Digital Design of Minimally Invasive Endodontic Access Cavity
Abstract
:1. Introduction
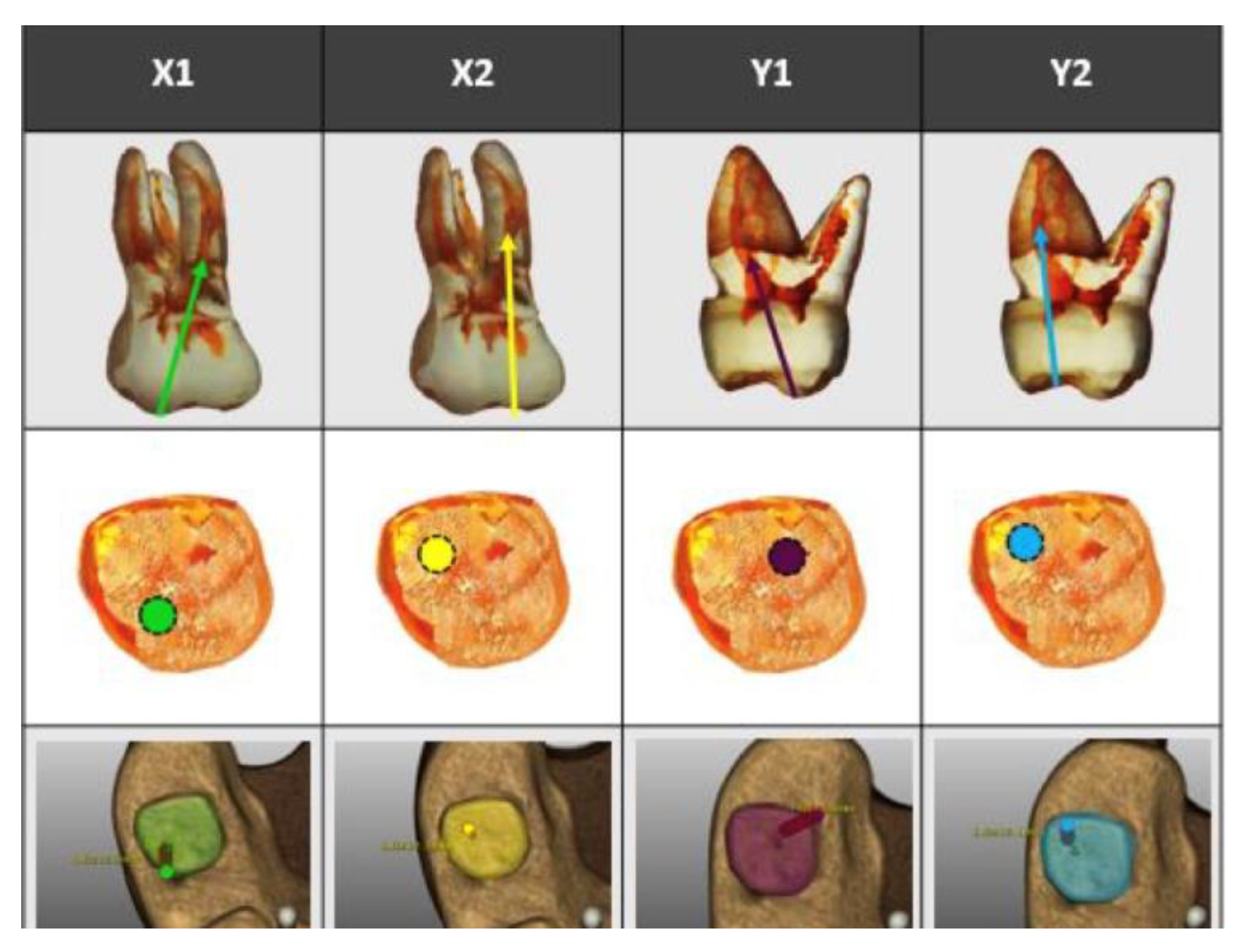
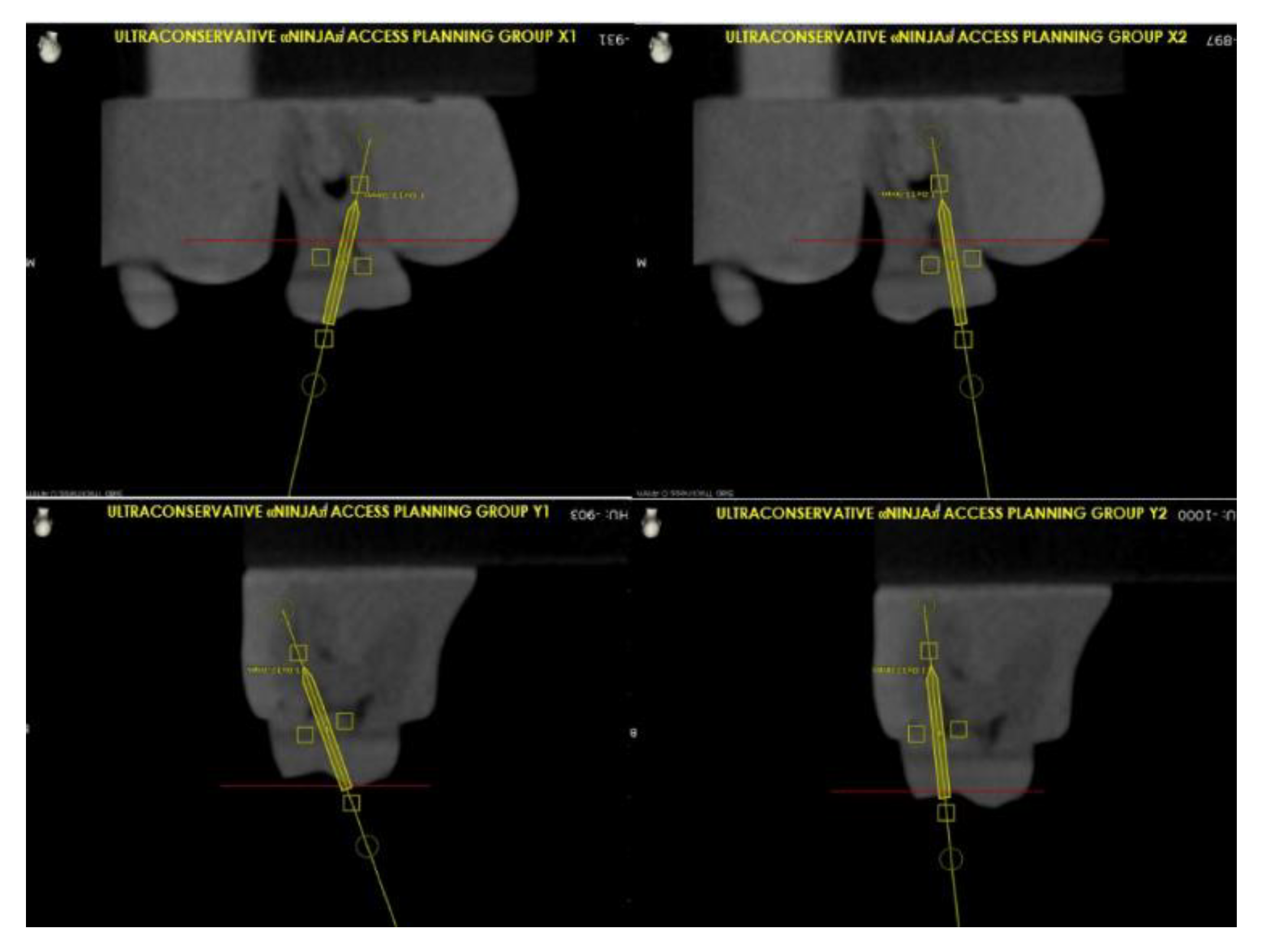
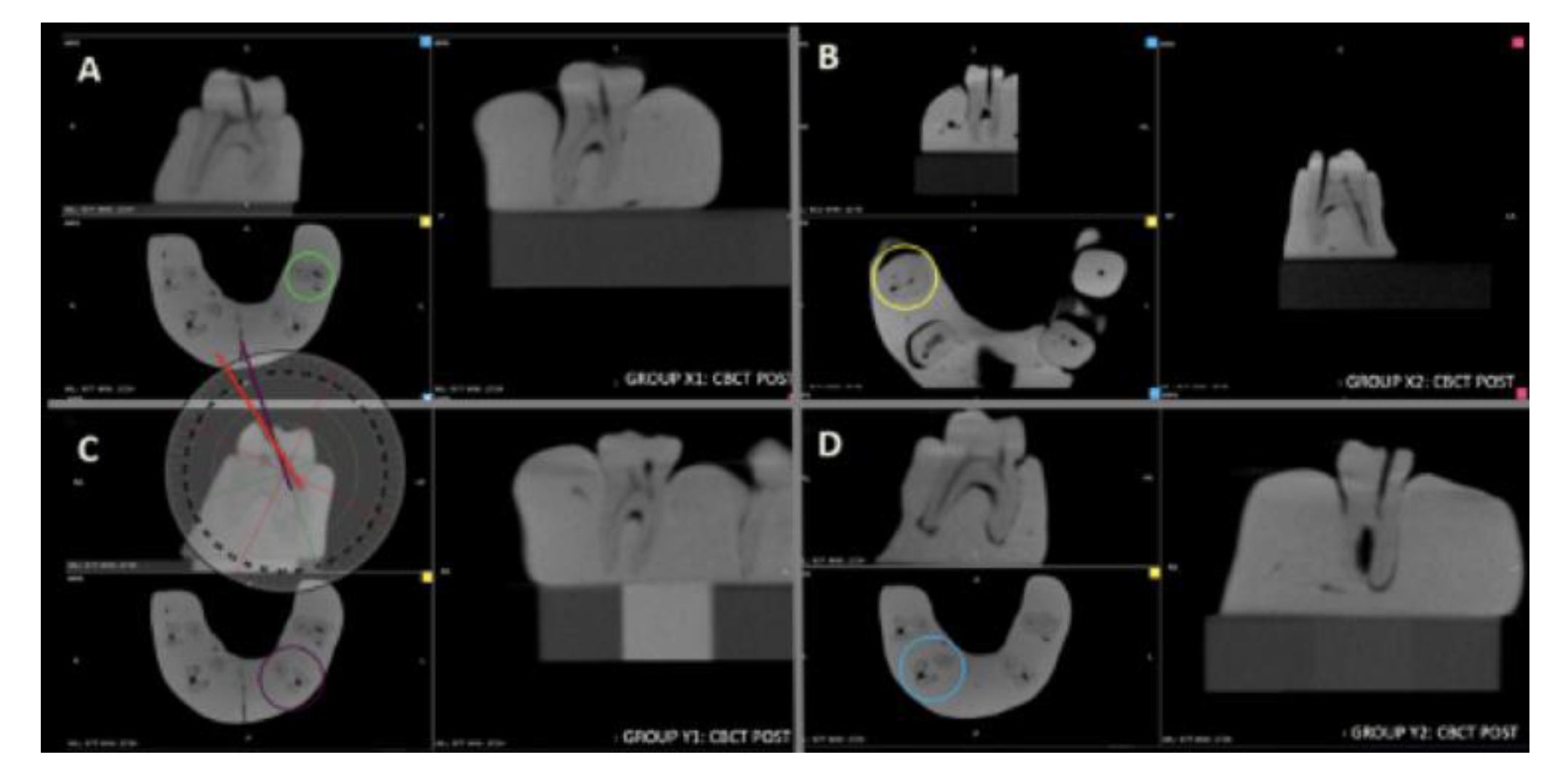
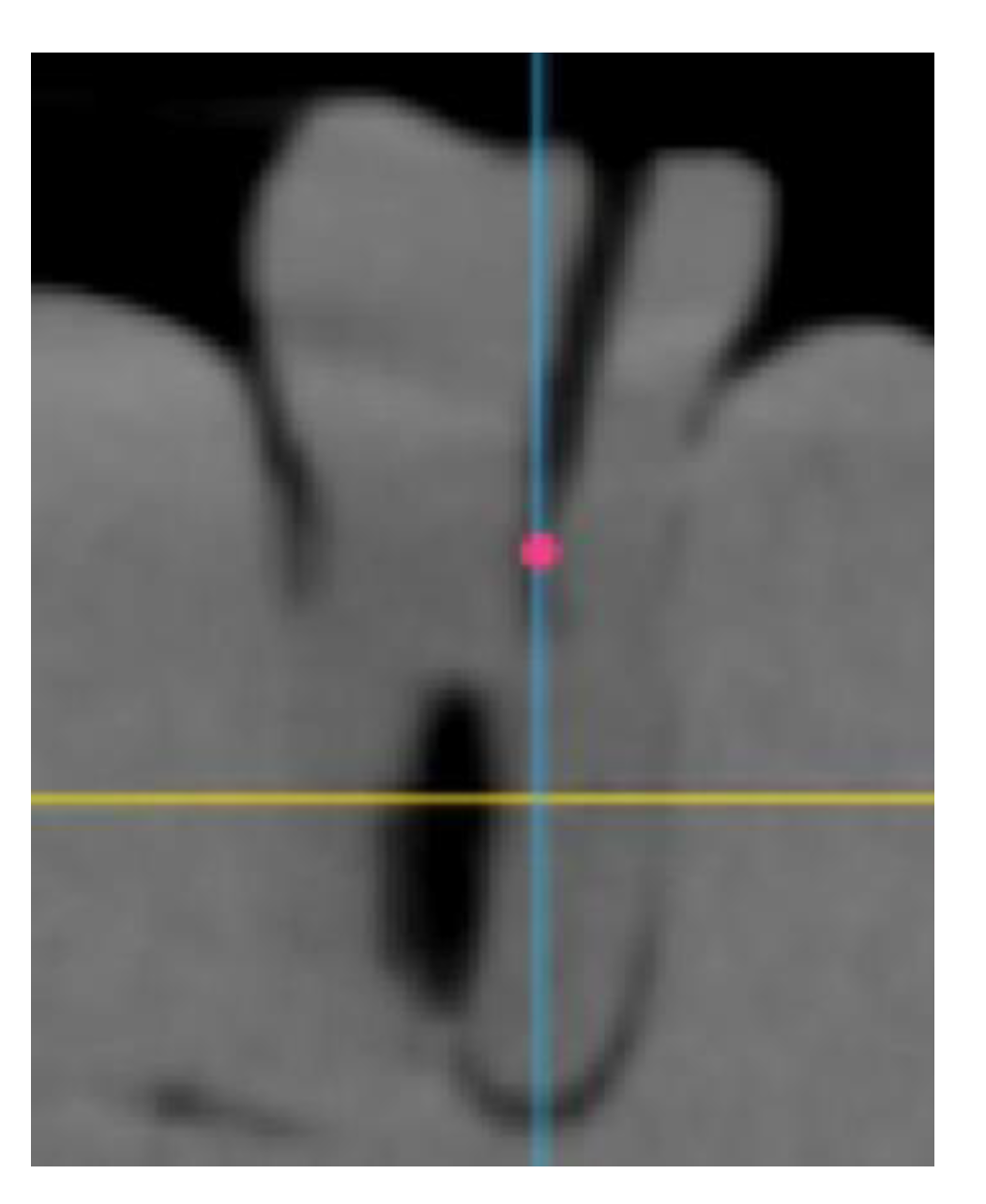
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Gambarini, G.; Seracchiani, M.; Piasecki, L.; Valenti Obino, F.; Galli, M.; Di Nardo, D.; Testarelli, L. Measurement of torque generated during intracanal instrumentation in vivo. Int. Endod. J. 2019, 52, 737–745. [Google Scholar] [CrossRef] [PubMed]
- Gambarini, G.; Piasecki, L.; Miccoli, G.; Gaimari, G.; Di Giorgio, R.; Di Nardo, D.; Azim, A.A.; Testarelli, L. Classification and cyclic fatigue evaluation of new kinematics for endodontic instruments. Aust. Endod. J. 2019, 45, 154–162. [Google Scholar] [CrossRef] [PubMed]
- Gambarini, G.; Miccoli, G.; Seracchiani, M.; Morese, A.; Piasecki, L.; Gaimari, G.; Di Nardo, D.; Testarelli, L. Fatigue Resistance of New and Used Nickel-Titanium Rotary Instruments: A Comparative Study. Clin. Ter. 2018, 169, 96–101. [Google Scholar]
- Gambarini, G.; Piasecki, L.; Miccoli, G.; Gaimari, G.; Di Nardo, D.; Testarelli, L. Cone-beam computed tomography in the assessment of periapical lesions in endodontically treated teeth. Eur. J. Dent. 2018, 12, 136–143. [Google Scholar] [CrossRef] [PubMed]
- Landys Boren, D.; Jonasson, P.; Kvist, T. Long-term survival of endodontically treated teeth at a public dental specialist clinic. J. Endod. 2015, 41, 176–181. [Google Scholar] [CrossRef] [PubMed]
- Fransson, H.; Dawson, V.S.; Frisk, F.; Bjørndal, L.; Kvist, T. Survival of root-filled teeth in the Swedish adult population. J. Endod. 2016, 42, 216–220. [Google Scholar] [CrossRef] [PubMed]
- Tang, W.; Wu, Y.; Smales, R.J. Identifying and reducing risks for potential fractures in endodontically treated teeth. J. Endod. 2010, 36, 609–617. [Google Scholar] [CrossRef]
- Clark, D.; Khademi, J. Modern molar endodontic access and directed dentin conservation. Dent. Clin. N. Am. 2010, 54, 249–273. [Google Scholar] [CrossRef]
- Pereira, J.; McDonald, A.; Petrie, A.; Knowles, J. Effect of cavity design on tooth surface strain. J. Prosthet. Dent. 2013, 110, 369–375. [Google Scholar] [CrossRef]
- Boveda, C.; Kishen, A. Contracted endodontic cavities: The foundation for less invasivealternatives in the management of apical periodontitis. Endod. Top. 2015, 33, 169–186. [Google Scholar] [CrossRef]
- Panitvisai, P.; Messer, H.H. Cuspal deflection in molars in relation to endodontic and restorative procedures. J. Endod. 1995, 21, 57–61. [Google Scholar] [CrossRef]
- Reeh, E.S.; Messer, H.H.; Douglas, W.H. Reduction in tooth stiffness as a result of endodontic and restorative procedures. J. Endod. 1989, 15, 512–516. [Google Scholar] [CrossRef]
- Patel, S.; Rhodes, J. A practical guide to endodontic access cavity preparation in molar teeth. Br. Dent. J. 2007, 203, 133–140. [Google Scholar] [CrossRef] [PubMed]
- Clark, D.; Khademi, J.A. Case studies in modern molar endodontic access and directed dentin conservation. Dent. Clin. N. Am. 2010, 54, 275–289. [Google Scholar] [CrossRef]
- Corsentino, G.; Pedullà, E.; Castelli, L.; Liguori, M.; Spicciarelli, V.; Martignoni, M.; Ferrari, M.; Grandini, S. Influence of Access Cavity Preparation and Remaining Tooth Substance on Fracture Strength of Endodontically Treated Teeth. J. Endod. 2018, 44, 1416–1421. [Google Scholar] [CrossRef]
- Plotino, G.; Grande, N.M.; Isufi, A.; Ioppolo, P.; Pedullà, E.; Bedini, R.; Gambarini, G.; Testarelli, L. Fracture Strength of Endodontically Treated Teeth with Differen Access Cavity Designs. J. Endod. 2017, 43, 995–1000. [Google Scholar] [CrossRef]
- Saygili, G.; Uysal, B.; Omar, B.; Ertas, E.T.; Ertas, H. Evaluation of relationship between endodontic access cavity types and secondary mesiobuccal canal detection. BMC Oral Health 2018, 18, 121–124. [Google Scholar] [CrossRef] [Green Version]
- Abou-Elnaga, M.Y.; Alkhawas, M.A.M.; Kim, H.C.; Refai, A.S. Effect of Truss Access and Artificial Truss Restoration on the Fracture Resistance of Endodontically Treated Mandibular First Molars. J. Endod. 2019, 45, 813–817. [Google Scholar] [CrossRef]
- Gambarini, G.; Galli, M.; Stefanelli, L.V.; Di Nardo, D.; Morese, A.; Seracchiani, M.; De Angelis, F.; Di Carlo, S.; Testarelli, L. Endodontic Microsurgery Using Dynamic Navigation System: A Case Report. J. Endod. 2019, 45, 1397–1402. [Google Scholar] [CrossRef]
- Moore, B.; Verdelis, K.; Kishen, A.; Dao, T.; Friedman, S. Impacts of contracted endodontic cavities on instrumentation efficacy and biomechanical responses in maxillary molars. J. Endod. 2016, 42, 1779–1783. [Google Scholar] [CrossRef] [Green Version]
- Zogheib, C.; Sfeir, G.; Plotino, G.; Deus, G.; Daou, M.; Khalil, I. Impact of Minimal Root Canal Taper on the Fracture Resistance of Endodontically Treated Bicuspids. J. Int. Soc. Prev. Community Dent. 2018, 8, 179–183. [Google Scholar] [CrossRef] [PubMed]
- Buchgreitz, J.; Buchgreitz, M.; Mortensen, D.; Bjørndal, L. Guided access cavity preparation using cone-beam computed tomography and optical surface scans—Anex vivo study. Int. Endod. J. 2016, 49, 790–795. [Google Scholar] [CrossRef] [PubMed]
- Stefanelli, L.V.; Mandelaris, G.A.; DeGroot, B.S.; Gambarini, G.; De Angelis, F.; Di Carlo, S. Accuracy of a Novel Trace-Registration Method for Dynamic Navigation Surgery. Int. J. Periodontics Restor. Dent. 2020, 40, 427–435. [Google Scholar] [CrossRef] [PubMed]
- Stefanelli, L.V.; DeGroot, B.S.; Lipton, D.I.; Mandelaris, G.A. Accuracy of a Dynamic Dental Implant Navigation System in a Private Practice. Int. J. Oral Maxillofac. Implants 2019, 34, 205–213. [Google Scholar] [CrossRef]
- Connert, T.; Zehnder, M.S.; Weiger, R.; Kühl, S.; Krastl, G. Microguided endodontics: Accuracy of aminiaturized technique for apically extended access cavity preparation in anterior teeth. J. Endod. 2017, 43, 787–790. [Google Scholar] [CrossRef]
- Connert, T.; Zehnder, M.S.; Amato, M.; Weiger, R.; Kühl, S.; Krastl, G. Microguided Endodontics: A method to achieve minimally invasive access cavity preparation and root canal location in mandibular incisors using a novel computer-guided technique. Int. Endod. J. 2018, 51, 247–255. [Google Scholar] [CrossRef]

| Group | Mean Values and Standard Deviations |
|---|---|
| X1 | 3.6° (±0.4) a |
| X2 | 3.4° (±0.3) a |
| Y1 | 7.1° (±0.8) b |
| Y2 | 7.2° (±0.7) b |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gambarini, G.; Galli, M.; Morese, A.; Abduljabbar, F.; Seracchiani, M.; Stefanelli, L.V.; Giovarruscio, M.; Di Nardo, D.; Testarelli, L. Digital Design of Minimally Invasive Endodontic Access Cavity. Appl. Sci. 2020, 10, 3513. https://doi.org/10.3390/app10103513
Gambarini G, Galli M, Morese A, Abduljabbar F, Seracchiani M, Stefanelli LV, Giovarruscio M, Di Nardo D, Testarelli L. Digital Design of Minimally Invasive Endodontic Access Cavity. Applied Sciences. 2020; 10(10):3513. https://doi.org/10.3390/app10103513
Chicago/Turabian StyleGambarini, Gianluca, Massimo Galli, Antonio Morese, Fouad Abduljabbar, Marco Seracchiani, Luigi Vito Stefanelli, Massimo Giovarruscio, Dario Di Nardo, and Luca Testarelli. 2020. "Digital Design of Minimally Invasive Endodontic Access Cavity" Applied Sciences 10, no. 10: 3513. https://doi.org/10.3390/app10103513







