Gait Kinematics Analysis of Flatfoot Adults
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Assessment
2.3. Data Processing and Analysis
2.4. Statistical Analysis
3. Results
3.1. Sample and Groups Characteristics
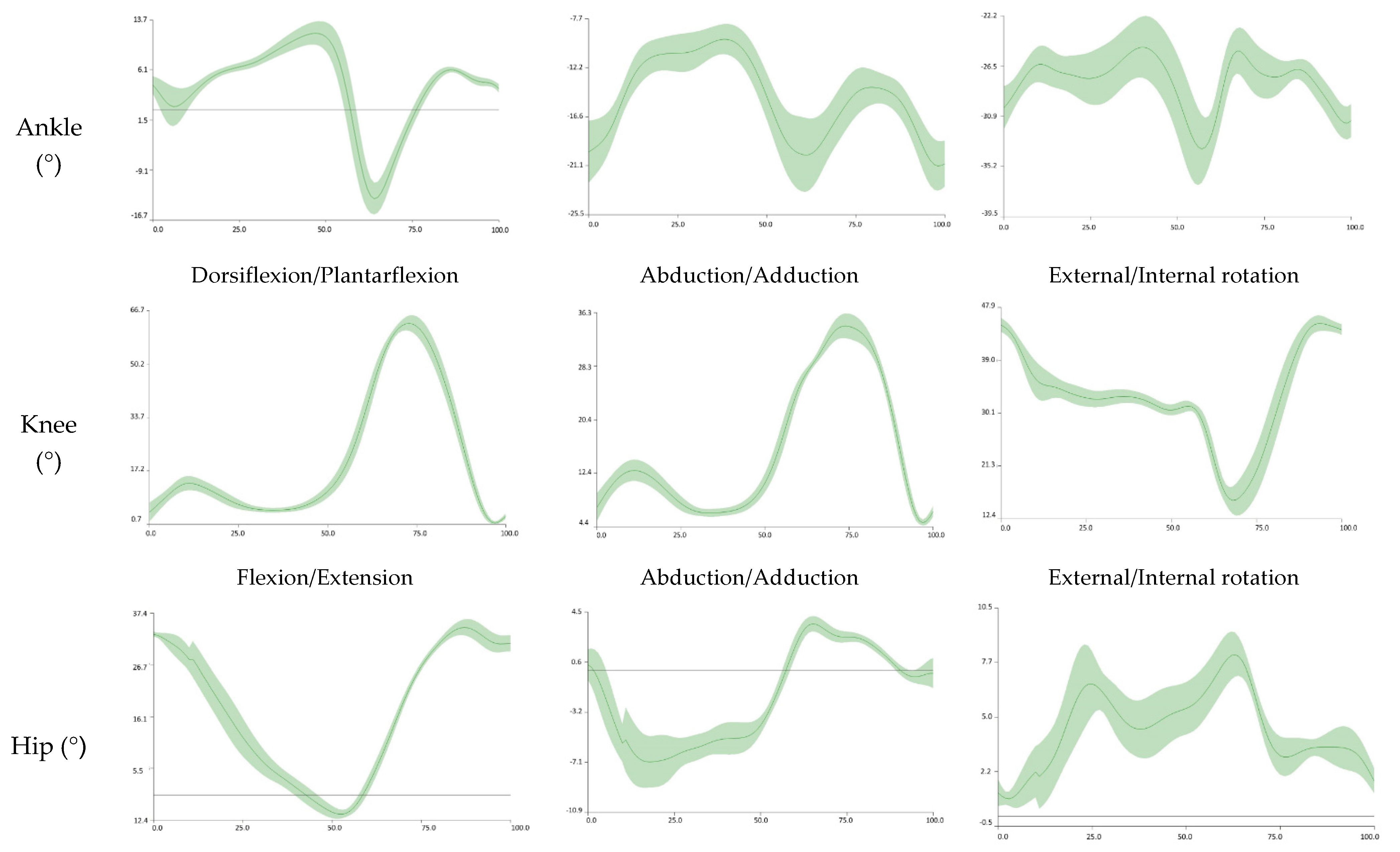
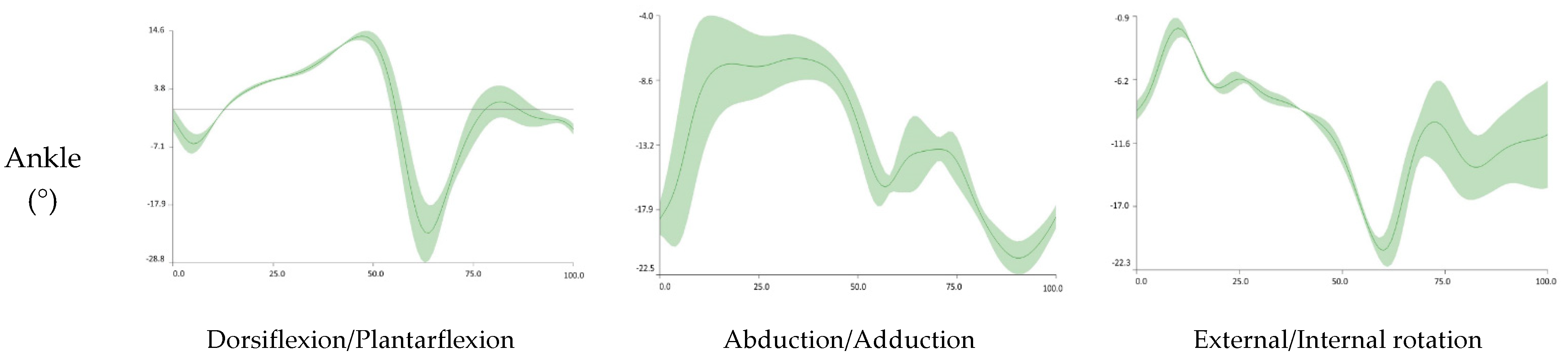
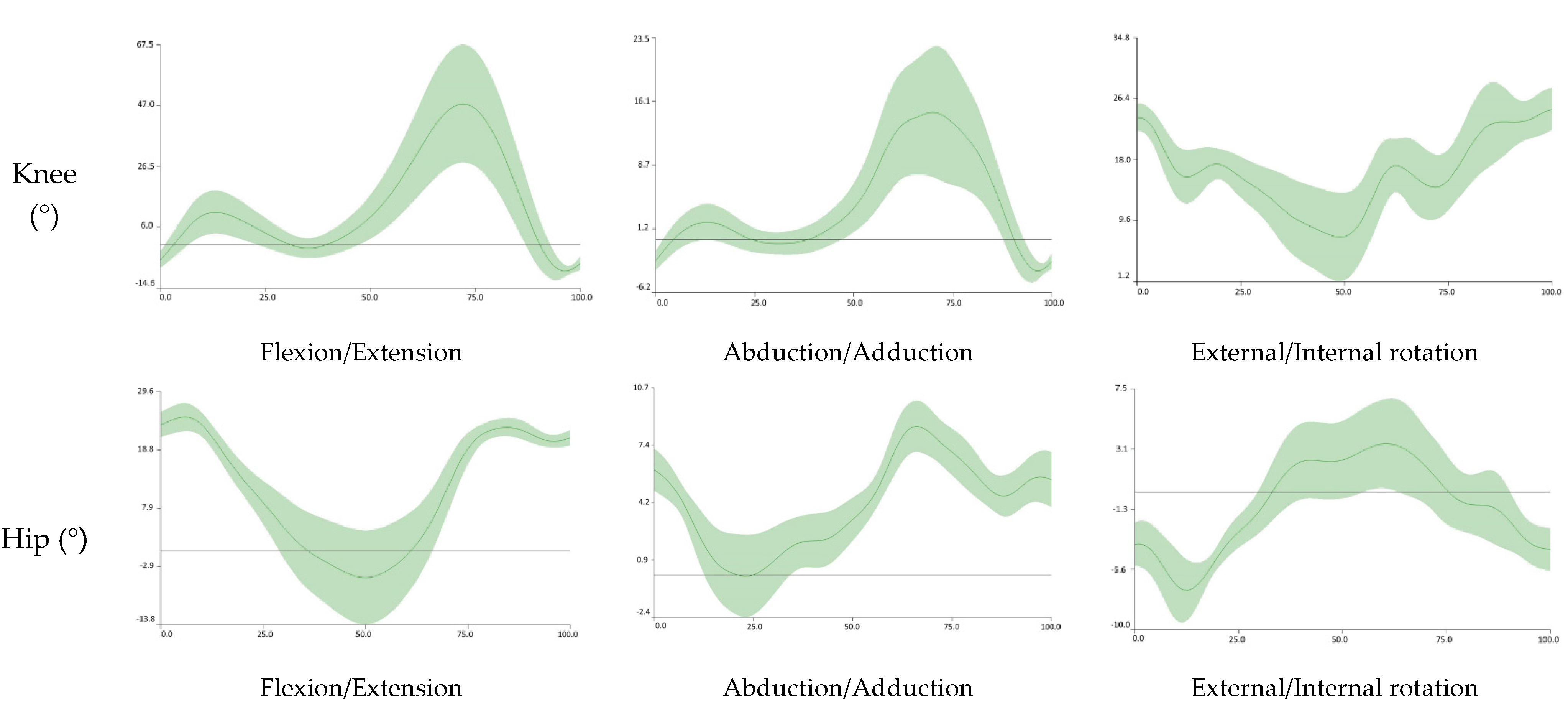
3.2. Kinematics Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kosashvili, Y.; Fridman, T.; Backstein, D.; Safir, O.; Ziv, Y.B. The Correlation between Pes Planus and Anterior Knee or Intermittent Low Back Pain. Foot Ankle Int. 2008, 29, 910–913. [Google Scholar] [CrossRef]
- Angin, S.; Crofts, G.; Mickle, K.J.; Nester, C.J. Ultrasound evaluation of foot muscles and plantar fascia in pes planus. Gait Posture 2014, 40, 48–52. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Caravaggi, P.; Sforza, C.; Leardini, A.; Portinaro, N.; Panou, A. Effect of plano-valgus foot posture on midfoot kinematics during barefoot walking in an adolescent population. J. Foot Ankle Res. 2018, 11, 55. [Google Scholar] [CrossRef] [PubMed]
- López-López, D.; Becerro-De-Bengoa-Vallejo, R.; Losa-Iglesias, M.E.; Palomo-López, P.; Rodríguez-Sanz, D.; Brandariz-Pereira, J.M.; Calvo-Lobo, C. Evaluation of foot health related quality of life in individuals with foot problems by gender: A cross-sectional comparative analysis study. BMJ Open 2018, 8, e023980. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Buldt, A.K.; Levinger, P.; Murley, G.S.; Menz, H.; Nester, C.J.; Landorf, K.B. Foot posture is associated with kinematics of the foot during gait: A comparison of normal, planus and cavus feet. Gait Posture 2015, 42, 42–48. [Google Scholar] [CrossRef]
- Buldt, A.K.; Murley, G.S.; Butterworth, P.; Levinger, P.; Menz, H.; Landorf, K.B. The relationship between foot posture and lower limb kinematics during walking: A systematic review. Gait Posture 2013, 38, 363–372. [Google Scholar] [CrossRef]
- Douglas Gross, K.; Felson, D.T.; Niu, J.; Hunter, D.J.; Guermazi, A.; Roemer, F.W.; Dufour, A.B.; Gensure, R.H.; Hannan, M.T. Association of flat feet with knee pain and cartilage damage in older adults. Arthritis Care Res. 2011, 63, 937–944. [Google Scholar] [CrossRef] [Green Version]
- Levinger, P.; Zeina, D.; Teshome, A.; Skinner, E.; Begg, R.; Abbott, J.H. A real time biofeedback using Kinect and Wii to improve gait for post-total knee replacement rehabilitation: A case study report. Disabil. Rehabil. Assist. Technol. 2016, 11, 251–262. [Google Scholar] [CrossRef]
- Powell, D.W.; Long, B.; Milner, C.; Zhang, S. Frontal plane multi-segment foot kinematics in high- and low-arched females during dynamic loading tasks. Hum. Mov. Sci. 2011, 30, 105–114. [Google Scholar] [CrossRef] [PubMed]
- Levinger, P.; Murley, G.S.; Barton, C.; Cotchett, M.P.; McSweeney, S.R.; Menz, H. A comparison of foot kinematics in people with normal- and flat-arched feet using the Oxford Foot Model. Gait Posture 2010, 32, 519–523. [Google Scholar] [CrossRef] [PubMed]
- Eslami, M.; Damavandi, M.; Ferber, R. Association of Navicular Drop and Selected Lower-Limb Biomechanical Measures during the Stance Phase of Running. J. Appl. Biomech. 2014, 30, 250–254. [Google Scholar] [CrossRef]
- Twomey, D.; McIntosh, A.; Simon, J.; Lowe, K.; Wolf, S. Kinematic differences between normal and low arched feet in children using the Heidelberg foot measurement method. Gait Posture 2010, 32, 1–5. [Google Scholar] [CrossRef]
- Hunt, A.E.; Smith, R.M. Mechanics and control of the flat versus normal foot during the stance phase of walking. Clin. Biomech. 2004, 19, 391–397. [Google Scholar] [CrossRef] [PubMed]
- Buldt, A.K.; Forghany, S.; Landorf, K.B.; Levinger, P.; Murley, G.S.; Menz, H.B. Foot posture is associated with plantar pressure during gait: A comparison of normal, planus and cavus feet. Gait Posture 2018, 62, 235–240. [Google Scholar] [CrossRef]
- Zuil-Escobar, J.C.; Martínez-Cepa, C.B.; Martín-Urrialde, J.A.; Gómez-Conesa, A. Evaluating the Medial Longitudinal Arch of the Foot: Correlations, Reliability, and Accuracy in People with a Low Arch. Phys. Ther. 2019, 99, 364–372. [Google Scholar] [CrossRef] [PubMed]
- Angin, S.; Mickle, K.J.; Nester, C.J. Contributions of foot muscles and plantar fascia morphology to foot posture. Gait Posture 2018, 61, 238–242. [Google Scholar] [CrossRef] [PubMed]
- Nagai, K.; Yamada, M.; Uemura, K.; Yamada, Y.; Ichihashi, N.; Tsuboyama, T. Differences in muscle coactivation during postural control between healthy older and young adults. Arch. Gerontol. Geriatr. 2011, 53, 338–343. [Google Scholar] [CrossRef] [Green Version]
- Varrecchia, T.; Rinaldi, M.; Serrao, M.; Draicchio, F.; Conte, C.; Conforto, S.; Schmid, M.; Ranavolo, A. Global lower limb muscle coactivation during walking at different speeds: Relationship between spatio-temporal, kinematic, kinetic, and energetic parameters. J. Electromyogr. Kinesiol. 2018, 43, 148–157. [Google Scholar] [CrossRef]
- Buldt, A.K.; Forghany, S.; Landorf, K.B.; Murley, G.S.; Levinger, P.; Menz, H.B. Centre of pressure characteristics in normal, planus and cavus feet. J. Foot Ankle Res. 2018, 11, 3. [Google Scholar] [CrossRef] [Green Version]
- Twomey, D.; McIntosh, A. The effects of low arched feet on lower limb gait kinematics in children. Foot 2012, 22, 60–65. [Google Scholar] [CrossRef] [PubMed]
- Kerr, C.; Zavatsky, A.; Theologis, T.; Stebbins, J. Kinematic differences between neutral and flat feet with and without symptoms as measured by the Oxford foot model. Gait Posture 2019, 67, 213–218. [Google Scholar] [CrossRef]
- Galli, M.; Cimolin, V.; Pau, M.; Costici, P.; Albertini, G. Relationship between flat foot condition and gait pattern alterations in children with Down syndrome. J. Intellect. Disabil. Res. 2014, 58, 269–276. [Google Scholar] [CrossRef] [PubMed]
- Shin, H.S.; Lee, J.H.; Kim, E.J.; Kyung, M.G.; Yoo, H.J.; Lee, D.Y. Flatfoot deformity affected the kinematics of the foot and ankle in proportion to the severity of deformity. Gait Posture 2019, 72, 123–128. [Google Scholar] [CrossRef] [PubMed]
- Yazdani, F.; Razeghi, M.; Ebrahimi, S. A comparison of the free moment pattern between normal and hyper-pronated aligned feet in female subjects during the stance phase of gait. J. Biomed. Phys. Eng. 2018, 10, 93–102. [Google Scholar] [CrossRef]
- Saraswat, P.; MacWilliams, B.; Davis, R.B.; D’Astous, J.L. Kinematics and kinetics of normal and planovalgus feet during walking. Gait Posture 2014, 39, 339–345. [Google Scholar] [CrossRef] [PubMed]
- Holt, G.R. Declaration of Helsinki—The World’s Document of Conscience and Responsibility. South Med. J. 2014, 107, 407. [Google Scholar] [CrossRef] [PubMed]
- Vandenbroucke, J.P.; von Elm, E.; Altman, D.G.; Gøtzsche, P.C.; Mulrow, C.D.; Pocock, S.J.; Poole, C.; Schlesselman, J.J.; Egger, M.; STROBE Initiative. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): Explanation and elaboration. Int. J. Surg. 2014, 12, 1500–1524. [Google Scholar] [CrossRef] [Green Version]
- Resende, R.A.; Deluzio, K.J.; Kirkwood, R.N.; Hassan, E.A.; Fonseca, S.T. Increased unilateral foot pronation affects lower limbs and pelvic biomechanics during walking. Gait Posture 2015, 41, 395–401. [Google Scholar] [CrossRef]
- Sung, P.S. The Sensitivity of Thresholds by Ground Reaction Force and Postural Stability in Subjects with and without Navicular Drop. J. Foot Ankle Surg. 2018, 57, 742–746. [Google Scholar] [CrossRef]
- Kim, J.A.; Lim, O.B.; Yi, C.H. Difference in static and dynamic stability between flexible flatfeet and neutral feet. Gait Posture 2015, 41, 546–550. [Google Scholar] [CrossRef]
- Tsai, L.-C.; Yu, B.; Mercer, V.S.; Gross, M.T. Comparison of Different Structural Foot Types for Measures of Standing Postural Control. J. Orthop. Sports Phys. Ther. 2006, 36, 942–953. [Google Scholar] [CrossRef] [Green Version]
- Wilken, J.M.; Rodriguez, K.M.; Brawner, M.; Darter, B.J. Reliability and minimal detectible change values for gait kinematics and kinetics in healthy adults. Gait Posture 2012, 35, 301–307. [Google Scholar] [CrossRef] [PubMed]
- Farokhmanesh, K.; Shirzadian, T.; Mahboubi, M.; Shahri, M.N. Effect of Foot Hyperpronation on Lumbar Lordosis and Thoracic Kyphosis in Standing Position Using 3-Dimensional Ultrasound-Based Motion Analysis System. Glob. J. Health Sci. 2014, 6, 254–260. [Google Scholar] [CrossRef] [Green Version]
- Tahmasebi, R.; Karimi, M.T.; Satvati, B.; Fatoye, F. Evaluation of Standing Stability in Individuals with Flatfeet. Foot Ankle Spéc. 2015, 8, 168–174. [Google Scholar] [CrossRef]
- López, D.; Pérez-Ríos, M.; Ruano-Ravina, A.; Losa-Iglesias, M.E.; Becerro-de-Bengoa-Vallejo, R.; Romero-Morales, C.; Calvo-Lobo, C.; Navarro-Flores, E. Impact of quality of life related to foot problems: A case–control study. Sci. Rep. 2021, 11, 14515. [Google Scholar] [CrossRef] [PubMed]
- Sung, P.S. The ground reaction force thresholds for detecting postural stability in participants with and without flat foot. J. Biomech. 2016, 49, 60–65. [Google Scholar] [CrossRef] [PubMed]
- Sung, P.S.; Zipple, J.T.; Andraka, J.M.; Danial, P.; Information, P.E.K.F.C.; Zipple, T.J. The kinetic and kinematic stability measures in healthy adult subjects with and without flat foot. Foot 2017, 30, 21–26. [Google Scholar] [CrossRef]
- López-López, D.; Vilar, J.M.; Barros-García, G.; Losa-Iglesias, M.E.; Palomo-López, P.; Becerro-De-Bengoa-Vallejo, R.; Calvo-Lobo, C. Foot Arch Height and Quality of Life in Adults: A Strobe Observational Study. Int. J. Environ. Res. Public Health 2018, 15, 1555. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ghasemi, M.S.; Koohpayehzadeh, J.; Kadkhodaei, H.; Ehsani, A.A. The effect of foot hyperpronation on spine alignment in standing position. Med. J. Islam. Repub. Iran 2016, 30, 466. [Google Scholar] [PubMed]
- Khamis, S.; Dar, G.; Peretz, C.; Yizhar, Z. The Relationship between Foot and Pelvic Alignment While Standing. J. Hum. Kinet. 2015, 46, 85–97. [Google Scholar] [CrossRef] [Green Version]
- Lee, H.-C.; Huang, C.-L.; Ho, S.-H.; Sung, W.-H. The Effect of a Virtual Reality Game Intervention on Balance for Patients with Stroke: A Randomized Controlled Trial. Games Health J. 2017, 6, 303–311. [Google Scholar] [CrossRef] [PubMed]
- Dietz, V. Spinal cord pattern generators for locomotion. Clin. Neurophysiol. 2003, 114, 1379–1389. [Google Scholar] [CrossRef]


| Total | NF | FF | p-Value | |
|---|---|---|---|---|
| n | 31 | 16 (37.5% Women) | 15 (46.6% Women) | |
| k | 62 | 32 | 30 | |
| NDT (mm) * | 5.06 ± 2.42 | 11.35 ± 1.43 | 0.000 | |
| RCSP (°) * | 1.44 ± 1.19 | 5.52 ± 2.22 | 0.000 | |
| Age (years) * | 23.26 ± 4.43 | 21.69 ± 2.98 | 24.93 ± 5.17 | 0.045 |
| Height (m) * | 1.70 ± 0.98 | 1.72 ± 0.09 | 1.68 ± 0.10 | 0.200 |
| Weight (kg) * | 75.14 ± 14.94 | 75.92 ± 17.03 | 74.32 ± 12.90 | 0.772 |
| Maximum and Minimum Value | Range of MOTION | ||||||
|---|---|---|---|---|---|---|---|
| FF | NF | p-Value | FF | NF | p-Value | ||
| Ankle (°) | Dorsiflexion | 12.49 ± 3.52 | 13.58 ± 6.94 | 0.029 | 27.87 ± 6.28 | 29.29 ± 8.47 | 0.163 |
| Plantarflexion | −15.67 ± 6.61 | −16.09 ± 8.36 | 0.541 | ||||
| Abduction | 0.38 ± 4.09 | 1.59 ± 9.95 | 0.033 | 16.81 ± 4.06 | 17.79 ± 10.51 | 0.003 | |
| Adduction | −16.61 ± 5.20 | −16.43 ± 6.43 | 0.398 | ||||
| External rotation | −3.35 ± 5.48 | −7.05 ± 8.08 | <0.001 | 15.85 ± 5.00 | 17.16 ± 7.89 | 0.105 | |
| Internal | −19.36 ± 5.42 | −19.63 ± 23.56 | <0.001 | ||||
| Knee (°) | Flexion | 60.60 ± 4.68 | 56.87 ± 12.41 | <0.001 | 65.64 ± 5.05 | 61.28 ± 8.93 | 0.000 |
| Extension | −5.04 ± 4.53 | −5.16 ± 10.71 | <0.001 | ||||
| Abduction | 18.04 ± 5.71 | 21.21 ± 9.60 | <0.001 | 18.84 ± 6.57 | 24.24 ± 11.20 | <0.001 | |
| Adduction | −0.81 ± 5.61 | −1.92 ± 8.34 | 0.236 | ||||
| External rotation | 29.19 ± 7.94 | 33.71 ± 15.30 | <0.001 | 23.77 ± 8.40 | 26.83 ± 5.69 | 0.079 | |
| Internal | 5.42 ± 10.37 | 0.15 ± 32.89 | 0.342 | ||||
| Hip (°) | Flexion | 30.67 ± 8.82 | 27.36 ± 10.90 | 0.002 | 40.88 ± 7.81 | 39.79 ± 7.54 | 0.002 |
| Extension | −10.21 ± 8.34 | −12.42 ± 10.36 | 0.006 | ||||
| Abduction | 18.18 ± 14.48 | 17.79 ± 13.60 | 0.552 | 14.80 ± 5.70 | 15.91 ± 7.05 | 0.156 | |
| Adduction | −9.27 ± 5.99 | −9.34 ± 6.31 | 0.883 | ||||
| External rotation | 7.48 ± 7.21 | 11.91 ± 12.71 | 0.012 | 15.80 ± 5.34 | 16.64 ± 10.26 | 0.007 | |
| Internal | −7.79 ± 7.08 | −2.61 ± 13.63 | <0.001 | ||||
| Pelvis (°) | Anterior Tilt | −4.13 ± 12.49 | −4.23 ± 10.90 | 0.905 | 7.83 ± 6.80 | 8.25 ± 6.72 | 0.744 |
| Posterior Tilt | 3.70 ± 10.93 | 4.02 ± 11.91 | 0.900 | ||||
| Lateral Tilt | 5.09 ± 3.63 | 4.71 ± 2.83 | 0.489 | 10.28 ± 4.44 | 9.81 ± 3.22 | 0.720 | |
| −5.18 ± 3.14 | −5.10 ± 3.15 | 0.909 | |||||
| Rotation | 10.66 ± 4.70 | 8.79 ± 6.33 | 0.017 | 20.98 ± 11.53 | 18.01 ± 7.81 | 0.009 | |
| −10.67 ± 8.20 | −9.22 ± 5.94 | 0.125 | |||||
| Center of Mass (height %) | Vertical Maximum | 55.07 ± 1.23 | 55.67 ± 0.85 | <0.001 | 2.38 ± 0.41 | 2.62 ± 0.39 | <0.001 |
| Vertical Minimum | 52.68 ± 1.40 | 53.04 ± 0.91 | 0.243 | ||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Marouvo, J.; Sousa, F.; Fernandes, O.; Castro, M.A.; Paszkiel, S. Gait Kinematics Analysis of Flatfoot Adults. Appl. Sci. 2021, 11, 7077. https://doi.org/10.3390/app11157077
Marouvo J, Sousa F, Fernandes O, Castro MA, Paszkiel S. Gait Kinematics Analysis of Flatfoot Adults. Applied Sciences. 2021; 11(15):7077. https://doi.org/10.3390/app11157077
Chicago/Turabian StyleMarouvo, Joel, Filipa Sousa, Orlando Fernandes, Maria António Castro, and Szczepan Paszkiel. 2021. "Gait Kinematics Analysis of Flatfoot Adults" Applied Sciences 11, no. 15: 7077. https://doi.org/10.3390/app11157077
APA StyleMarouvo, J., Sousa, F., Fernandes, O., Castro, M. A., & Paszkiel, S. (2021). Gait Kinematics Analysis of Flatfoot Adults. Applied Sciences, 11(15), 7077. https://doi.org/10.3390/app11157077








