Abstract
Purpose: Although the protective effect of social support against depression is well known, limited information exists on racial differences in this association. The current study examined Black-White differences in the effects of religious and secular emotional social support on depressive symptoms in a national sample of older adults in the United States. Methods: With a longitudinal prospective design, the Religion, Aging and Health Survey, 2001–2004, followed 1493 Black (n = 734) and White (n = 759) elderly individuals (age 66 and older) for three years. Race, demographics (age and gender), socio-economics (education and marital status) and frequency of church attendance were measured at baseline in 2001. Secular social support, religious social support, chronic medical conditions and depressive symptoms [8- item Center for Epidemiological Studies-Depression scale (CES-D)] were measured in 2004. Multiple linear regression models were used for data analysis. Results: In the pooled sample, secular and religious social support were both protective against depressive symptoms, net of all covariates. Race interacted with secular (β = −0.62 for interaction) and religious (β = −0.21 for interaction) social support on baseline depressive symptoms (p < 0.05 for both interactions), suggesting larger protections for Blacks compared to Whites. In race-specific models, the regression weight for the effect of secular social support on depressive symptoms was larger for Blacks (β = −0.64) than Whites (β = −0.16). Conclusion: We found Black—White differences in the protective effects of secular and religious social support against depressive symptoms. Blacks seem to benefit more from the same level of emotional social support, regardless of its source, compared to Whites.
1. Introduction
Paradoxically, despite being more frequently exposed to a wide range of stressors, Blacks have a lower risk of depression compared to Whites [1,2,3,4,5,6,7,8,9,10,11,12,13]. Also known as the Black-White mental health paradox, this phenomenon is one of the mysteries of racial and ethnic mental health research in the United States [4,5,6,7,8,14]. Many researchers have tried to find possible explanations for this paradox. Keyes has suggested that Blacks may experience psychological growth and flourishing due to social and economic adversities [4].
Built on differential effects hypothesis [15,16], we have shown that Blacks and Whites differently gain health from the economic resources that become available to them [16,17]. In this view, Blacks gain less from economic resources that have not been available to them for decades [18,19,20,21,22]. In contrast, Blacks may have turned to non-economic resources that they could freely mobilize, to compensate lack of economic resources [23]. Among freely available resources to Blacks, even from the time of slavery, has been religion and religious social support [24]. In this view, not only Blacks are more religious than Whites, they have better learned to mobilize it to cope with stress and adversity [25,26].
In their landmark review paper in 1998, Ellison and Levin proposed several mechanisms to explain the effect of religion on health [27]. Central to their explanation was social support that could be used to buffer stress. Several other studies. This is also in line with other theoretical [28] and empirical [29,30,31] work on the protective effects of religious social support on health. Neal Krause has documented extensive evidence showing that social support is a main mechanism that explains the protective effects of religion on health [32,33,34]. Taylor and Chatters have also documented supportive relations in the church setting in the lives of Blacks [35,36,37,38,39]. Cohen’s social support theory also emphasizes [40], Protective effects of social support. These effects, however, vary across racial groups [25,26,41,42].
One potential explanation for this paradox is a higher availability and a higher efficacy of positive psychosocial and cognitive resources such as social support, family relations and religion in the life of Blacks compared to Whites [4,5,6,7,8]. For instance, Mouzen has used data from the National Survey of American Life (n = 4086) to examine whether family and religion explain the better mental health of Blacks, despite higher levels of adversities [7,8]. She, however, has found few race differences in the quantity and quality of friendships, fictive kinships and family relationships and such differences did not explain the race paradox in mental health [7,8].
In a series of attempts to understand the Black-White mental health paradox, we have documented major racial differences in the psychosocial and medical correlates of depression and depressive symptoms [5,43,44,45,46,47,48,49]. For instance, in two studies, depressive symptoms predicted mortality of Whites but not Blacks [50,51]. In other studies, depressive symptoms and negative affect predicted an increase in chronic medical conditions of Whites but not Blacks [6,52,53]. Baseline level of depressive symptoms was also found to predict subsequent risk of major depressive symptoms (MDD) among Whites but not Blacks [54]. Weaker effects of psychosocial risk factors on physical health outcomes in Blacks compared to Whites were not limited to depressive symptoms and were replicated for education, perceived control over life and self-rated health [6,18,40,50,52,53,54,55,56,57]. These patterns are indicative of a systemic resilience among Blacks [4,5].
One potential hypothesis that may explain the weaker effects of risk factors on Blacks is a higher availability of social support and religion [7,8,25,41]. In this view, social support and religiosity are not only more commonly found among Blacks, they are also more effective among them [41,42], making Blacks more resilient to the harmful effects of social and economic adversities compared to Whites.
In 2013, we analyzed data from National Survey of American Life (NSAL) and showed that religious social support fully mediated the association between church attendance and life satisfaction for Blacks but not Whites. Authors concluded that religious social support may have more health benefits for Blacks compared to Whites [25]. On a nationwide sample of older adults, Krause documented stress-buffering effects of church-based support for Blacks but not Whites [42]. Lincoln, Chatters and Taylor conducted a secondary analysis of the National Comorbidity Survey (NCS) and found stronger protective effects of social support against psychological distress in Blacks compared to Whites [41]. All these studies are indicative of Blacks’ faith advantage in health [26].
We conducted this study to compare Black and White older adults for the effects of secular and religious emotional social support on depressive symptoms in the United States. In line with previous studies [25,41,42], we hypothesized stronger protective effects of religious and secular social support against depressive symptoms in Black than White older Americans.
2. Methods
2.1. Design, Setting and Sampling
The Religion, Aging and Health Survey, 2001–2004, is a national household longitudinal study of Black and White older adults in the United States [58,59]. The study participants were 1500 older adults who were either White or Black older adults. The study only sampled non-institutionalized English speaking Americans with more than 65 years of age. Participants were either Christians or individuals who were not associated with any faith. The study oversampled older Blacks [58,59]. As a result, older Blacks represented half of the sample. The overall response rate for the baseline interviews was 62%. Geographically, the study population was restricted to all eligible persons residing in the coterminous United States (i.e., residents of Alaska and Hawaii were excluded). The sampling frame of this study consisted of all eligible persons contained in the Health Care Finance Administration (HCFA) Medicare Beneficiary Eligibility List, currently called the Center for Medicare and Medicaid Services (CMMS). This list contains the name, gender and race of older individuals in the United States [58,59].
2.2. Measures
Age, gender, race, education and religious involvement were measured at baseline in 2001. Secular emotional social support, religious emotional social support, number of chronic medical conditions (12 chronic medical conditions), self-rated health (SRH) and depressive symptoms were measured in 2004.
Depressive symptoms. Depressive symptoms were measured using the 8–item Center for Epidemiological Studies-Depression scale (CES-D) scale [60], which were administered both in 2001 and 2004. The measure included items to capture two domains of depression: negative emotions and somatic symptoms. This abbreviated CES-D measure has shown acceptable reliability and validity [61,62,63]. Some examples of the items included (1) I felt depressed; (2) I felt sad; and (3) I could not get going. Item responses were on a four Likert scale, ranging from 1 (“Rarely or none”) to 4 (“most or all of the time”). A mean score was calculated. Depressive score, with a potential range from 1 to 4, was treated as a continuous measure. Higher scores were indicative of more severe depressive symptoms [64,65].
Frequency of Church Attendance. Frequency of church attendance was measured in 2001 (Wave 1) using the following item: How often do you attend religious services? Responses were never (1); less than once a year (2); about once or twice a year (3); several times a year (4); about once a month (5); 2–3 times a month (6); nearly every week (7); every week (8); and several times a week (9) [66].
Religious Social Support. We measured religious emotional social support at Wave 2 with a 3–item measure developed by Krause (2002) [66,67]. The items included: (1) “Not counting your minister, pastor, or priest, how often does someone in your congregation let you know they love and care for you?”; (2) “How often does someone in your congregation talk with you about your private problems and concerns?”; and (3) “How often does someone in your congregation express interest and concern in your well-being?” These items were scored as follows: (1) never; (2) once in a while; (3) fairly often; and (4) very often. Authors calculated a mean score, ranging from 1 to 4, where a higher score on the scale indicates receiving more spiritual support from fellow church members. The reliability is high with a Cronbach’s alpha of 0.825 [68].
Secular Social Support. We used a 3–item measure developed by Krause (2002) to evaluate participants’ received emotional support from people outside of their congregations [67]. Items included: (1) “Not counting your minister or fellow church members, how often do your family and friends let you know they love and care for you”?; (2) “Not counting your minister or fellow church members, how often do your family and friends talk with you about your private problems and concerns?”; and (3) “Not counting your minister or fellow church members, how often do your family and friends express interest and concern in your well-being?.” These item responses were as follow: (1) never; (2) once in a while; (3) fairly often; and (4) very often. We computed the mean score as the total score, ranging from 1 to 4, with a higher score denoting more frequent secular emotional support. The measure had acceptable reliability with a Cronbach alpha estimate of 0.786 [68].
Chronic Medical Conditions. The presence of the following chronic medical conditions during the past 12 months was measured during Wave 2 in 2004: (1) hypertension; (2) heart problems; (3) diabetes; (4) cancer; (5) renal disease; (6) arthritis; (7) gastrointestinal disease; (8) chronic liver disease; (9) urinary tract disorders; (10) ophthalmological diseases; (11) respiratory conditions; and (12) other chronic health problems. Number of conditions potentially ranged between 0 and 12, with a higher score reflecting higher number of conditions [14].
2.3. Statistical Analysis
SPSS 22.0 for Windows (IBM Inc. Armonk, NY, USA) was used for data analysis. Multiple linear regression models were estimated in the pooled sample as well as specific to race. In all models, frequency of depressive symptoms was the dependent variable. We ran separate models with church attendance, religious social support and secular social support as independent variables. Model 1 was conducted in the pooled sample and only included the main effects, without the interaction term. Model 2 was tested in the pooled sample but also included the interaction term between race and the predictor of interest. Model 3 and Model 4 were specific to Whites (Model 3) and Blacks (Model 4). In all models, demographics, socio-economics and physical health were covariates. Race was the focal moderator. Standardized Beta with p values were reported. We considered p less than 0.05 as significant. Less than 5% of the data had a missing value.
2.4. Ethics
All participants provided written informed consent. All data were collected anonymously. The University of Michigan Institutional Review Board (IRB) approved the study protocol.
3. Results
The study followed 1493 older adults who were either Black (n = 734) or White (n = 759) (age 65 or older) for three years. Table 1 summarizes the descriptive statistics in the overall sample and also by race. Average age was similar across racial groups, whereas Blacks were more often female, had lower education and were less frequently married. Blacks more frequently attended church and reported higher secular and religious emotional social support, yet reported feeling more depressed (Table 1).

Table 1.
Descriptive Statistics for the analytic sample, stratified by race and overall.
Table 2 shows a summary of four linear regression models in the pooled sample with (Model 1) and without (Model 2) interactions terms and also in Whites (Model 3) and Blacks (Model 4). High church attendance showed a protective effect against depressive symptoms in the pooled sample (Model 1) and race did not interact with the church attendance on depressive symptoms (Model 2). Model 3 and Model 4 also shows that church attendance protects both Whites and Blacks against depressive symptoms (Table 2).

Table 2.
Effects of church attendance on depressive symptoms based on race in older adults using linear regressions.
Table 3 summarizes four linear regressions that show higher levels of religious social support is associated with lower levels of depressive symptoms, net of all covariates in the pooled sample (Model 1). A significant interaction was found between race and religious social support, suggesting larger effects for Blacks compared to Whites (Model 2). These interactions were significant, net of all covariates. Model 3 and Model 4 also showed that religious social support protects Whites and Blacks against depressive symptoms (Table 3).

Table 3.
Effects of religious social support on depressive symptoms based on race in older adults using linear regressions.
Table 4 provides a summary of the effects of secular social support on depressive symptoms among Blacks and Whites net of covariates. Higher levels of secular social support were associated with lower levels of depressive symptoms in the pooled sample (Model 1) and we found an interaction between race and secular social support, suggesting larger effects for Blacks compared to Whites (Model 2). Although significant for Whites (Model 3) and Blacks (Model 4), the regression coefficient for the effect of secular social support on depressive symptoms was larger for Blacks (B = −0.64) compared to Whites (B = −0.16) (Table 4, Figure 1).

Table 4.
Effects of secular social support on depressive symptoms based on race in older adults using linear regressions.
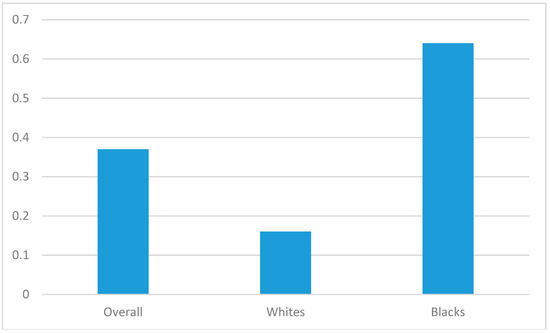
Figure 1.
Protective effect of secular social support overall and by race. (Numbers are standardized regression coefficients for the effects of social support on depressive symptoms).
4. Discussion
Our first finding suggests that church attendance, secular social support, as well as religious social support, were all protective against depressive symptoms among older adults. Our second finding showed Black—White differences in the effects of secular and religious social support on depressive symptoms, with Blacks benefiting more from the same level of emotional social support, regardless of its source, compared to Whites. Black and White older adults, however, did not differ in the protective effect of church attendance on depressive symptoms.
Our first finding in the pooled sample is in line with previous theoretical and empirical work. There are at least three theoretical perspectives on the health effects of social support: (1) the stress and coping perspective; (2) the social constructionist perspective; and (3) the relationship perspective. These models suggest that either directly, or through buffering the effects of stressors, via enhancing coping abilities, social support protects people against poor mental health including depression. Social support promotes self-esteem and self-regulation and coping and reduces perceived stress [69].
Our second result regarding the interaction between race and support on depressive symptoms is in harmony with previous findings by our team [25], Lincoln et al., [41] and Krause [70] on racial differences in mental health benefits associated with social support in the church setting. All of these studies have suggested that Blacks gain more health benefits from religion, compared to Whites [70]. Skarupski has called this phenomenon Blacks’ faith advantage in health [26]. Blacks and Whites have different transactions in their social networks inside and outside church settings [71,72,73,74] which may be in part due to their different network composition [74,75]. Our findings may be due to racial and ethnic differences in the organization and programmatic emphases of religious services and churches that have major implications for the religion–health link across racial groups [25,41]. Patterns and contents of religious activities differ for Blacks and Whites [76]. The structure and mission of church also differs for Blacks and Whites [77]. Such differences may result in stronger associations between emotional support in the context of religion and health outcomes [2,78]. Our finding is, however, does not support a stronger effect of social network on health of Whites compared to Blacks [79].
Self-construals may also help us understand our findings. Blacks and other minority groups have higher value orientations that are supportive of familyism, collectivism and interdependence. Higher interconnected cultural beliefs may result in a higher susceptibility of Blacks to the effects of social support [80]. Self-construals shape individuals’ approaches to their environment, including social ties [81]. In fact, interdependent or communal cultural systems support a sense of harmony control via establishing social networks of loyalty and support [82,83]. Blacks, who may have higher collectivistic attitudes, may place a higher priority on fostering social harmony; they may prefer to maintain relationships with others rather than control the situation, which may result in higher wellbeing [81]. These traits also shape how the individual maintains harmony, sense of control and coping skills; how the individual interacts with the contextual, social, or spiritual forces; and how the individual attempts to merge with or distinct from these forces [82,84]. Blacks who are from more communal or interdependent cultures, often value interpersonal relationships and have a higher tendency to see others as a part of the self. Whites are more often from cultures that endorse more independent attitudes and value uniqueness and distinction of self from others [81].
We found differential effects of social support for Blacks and Whites. As Lincoln et al. [41] argued in 2003, social factors operate differently across racial groups. They also mentioned that particular psychosocial constructs may have differential salience across race and ethnic groups. In addition, social and psychological processes may operate in unique ways for some racial and ethnic groups [41]. There is a need to study how racial groups differ in psychosocial processes that shape health and illness [41,85,86,87]. Failure to account for the unique population specific cultural factors that accompany the life circumstances of diverse racial group may result in biased findings. Researchers should not always assume that the same social theories and models similarly explain outcomes across diverse racial or ethnic groups [41]. Each racial or ethnic group may benefit or be vulnerable to specific set of risk and protective factors [41]. This is the argument behind the differential effects hypothesis [15]. Understanding nuances of the association between social support and depression is important for mental health promotion of populations. Low social support typically leads to the development or worsening of depression [88]. The findings of this study are in line with the literature on the protective effects of positive social relationships on physical and mental health [89,90,91,92]. The support individuals receive from others [91], the quality and quantity of their social interactions [93] and their feelings of isolation and loneliness [94] have major implications for their health and wellbeing [69,95].
Higher tendency for Blacks to receive social support from fellow church members is possibly due to scarcity of economic resources in their lives [16,17]. In response, Black communities have been historically seeking resilience in Black church [96]. As argued by Nelsen and Nelsen, in 1975, as a result of centuries of racism, slavery, prejudice and discrimination, church has become the center of the Black community [97]. Blacks have turned to the church primarily because for decades as Black church was almost the only institution that was built, funded and wholly owned by them. For Blacks, church has become more than a place of worship; it has also become a social institution for interchange of social services. Given the central role of church for Blacks, supportive social relationships with the fellow church members should be expected to have a stronger effect for Blacks than Whites 705. It has been suggested that church, as a social and religious body, serves as an ‘extended family’ for Blacks. Many Blacks who face adversities in daily life exchange support with their kin in church [98].
Stronger effects of secular and religious emotional social support on depressive symptoms in Blacks compared to Whites may explain the weaker health effects of psychical risk factors such as depressive symptoms, self-rated health and hostility on mortality risk for Blacks compared to Whites [50,55,56,57,73,74,99]. These studies have suggested that regardless of the type of predictor, psychological variables better predict physical health outcomes for Whites than Blacks [55,57,100]. The authors suggest that psychosocial resources may have stronger effects on depressive symptoms for Blacks compared to Whites.
Major race differences exist in the complex associations between psychosocial resources such as socioeconomic status (SES), social support, stress, depression and physical health [43,44,51,56,101,102,103,104,105,106,107]. For instance, race and ethnicity modify the effects of SES resources on mortality [18,53,101,102]. Similarly, race alters how depression is linked to obesity [43,44,104,105], self-rated health [6,45,50], chronic medical conditions [14,46,52] and mortality [50,51]. Such race differences may be a consequence of racial differences in the distribution of psychosocial risk and protective factors, or race differences in susceptibilities or vulnerabilities to the effect of risk and protective factors [50,55,56,57]. In the latter view, race may play a major contextual role in shaping vulnerability to the effects of resources such as SES and social support on physical or mental health [18,45,48,104,108,109,110,111,112], in an adaptive response to racism.
Limitations
Our study has several limitations. First, we studied depressive symptoms rather than major depressive disorder diagnosed by a clinician, nor did we include the use of anti-depressant medications by the participants as an outcome. Second, we cannot rule out the possibility that psychosocial constructs may not reflect the same aspects across populations [56,108]. Third, we did not control for a number of potential confounders including fatigue, daily activity, cognitive ability and access to the health care system. Fourth, this study exclusively focused on emotional social support and did not include other types of social support. In 1985, House & Kahn differentiated emotional social support from other instrumental and informational support [90]. Instrumental support involves the provision of material aid, whereas informational support refers to the provision of relevant information intended and emotional support involves providing empathy, caring, reassurance and trust [90]. Social support can be seen as flow of psychological and material resources in social network, which is commonly with the intention to benefit members of the social network [95]. We did not control for church attendance because this could be a case of over-adjustment or un-necessary adjustment [113,114]. Future research is needed to explore racial and ethnic differences in the effects of other types of social support on health. Despite the above limitations, using a national sample of older American adults was a strength of this study. Another strength of this study was that we controlled for chronic medical conditions, which may confound the link between social support and depression [5,6,47,48,50,109,115]. The results reported here may also have implications for the reducing racial gaps in treatment of depression in the United States, which has been a challenge for decades [116,117].
5. Conclusions
To conclude, Black and White older adults differ in their susceptibility to the protective effects of secular and religious social support against depressive symptoms. Differential access and susceptibility to social support may be a mechanism behind the Black—White health paradox in the United States.
Author Contributions
S.A. designed and analyzed this work and contributed to draft and revision. M.M.L. drafted and revised the paper. Both authors confirmed the last version.
Funding
The Religion, Aging and Health Survey was supported by National Institute on Aging (PI: Neal Krause). The NIH Public Access Policy requires that peer-reviewed research publications generated with NIH support are made available to the public through PubMed Central. NIH is not responsible for the data collection or analyses represented in this article. Data was accessed through The Interuniversity Consortium for Political and Social Research (ICPSR), at the Institute of Social Research, University of Michigan.
Acknowledgments
S.A. is supported by the Heinz C. Prechter Bipolar Research Fund and the Richard Tam Foundation at the University of Michigan Depression Center.
Conflicts of Interest
Shervin Assari and Maryam Moghani Lankarani declare they have no conflicts of interest.
Ethics
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) with the Helsinki Declaration of 1975, as revised in 2000. Informed consent was obtained from all participants included in the study. University of Michigan Institutional review board (IRB) approved the study protocol.
References
- González, H.M.; Tarraf, W.; Whitfield, K.E.; Vega, W.A. The epidemiology of major depression and ethnicity in the United States. J. Psychol. Res. 2010, 44, 1043–1051. [Google Scholar] [CrossRef] [PubMed]
- Williams, D.R.; González, H.M.; Neighbors, H.; Nesse, R.; Abelson, J.M.; Sweetman, J.; Jackson, J.S. Prevalence and distribution of major depressive disorder in African Americans, Caribbean Blacks and Non-Hispanic Whites: Results from the National Survey of American Life. Arch. Gen. Psychiatr. 2007, 64, 305–315. [Google Scholar] [CrossRef] [PubMed]
- Owen, W.F., Jr. Racial differences in incidence, outcome and quality of life for African-Americans on hemodialysis. Blood Purif. 1996, 14, 278–285. [Google Scholar] [CrossRef] [PubMed]
- Keyes, C.L. The Black–White paradox in health: Flourishing in the face of social inequality and discrimination. J. Pers. 2009, 77, 1677–1706. [Google Scholar] [CrossRef] [PubMed]
- Barnes, D.M.; Keyes, K.M.; Bates, L.M. Racial differences in depression in the United States: How do subgroup analyses inform a paradox? Soc. Psychiatry Psychiatr. Epidemiol. 2013, 48, 1941–1949. [Google Scholar] [CrossRef] [PubMed]
- Assari, S.; Zivin, K.; Burgard, S. Long-term reciprocal associations between depressive symptoms and number of chronic medical conditions: Longitudinal support for black? White health paradox. J. Racial Ethn. Health Dispar. 2015, 2, 589–597. [Google Scholar] [CrossRef] [PubMed]
- Mouzon, D.M. Relationships of Choice: Can Friendships or Fictive Kin Explain the Race Paradox in Mental Health? Soc. Sci. Res. 2014, 44, 32–43. [Google Scholar] [CrossRef] [PubMed]
- Mouzon, D.M. Can Family Relationships Explain the Race Paradox in Mental Health? J. Marriage Fam. 2013, 75, 470–485. [Google Scholar] [CrossRef]
- Cabassa, L.J.; Humensky, J.; Druss, B.; Lewis-Fernández, R.; Gomes, A.P.; Wang, S.; Blanco, C. Do race, ethnicity and psychiatric diagnoses matter in the prevalence of multiple chronic medical conditions? Med. Care 2013, 51, 540–547. [Google Scholar] [CrossRef] [PubMed]
- Johnson-Lawrence, V.D.; Griffith, D.M.; Watkins, D.C. The effects of race, ethnicity and mood/anxiety disorders on the chronic physical health conditions of men from a national sample. Am. J. Men Health 2013, 7, 58S–67S. [Google Scholar] [CrossRef] [PubMed]
- Lindhorst, J.; Alexander, N.; Blignaut, J.; Rayner, B. Differences in hypertension between blacks and whites: An overview. Cardiovasc. J. Afr. 2007, 18, 241–247. [Google Scholar] [PubMed]
- Signorello, L.B.; Schlundt, D.G.; Cohen, S.S.; Steinwandel, M.D.; Buchowski, M.S.; McLaughlin, J.K.; Blot, W.J. Comparing diabetes prevalence between African Americans and Whites of similar socioeconomic status. Am. J. Public Health 2007, 97, 2260–2267. [Google Scholar] [CrossRef] [PubMed]
- Jackson, C.L.; Szklo, M.; Yeh, H.C.; Wang, N.Y.; Dray-Spira, R.; Thorpe, R.; Brancati, F.L. Black-white disparities in overweight and obesity trends by educational attainment in the United States, 1997–2008. J. Obes. 2013, 2013, 140743. [Google Scholar] [CrossRef] [PubMed]
- Watkins, D.C.; Assari, S.; Johnson-Lawrence, V. Race and ethnic group differences in comorbid major depressive disorder, generalized anxiety disorder and chronic medical conditions. J. Racial Ethn. Health Dispar. 2015, 2, 385–394. [Google Scholar] [CrossRef] [PubMed]
- Assari, S. Race and ethnic differences in additive and multiplicative effects of depression and anxiety on cardiovascular risk. Int. J. Prev. Med. 2016, 7, 22. [Google Scholar] [CrossRef] [PubMed]
- Assari, S. Unequal gain of equal resources across racial groups. Int. J. Health Policy Manag. 2018, 7, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Assari, S. Health disparities due to diminished return among black Americans: Public policy solutions. Soc. Issues Policy Rev. 2018, 12, 112–145. [Google Scholar] [CrossRef]
- Assari, S.; Lankarani, M.M. Race and urbanity alter the protective effect of education but not income on mortality. Front. Public Health 2016, 4, 100. [Google Scholar] [CrossRef] [PubMed]
- Assari, S. Life expectancy gain due to employment status depends on race, gender, education and their intersections. J. Racial Ethn. Health Dispar. 2018, 5, 375–386. [Google Scholar] [CrossRef] [PubMed]
- Assari, S. The Benefits of Higher Income in Protecting against Chronic Medical Conditions Are Smaller for African Americans than Whites. Healthcare 2018, 6. [Google Scholar] [CrossRef] [PubMed]
- Assari, S.; Mistry, R. Educational Attainment and Smoking Status in a National Sample of American Adults; Evidence for the Blacks’ Diminished Return. Int. J. Environ. Res. Public Health 2018, 15. [Google Scholar] [CrossRef] [PubMed]
- Assari, S.; Thomas, A.; Caldwell, C.H.; Mincy, R.B. Blacks’ diminished health return of family structure and socioeconomic status; 15 years of follow-up of a national urban sample of youth. J. Urban Health 2018, 95, 21–35. [Google Scholar] [CrossRef] [PubMed]
- Blank, M.B.; Mahmood, M.; Fox, J.C.; Guterbock, T. Alternative mental health services: The role of the Black church in the South. Am. J. Public Health 2002, 92, 1668–1672. [Google Scholar] [CrossRef] [PubMed]
- Constantine, M.G.; Lewis, E.L.; Conner, L.C.; Sanchez, D. Addressing spiritual and religious issues in counseling African Americans: Implications for counselor training and practice. Couns. Values 2000, 45, 28–38. [Google Scholar] [CrossRef]
- Assari, S. Race and Ethnicity, Religion Involvement, Church-based Social Support and Subjective Health in United States: A Case of Moderated Mediation. Int. J. Prev. Med. 2013, 4, 208–217. [Google Scholar] [PubMed]
- Skarupski, K.A.; Fitchett, G.; Evans, D.A. Mendes de Leon CF. Race differences in the association of spiritual experiences and life satisfaction in older age. Aging Ment. Health 2013, 17, 888–895. [Google Scholar] [CrossRef] [PubMed]
- Ellison, C.G.; Levin, J.S. The religion-health connection: Evidence, theory and future directions. Health Educ. Behav. 1998, 25, 700–720. [Google Scholar] [CrossRef] [PubMed]
- Koenig, H.G. Research on religion, spirituality and mental health: A review. Can. J. Psychiatry 2009, 54, 283–291. [Google Scholar] [CrossRef] [PubMed]
- Holt, C.L.; Wang, M.Q.; Clark, E.M.; Williams, B.R.; Schulz, E. Religious involvement and physical and emotional functioning among African Americans: The mediating role of religious support. Psychol. Health 2013, 28, 267–283. [Google Scholar] [CrossRef] [PubMed]
- Brownfield, D.; Sorenson, A.M. Religion and drug use among adolescents: A social support conceptualization and interpretation. Deviant Behav. 1991, 12, 259–276. [Google Scholar] [CrossRef]
- Ferraro, K.F.; Koch, J.R. Religion and health among black and white adults: Examining social support and consolation. J. Sci. Study Relig. 1994, 362–375. [Google Scholar] [CrossRef]
- Krause, N.; Ellison, C.G.; Marcum, J.P. The effects of church-based emotional support on health: Do they vary by gender? Sociol. Relig. 2002, 63, 21–47. [Google Scholar] [CrossRef]
- Krause, N. Exploring race differences in a comprehensive battery of church-based social support measures. Rev. Relig. Res. 2002, 126–149. [Google Scholar] [CrossRef]
- Krause, N.; Ellison, C.G.; Shaw, B.A.; Marcum, J.P.; Boardman, J.D. Church-based social support and religious coping. J. Sci. Study Relig. 2001, 40, 637–656. [Google Scholar] [CrossRef]
- Chatters, L.M.; Nguyen, A.W.; Taylor, R.J.; Hope, M.O. Church and family support networks and depressive symptoms among African Americans: Findings from the National Survey of American Life. J. Community Psychol. 2018, 46, 403–417. [Google Scholar] [CrossRef]
- Chatters, L.M.; Taylor, R.J.; Woodward, A.T.; Nicklett, E.J. Social support from church and family members and depressive symptoms among older African Americans. Am. J. Geriatr. Psychiatry 2015, 23, 559–567. [Google Scholar] [CrossRef] [PubMed]
- Taylor, R.J.; Chatters, L.M. Church members as a source of informal social support. Rev. Relig. Res. 1988, 193–203. [Google Scholar] [CrossRef]
- Taylor, R.J.; Chatters, L.M. Church-based informal support among elderly blacks. Gerontologist 1986, 26, 637–642. [Google Scholar] [CrossRef] [PubMed]
- Taylor, R.J.; Chatters, L.M.; Levin, J. Religion in the Lives of African Americans: Social, Psychological and Health Perspectives; Sage Publications: Thousand Oaks, CA, USA, 2003. [Google Scholar]
- Cohen, S.; Wills, T.A. Stress, social support and the buffering hypothesis. Psychol. Bull. 1985, 98, 310–357. [Google Scholar] [CrossRef] [PubMed]
- Lincoln, K.D.; Chatters, L.M.; Taylor, R.J. Psychological distress among Black and White Americans: Differential effects of social support, negative interaction and personal control. J. Health Soc. Behav. 2003, 44, 390–407. [Google Scholar] [CrossRef] [PubMed]
- Krause, N. Exploring the stress-buffering effects of church-based and secular social support on self-rated health in late life. J. Gerontol. B Psychol. Sci. Soc. Sci. 2006, 61, S35–S43. [Google Scholar] [CrossRef] [PubMed]
- Sachs-Ericsson, N.; Burns, A.B.; Gordon, K.H.; Eckel, L.A.; Wonderlich, S.A.; Crosby, R.D.; Blazer, D.G. Body mass index and depressive symptoms in older adults: The moderating roles of race, sex and socioeconomic status. Am. J. Geriatr. Psychiatry 2007, 15, 815–825. [Google Scholar] [CrossRef] [PubMed]
- Gavin, A.R.; Rue, T.; Takeuchi, D. Racial/ethnic differences in the association between obesity and major depressive disorder: Findings from the Comprehensive Psychiatric Epidemiology Surveys. Public Health Rep. 2010, 125, 698–708. [Google Scholar] [CrossRef] [PubMed]
- Assari, S. Separate and Combined Effects of Anxiety, Depression and Problem Drinking on Subjective Health among Black, Hispanic and Non-Hispanic White Men. Int. J. Prev. Med. 2014, 5, 269–279. [Google Scholar] [PubMed]
- Assari, S.; Lankarani, M.M. Race and ethnic differences in associations between cardiovascular diseases, anxiety and depression in the United States. Int. J. Travel Med. Glob. Health 2014, 2, 103–109. [Google Scholar]
- Lewis, T.T.; Guo, H.; Lunos, S.; de Leon, C.F.M.; Skarupski, K.A.; Evans, D.A.; Everson-Rose, S.A. Depressive Symptoms and Cardiovascular Mortality in Older Black and White Adults Evidence for a Differential Association by Race. Circ. Cardiovasc. Qual. Outcomes 2011, 4, 293–299. [Google Scholar] [CrossRef] [PubMed]
- Capistrant, B.D.; Gilsanz, P.; Moon, J.R.; Kosheleva, A.; Patton, K.K.; Glymour, M.M. Does the association between depressive symptoms and cardiovascular mortality risk vary by race? Evidence from the Health and Retirement Study. Ethn. Dis. 2013, 23, 155–160. [Google Scholar] [PubMed]
- Assari, S.; Sonnega, A.; Pepin, R.; Leggett, A. Residual Effects of Restless Sleep over Depressive Symptoms on Chronic Medical Conditions: Race by Gender Differences. J. Racial Ethn. Health Dispar. 2016. [Google Scholar] [CrossRef] [PubMed]
- Assari, S.; Burgard, S. Black-White differences in the effect of baseline depressive symptoms on deaths due to renal diseases: 25 year follow up of a nationally representative community sample. J. Renal Inj. Prev. 2015, 4, 127–134. [Google Scholar] [CrossRef] [PubMed]
- Assari, S.; Moazen-Zadeh, E.; Lankarani, M.M.; Micol-Foster, V. Race, Depressive Symptoms and All-Cause Mortality in the United States. Front. Public Health 2016, 4, 40. [Google Scholar] [CrossRef] [PubMed]
- Assari, S.; Lankarani, M.M. Chronic Medical Conditions and Negative Affect; Racial Variation in Reciprocal Associations over Time. Front. Psychiatry 2016. [Google Scholar] [CrossRef] [PubMed]
- Assari, S. Combined Racial and Gender Differences in the Long-Term Predictive Role of Education on Depressive Symptoms and Chronic Medical Conditions. J. Racial Ethn. Health Dispar. 2016. [Google Scholar] [CrossRef] [PubMed]
- Moazen-Zadeh, E.; Assari, S. Depressive Symptoms Predict Major Depressive Disorder after 15 Years among Whites but Not Blacks. Front. Public Health 2016, 4, 13. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.J.; Moody-Ayers, S.Y.; Landefeld, C.S.; Walter, L.C.; Lindquist, K.; Segal, M.R.; Covinsky, K.E. The relationship between self-rated health and mortality in older black and white Americans. J. Am. Geriatr. Soc. 2007, 55, 1624–1629. [Google Scholar] [CrossRef] [PubMed]
- Assari, S.; Lankarani, M.M.; Burgard, S. Black White Difference in Long Term Predictive Power of Self-Rated Health on All-Cause Mortality in United States. Ann. Epidemiol. 2016, 26, 106–114. [Google Scholar] [CrossRef] [PubMed]
- Ferraro, K.F.; Kelley-Moore, J.A. Self-rated health and mortality among black and white adults: Examining the dynamic evaluation thesis. J. Gerontol. B Psychol. Sci. Soc. Sci. 2001, 56, S195–S205. [Google Scholar] [CrossRef] [PubMed]
- Krause, N. Religion, Aging and Health Survey, 2001, 2004 [United States]. ICPSR03255-v2; Inter-University Consortium for Political and Social Research [distributor]: Ann Arbor, MI, USA, 2006. [Google Scholar]
- Krause, N. Church-based volunteering, providing informal support at church and self-rated health in late life. J. Aging Health 2009, 21, 63–84. [Google Scholar] [CrossRef] [PubMed]
- Radloff, L.S. The CES-D scale: A self-report depression scale for research in the general population. Appl. Psychol. Meas. 1977, 1, 385–401. [Google Scholar] [CrossRef]
- Amtmann, D.; Kim, J.; Chung, H.; Bamer, A.M.; Askew, R.L.; Wu, S.; Cook, K.F.; Johnson, K.L. Comparing CESD-10, PHQ-9 and PROMIS depression instruments in individuals with multiple sclerosis. Rehabil. Psychol. 2014, 59, 220–229. [Google Scholar] [CrossRef] [PubMed]
- Zhang, W.; O’Brien, N.; Forrest, J.I.; Salters, K.A.; Patterson, T.L.; Montaner, J.S.; Hogg, R.S.; Lima, V.D. Validating a shortened depression scale (10 item CES-D) among HIV-positive people in British Columbia, Canada. PLoS ONE 2012, 7, e40793. [Google Scholar] [CrossRef] [PubMed]
- Andresen, E.M.; Malmgren, J.A.; Carter, W.B.; Patrick, D.L. Screening for depression in well older adults: Evaluation of a short form of the CES-D (Center for Epidemiologic Studies Depression Scale). Am. J. Prev. Med. 1994, 10, 77–84. [Google Scholar] [CrossRef]
- Abu-Raiya, H.; Pargament, K.I.; Krause, N. Religion as problem, religion as solution: Religious buffers of the links between religious/spiritual struggles and well-being/mental health. Qual. Life Res. 2016, 25, 1265–1274. [Google Scholar] [CrossRef] [PubMed]
- Hayward, R.D.; Krause, N. Forms of Attrition in a Longitudinal Study of Religion and Health in Older Adults and Implications for Sample Bias. J. Relig. Health 2016, 55, 50–66. [Google Scholar] [CrossRef] [PubMed]
- Krause, N. Church-Based Emotional Support and Self-Forgiveness in Late Life. Rev. Relig. Res. 2010, 52, 72–89. [Google Scholar] [PubMed]
- Krause, N. A comprehensive strategy for developing closed-ended survey items for use in studies of older adults. J. Gerontol. Soc. Sci. 2002, 57, S263–S274. [Google Scholar] [CrossRef]
- Krause, N.; Hayward, R.D. Church-based social support, functional disability and change in personal control over time. J. Relig. Health 2014, 53, 267–278. [Google Scholar] [CrossRef] [PubMed]
- Cohen, S.; Underwood, L.G.; Gottlieb, B.H. (Eds.) Social Support Measurement and Intervention: A Guide for Health and Social Scientists; Oxford University Press: Oxford, UK, 2000. [Google Scholar]
- Krause, N. Church-based social support and health in old age: Exploring variations by race. J. Gerontol. B Psychol. Sci. Soc. Sci. 2002, 57, S332–S347. [Google Scholar] [CrossRef] [PubMed]
- Mutran, E. Intergenerational family support among blacks and whites: Response to culture or to socioeconomic differences. J. Gerontol. 1985, 40, 382–389. [Google Scholar] [CrossRef] [PubMed]
- Strogatz, D.S.; James, S.A. Social support and hypertension among blacks and whites in a rural, southern community. Am. J. Epidemiol. 1986, 124, 949–956. [Google Scholar] [CrossRef] [PubMed]
- Taylor, R.J.; Chatters, L.M.; Jackson, J.S. Changes over time in support network involvement among black Americans. In Family Life in Black America; Taylor, R.J., Jackson, J.S., Chatters, L.M., Eds.; Sage Publications: Thousand Oaks, CA, USA, 1997; pp. 293–316. [Google Scholar]
- Drevenstedt, G. Race and ethnic differences in the effects of religious attendance on subjective health. Rev. Relig. Res. 1998, 39, 245–263. [Google Scholar] [CrossRef]
- Billingsley, A. Climbing Jacob’s Ladder: Enduring Legacy of African American Familie; Simon and Schuster: New York, NY, USA, 1992. [Google Scholar]
- Chaves, M.L.; Higgins, M. Comparing the community involvement of black and white congregations. J. Sci. Study Relig. 1992, 31, 425–440. [Google Scholar] [CrossRef]
- Ammerman, N. Tatom Bible Believers: Fundamentalists in the Modern World; Rutgers University Press: New Brunswick, NJ, USA, 1987. [Google Scholar]
- Chatters, L.M.; Taylor, R.J.; Jackson, J.S.; Lincoln, K.D. Religious coping among African Americans, caribbean blacks and non-hispanic whites. J. Community Psychol. 2008, 36, 371–386. [Google Scholar] [CrossRef] [PubMed]
- Assari, S. Whites but Not Blacks Gain Life Expectancy from Social Contacts. Behav. Sci. 2017, 7. [Google Scholar] [CrossRef] [PubMed]
- Schwartz, S.J. The applicability of familism to diverse ethnic groups: A preliminary study. J. Soc. Psychol. 2007, 147, 101–118. [Google Scholar] [CrossRef] [PubMed]
- Constantine, M.G.; Gainor, K.A.; Ahluwalia, M.K.; Berkel, L.A. Independent and interdependent self-construals, individualism, collectivism and harmony control in African Americans. J. Black Psychol. 2003, 29, 87–101. [Google Scholar] [CrossRef]
- Morling, B.; Fiske, S.T. Defining and measuring harmony control. J. Res. Personal. 1999, 33, 379–414. [Google Scholar] [CrossRef]
- Ebigbo, P.O.; Oluka, J.; Ezenwa, M.; Obidigbo, G.; Okwaraji, E. Harmony restoration therapy—An African contribution to psychotherapy. IFE Psychol. Int. J. 1997, 5, 51–70. [Google Scholar]
- Morling, B.; Kitayama, S.; Miyamoto, Y. Cultural practices emphasize influence in the United States and adjustment in Japan. Personal. Soc. Psychol. Bull. 2002, 28, 311–323. [Google Scholar] [CrossRef]
- McDowell, I. Measures of self-perceived well-being. J. Psychosom. Res. 2010, 69, 69–79. [Google Scholar] [CrossRef] [PubMed]
- Hunt, M.O. The Individual, society, or both? A comparison of black, latino and white beliefs about the causes of poverty. Soc. Forces 1996, 75, 293–332. [Google Scholar] [CrossRef]
- Hunt, M.O.; Jackson, P.B.; Powell, B.; Steelman, L.C. Color-blind: The treatment of race and ethnicity in social psychology. Soc. Psychol. Q. 2000, 63, 352–364. [Google Scholar] [CrossRef]
- Lett, H.S.; Blumenthal, J.A.; Babyak, M.A.; Strauman, T.J.; Robins, C.; Sherwood, A. Social support and coronary heart disease: Epidemiologic evidence and implications for treatment. Psychosom. Med. 2005, 67, 869–878. [Google Scholar] [CrossRef] [PubMed]
- House, J.S. Work Stress and Social Support; Addison-Wesley: Reading, MA, USA, 1981. [Google Scholar]
- House, J.S.; Kahn, R.L. Measures and concepts of social support. In Social Support and Health; Cohen, S., Syme, S.L., Eds.; Academic Press: New York, NY, USA, 1985; pp. 83–108. [Google Scholar]
- House, J.S.; Landis, K.R.; Umberson, D. Social relationships and health. Science 1988, 241, 540–545. [Google Scholar] [CrossRef] [PubMed]
- Uchino, B.N.; Cacioppo, J.T.; Kiecolt-Glaser, J.K. The relationship between social support and physiological processes: A review with emphasis on underlying mechanisms and implications for health. Psychol. Bull. 1996, 119, 488–531. [Google Scholar] [CrossRef] [PubMed]
- Kiecolt-Glaser, J.K.; Newton, T.L. Marriage and health: His and hers. Psychol. Bull. 2001, 127, 472–503. [Google Scholar] [CrossRef] [PubMed]
- Cacioppo, J.T.; Hawkley, L.C.; Crawford, E.; Ernst, J.M.; Burleson, M.H.; Kowalewski, R.B.; Berntson, G.G. Loneliness and health: Potential mechanisms. Psychosom. Med. 2002, 64, 407–417. [Google Scholar] [CrossRef] [PubMed]
- Cohen, S. Social Relationships and Health. Am. Psychol. 2004, 59, 676–684. [Google Scholar] [CrossRef] [PubMed]
- Krause, N. Feelings of Gratitude toward God among Older Whites, Older African Americans and Older Mexican Americans. Res. Aging 2012, 34, 156–173. [Google Scholar] [CrossRef] [PubMed]
- Nelsen, H.M.; Nelsen, A.K. Black Church in the Sixties; University of Kentucky Press: Lexington, KY, USA, 1975. [Google Scholar]
- Roberts, J.D. Black Religion, Black Theology; Goatley, E.M., Ed.; Trinity Press International: Harrisburg, PA, USA, 2003. [Google Scholar]
- Dowd, J.B.; Zajacova, A. Does the predictive power of self-rated health for subsequent mortality risk vary by socioeconomic status in the US? Int. J. Epidemiol. 2007, 36, 1214–1221. [Google Scholar] [CrossRef] [PubMed]
- Assari, S. Hostility and Cardiovascular Mortality among Blacks and Whites. Res. Cardiovasc. Med. 2016. [Google Scholar] [CrossRef]
- Flegal, K.M.; Kit, B.K.; Orpana, H.; Graubard, B.I. Association of all-cause mortality with overweight and obesity using standard body mass index categories: A systematic review and meta-analysis. JAMA 2013, 309, 71–82. [Google Scholar] [CrossRef] [PubMed]
- Patel, A.V.; Hildebrand, J.S.; Gapstur, S.M. Body mass index and all-cause mortality in a large prospective cohort of white and black us Adults. PLoS ONE 2014, 9, e109153. [Google Scholar] [CrossRef] [PubMed]
- Cohen, S.S.; Signorello, L.B.; Cope, E.L.; McLaughlin, J.K.; Hargreaves, M.K.; Zheng, W.; Blot, W.J. Obesity and all-cause mortality among black adults and white adults. Am. J. Epidemiol. 2012, 176, 431–442. [Google Scholar] [CrossRef] [PubMed]
- Assari, S. Additive effects of anxiety and depression on body mass index among blacks: Role of ethnicity and gender. Int. Cardiovasc. Res. J. 2014, 8, 44–51. [Google Scholar] [PubMed]
- Assari, S. Association between obesity and depression among American Blacks: Role of ethnicity and gender. J. Racial Ethn. Health Dispar. 2014, 1, 36–44. [Google Scholar] [CrossRef]
- Gariepy, G.; Wang, J.; Lesage, A.D.; Schmitz, N. The Longitudinal Association from Obesity to Depression: Results From the 12-year National Population Health Survey. Obesity 2010, 18, 1033–1038. [Google Scholar] [CrossRef] [PubMed]
- Cheng, J.K.Y.; Fancher, T.L.; Ratanasen, M.; Conner, K.R.; Duberstein, P.R.; Sue, S.; Takeuchi, D. Lifetime suicidal ideation and suicide attempts in Asian Americans. Asian Am. J. Psychol. 2010, 1, 18–30. [Google Scholar] [CrossRef] [PubMed]
- Assari, D.; Dejman, M.; Neighbors, H.W. Ethnic Differences in Separate and Additive Effects of Anxiety and Depression on Self Rated Mental Health among Blacks. J. Racial Ethn. Health Dispar. 2015. [Google Scholar] [CrossRef] [PubMed]
- Lynch, C.P.; Gebregziabher, M.; Echols, C.; Gilbert, G.E.; Zhao, Y.; Egede, L.E. Racial disparities in all-cause mortality among veterans with type 2 diabetes. J. Gen. Intern. Med. 2010, 25, 1051–1056. [Google Scholar] [CrossRef] [PubMed]
- Assari, S. Cross-Country Differences in the Additive Effects of Socioeconomics, Health Behaviors and Medical Comorbidities on Disability among Older Adults with Heart Disease. J. Tehran Heart Cent. 2015, 10, 24–33. [Google Scholar] [PubMed]
- Assari, S. Cross-country variation in additive effects of socio-economics, health behaviors and comorbidities on subjective health of patients with diabetes. J. Diabetes Metab. Disord. 2014, 13, 36. [Google Scholar]
- Assari, S. Race, sense of control over life and short-term risk of mortality among older adults in the United States. Arch. Med. Sci. 2016. [Google Scholar] [CrossRef] [PubMed]
- Assari, S. Over-adjustment bias by controlling for overall health. Int. J. Prev. Med. 2013, 4, 491–492. [Google Scholar] [PubMed]
- Schisterman, E.F.; Cole, S.R.; Platt, R.W. Overadjustment bias and unnecessary adjustment in epidemiologic studies. Epidemiology 2009, 20, 488–495. [Google Scholar] [CrossRef] [PubMed]
- MacKinnon, D.P.; Krull, J.L.; Lockwood, C.M. Equivalence of the mediation, confounding and suppression effect. Prev. Sci. 2000, 1, 173–181. [Google Scholar] [CrossRef] [PubMed]
- Deaton, A.; Lubotsky, D. Mortality, inequality and race in American cities and states. Soc. Sci. Med. 2003, 56, 1139–1153. [Google Scholar] [CrossRef]
- Dressler, W.W.; Oths, K.S.; Gravlee, C.C. Race and ethnicity in public health research: Models to explain health disparities. Annu. Rev. Anthropol. 2005, 34, 231–252. [Google Scholar] [CrossRef]
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).