A Non-Contact Photoplethysmography Technique for the Estimation of Heart Rate via Smartphone
Abstract
1. Introduction
2. Materials and Methods
2.1. Characteristics of Equipment Used
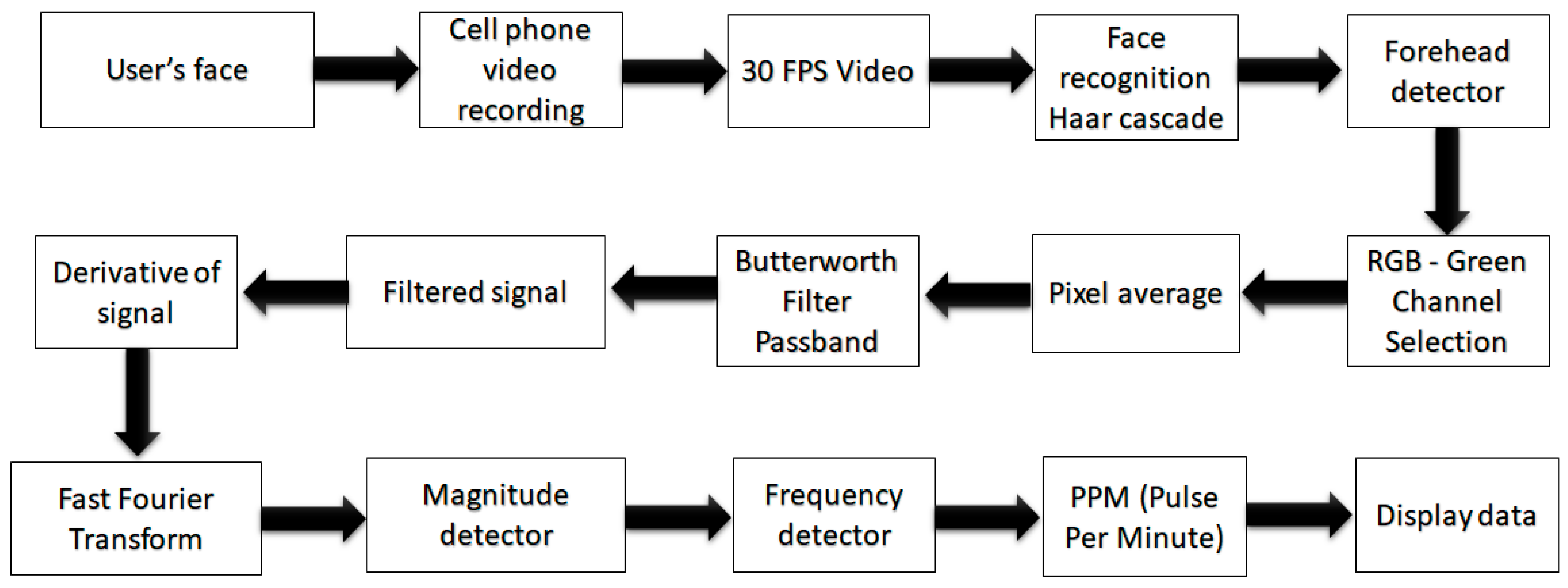
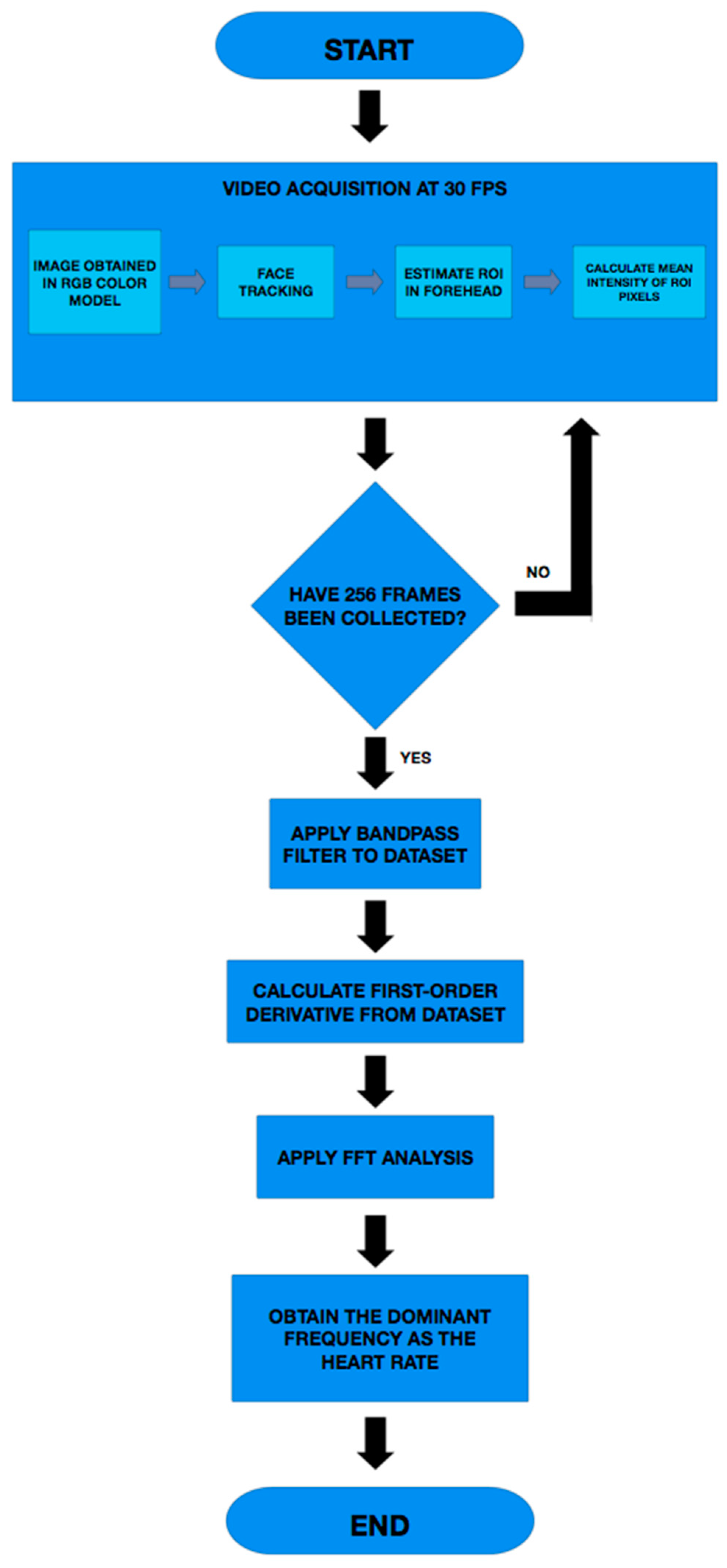
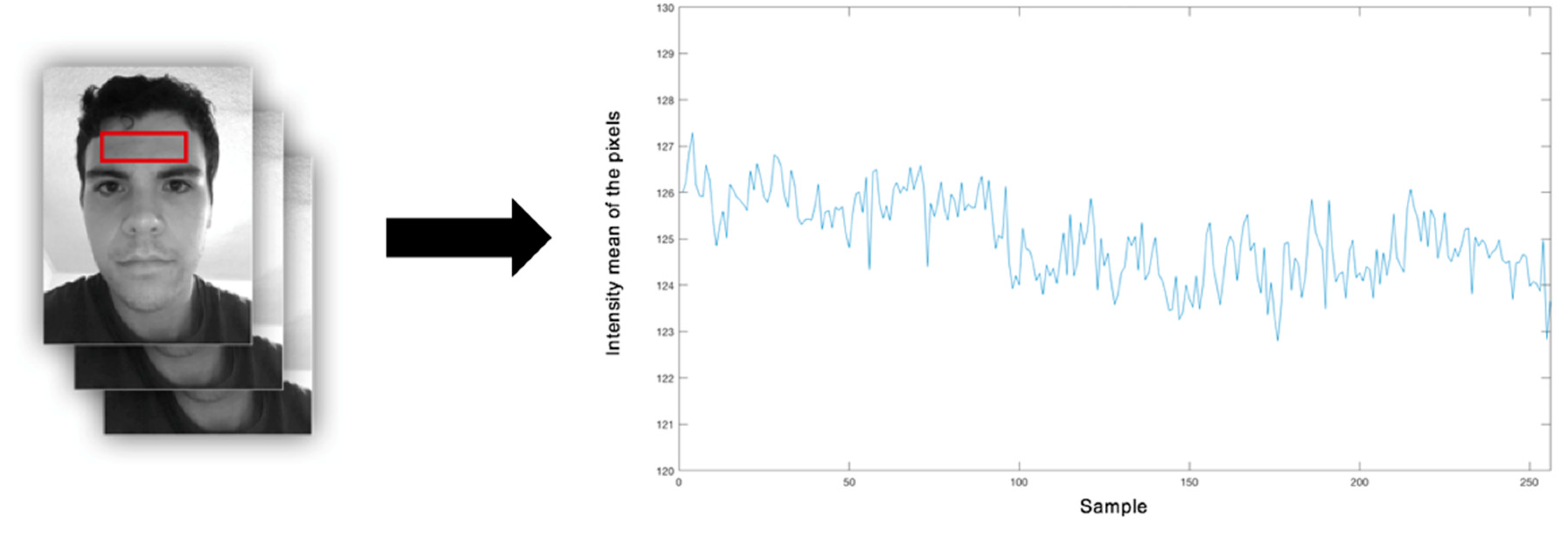
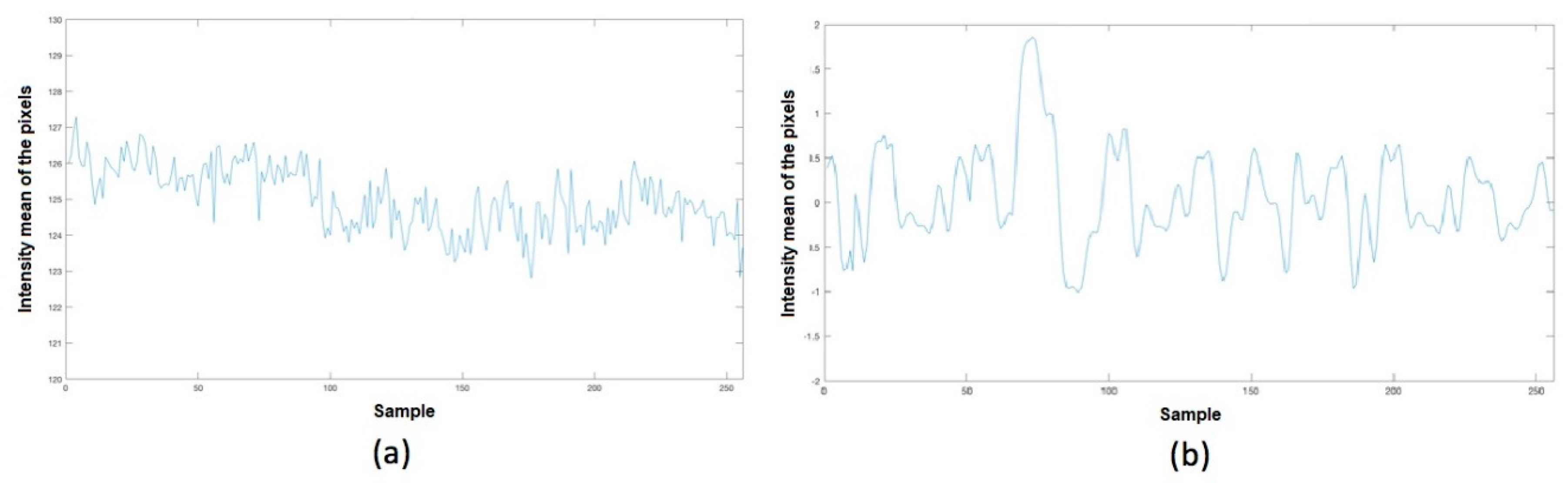
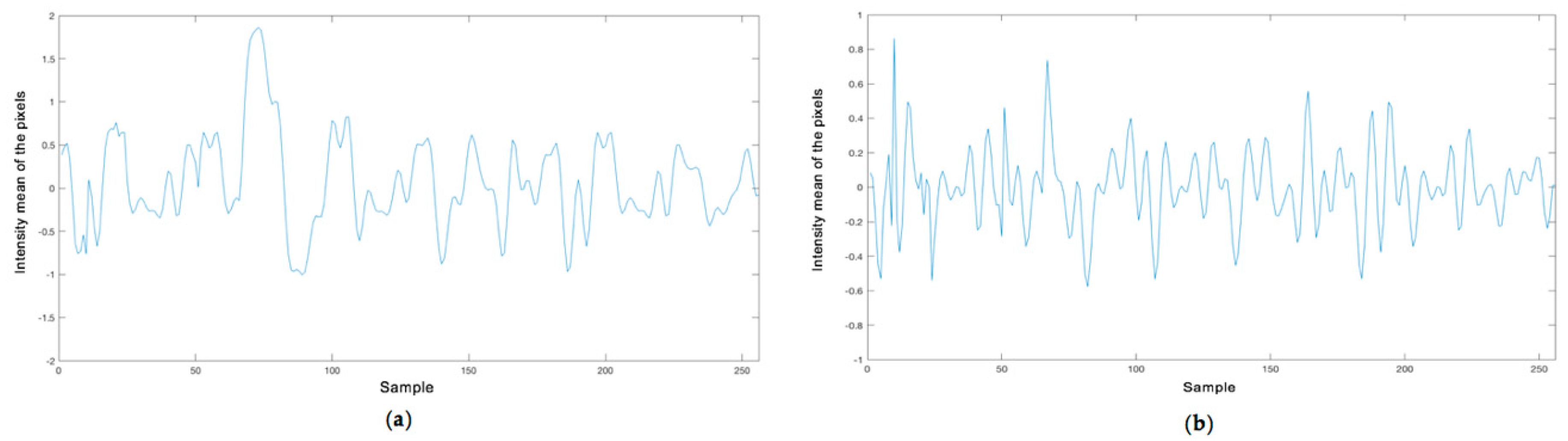
2.2. Implemented Technique
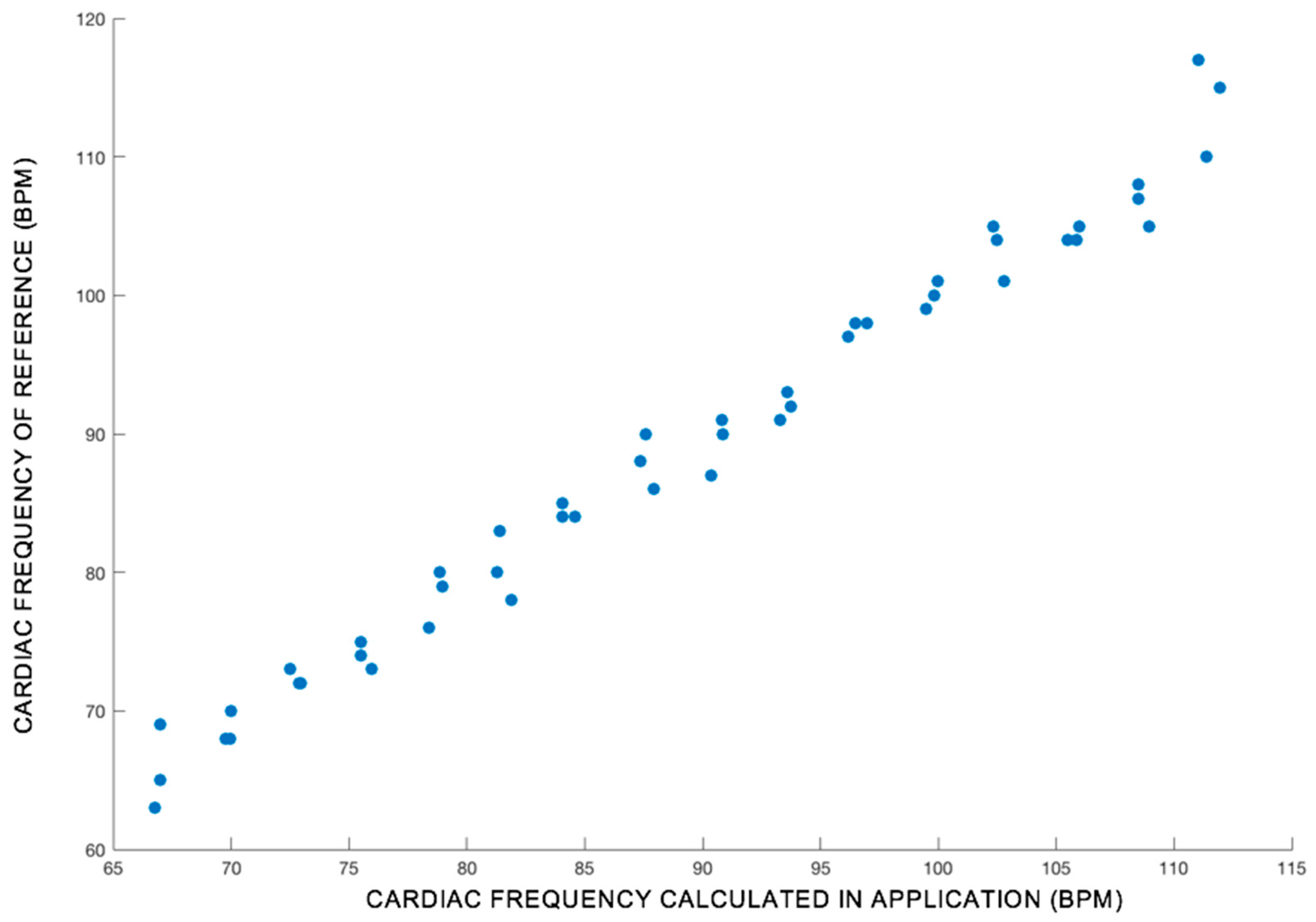
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Ethical Statements
Abbreviations
| PPG | Photoplethysmography |
| HR | Heart Rate |
| FFT | Fast Fourier Transform |
| ROI | Region of Interest |
| FPS | Frames Per Second |
| ECG | Electrocardiography |
| HRV | Heart Rate Variability |
| PPM | Pulses Per Minute |
| RGB | Red, Green, and Blue Channels |
| PPM | Pulses Per Minute |
References
- World Health Organization. Cardiovascular Diseases (CVDS): Fact Sheet No. 317. 2011; World Health Organization Google Scholar: Geneva, Switzerland, 2011. [Google Scholar]
- McCann, K.; Holdgate, A.; Mahammad, R.; Waddington, A. Accuracy of ECG electrode placement by emergency department clinicians. Emerg. Med. Australas. 2007, 19, 442–448. [Google Scholar] [CrossRef] [PubMed]
- Baek, J.-Y.; An, J.-H.; Choi, J.-M.; Park, K.-S.; Lee, S.-H. Flexible polymeric dry electrodes for the long-term monitoring of ecg. Sens. Actuators A Phys. 2008, 143, 423–429. [Google Scholar] [CrossRef]
- Bates, D.W.; Cohen, M.; Leape, L.L.; Overhage, J.M.; Shabot, M.M.; Sheridan, T. Reducing the frequency of errors in medicine using information technology. J. Am. Med. Inform. Assoc. 2001, 8, 299–308. [Google Scholar] [CrossRef] [PubMed]
- Selvaraj, N.; Jaryal, A.; Santhosh, J.; Deepak, K.K.; Anand, S. Assessment of heart rate variability derived from finger-tip photoplethysmography as compared to electrocardiography. J. Med. Eng. Technol. 2008, 32, 479–484. [Google Scholar] [CrossRef] [PubMed]
- Lin, S.-T.; Chen, W.-H.; Lin, Y.-H. A pulse rate detection method for mouse application based on multi-PPG sensors. Sensors 2017, 17, 1628. [Google Scholar]
- Gambi, E.; Agostinelli, A.; Belli, A.; Burattini, L.; Cippitelli, E.; Fioretti, S.; Pierleoni, P.; Ricciuti, M.; Sbrollini, A.; Spinsante, S. Heart rate detection using microsoft kinect: Validation and comparison to wearable devices. Sensors 2017, 17, 1776. [Google Scholar] [CrossRef] [PubMed]
- Poh, M.-Z.; McDuff, D.J.; Picard, R.W. Advancements in noncontact, multiparameter physiological measurements using a webcam. IEEE Trans. Biomed. Eng. 2011, 58, 7–11. [Google Scholar] [CrossRef] [PubMed]
- Bradski, G. OpenCV library. Dr. Dobbs J. 2000, 25, 120–126. [Google Scholar]
- Viola, P.; Jones, M. In Rapid object detection using a boosted cascade of simple features. In Proceedings of the 2001 IEEE Computer Society Conference on Computer Vision and Pattern Recognition, CVPR 2001, Kauai, HI, USA, 8–14 December 2001; IEEE: Piscataway, NJ, USA, 2001; p. 1. [Google Scholar]
- Bal, U. Non-contact estimation of heart rate and oxygen saturation using ambient light. Biomed. Opt. Express 2015, 6, 86–97. [Google Scholar] [CrossRef] [PubMed]
- Humphreys, K.; Ward, T.; Markham, C. Noncontact simultaneous dual wavelength photoplethysmography: A further step toward noncontact pulse oximetry. Rev. Sci. Instrum. 2007, 78, 044304. [Google Scholar] [CrossRef] [PubMed]
- Takano, C.; Ohta, Y. Heart rate measurement based on a time-lapse image. Med. Eng. Phys. 2007, 29, 853–857. [Google Scholar] [CrossRef] [PubMed]
- Tarassenko, L.; Villarroel, M.; Guazzi, A.; Jorge, J.; Clifton, D.; Pugh, C. Non-contact video-based vital sign monitoring using ambient light and auto-regressive models. Physiol. Meas. 2014, 35, 807. [Google Scholar] [CrossRef] [PubMed]
- Jerri, A.J. The shannon sampling theorem—Its various extensions and applications: A tutorial review. Proc. IEEE 1977, 65, 1565–1596. [Google Scholar] [CrossRef]
- Ori, Z.; Monir, G.; Weiss, J.; Sayhouni, X.; Singer, D. Heart rate variability. Frequency domain analysis. Cardiol. Clin. 1992, 10, 499–537. [Google Scholar] [CrossRef]


| Reference PPM | Application Estimated PPM |
|---|---|
| 67 | 65 |
| 70 | 70 |
| 82 | 83 |
| 84 | 85 |
| 87 | 88 |
| 88 | 90 |
| 100 | 99 |
| 106 | 104 |
| 108 | 107 |
| 111 | 110 |
| Descriptive Statistics | |||||
|---|---|---|---|---|---|
| Variable | Count | Mean | Standard Deviation | 95% LCL of Mean | 95% UCL of Mean |
| POX reference device | 47 | 89.40 | 13.9 | 85.4 | 93.38 |
| App PPM | 47 | 89.04 | 14.4 | 84.9 | 93.2 |
| Correlation Coefficient | 0.97898971 | ||||
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Maestre-Rendon, J.R.; Rivera-Roman, T.A.; Fernandez-Jaramillo, A.A.; Guerrón Paredes, N.E.; Serrano Olmedo, J.J. A Non-Contact Photoplethysmography Technique for the Estimation of Heart Rate via Smartphone. Appl. Sci. 2020, 10, 154. https://doi.org/10.3390/app10010154
Maestre-Rendon JR, Rivera-Roman TA, Fernandez-Jaramillo AA, Guerrón Paredes NE, Serrano Olmedo JJ. A Non-Contact Photoplethysmography Technique for the Estimation of Heart Rate via Smartphone. Applied Sciences. 2020; 10(1):154. https://doi.org/10.3390/app10010154
Chicago/Turabian StyleMaestre-Rendon, J. Rodolfo, Tomas A. Rivera-Roman, Arturo A. Fernandez-Jaramillo, Nancy E. Guerrón Paredes, and José Javier Serrano Olmedo. 2020. "A Non-Contact Photoplethysmography Technique for the Estimation of Heart Rate via Smartphone" Applied Sciences 10, no. 1: 154. https://doi.org/10.3390/app10010154
APA StyleMaestre-Rendon, J. R., Rivera-Roman, T. A., Fernandez-Jaramillo, A. A., Guerrón Paredes, N. E., & Serrano Olmedo, J. J. (2020). A Non-Contact Photoplethysmography Technique for the Estimation of Heart Rate via Smartphone. Applied Sciences, 10(1), 154. https://doi.org/10.3390/app10010154





