitter, B.; Smeets, R.; Heiland, M.; Huber, G.; Hanken, H. CAD–CAM plates versus conventional fixation plates for primary mandibular reconstruction: A biomechanical in vitro analysis. J. Cranio-Maxillofac. Surg. 2017, 45, 1878–1883. [Google Scholar] [CrossRef]
- Gagnier, J.J.; Kienle, G.; Altman, D.G.; Moher, D.; Sox, H.; Riley, D.; CARE Group. The CARE guidelines: Consensus-based clinical case report guideline development. J. Clin. Epidemiol. 2014, 67, 46–51. [Google Scholar] [CrossRef]
- Campisi, G.; Mauceri, R.; Bertoldo, F.; Bettini, G.; Biasotto, M.; Colella, G.; Consolo, U.; Di Fede, O.; Favia, G.; Fusco, V.; et al. Medication-Related Osteonecrosis of Jaws (MRONJ) Prevention and Diagnosis: Italian Consensus Update 2020. Int. J. Environ. Res. Public Health 2020, 17, 5998. [Google Scholar] [CrossRef] [PubMed]
- Otto, S.; Ristow, O.; Pache, C.; Troeltzsch, M.; Fliefel, R.; Ehrenfeld, M.; Pautke, C. Fluorescence-guided surgery for the treatment of medication-related osteonecrosis of the jaw: A prospective cohort study. J. Cranio-Maxillofac. Surg. 2016, 44, 1073–1080. [Google Scholar] [CrossRef] [PubMed]
- Carlson, E.R.; Basile, J.D. The Role of Surgical Resection in the Management of Bisphosphonate-Related Osteonecrosis of the Jaws. J. Oral Maxillofac. Surg. 2009, 67, S85–S95. [Google Scholar] [CrossRef]
- Khosla, S.; Burr, D.; Cauley, J.; Dempster, D.W.; Ebeling, P.R.; Felsenberg, D.; Gagel, R.F.; Gilsanz, V.; Guise, T.; Koka, S.; et al. Bisphosphonate-associated osteonecrosis of the jaw: Report of a Task Force of the American Society for Bone and Mineral Research. J. Bone Miner Res. 2007, 22, 1479–1491. [Google Scholar] [CrossRef]
- Giudice, A.; Bennardo, F.; Barone, S.; Antonelli, A.; Figliuzzi, M.M.; Fortunato, L. Can Autofluorescence Guide Surgeons in the Treatment of Medication-Related Osteonecrosis of the Jaw? A Prospective Feasibility Study. J. Oral Maxillofac. Surg. 2018, 76, 982–995. [Google Scholar] [CrossRef] [PubMed]
- Brucoli, M.; Boffano, P.; Romeo, I.; Corio, C.; Benech, A.; Ruslin, M.; Forouzanfar, T.; Rodríguez-Santamarta, T.; de Vicente, J.C.; Tarle, M.; et al. The epidemiology of edentulous atrophic mandibular fractures in Europe. J. Cranio-Maxillofac. Surg. 2019, 47, 1929–1934. [Google Scholar] [CrossRef]
- Turrentine, F.E.; Wang, H.; Simpson, V.B.; Jones, R.S. Surgical Risk Factors, Morbidity, and Mortality in Elderly Patients. J. Am. Coll. Surg. 2006, 203, 865–877. [Google Scholar] [CrossRef] [PubMed]
- Martola, M.; Lindqvist, C.; Hänninen, H.; Al-Sukhun, J. Fracture of titanium plates used for mandibular reconstruction following ablative tumor surgery. J. Biomed. Mater. Res. Part B Appl. Biomater. 2007, 80, 345–352. [Google Scholar] [CrossRef] [PubMed]
- Martins, A.S.; Correia, J.A.; Salvado, F.; Caldas, C.; Santos, N.; Capelo, A.; Palmela, P. Relevant factors for treatment outcome and time to healing in medication-related osteonecrosi of the jaws—A retrospective cohort study. J. Cranio-Maxillofac. Surg. 2017, 45, 1736–1742. [Google Scholar] [CrossRef] [PubMed]
- Hinson, A.M.; Siegel, E.R.; Stack, B.C. Temporal correlation between bisphosphonate termination and symptom resolution in osteonecrosis of the jaw: A pooled case report analysis. J. Oral Maxillofac. Surg. 2015, 73, 53–62. [Google Scholar] [CrossRef]
- Otto, S.; Pautke, C.; Arens, D.; Poxleitner, P.; Eberli, U.; Nehrbass, D.; Zeiter, S.; Stoddart, M.J. A Drug Holiday Reduces the Frequency and Severity of Medication-Related Osteonecrosis of the Jaw in a Minipig Model. J. Bone Miner Res. 2020, 35, 2179–2192. [Google Scholar] [CrossRef]
- Kobayashi, Y.; Hiraga, T.; Ueda, A.; Wang, L.; Matsumoto-Nakano, M.; Hata, K.; Yatani, H.; Yoneda, T. Zoledronic acid delays wound healing of the tooth extraction socket, inhibits oral epithelial cell migration, and promotes proliferation and adhesion to hydroxyapatite of oral bacteria, without causing osteonecrosis of the jaw, in mice. J. Bone Miner Metab. 2010, 28, 165–175. [Google Scholar] [CrossRef]
- Milstein, D.M.J.; Lindeboom, J.A.H.; Ince, C. The influence of zoledronic acid and cyclophosphamide on microcirculation regeneration in healing oral mucosal flaps. Arch. Oral. Biol. 2011, 56, 599–606. [Google Scholar] [CrossRef] [PubMed]
- Fortunato, L.; Bennardo, F.; Buffone, C.; Guidice, A. Is the application of platelet concentrates effective in the prevention and treatment of medication-related osteonecrosis of the jaw? A systematic review. J. Craniomaxillofac. Surg. 2020, 48, 268–285. [Google Scholar] [CrossRef] [PubMed]
- Tripathi, A.; Pandey, S.; Singh, S.; Kumar Sharma, N.; Singh, R. Bisphosphonate therapy for skeletal malignancies and metastases: Impact on jaw bones and prosthodontic concerns. J. Prosthodont. 2011, 20, 601–603. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Correia, J.A.; Ferreira, J.R.; Amaral Nunes, M.; Capelo, A.; de Araújo Nobre, M.; Salvado, F. Prevention of Mandible Fractures in Medication-Related Osteonecrosis of the Jaws: The Role of Virtual Surgical Planning and Computer-Aided Design and Manufacturing in Two Clinical Case Reports. Appl. Sci. 2021, 11, 7894. https://doi.org/10.3390/app11177894
Correia JA, Ferreira JR, Amaral Nunes M, Capelo A, de Araújo Nobre M, Salvado F. Prevention of Mandible Fractures in Medication-Related Osteonecrosis of the Jaws: The Role of Virtual Surgical Planning and Computer-Aided Design and Manufacturing in Two Clinical Case Reports. Applied Sciences. 2021; 11(17):7894. https://doi.org/10.3390/app11177894
Chicago/Turabian StyleCorreia, João André, José Ricardo Ferreira, Miguel Amaral Nunes, António Capelo, Miguel de Araújo Nobre, and Francisco Salvado. 2021. "Prevention of Mandible Fractures in Medication-Related Osteonecrosis of the Jaws: The Role of Virtual Surgical Planning and Computer-Aided Design and Manufacturing in Two Clinical Case Reports" Applied Sciences 11, no. 17: 7894. https://doi.org/10.3390/app11177894
APA StyleCorreia, J. A., Ferreira, J. R., Amaral Nunes, M., Capelo, A., de Araújo Nobre, M., & Salvado, F. (2021). Prevention of Mandible Fractures in Medication-Related Osteonecrosis of the Jaws: The Role of Virtual Surgical Planning and Computer-Aided Design and Manufacturing in Two Clinical Case Reports. Applied Sciences, 11(17), 7894. https://doi.org/10.3390/app11177894








