Home-Based Interventions to Treat and Prevent Childhood Obesity: A Systematic Review and Meta-Analysis
Abstract
1. Introduction
2. Objective
3. Methods
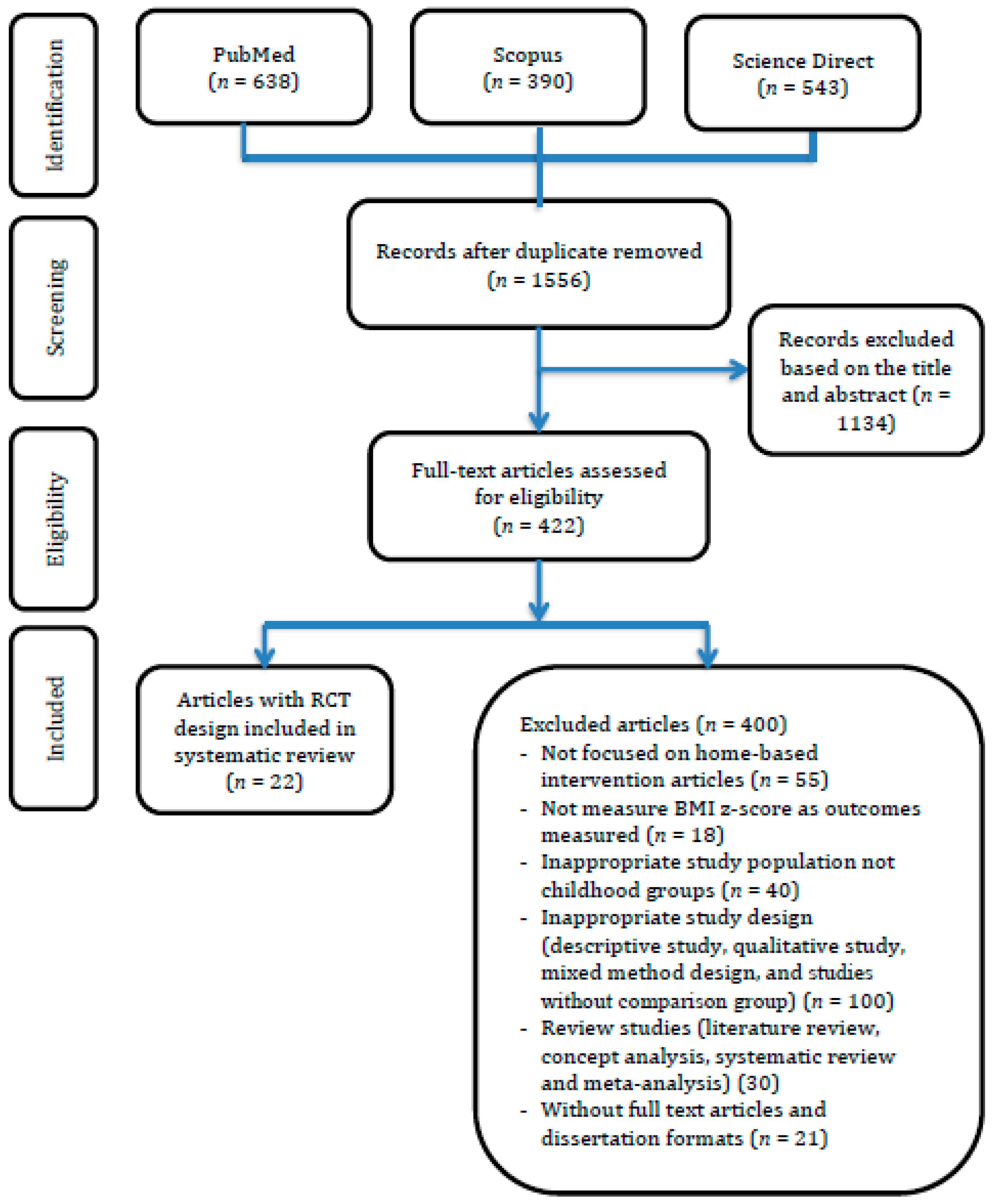
3.1. Data Sources
3.2. Search Strategy
3.3. Inclusion Criteria of Study
3.4. Exclusion Criteria
3.5. Quality Assessment and Controlling the Risk of Bias
3.6. Statistical Analysis
4. Results
4.1. Study Literature
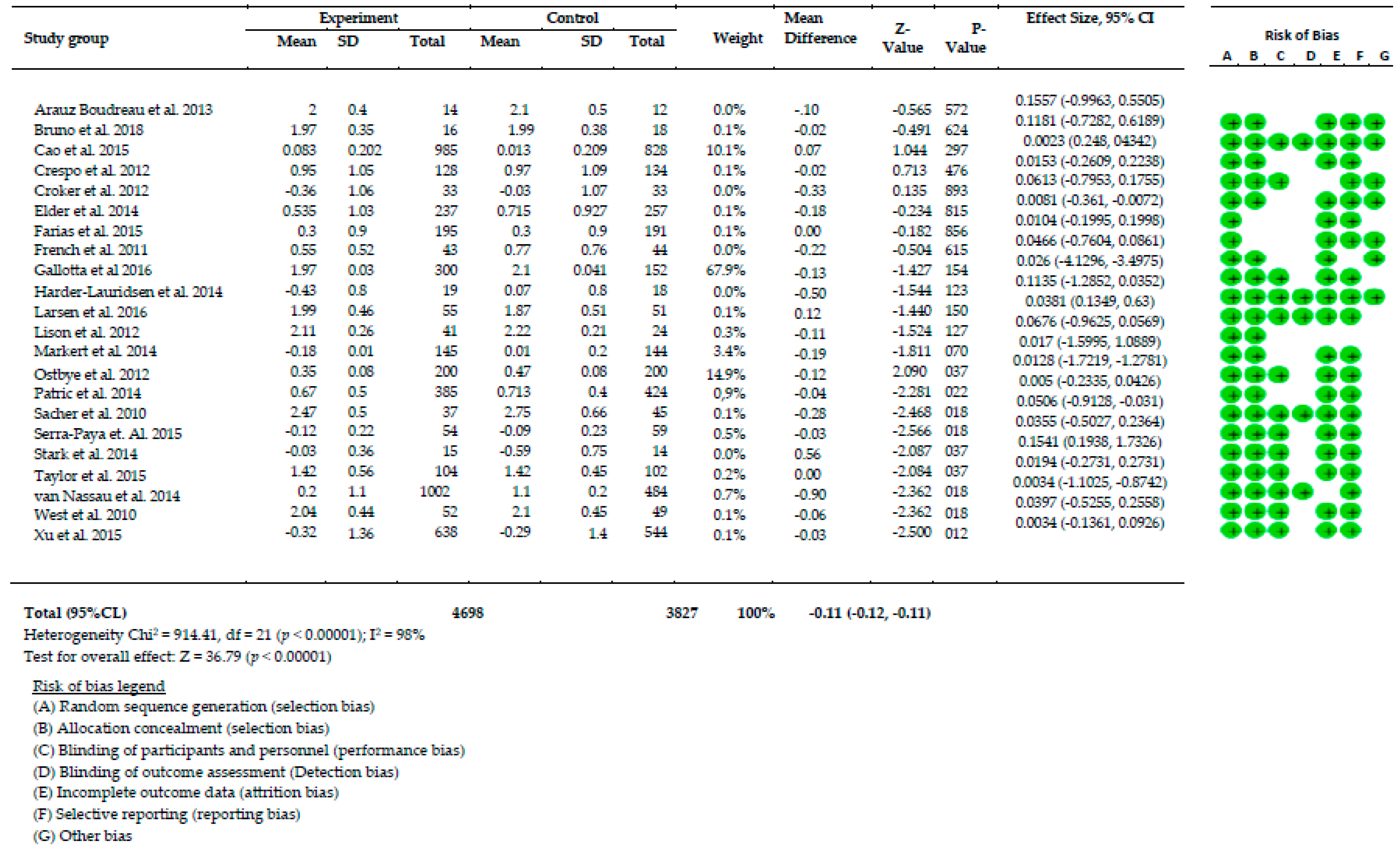
4.2. Controlling Risk of Bias
4.3. Home-Based Intervention Features
4.3.1. Parental Involvement
4.3.2. Nutrition Strategies
4.3.3. Increased Physical Activity
4.3.4. Reduction of Sedentary Behaviors
4.4. Effectiveness of Home-Based Interventions on Health Outcomes
4.4.1. Body Weight
4.4.2. Healthy Eating Behaviors
4.4.3. Physical Activity and Sedentary Lifestyle
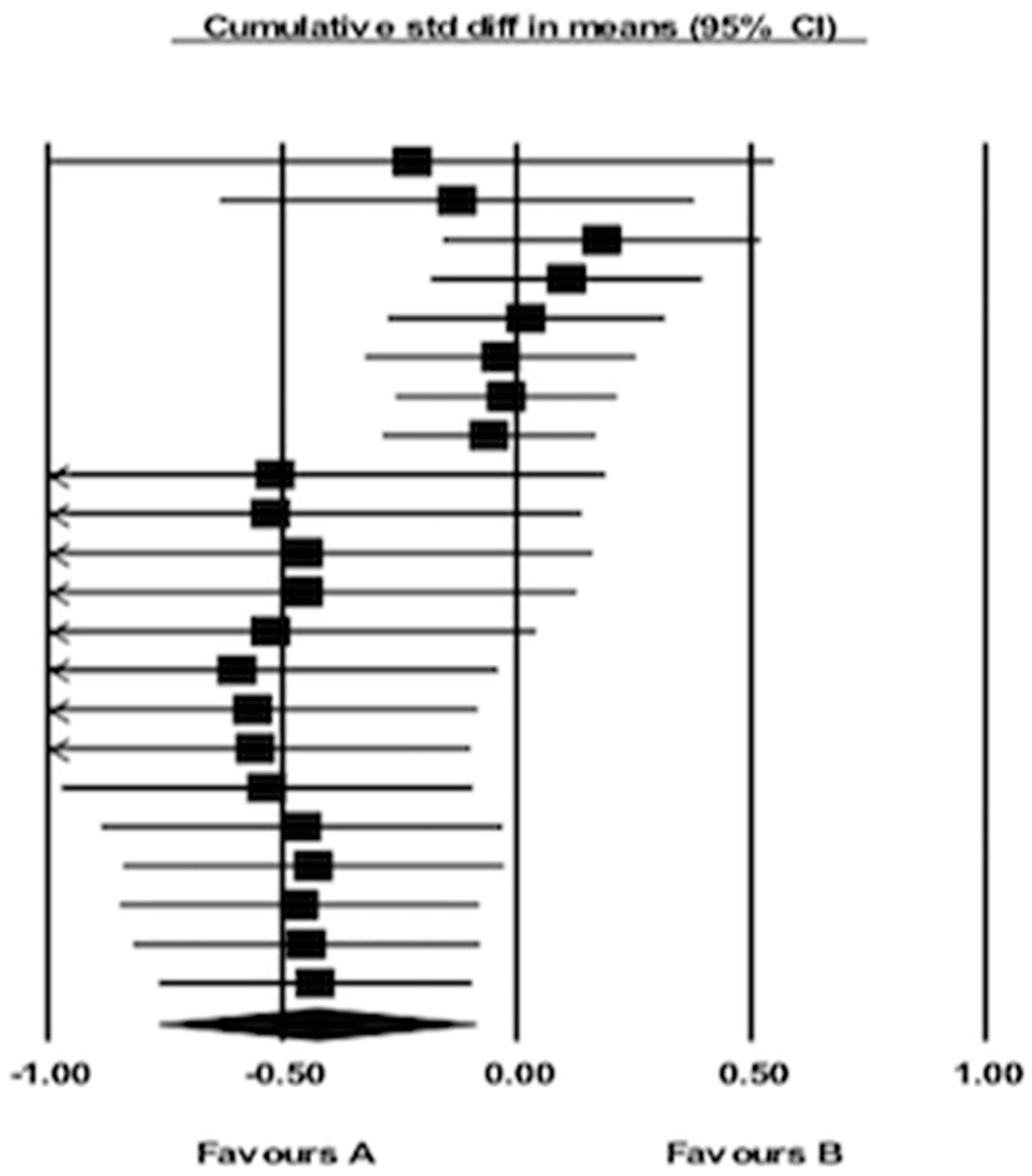
4.5. Summary of Effects Analysis of Interventions
5. Discussion
6. Strengths and Limitations
7. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Appendix A
| Author, Year | Target Group Intervention | Focused Activities | Home-based Program | Instrument | Outcomes | ||
|---|---|---|---|---|---|---|---|
| (DB) | (PA) | (SB) | |||||
| Araus Boudreau, 2013 [15] | Both the child and parents | * | * | * | Power up classes including
|
|
|
| Bruno, 2018 [22] | Both the child and parents | * | * |
|
|
| |
| Cao, 2015 [23] | Both the child and parents | * | * |
|
|
| |
| Crespo, 2012 [40] | Both the child and parents | * | * | * |
|
|
|
| Croker, 2012 [11] | Both the child and parents | * | * |
|
|
| |
| Elder, 2014 [24] | Both the child and parents | * | * | * |
|
|
|
| Farias, 2015 [32] | Child-only | * |
|
|
| ||
| French, 2011 [12] | Parents only | * | * | * |
|
|
|
| Gallota, 2016 [25] | Both the child and parents | * | * | * | Healthy Nutrition Intervention
|
|
|
| Hander-Lauridsen, 2014 [36] | Both the child and parents | * |
|
|
| ||
| Larsen, 2016 [31] | Both the child and parents | * | * |
|
|
| |
| Lison, 2012 [30] | Both the child and parents | * |
|
|
| ||
| Markert, 2014 [37] | Both the child and parents | * | * | * |
|
|
|
| Østbye, 2012 [10] | Both the child and parents | * | * | * |
|
|
|
| Patric, 2013 [38] | Both the child and parents | * | * | The intervention group received interventions including
|
|
| |
| Sacher, 2010 [17] | Both the child and parents | * | * |
|
|
| |
| Serra-Paya, 2015 [39] | Both the child and parents | * | * | * |
|
|
|
| Stark, 2014 [9] | Both the child and parents | * | * | Phase 1 (intensive intervention)
|
|
| |
| Taylor, 2018 [41] | Both the child and parents | * | * | Phase 1: Screening of health status and motivational interviewing for parents regarding child weight Phase 2
|
|
| |
| van Nassau, 2014 [18] | Both the child and parents | * | * | * |
|
|
|
| West, 2010 [8] | Both the child and parents | * | * | * |
|
|
|
| Xu, 2015 [26] | Both the child and parents | * | * | * |
|
|
|
References
- WHO. Taking Action on Childhood Obesity Report; WHO: Geneva, Switzwelnd, 2018. [Google Scholar]
- Reilly, J.J.; Kelly, J. Long-term impact of overweight and obesity in childhood and adolescence on morbidity and premature mortality in adulthood: Systematic review. Int. J. Obes. 2011, 35, 891–898. [Google Scholar] [CrossRef]
- Pigeot, I.; Barba, G.; Chadjigeorgiou, C.; de Henauw, S.; Kourides, Y.; Lissner, L.; Marild, S.; Pohlabeln, H.; Russo, P.; Tornaritis, M.; Veidebaum, T.; Wawro, N.; Siani, A. Prevalence and determinants of childhood overweight and obesity in European countries: Pooled analysis of the existing surveys within the IDEFICS Consortium. Int. J. Obes. 2009, 33, 1103–1110. [Google Scholar] [CrossRef][Green Version]
- Tim, L.; Boyd, S. Health Promotion to Prevent Obesity In Global Perspectives on Health Promotion Effectiveness; McQueen, D.V., Jones, C.M., Eds.; Springer: New York, NY, USA, 2007. [Google Scholar]
- Kreb, N.F.; Jacobson, M.S.; American Academy of Pediatrics Committee on Nutrition. Prevention of Pediatric Overweight and Obesity. Pediatrics 2003, 112, 422. [Google Scholar]
- Mulrin, H. Interventions to Prevent Childhood Obesity Literature Review; Canterbury District Health Board: Christchurch, New Zealand, 2013. [Google Scholar]
- Danford, C.A.; Schultz, C.; Marvicsin, D. Parental roles in the development of obesity in children: Challenges and opportunities. Res. Rep. Biol. 2015, 6, 39–53. [Google Scholar] [CrossRef]
- West, F.; Sanders, M.R.; Cleghorn, G.J.; Davies, P.S. Randomised clinical trial of a family-based lifestyle intervention for childhood obesity involving parents as the exclusive agents of change. Behav. Res. Ther. 2010, 48, 1170–1179. [Google Scholar] [CrossRef] [PubMed]
- Stark, L.J.; Clifford, L.M.; Towner, E.K.; Filigno, S.S.; Zion, C.; Bolling, C.; Rausch, J. A pilot randomized controlled trial of a behavioral family-based intervention with and without home visits to decrease obesity in preschoolers. J. Pediatr. Psychol. 2014, 39, 1001–1012. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Ostbye, T.; Krause, K.M.; Stroo, M.; Lovelady, C.A.; Evenson, K.R.; Peterson, B.L.; Bastian, L.A.; Swamy, G.K.; West, D.G.; Brouwer, R.J.; Zucker, N.L. Parent-focused change to prevent obesity in preschoolers: Results from the KAN-DO study. Prev. Med. 2012, 55, 188–195. [Google Scholar] [CrossRef]
- Croker, H.; Viner, R.M.; Nicholls, D.; Haroun, D.; Chadwick, P.; Edwards, C.; Wells, J.C.; Wardle, J. Family-based behavioural treatment of childhood obesity in a UK National Health Service setting: Randomized controlled trial. Int. J. Obes. 2012, 36, 16–26. [Google Scholar] [CrossRef]
- French, S.A.; Gerlach, A.F.; Mitchell, N.R.; Hannan, P.J.; Welsh, E.M. Household obesity prevention: Take Action—A group-randomized trial. Obesity 2011, 19, 2082–2088. [Google Scholar] [CrossRef]
- Turner, L.S.L.; Altman, D.G.; Weeks, L.; Peters, J.; Kober, T.; Dias, S.; Schulz, K.F.; Plint, A.C.; Moher, D. Consolidated standards of reporting trials (CONSORT) and the completeness of reporting of randomised controlled trials (RCTs) published in medical journals. Cochrane Database Syst. Rev. 2012, 11, MR000030. [Google Scholar] [CrossRef]
- Taylor, R.W.; Cox, A.; Knight, L.; Brown, D.A.; Meredith-Jones, K.; Haszard, J.J.; Dawson, A.M.; Taylor, B.J.; Williams, S.M. A Tailored Family-Based Obesity Intervention: A Randomized Trial. Pediatrics 2015, 136, 281–289. [Google Scholar] [CrossRef]
- Arauz Boudreau, A.D.; Kurowski, D.S.; Gonzalez, W.I.; Dimond, M.A.; Oreskovic, N.M. Latino families, primary care, and childhood obesity: A randomized controlled trial. Am. J. Prev. Med. 2013, 44, S247–S257. [Google Scholar] [CrossRef]
- Gerards, S.M.; Dagnilie, P.C.; Jansen, M.W.; van der Goot, L.O.; de Vries, N.K.; Sanders, M.R.; Kremers, S.P. Lifestyle Triple P: A parenting intervention for childhood obesity. BMC Public Health. 2012, 3, 267. [Google Scholar] [CrossRef]
- Sacher, P.M.; Kolotourou, M.; Chadwick, P.M.; Cole, T.J.; Lawson, M.S.; Lucas, A.; Singhal, A. Randomized controlled trial of the MEND program: A family-based community intervention for childhood obesity. Obesity 2010, 18, S62–S68. [Google Scholar] [CrossRef]
- Van Nassau, F.S.A.; Cerin, E.; Salmon, J.; van Mechelen, W.; Brug, J.; Chinapaw, M.J.M. The Dutch Obesity Intervention in Teenagers (DOiT) cluster controlled implementation trial: Intervention effects and mediators and moderators of adiposity and energy balance-related behaviours. Int. J. Behav. Nutr. 2014, 11, 158. [Google Scholar] [CrossRef]
- Epstein, L.H.; Gordy, C.C.; Raynor, H.A.; Beddome, M.; Kilanowski, C.K.; Paluch, R. Increasing fruit and vegetable intake and decreasing fat and sugar intake in families at risk for childhood obesity. Obes. Res. 2001, 9, 171–178. [Google Scholar]
- Burrows, T.W.J.; Collins, C.E. The impact of a child obesity treatment intervention on parent child-feeding practices. Int. J. Pediatr. Obes. 2010, 5, 43–50. [Google Scholar] [CrossRef]
- Knowlden, A.P.; Sharma, M. Systematic review of family and home-based interventions targeting paediatric overweight and obesity. Obes. Rev. 2012, 13, 499–508. [Google Scholar] [CrossRef]
- Bruno, A.; Escobar, P.; Cebolla, A.; Alvarez-Pitti, J.; Guixeres, J.; Lurbe, E.; Banos, R.; Lison, J.F. Home-exercise Childhood Obesity Intervention: A Randomized Clinical Trial Comparing Print Versus Web-based (Move It) Platforms. J. Pediatr. Nurs. 2018, 42, e79–e84. [Google Scholar] [CrossRef]
- Cao, Z.J.; Wang, S.M.; Chen, Y. A randomized trial of multiple interventions for childhood obesity in China. Am. J. Prev. Med. 2015, 48, 552–560. [Google Scholar] [CrossRef]
- Elder, J.P.; Crespo, N.C.; Corder, K.; Ayala, G.X.; Slymen, D.J.; Lopez, N.V.; Moody, J.S.; McKenzie, T.L. Childhood obesity prevention and control in city recreation centres and family homes: The MOVE/me Muevo Project. Pediatric Obes. 2014, 9, 218–231. [Google Scholar] [CrossRef]
- Gallotta, M.C.; Iazzoni, S.; Emerenziani, G.P.; Meucci, M.; Migliaccio, S.; Guidetti, L.; Baldari, C. Effects of combined physical education and nutritional programs on schoolchildren’s healthy habits. PeerJ 2016, 4, e1880. [Google Scholar] [CrossRef]
- Xu, F.; Ware, R.S.; Leslie, E.; Tse, L.A.; Wang, Z.; Li, J.; Wang, Y. Effectiveness of a Randomized Controlled Lifestyle Intervention to Prevent Obesity among Chinese Primary School Students: CLICK-Obesity Study. PLoS ONE 2015, 10, e0141421. [Google Scholar] [CrossRef]
- Colley, R.C.; Brownrigg, M.; Tremblay, M.S. A model of knowledge translation in health: The Active Healthy Kids Canada Report Card on physical activity for children and youth. Health Promot. Pract. 2012, 13, 320–330. [Google Scholar] [CrossRef] [PubMed]
- Gruber, K.J.; Haldeman, L. Using the family to combat childhood and adult obesity. Prev. Chronic. Dis. 2009, 6, A106. [Google Scholar] [PubMed]
- Spear, B.A.; Barlow, S.E.; Ervin, C.; Ludwig, D.S.; Saelens, B.E.; Schetzina, K.E.; Taveras, E.M. Recommendations for treatment of child and adolescent overweight and obesity. Pediatrics 2007, 120 (Suppl. 4), S254–S288. [Google Scholar] [CrossRef]
- Lison, J.F.; Real-Montes, J.M.; Torro, I.; Arguisuelas, M.D.; Alvarez-Pitti, J.; Martinez-Gramage, J.; Aguilar, F.; Lurbe, E. Exercise intervention in childhood obesity: A randomized controlled trial comparing hospital-versus home-based groups. Acad. Pediatrics 2012, 12, 319–325. [Google Scholar] [CrossRef]
- Larsen, K.T.; Huang, T.; Ried-Larsen, M.; Andersen, L.B.; Heidemann, M.; Moller, N.C. A Multi-Component Day-Camp Weight-Loss Program Is Effective in Reducing BMI in Children after One Year: A Randomized Controlled Trial. PLoS ONE 2016, 11, e0157182. [Google Scholar] [CrossRef]
- Farias Edos, S.; Goncalves, E.M.; Morcillo, A.M.; Guerra-Junior, G.; Amancio, O.M. Effects of programmed physical activity on body composition in post-pubertal schoolchildren. J. Pediatr. 2015, 91, 122–129. [Google Scholar] [CrossRef]
- Baranowski, T.T.D.; Buday, R.; Lu, A.S.; Baranowski, J. Design of Video Games for Children’s Diet and Physical Activity Behavior Change. Int. J. Comput. Sci. Sport. 2010, 9, 3–17. [Google Scholar] [PubMed]
- Atkin, A.J.; Gorely, T.; Clemes, S.A.; Yates, T.; Edwardson, C.; Brage, S.; Salmon, J.; Marshall, S.J.; Biddle, S.J. Methods of Measurement in epidemiology: Sedentary Behaviour. Int. J. Epidemiol. 2012, 41, 1460–1471. [Google Scholar] [CrossRef]
- American Academic of Paediatrics. American Academy of Pediatrics: Children, adolescents, and television. Paediatrics 2001, 107, 423–426. [Google Scholar] [CrossRef]
- Harder-Lauridsen, N.M.; Birk, N.M.; Ried-Larsen, M.; Juul, A.; Andersen, L.B.; Pedersen, B.K.; Krogh-Madsen, R. A randomized controlled trial on a multicomponent intervention for overweight school-aged children—Copenhagen, Denmark. BMC Pediatr. 2014, 14, 273. [Google Scholar] [CrossRef] [PubMed]
- Markert, J.; Herget, S.; Petroff, D.; Gausche, R.; Grimm, A.; Kiess, W.; Bluher, S. Telephone-based adiposity prevention for families with overweight children (T.A.F.F.-Study): One year outcome of a randomized, controlled trial. Int. J. Environ. Res. Public Health 2014, 11, 10327–10344. [Google Scholar] [CrossRef] [PubMed]
- Patrick, K.; Norman, G.J.; Davila, E.P.; Rosenberg, D.E.; Calfas, K.J.; Covin, J.; Sallis, J.F. Two-Year Outcomes of a Primary Care–and Home-Based Intervention for Physical Activity, Sedentary Behavior, and Diet in Adolescents. ICAN Infant Child Adolesc. Nutr. 2013, 6, 44–51. [Google Scholar] [CrossRef][Green Version]
- Serra-Paya, N.; Ensenyat, A.; Castro-Vinuales, I.; Real, J.; Sinfreu-Bergues, X.; Zapata, A.; Mur, J.M.; Galindo-Ortego, G.; Sole-Mir, E.; Teixido, C. Effectiveness of a Multi-Component Intervention for Overweight and Obese Children (Nereu Program): A Randomized Controlled Trial. PLoS ONE 2015, 10, e0144502. [Google Scholar] [CrossRef]
- Crespo, N.C.; Elder, J.P.; Ayala, G.X.; Slymen, D.J.; Campbell, N.R.; Sallis, J.F.; McKenzie, T.L.; Baquero, B.; Arredondo, E.M. Results of a multi-level intervention to prevent and control childhood obesity among Latino children: The Aventuras Para Ninos Study. Ann. Behav. Med. A Publ. Soc. Behav. Med. 2012, 43, 84–100. [Google Scholar] [CrossRef] [PubMed]
- Taylor, S.F.Y.; Solomon, S. Factors affecting the self-monitoring of blood glucose levels in Aboriginal patients: Findings from a remote community. Aust. Indig. Health 2017, 17, 1–7. [Google Scholar]
- Ash, T.; Agaronov, A.; Young, T.; Aftosmes-Tobio, A.; Davison, K.K. Family-based childhood obesity prevention interventions: A systematic review and quantitative content analysis. Int. J. Behav. Nutr. Phys. Act. 2017, 14, 113. [Google Scholar] [CrossRef] [PubMed]
- Berge, J.M.; Everts, J.C. Family-Based Interventions Targeting Childhood Obesity: A Meta-Analysis. Child. Obes. 2011, 7, 110–121. [Google Scholar] [CrossRef]
- Bleich, S.N.; Vercammen, K.A.; Zatz, L.Y.; Frelier, J.M.; Ebbeling, C.B.; Peeters, A. Interventions to prevent global childhood overweight and obesity: A systematic review. Lancet Diabetes Endocrinol. 2018, 6, 332–346. [Google Scholar] [CrossRef]
- Showell, N.N.; Fawole, O.; Segal, J.; Wilson, R.F.; Cheskin, L.J.; Bleich, S.N.; Wu, L.; Lau, B.; Wang, Y. A systematic review of home-based childhood obesity prevention studies. Pediatrics 2013, 132, e193–e200. [Google Scholar] [CrossRef] [PubMed]
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pamungkas, R.A.; Chamroonsawasdi, K. Home-Based Interventions to Treat and Prevent Childhood Obesity: A Systematic Review and Meta-Analysis. Behav. Sci. 2019, 9, 38. https://doi.org/10.3390/bs9040038
Pamungkas RA, Chamroonsawasdi K. Home-Based Interventions to Treat and Prevent Childhood Obesity: A Systematic Review and Meta-Analysis. Behavioral Sciences. 2019; 9(4):38. https://doi.org/10.3390/bs9040038
Chicago/Turabian StylePamungkas, Rian Adi, and Kanittha Chamroonsawasdi. 2019. "Home-Based Interventions to Treat and Prevent Childhood Obesity: A Systematic Review and Meta-Analysis" Behavioral Sciences 9, no. 4: 38. https://doi.org/10.3390/bs9040038
APA StylePamungkas, R. A., & Chamroonsawasdi, K. (2019). Home-Based Interventions to Treat and Prevent Childhood Obesity: A Systematic Review and Meta-Analysis. Behavioral Sciences, 9(4), 38. https://doi.org/10.3390/bs9040038





