Non-Contact Sensing Testbed for Post-Surgery Monitoring by Exploiting Artificial-Intelligence
Abstract
1. Introduction
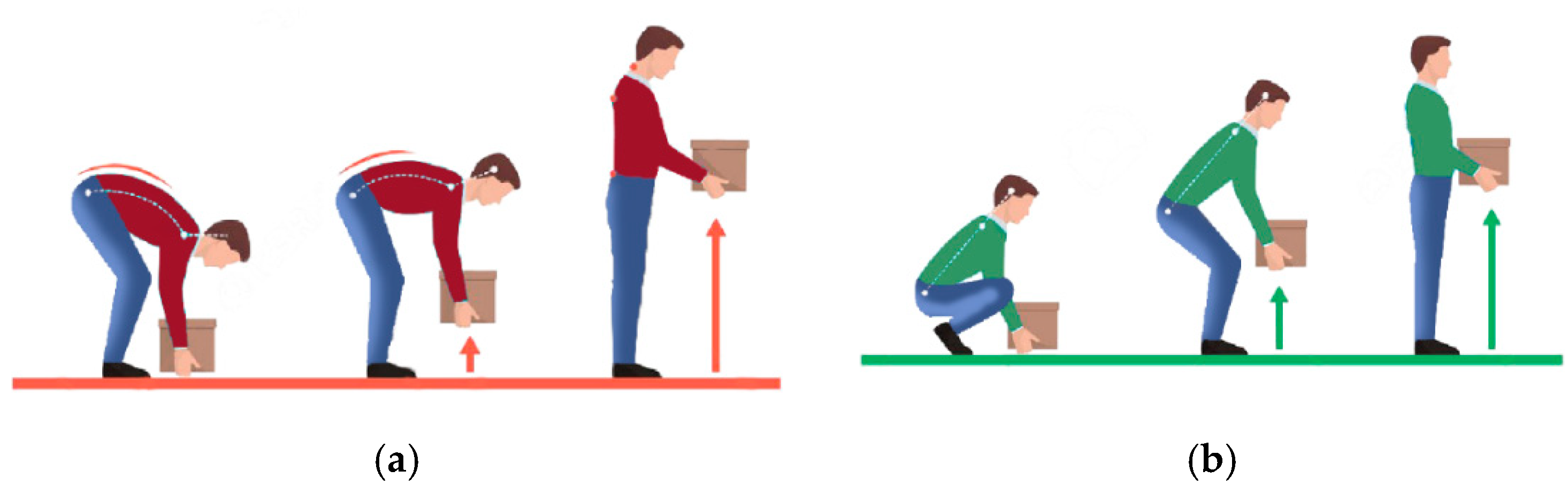
- We verify the feasibility of non-contact sensing using USRP by exploiting AI for post-surgery activities detection, especially weight lifting activity. To the great of our knowledge, this is the first work using universal software-defined radio peripheral (USRP) to extract WCSI for healthcare purposes and to monitor patients’ activities.
- We suggest a dynamic feature extraction technique of WCSI, which efficiently decreases the influence of environmental changes.
- We only depend on training data derived in ordinary situations. We collect data when a patient is normally lifting things and feed them into an algorithm to avoid collecting the data after when the patient had surgery, which is hard to collect in practical use.
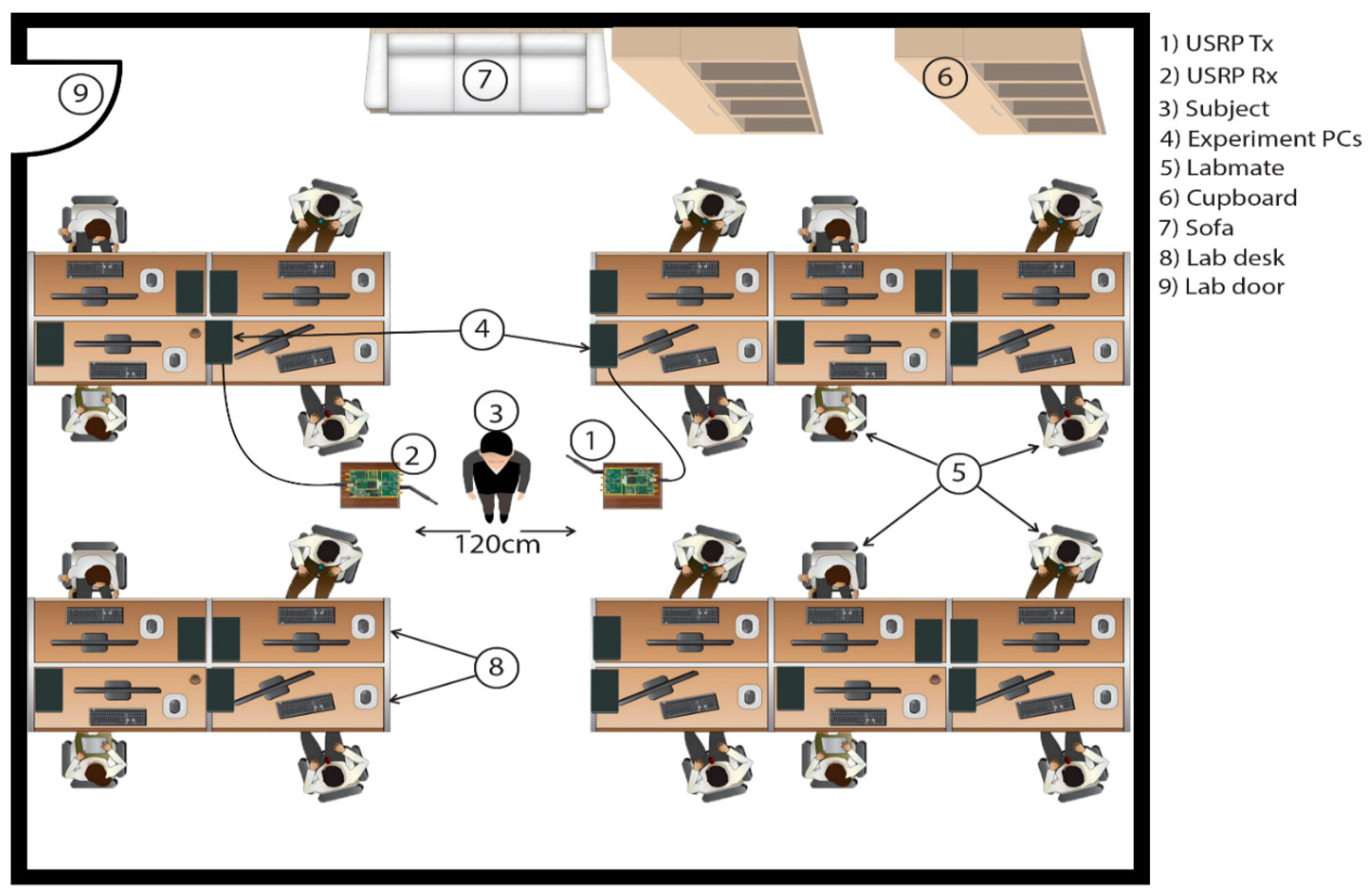
- We measured the execution of this technique in an actual environment, which we perform in our lab. The experimental outcomes show that the post-surgery activities monitoring testbed has high detection performance in a line of sight (LOS) as well as non-line-of sight (NLOS) scenario.
2. Related Work
2.1. Traditional Health Care Techniques
2.2. Using Wi-Fi Communication Signals for Sensing
3. Materials and Methods
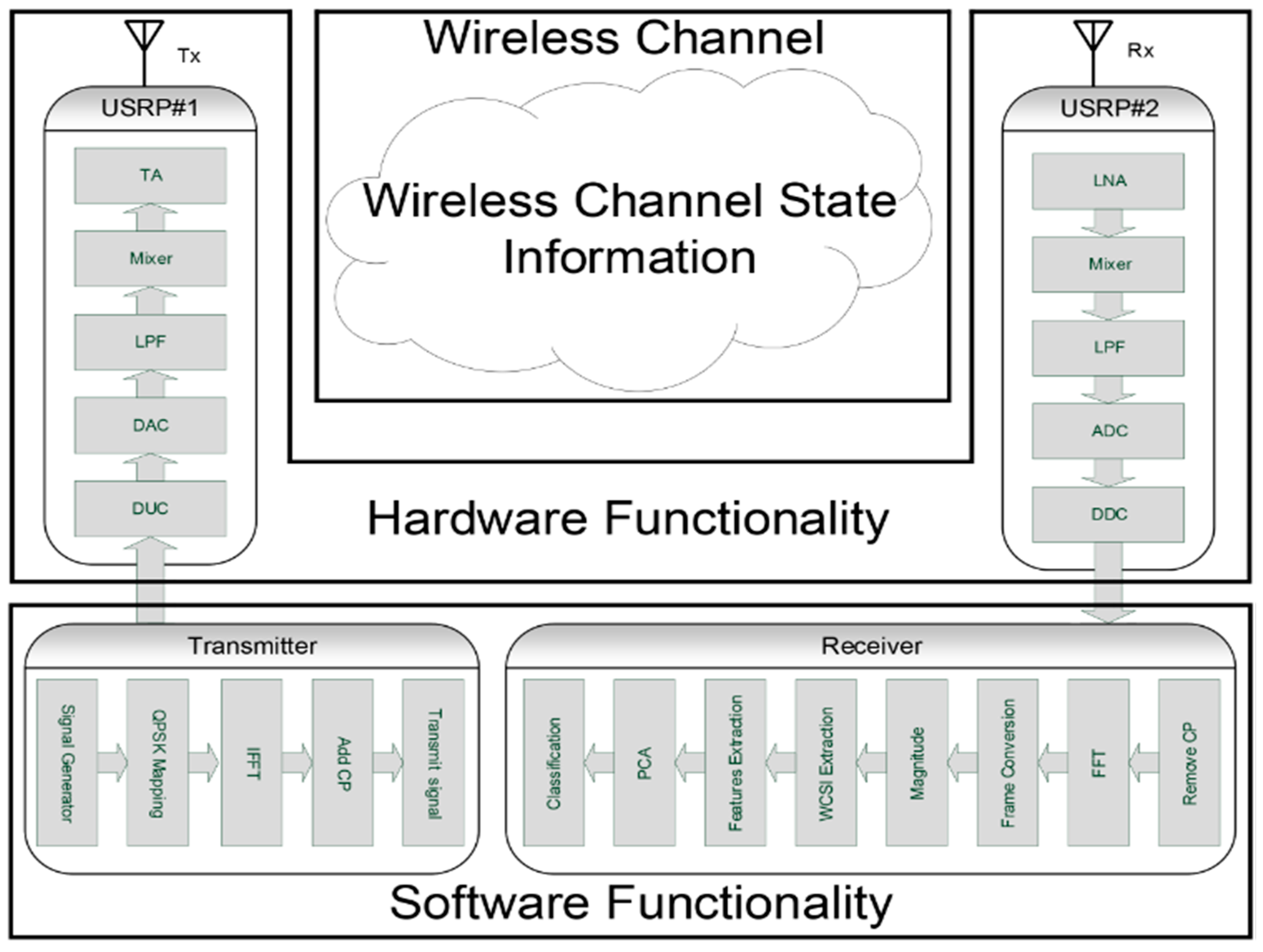
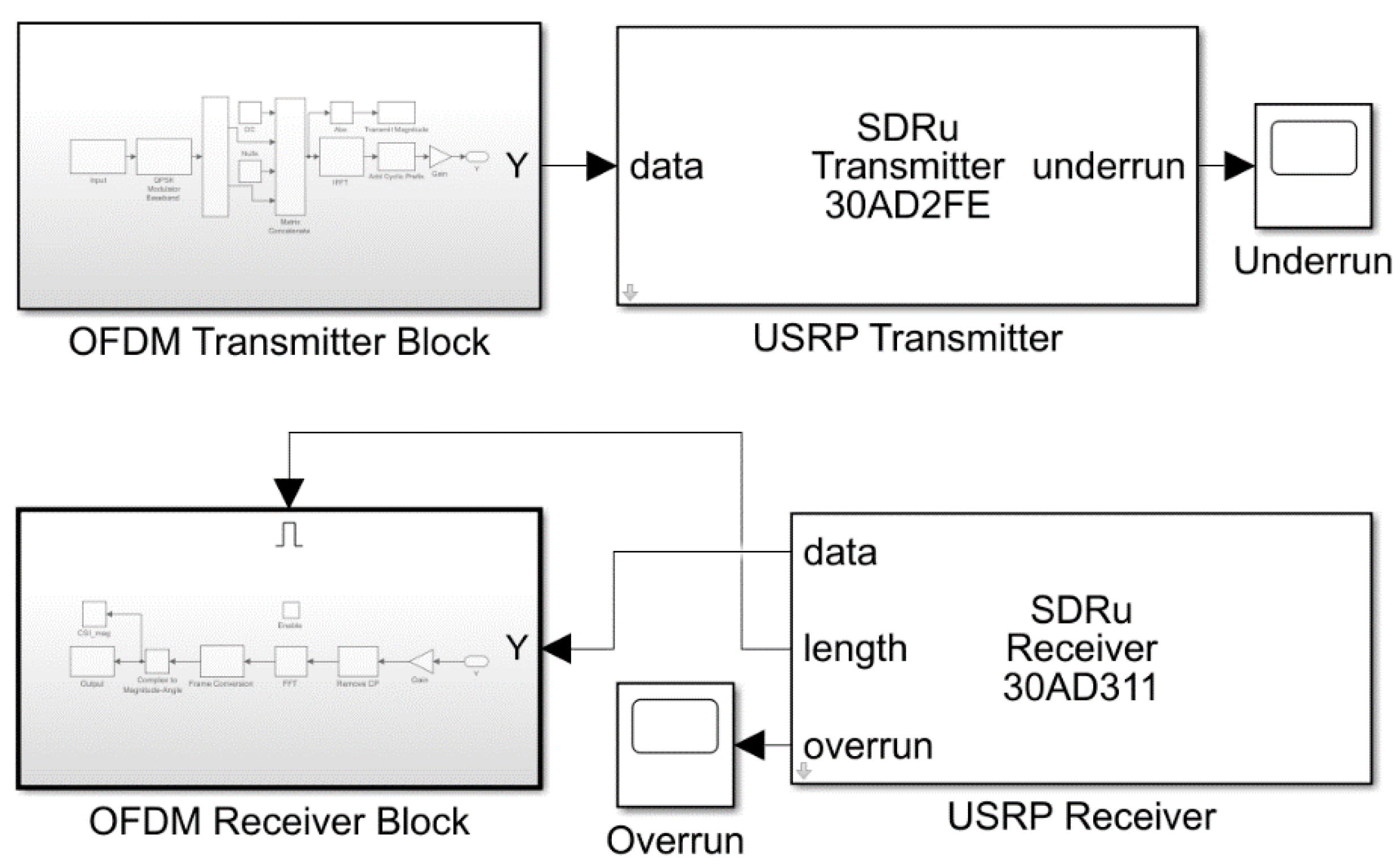
3.1. Hardware Functionality
3.2. Software Functionality
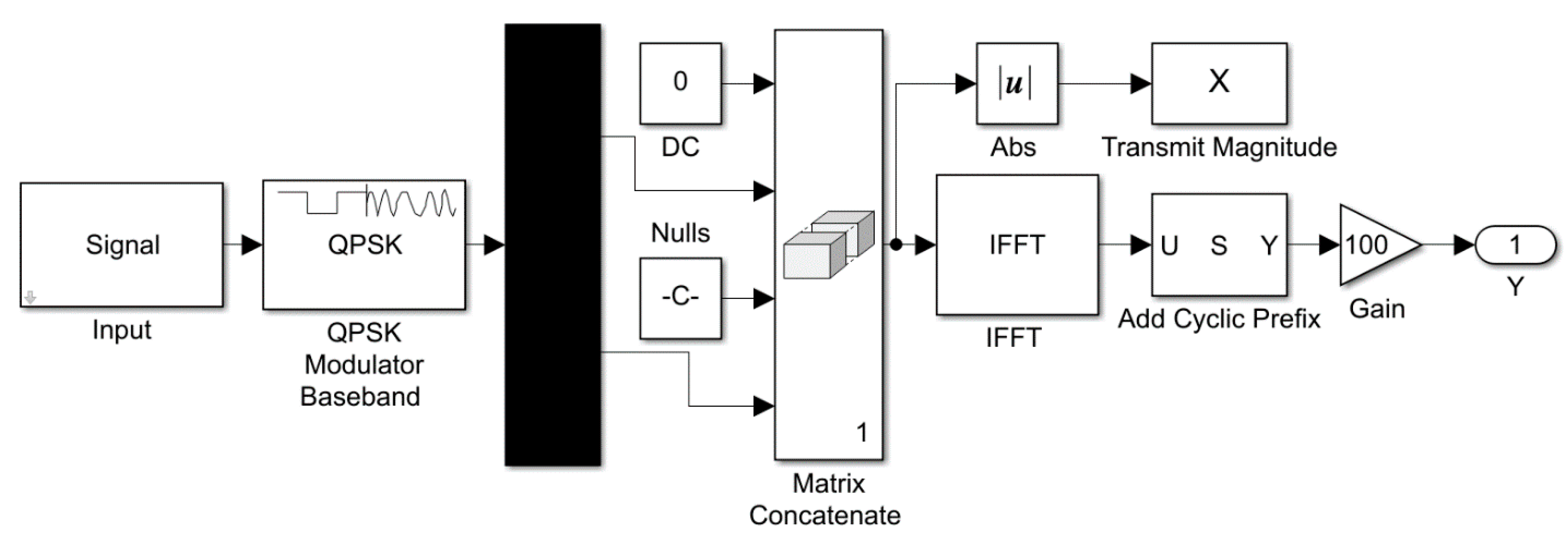
3.2.1. Transmitter Process
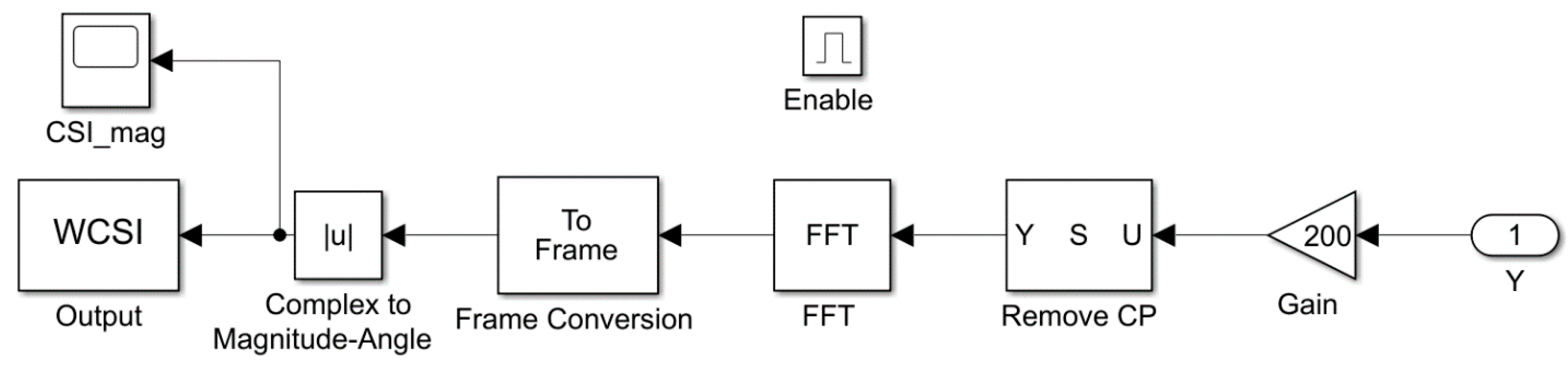
3.2.2. Receiver Process
3.3. Classification Approach
4. Experimental Setup
5. Results and Discussion
- I.
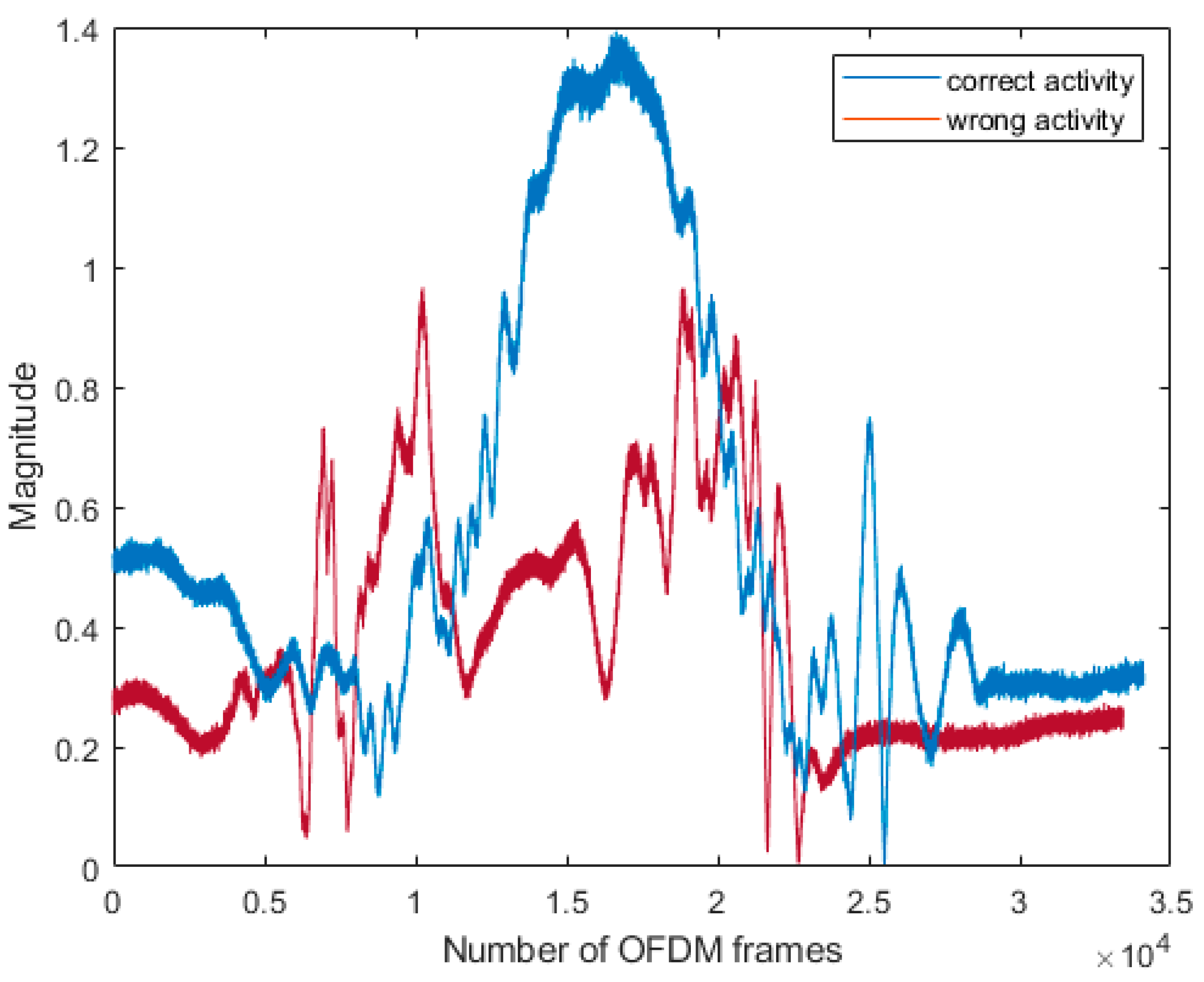
- Correct and wrong activity magnitude response in the frequency domain.
- II.
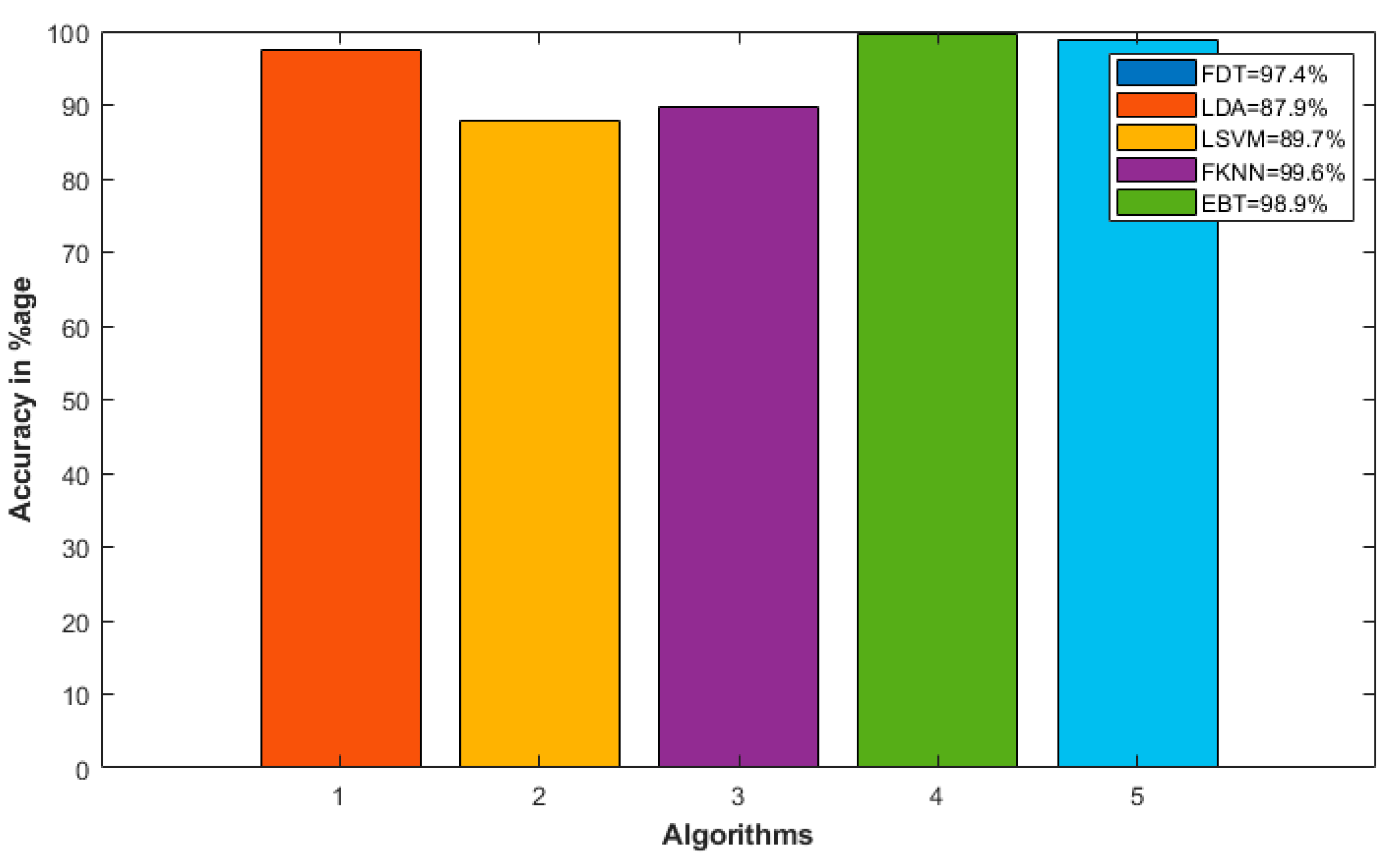
- Accuracy of the machine-learning algorithms model.
5.1. Correct and Wrong Activity Magnitude Response in the Frequency Domain
5.2. Accuracy of the Machine Learning Algorithms Model
- Fine decision tree (FDT)
- Linear discriminant analysis (LDA)
- Linear support vector machine (LSVM)
- Fine k-nearest neighbor (FKNN)
- Ensemble boosted trees (EBT)
6. Conclusions and Future Recommendations
Author Contributions
Funding
Conflicts of Interest
References
- Rahmani, A.M.; Gia, T.N.; Negash, B.; Anzanpour, A.; Azimi, I.; Jiang, M.; Liljeberg, P.J.F.G.C.S. Exploiting smart e-Health gateways at the edge of healthcare Internet-of-Things: A fog computing approach. Future Gener. Comput. Syst. 2018, 78, 641–658. [Google Scholar] [CrossRef]
- Oueida, S.; Kotb, Y.; Aloqaily, M.; Jararweh, Y.; Baker, T.J.S. An edge computing based smart healthcare framework for resource management. Sensors 2018, 18, 4307. [Google Scholar] [CrossRef] [PubMed]
- Al-Turjman, F.; Zahmatkesh, H.; Mostarda, L.J.I.A. Quantifying uncertainty in internet of medical things and big-data services using intelligence and deep learning. IEEE Access 2019, 7, 115749–115759. [Google Scholar] [CrossRef]
- Deebak, B.; Al-Turjman, F.; Aloqaily, M.; Alfandi, O.J.I.A. An Authentic-Based Privacy Preservation Protocol for Smart e-Healthcare Systems in IoT. IEEE Access 2019, 7, 135632–135649. [Google Scholar] [CrossRef]
- Samani, H.; Zhu, R.J.I.A. Robotic automated external defibrillator ambulance for emergency medical service in smart cities. IEEE Access 2016, 4, 268–283. [Google Scholar] [CrossRef]
- Bickenbach, J.E.; Biering-Sorensen, F.; Knott, J.; Shakespeare, T.; Stucki, G.; Tharion, G. Understanding spinal cord injury. In International Perspectives on Spinal Cord Injury; Bickenbach, J.E., Ed.; WHO: Geneva, Switzerland, 2013; pp. 15–17. [Google Scholar]
- Fleury, A.; Vacher, M.; Noury, N. SVM-based multimodal classification of activities of daily living in health smart homes: Sensors, algorithms, and first experimental results. IEEE Trans. Inf. Technol. Biomed. 2010, 14, 274–283. [Google Scholar] [CrossRef]
- Kasteren, T.L.; Englebienne, G.; Kröse, B.J. An activity monitoring system for elderly care using generative and discriminative models. J. Pers. Ubiquitous Comput. 2010, 14, 489–498. [Google Scholar] [CrossRef]
- Khan, B.; Yang, X.; Ren, A.; Al-hababi, M.; Zhao, N.; Guan, L.; Fan, D.; Aziz Shah, S. Design of Software Defined Radios Based Test bed for Activity Recognition. IEEE Access 2019, 7, 31083–31088. [Google Scholar] [CrossRef]
- Nee, R.V.; Prasad, R. OFDM for Wireless Multimedia Communications; Artech House, Inc.: Norwood, MA, USA, 2000. [Google Scholar]
- Siamak, Y.; Narui, H.; Dayal, S.; Ermon, S.; Valaee, S. A survey on behavior recognition using wifi channel state information. IEEE Commun. Mag. 2017, 55, 98–104. [Google Scholar]
- Wang, Y.; Jiang, X.; Cao, R.; Wang, X. Robust indoor human activity recognition using wireless signals. Sensors 2015, 15, 17195–17208. [Google Scholar] [CrossRef]
- Wang, H.; Zhang, D.; Wang, Y.; Ma, J.; Wang, Y.; Li, S. RT-Fall: A Real-Time and Contactless Fall Detection System with Commodity WiFi Devices. IEEE Trans. Mobile Comput. 2017, 16, 511–526. [Google Scholar] [CrossRef]
- Wang, X.; Yang, C.; Mao, S. TensorBeat: Tensor Decomposition for Monitoring Multiperson Breathing Beats with Commodity WiFi. ACM Trans. Intell. Syst. Technol. (TIST) 2017, 9, 1–27. [Google Scholar] [CrossRef]
- Al-Turjman, F.; Nawaz, M.H.; Ulusar, U.D.J.C.C. Intelligence in the Internet of Medical Things era: A systematic review of current and future trends. Comput. Commun. 2019, 150, 644–660. [Google Scholar] [CrossRef]
- Vallabh, P.; Malekian, R. Fall Detection Monitoring Systems: A Comprehensive Review. J. Ambient Intell. Hum. Comput. 2018, 9, 1809–1833. [Google Scholar] [CrossRef]
- Lotfi, A.; Albawendi, S.; Powell, H.; Appiah, K.; Langensiepen, C. Supporting Independent Living for Older Adults; Employing a Visual Based Fall Detection Through Analysing the Motion and Shape of the Human Body. IEEE Access 2016, 6, 70272–70282. [Google Scholar] [CrossRef]
- Zhang, Z.; Conly, C.; Anthitsos, V. A Survey on Vision-based Fall Detection. In Proceedings of the 8th ACM International Conference on Pervasive Technologies Related to Assistive Environments, Corfu, Greece, 1–3 July 2015; pp. 1–7. [Google Scholar]
- De Miguel, K.; Brunete, A.; Hernando, M.; Gambao, E. Home camera-based fall detection system for the elderly. Sensors 2017, 17, 2864. [Google Scholar] [CrossRef]
- Balakrishnan, G.; Durand, F.; Guttag, J. Detecting pulse from head motions in video. In Proceedings of the IEEE Conference on Computer Vision and Pattern Recognition (CVPR), Portland, OR, USA, 25–27 June 2013; pp. 3430–3437. [Google Scholar]
- Jain, H.; Chen, H. A Portable Fall Detection and Alerting System Based on k-NN Algorithm and Remote Medicine. China Commun. Mag. 2015, 12, 23–31. [Google Scholar] [CrossRef]
- Sabatini, A.M.; Ligorio, G.; Mannini, A.; Genovese, V.; Pinna, L. Prior-to- and Post-Impact Fall Detection Using Inertial and Barometric Altimeter Measurements. IEEE Trans. Neural Syst. Rehabil. Eng. 2016, 24, 774–783. [Google Scholar] [CrossRef]
- Zigel, Y.; Litvak, D.; Gannot, I. A Method for Automatic Fall Detection of Elderly People Using loor Vibrations and Sound—Proof of Concept on Human Mimicking Doll Falls. IEEE Trans. Biomed. Eng. 2009, 56, 2858–2867. [Google Scholar] [CrossRef]
- Luque, R.; Casilari, E.; Morón, M.J.; Redondo, G. Comparison and Characterization of Android-Based Fall Detection Systems. Sensors 2014, 14, 18543–18574. [Google Scholar] [CrossRef]
- Garripoli, C.; Mercuri, M.; Karsmakers, P.; Soh, P.J.; Crupi, G.; Vandenbosch, G.A.E.; Pace, C.; Leroux, P.; Schreurs, D. Embedded DSP-Based Telehealth Radar System for Remote In-Door Fall Detection. IEEE J. Biomed. Health Inform. 2015, 19, 92–101. [Google Scholar] [CrossRef] [PubMed]
- Jokanovíc, B.; Amin, M. Fall Detection Using Deep Learning in Range-Doppler Radars. IEEE Trans. Aerosp. Electron. Syst. 2018, 54, 180–189. [Google Scholar] [CrossRef]
- Sugano, M.; Kawazoe, T.; Ohta, Y.; Murata, M. Indoor Localization System using RSSI Measurement of Wireless Sensor Network based on ZigBee Standard. In Proceedings of the 2006 IFIP International Conference on Wireless and Optical Communications, Bangalore, India, 11–13 April 2006; pp. 1–6. [Google Scholar]
- Vasisht, D.; Kumar, S.; Katabi, D. Decimeter-Level Localization with a Single WiFi Access Point. In Proceedings of the USENIX Symposium on Networked Systems Design and Implementation (NSDI), Santa Clara, CA, USA, 16–18 March 2016; pp. 165–178. [Google Scholar]
- Ali, K.; Liu, A.X.; Wang, W.; Shahzad, M. Recognizing Keystrokes Using WiFi Devices. IEEE J. Sel. Areas Commun. 2017, 35, 1175–1190. [Google Scholar] [CrossRef]
- Zhao, M.; Li, T.; Abu Alsheikh, M.; Tian, Y.; Zhao, H.; Torralba, A.; Katabi, D. Through-wall human pose estimation using radio signals. In Proceedings of the IEEE Conference on Computer Vision and Pattern Recognition (CVPR), Salt Lake City, UT, USA, 19–21 June 2018; pp. 7356–7365. [Google Scholar]
- Zhang, Z.; Ishida, S.; Tagashira, S.; Fukuda, A. Danger-pose detection system using commodity Wi-Fi for bathroom monitoring. Sensors 2019, 19, 884. [Google Scholar] [CrossRef] [PubMed]
- Available online: http://www.sasksurgery.ca/patient/spine.html (accessed on 2 July 2020).


| Abbreviation | Description | Abbreviation | Description |
|---|---|---|---|
| ADC | Analog to Digital Converter | LOS | Line of Sight |
| AI | Artificial Intelligence | LPA | Log Periodic Antenna |
| CP | Cyclic Prefix | LPF | Low Pass Filter |
| DAC | Analog Conversion | LSVM | Linear Support Vector Machine |
| DAC | Digital to Analog Converter | NLOS | Non-Line-of Sight |
| DC | Direct Current | OFDM | Orthogonal Frequency Division Multiplexing |
| DDC | Digital down Converter | PCA | Principal Component Analysis |
| DUC | Digital up Conversion | QPSK | Quadrature Phase Shift Keying |
| EBT | Ensemble Boosted Trees | RF | Radio Frequency |
| FDT | Fine Decision Tree | RGB | Red Green Blue |
| FFT | Fast Fourier Transform | RSS | Received Signal Strength |
| FKNN | Fine K-Nearest Neighbor | TA | Transmit Amplification |
| IFFT | Inverse Fast Fourier Transform | ToF | Time of Flight |
| ISCOS | International Spinal Cord Society | USRP | Universal Software-Defined Radio Peripheral |
| ISI | Inter Symbol Interference | WCSI | Wireless Channel State Information |
| LDA | Linear Discriminant Analysis | WHO | World Health Organization |
| Testbed | USRP B210 |
|---|---|
| Antenna | Omni-directional |
| Device Frequency Range | 70 MHz–6 GHz |
| Channel Mapping Rx | 1 |
| Channel Mapping Tx | 1 |
| Center Frequency | 5.32 GHz |
| Clock Source & PPS Source | Internal |
| Master Clock Rate | 200 MHz |
| Interpolation Factor | 250 |
| Enable Burst mode | False |
| Transport data type | int16 |
| Decimation Factor | 250 |
| Output data type | Same as transport data type |
| Transmitter serial number | 30AD2FE |
| Receiver serial number | 30AD311 |
| Transmitter Gain | 70 |
| Receiver Gain | 50 |
| Samples per frames | 80 |
| Parameter | Values/Type |
|---|---|
| Input Bits | 104 |
| Bits per Symbols (M) | 2 |
| Modulation type | QPSK |
| OFDM subcarriers | 64 |
| Data subcarriers | 52 |
| Null subcarriers | 11 |
| DC | 1 |
| Used subcarriers | 52 |
| NFFT | 64 |
| Cyclic prefix | NFFT - Data subcarriers |
| Sampling Frequency | 80,000 |
| Samples per frames | 80 |
| Sr.No | Subject | Body structure | Height (cm) | Weight (Kg) |
|---|---|---|---|---|
| 1 | Male | Ectomorph | 168 | 55 |
| 2 | Male | Endomorph | 180 | 95 |
| 3 | Female | Mesomorph | 168 | 60 |
| 4 | Male | Mesomorph | 174 | 76 |
| 5 | Male | Ectomorph | 176 | 60 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Al-hababi, M.A.M.; Khan, M.B.; Al-Turjman, F.; Zhao, N.; Yang, X. Non-Contact Sensing Testbed for Post-Surgery Monitoring by Exploiting Artificial-Intelligence. Appl. Sci. 2020, 10, 4886. https://doi.org/10.3390/app10144886
Al-hababi MAM, Khan MB, Al-Turjman F, Zhao N, Yang X. Non-Contact Sensing Testbed for Post-Surgery Monitoring by Exploiting Artificial-Intelligence. Applied Sciences. 2020; 10(14):4886. https://doi.org/10.3390/app10144886
Chicago/Turabian StyleAl-hababi, Mohammed Ali Mohammed, Muhammad Bilal Khan, Fadi Al-Turjman, Nan Zhao, and Xiaodong Yang. 2020. "Non-Contact Sensing Testbed for Post-Surgery Monitoring by Exploiting Artificial-Intelligence" Applied Sciences 10, no. 14: 4886. https://doi.org/10.3390/app10144886
APA StyleAl-hababi, M. A. M., Khan, M. B., Al-Turjman, F., Zhao, N., & Yang, X. (2020). Non-Contact Sensing Testbed for Post-Surgery Monitoring by Exploiting Artificial-Intelligence. Applied Sciences, 10(14), 4886. https://doi.org/10.3390/app10144886





