Development of an Automatic Ultrasound Image Classification System for Pressure Injury Based on Deep Learning
Abstract
:1. Introduction
2. Materials and Methods
2.1. Development of the Deep Learning-Based Classification System
2.1.1. U-Net
2.1.2. Training Datasets
2.1.3. Implementation
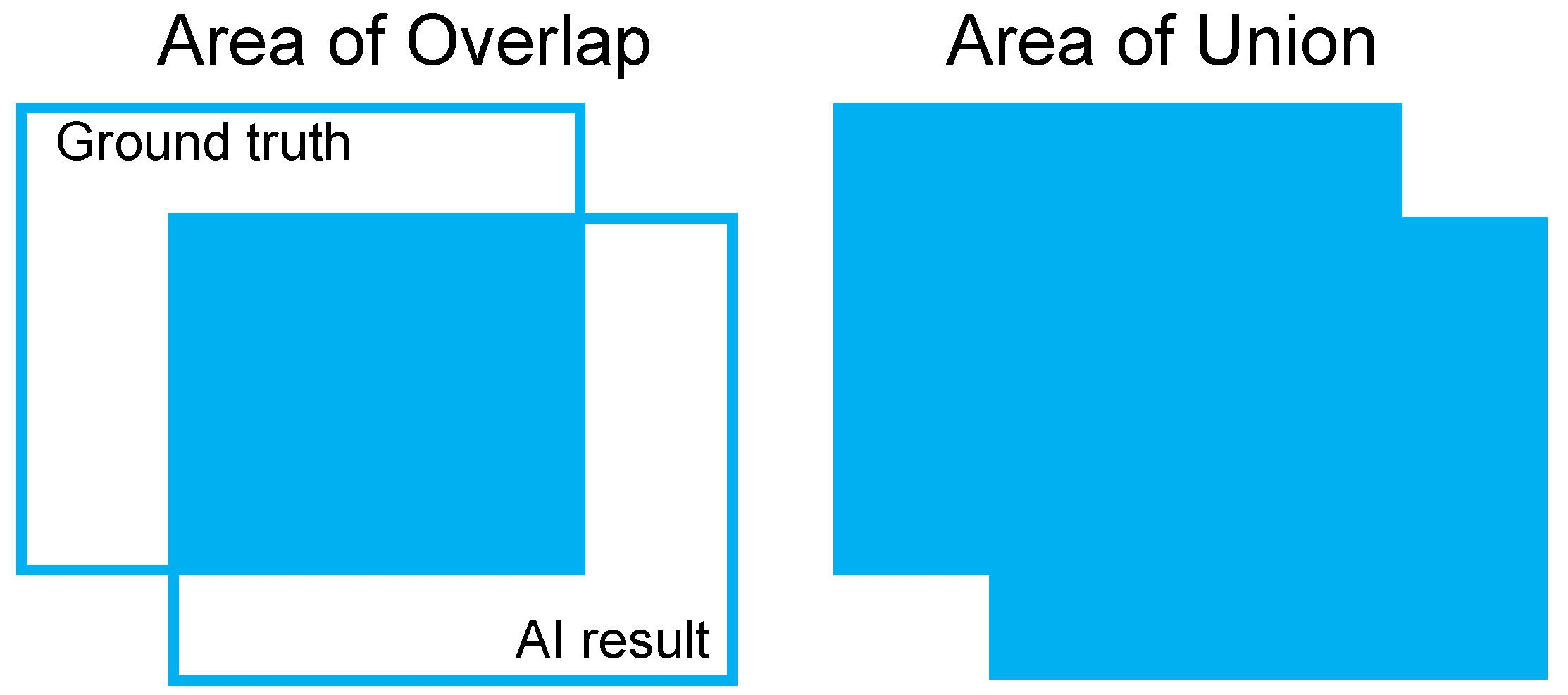
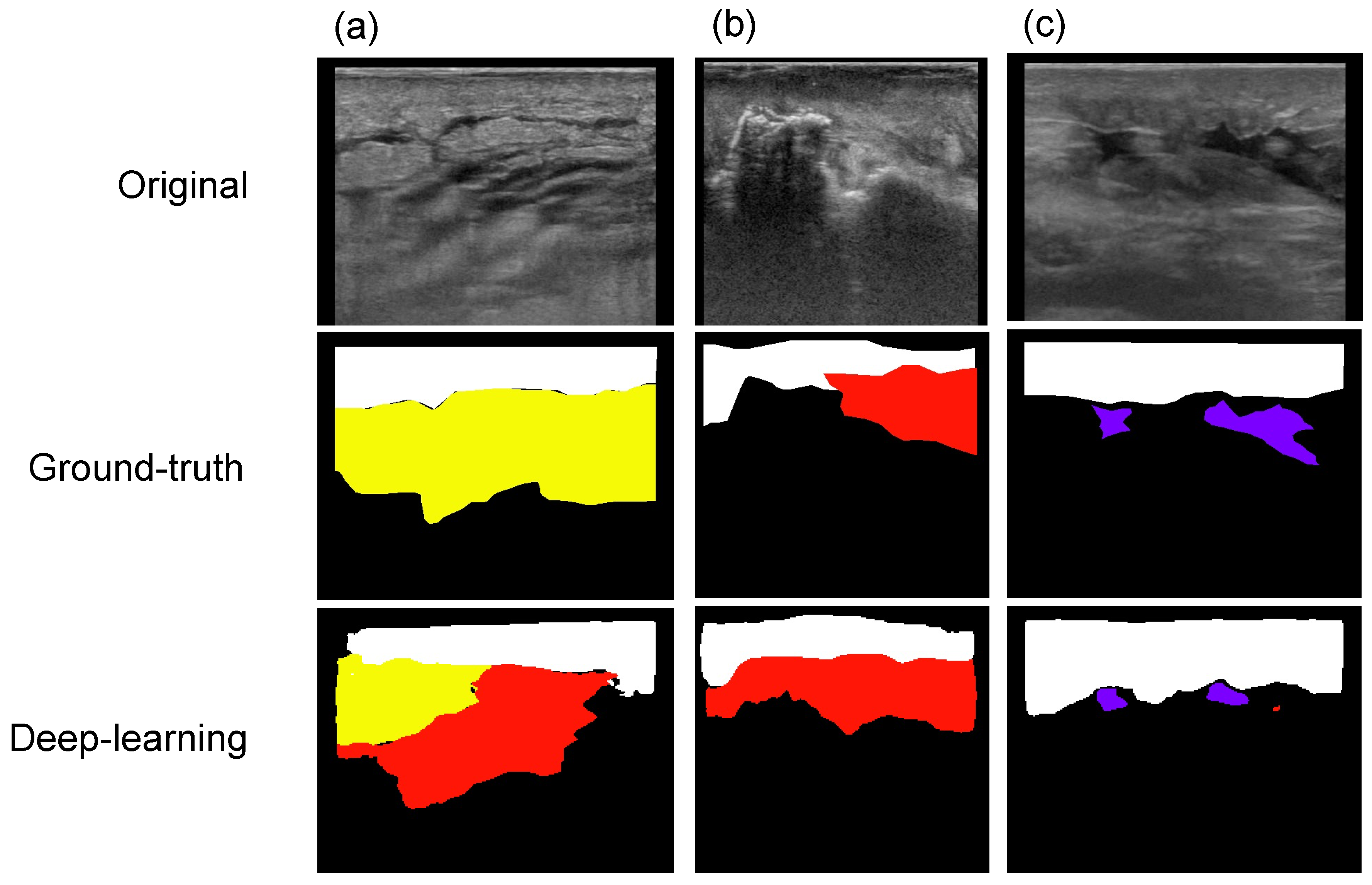
2.2. Evaluation of the Deep Learning-Based Classification System
2.2.1. Patients and Settings
2.2.2. US Technique
2.2.3. Application of the Deep Learning-Based Classification System
2.2.4. Data Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Franks, P.J.; Winterberg, H.; Moffatt, C.J. Health-related quality of life and pressure ulceration assessment in patients treated in the community. Wound Repair Regen. 2002, 10, 133–140. [Google Scholar] [CrossRef] [PubMed]
- Gorecki, C.; Brown, J.M.; Nelson, E.A.; Briggs, M.; Schoonhoven, L.; Dealey, C.; Defloor, T.; Nixon, J. Impact of pressure ulcers on quality of life in older patients: A systematic review. J. Am. Geriatr. Soc. 2009, 57, 1175–1183. [Google Scholar] [CrossRef] [PubMed]
- Jaul, E.; Calderon-Margalit, R. Systemic factors and mortality in elderly patients with pressure ulcers. Int. Wound J. 2015, 12, 254–259. [Google Scholar] [CrossRef] [PubMed]
- Leijon, S.; Bergh, I.; Terstappen, K. Pressure ulcer prevalence, use of preventive measures, and mortality risk in an acute care population: A quality improvement project. JWOCN 2013, 40, 469–474. [Google Scholar] [CrossRef] [PubMed]
- Chacon, J.M.F.; Blanes, L.; Borba, L.G.; Rocha, L.R.M.; Ferreira, L.M. Direct variable cost of the topical treatment of stages III and IV pressure injuries incurred in a public university hospital. J. Tissue Viability 2017, 26, 108–112. [Google Scholar] [CrossRef] [PubMed]
- Nakagami, G.; Sanada, H.; Iizaka, S.; Kadono, T.; Higashino, T.; Koyanagi, H.; Haga, N. Predicting delayed pressure ulcer healing using thermography: A prospective cohort study. J. Wound Care 2010, 19, 465–466, 468, 470. [Google Scholar] [CrossRef] [PubMed]
- Vetrano, D.L.; Landi, F.; De Buyser, S.L.; Carfì, A.; Zuccalà, G.; Petrovic, M.; Volpato, S.; Cherubini, A.; Corsonello, A.; Bernabei, R.; et al. Predictors of length of hospital stay among older adults admitted to acute care wards: A multicentre observational study. Eur. J. Intern. Med. 2014, 25, 56–62. [Google Scholar] [CrossRef] [PubMed]
- Brem, H.; Maggi, J.; Nierman, D.; Rolnitzky, L.; Bell, D.; Rennert, R.; Golinko, M.; Yan, A.; Lyder, C.; Vladeck, B. High cost of stage IV pressure ulcers. Am. J. Surg. 2010, 200, 473–477. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bouten, C.V.; Oomens, C.W.; Baaijens, F.P.; Bader, D.L. The etiology of pressure ulcers: Skin deep or muscle bound? Arch. Phys. Med. Rehabil. 2003, 84, 616–619. [Google Scholar] [CrossRef] [PubMed]
- Scafide, K.N.; Narayan, M.C.; Arundel, L. Bedside technologies to enhance the early detection of pressure injuries: A systematic review. JWOCN 2020, 47, 128–136. [Google Scholar] [CrossRef] [PubMed]
- Oliveira, A.L.; Moore, Z.; O’Connor, T.; Patton, D. Accuracy of ultrasound, thermography and subepidermal moisture in predicting pressure ulcers: A systematic review. J. Wound Care 2017, 26, 199–215. [Google Scholar] [CrossRef] [Green Version]
- Aoi, N.; Yoshimura, K.; Kadono, T.; Nakagami, G.; Iizaka, S.; Higashino, T.; Araki, J.; Koshima, I.; Sanada, H. Ultrasound assessment of deep tissue injury in pressure ulcers: Possible prediction of pressure ulcer progression. Plast. Reconstr. Surg. 2009, 124, 540–550. [Google Scholar] [CrossRef] [Green Version]
- Higashino, T.; Nakagami, G.; Kadono, T.; Ogawa, Y.; Iizaka, S.; Koyanagi, H.; Sasaki, S.; Haga, N.; Sanada, H. Combination of thermographic and ultrasonographic assessments for early detection of deep tissue injury. Int. Wound J. 2014, 11, 509–516. [Google Scholar] [CrossRef]
- Shimizu, Y.; Mutsuzaki, H.; Tachibana, K.; Tsunoda, K.; Hotta, K.; Fukaya, T.; Ikeda, E.; Yamazaki, M.; Wadano, Y. A survey of deep tissue injury in elite female wheelchair basketball players. J. Back Musculoskelet. Rehabil. 2017, 30, 427–434. [Google Scholar] [CrossRef]
- Swaine, J.M.; Breidahl, W.; Bader, D.L.; Oomens, C.W.J.; O’Loughlin, E.; Santamaria, N.; Stacey, M.C. Ultrasonography detects deep tissue injuries in the subcutaneous layers of the buttocks following spinal cord injury. Top. Spinal Cord Injury Rehabil. 2018, 24, 371–378. [Google Scholar] [CrossRef] [Green Version]
- Yabunaka, K.; Nakagami, G.; Miyagaki, T.; Sasaki, S.; Hayashi, C.; Sanada, H. Color Doppler ultrasonography to evaluate hypoechoic areas in pressure ulcers: A report of two cases. J. Med. Ultrasound 2018, 26, 163–165. [Google Scholar] [CrossRef] [PubMed]
- Matsumoto, M.; Nakagami, G.; Kitamura, A.; Kurita, M.; Suga, H.; Miyake, T.; Kawamoto, A.; Sanada, H. Ultrasound assessment of deep tissue on the wound bed and periwound skin: A classification system using ultrasound images. J. Tissue Viability 2021, 30, 28–35. [Google Scholar] [CrossRef]
- Ueta, M.; Sugama, J.; Konya, C.; Matsuo, J.; Matsumoto, M.; Yabunaka, K.; Nakatani, T.; Tabata, K. Use of ultrasound in assessment of necrotic tissue in pressure ulcers with adjacent undermining. J. Wound Care 2011, 20, 503–504, 506, 508, passim. [Google Scholar] [CrossRef] [PubMed]
- Zahia, S.; Garcia Zapirain, M.B.; Sevillano, X.; González, A.; Kim, P.J.; Elmaghraby, A. Pressure injury image analysis with machine learning techniques: A systematic review on previous and possible future methods. Artif. Intell. Med. 2020, 102, 101742. [Google Scholar] [CrossRef]
- Xu, Y.; Wang, Y.; Yuan, J.; Cheng, Q.; Wang, X.; Carson, P.L. Medical breast ultrasound image segmentation by machine learning. Ultrasonics 2019, 91, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Mielnik, P.; Fojcik, M.; Segen, J.; Kulbacki, M. A novel method of synovitis stratification in ultrasound using machine learning algorithms: Results from clinical validation of the MEDUSA project. Ultrasound Med. Biol. 2018, 44, 489–494. [Google Scholar] [CrossRef]
- Kise, Y.; Shimizu, M.; Ikeda, H.; Fujii, T.; Kuwada, C.; Nishiyama, M.; Funakoshi, T.; Ariji, Y.; Fujita, H.; Katsumata, A.; et al. Usefulness of a deep learning system for diagnosing Sjögren’s syndrome using ultrasonography images. Dentomaxillofac. Radiol. 2020, 49, 20190348. [Google Scholar] [CrossRef]
- Burlina, P.; Billings, S.; Joshi, N.; Albayda, J. Automated diagnosis of myositis from muscle ultrasound: Exploring the use of machine learning and deep learning methods. PLoS ONE 2017, 12, e0184059. [Google Scholar] [CrossRef]
- Antico, M.; Sasazawa, F.; Dunnhofer, M.; Camps, S.M.; Jaiprakash, A.T.; Pandey, A.K.; Crawford, R.; Carneiro, G.; Fontanarosa, D. Deep learning-based femoral cartilage automatic segmentation in ultrasound imaging for guidance in robotic knee arthroscopy. Ultrasound Med. Biol. 2020, 46, 422–435. [Google Scholar] [CrossRef]
- Russakovsky, O.; Deng, J.; Su, H.; Krause, J.; Satheesh, S.; Ma, S.; Huang, Z.; Karpathy, A.; Khosla, A.; Bernstein, M.; et al. ImageNet large scale visual recognition challenge. Int. J. Comput. Vis. 2015, 115, 211–252. [Google Scholar] [CrossRef] [Green Version]
- Ronneberger, O.; Fischer, P.; Brox, T. U-Net: Convolutional networks for biomedical image segmentation. In Proceedings of the Medical Image Computing and Computer-Assisted Intervention—MICCAI 2015, Munich, Germany, 5–9 October 2015; pp. 234–241. [Google Scholar]
- Xie, S.; Girshick, R.; Dollár, P.; Tu, Z.; He, K. Aggregated residual transformations for deep neural networks. In Proceedings of the 2017 IEEE Conference on Computer Vision and Pattern Recognition (CVPR), Honolulu, HI, USA, 21–26 July 2017; pp. 5987–5995. [Google Scholar]
- Lee, S.; Rahul; Ye, H.; Chittajallu, D.; Kruger, U.; Boyko, T.; Lukan, J.K.; Enquobahrie, A.; Norfleet, J.; De, S. Real-time burn classification using ultrasound imaging. Sci. Rep. 2020, 10, 5829. [Google Scholar] [CrossRef] [Green Version]
- Huang, C.; Zhou, Y.; Tan, W.; Qiu, Z.; Zhou, H.; Song, Y.; Zhao, Y.; Gao, S. Applying deep learning in recognizing the femoral nerve block region on ultrasound images. Ann. Transl. Med. 2019, 7, 453. [Google Scholar] [CrossRef]
- Vukicevic, A.M.; Radovic, M.; Zabotti, A.; Milic, V.; Hocevar, A.; Callegher, S.Z.; De Lucia, O.; De Vita, S.; Filipovic, N. Deep learning segmentation of Primary Sjögren’s syndrome affected salivary glands from ultrasonography images. Comput. Biol. Med. 2021, 129, 104154. [Google Scholar] [CrossRef]


| US Findings | Detection Performance | Mean Value of IoU | Mean Value of DICE Score | Number of Cases in Test Data | Number of Images in Test Data |
|---|---|---|---|---|---|
| Unclear layer structure | 100.0% | 0.80 | 0.89 | 2 | 37 |
| Cobblestone-like pattern | 85.7% | 0.56 | 0.71 | 1 | 7 |
| Cloud-like pattern | 71.4% | 0.38 | 0.51 | 1 | 14 |
| Anechoic pattern | 93.3% | 0.62 | 0.76 | 1 | 15 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Matsumoto, M.; Karube, M.; Nakagami, G.; Kitamura, A.; Tamai, N.; Miura, Y.; Kawamoto, A.; Kurita, M.; Miyake, T.; Hayashi, C.; et al. Development of an Automatic Ultrasound Image Classification System for Pressure Injury Based on Deep Learning. Appl. Sci. 2021, 11, 7817. https://doi.org/10.3390/app11177817
Matsumoto M, Karube M, Nakagami G, Kitamura A, Tamai N, Miura Y, Kawamoto A, Kurita M, Miyake T, Hayashi C, et al. Development of an Automatic Ultrasound Image Classification System for Pressure Injury Based on Deep Learning. Applied Sciences. 2021; 11(17):7817. https://doi.org/10.3390/app11177817
Chicago/Turabian StyleMatsumoto, Masaru, Mikihiko Karube, Gojiro Nakagami, Aya Kitamura, Nao Tamai, Yuka Miura, Atsuo Kawamoto, Masakazu Kurita, Tomomi Miyake, Chieko Hayashi, and et al. 2021. "Development of an Automatic Ultrasound Image Classification System for Pressure Injury Based on Deep Learning" Applied Sciences 11, no. 17: 7817. https://doi.org/10.3390/app11177817
APA StyleMatsumoto, M., Karube, M., Nakagami, G., Kitamura, A., Tamai, N., Miura, Y., Kawamoto, A., Kurita, M., Miyake, T., Hayashi, C., Kawasaki, A., & Sanada, H. (2021). Development of an Automatic Ultrasound Image Classification System for Pressure Injury Based on Deep Learning. Applied Sciences, 11(17), 7817. https://doi.org/10.3390/app11177817






