Development and Validation of a Questionnaire to Assess Knowledge, Threat and Coping Appraisal, and Intention to Practice Healthy Behaviors Related to Non-Communicable Diseases in the Thai Population
Abstract
:1. Introduction
2. Materials and Methods
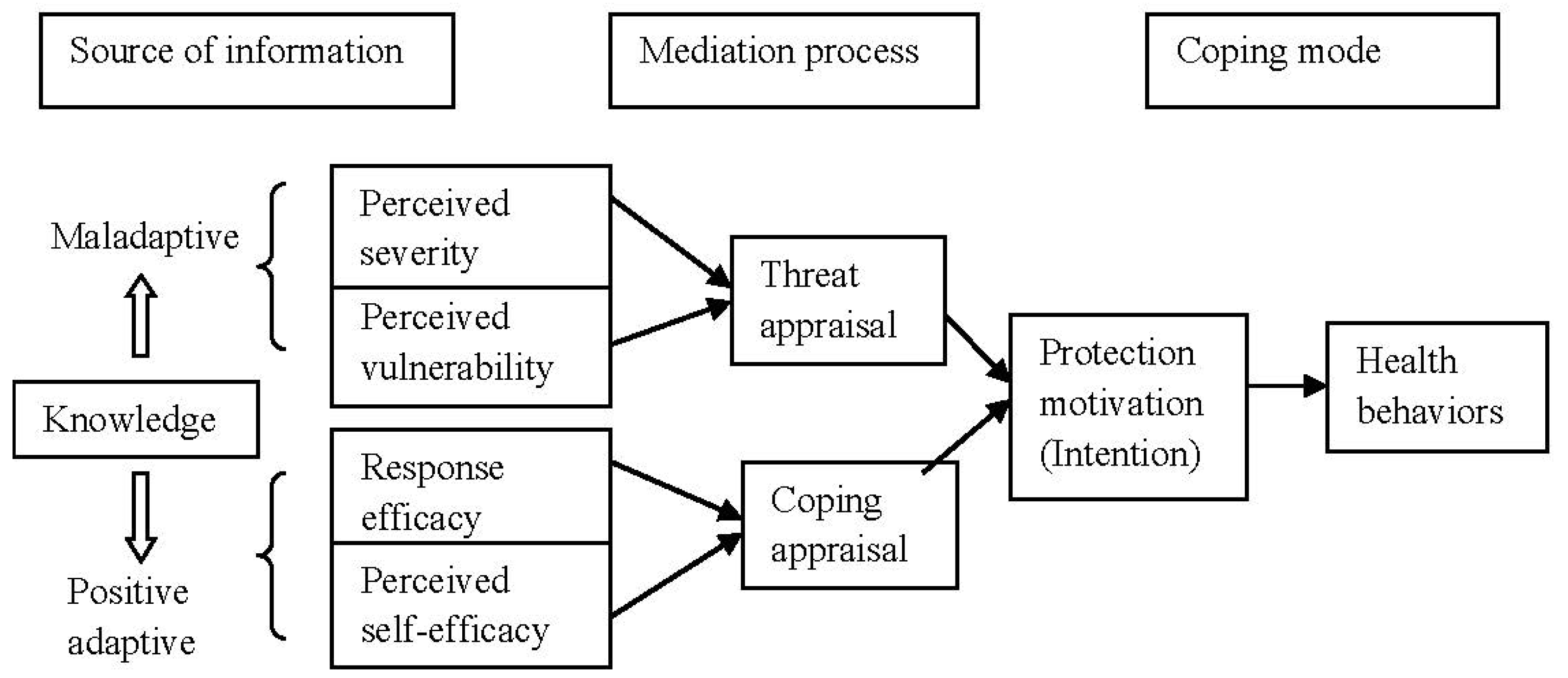
2.1. Conceptual Framework
2.2. Initial Questionnaire Construction
2.2.1. Knowledge on NCDs
2.2.2. Threat Appraisal on NCDs
2.2.3. Coping Appraisal toward NCDs
2.2.4. Intention to Practice
2.3. Subjects and Data Collection Procedures
2.4. Data Analysis
2.5. Ethical Consideration
3. Results
4. Discussion
5. Strengths and Limitations of the Study
6. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Leanne Riley, M.C. Noncommunicable Diseases Country Profiles 2014; WHO: Geneva, Switzerland, 2014. [Google Scholar]
- Disease Control, Department of Disease Control. NCDS Annual Report; Bureau of Noncommunicable Disease Control, Department of Disease Control, The War Veterans Organization of Thailand Publication: Bangkok, Thailand, 2016.
- World Health Organization. Noncommunicable Diseases (Fact Sheet); World Health Organization: Geneva, Switzerland, 2015. [Google Scholar]
- World Health Organization. Assessment of National Capacity for Noncommunicable Disease Prevention and Control 2001; World Health Organization: Geneva, Switzerland, 2015. [Google Scholar]
- World Health Organization, Regional Office for South-East Asia. Global Adult Tobacco Survey: Thailand Report 2011; WHO Library Cataloguing-in-Publication Data, World Health Organization: Bangkok, Thailand, 2011. [Google Scholar]
- Rogers, R.W. Cognitive and Physiological Processes in Fear Appeal and Attitude Change: A Revised Theory of Protection Motivation; Guilford Press: New York, NY, USA, 1983. [Google Scholar]
- Rogers, R.W. A protection motivation theory of fear appeals and attitude change1. J. Psychol. 1975, 91, 93–114. [Google Scholar] [CrossRef] [PubMed]
- Norman, P.; Boer, H.; Seydel, E.R. Protection Motivation Theory, 2nd ed.; Open University Press: Maidenhead, UK, 2005. [Google Scholar]
- Bursey, M.; Craig, D. Attitudes, subjective norm, perceived behavioral control, and intentions related to adult smoking cessation after coronary artery bypass graft surgery. Public Health Nurs. 2000, 17, 460–467. [Google Scholar] [CrossRef] [PubMed]
- Plotnikoff, R.C.; Rhodes, R.E.; Trinh, L. Protection motivation theory and physical activity: A longitudinal test among a representative population sample of Canadian adults. J. Health Psychol. 2009, 14, 1119–1134. [Google Scholar] [CrossRef] [PubMed]
- Knight, H.; Stetson, B.; Krishnasamy, S.; Mokshagundam, S.P. Diet self-management and readiness to change in underserved adults with type 2 diabetes. Prim. Care Diabetes 2015, 9, 219–225. [Google Scholar] [CrossRef] [PubMed]
- Chen, M.F.; Wang, R.H.; Hung, S.L. Predicting health-promoting self-care behaviors in people with pre-diabetes by applying bandura social learning theory. Appl. Nurs. Res. (ANR) 2015, 28, 299–304. [Google Scholar] [CrossRef] [PubMed]
- Kang, C.M.; Chang, S.C.; Chen, P.L.; Liu, P.F.; Liu, W.C.; Chang, C.C.; Chang, W.Y. Comparison of family partnership intervention care vs. Conventional care in adult patients with poorly controlled type 2 diabetes in a community hospital: A randomized controlled trial. Int. J. Nurs. Stud. 2010, 47, 1363–1373. [Google Scholar] [CrossRef] [PubMed]
- Yao, D.K.; Su, W.; Zheng, X.; Wang, L.X. Knowledge and understanding of hypertension among Tibetan people in Lhasa, Tibet. Heart Lung Circ. 2016, 25, 600–606. [Google Scholar] [CrossRef] [PubMed]
- Demaio, A.R.; Nehme, J.; Otgontuya, D.; Meyrowitsch, D.W.; Enkhtuya, P. Tobacco smoking in Mongolia: Findings of a national knowledge, attitudes and practices study. BMC Publ. Health 2014, 14, 213. [Google Scholar] [CrossRef] [PubMed]
- McDonnell, L.A.; Pipe, A.L.; Westcott, C.; Perron, S.; Younger-Lewis, D.; Elias, N.; Nooyen, J.; Reid, R.D. Perceived vs actual knowledge and risk of heart disease in women: Findings from a Canadian survey on heart health awareness, attitudes, and lifestyle. Can. J. Cardiol. 2014, 30, 827–834. [Google Scholar] [CrossRef] [PubMed]
- Diez-Ascaso, O.; Martinez-Sanchez, P.; Fernandez-Fournier, M.; Diez-Tejedor, E.; Fuentes, B. Stroke patients’ recognition and knowledge of their own vascular risk factors: A sociocultural study. J. Stroke Cerebrovasc. Dis. 2015, 24, 2839–2844. [Google Scholar] [CrossRef] [PubMed]
- Koo, J.H.; Arasaratnam, M.M.; Liu, K.; Redmond, D.M.; Connor, S.J.; Sung, J.J.; Leong, R.W. Knowledge, perception and practices of colorectal cancer screening in an ethnically diverse population. Cancer Epidemiol. 2010, 34, 604–610. [Google Scholar] [CrossRef] [PubMed]
- Walker, S.L.; Saltman, D.L.; Colucci, R.; Martin, L. Awareness of risk factors among persons at risk for lung cancer, chronic obstructive pulmonary disease and sleep apnea: A Canadian population-based study. Can. Respir. J. 2010, 17, 287–294. [Google Scholar] [CrossRef] [PubMed]
- Dawood, O.T.; Rashan, M.A.; Hassali, M.A.; Saleem, F. Knowledge and perception about health risks of cigarette smoking among Iraqi smokers. J. Pharm. Bioallied Sci. 2016, 8, 146–151. [Google Scholar] [CrossRef] [PubMed]
- Hivert, M.F.; Warner, A.S.; Shrader, P.; Grant, R.W.; Meigs, J.B. Diabetes risk perception and intention to adopt healthy lifestyles among primary care patients. Diabetes Care 2009, 32, 1820–1822. [Google Scholar] [CrossRef] [PubMed]
- Aghili, R.; Khamseh, M.E.; Malek, M.; Banikarimi, A.S.; Baradaran, H.R.; Ebrahim Valojerdi, A. Development and validation of diabetes empowerment questionnaire in Iranian people with type 2 diabetes. Int. Nurs. Rev. 2013, 60, 267–273. [Google Scholar] [CrossRef] [PubMed]
- Yan, Y.; Jacques-Tiura, A.J.; Chen, X.; Xie, N.; Chen, J.; Yang, N.; Gong, J.; Macdonell, K.K. Application of the protection motivation theory in predicting cigarette smoking among adolescents in China. Addict. Behav. 2014, 39, 181–188. [Google Scholar] [CrossRef] [PubMed]
- Thrul, J.; Stemmler, M.; Buhler, A.; Kuntsche, E. Adolescents’ protection motivation and smoking behavior. Health Educ. Res. 2013, 28, 683–691. [Google Scholar] [CrossRef] [PubMed]
- Hsiao, C.Y.; Chang, C.; Chen, C.D. An investigation on illness perception and adherence among hypertensive patients. Kaohsiung J. Med. Sci. 2012, 28, 442–447. [Google Scholar] [CrossRef] [PubMed]
- Yan, J.; You, L.M.; He, J.G.; Wang, J.F.; Chen, L.; Liu, B.L.; Zhou, J.J.; Chen, J.H.; Jin, S.Y. Illness perception among Chinese patients with acute myocardial infarction. Patient Educ. Couns. 2011, 85, 398–405. [Google Scholar] [CrossRef] [PubMed]
- Abed, M.A.; Khalil, A.A.; Moser, D.K. Awareness of modifiable acute myocardial infarction risk factors has little impact on risk perception for heart attack among vulnerable patients. Heart Lung J. Crit. Care 2015, 44, 183–188. [Google Scholar] [CrossRef] [PubMed]
- Santarelli, R.L.; Pierre, F.; Corpet, D.E. Processed meat and colorectal cancer: A review of epidemiologic and experimental evidence. Nutr. Cancer 2008, 60, 131–144. [Google Scholar] [CrossRef] [PubMed]
- Wong, M.C.; Hirai, H.W.; Luk, A.K.; Lam, T.Y.; Ching, J.Y.; Griffiths, S.M.; Chan, F.K.; Sung, J.J. The knowledge of colorectal cancer symptoms and risk factors among 10,078 screening participants: Are high risk individuals more knowledgeable? PLoS ONE 2013, 8, e60366. [Google Scholar] [CrossRef] [PubMed]
- Lipkus, I.M.; Green, L.G.; Marcus, A. Manipulating perceptions of colorectal cancer threat: Implications for screening intentions and behaviors. J. Health Commun. 2003, 8, 213–228. [Google Scholar] [CrossRef] [PubMed]
- Mun, S.Y.; Hwang, Y.I.; Kim, J.H.; Park, S.; Jang, S.H.; Seo, J.Y.; Kim, J.K.; Park, Y.B.; Shim, J.J.; Jung, K.S. Awareness of chronic obstructive pulmonary disease in current smokers: A nationwide survey. Korean J. Int. Med. 2015, 30, 191–197. [Google Scholar] [CrossRef] [PubMed]
- Miravitlles, M.; Ferrer, J.; Baro, E.; Lleonart, M.; Galera, J. Differences between physician and patient in the perception of symptoms and their severity in COPD. Respir. Med. 2013, 107, 1977–1985. [Google Scholar] [CrossRef] [PubMed]
- Park, S.K.; Larson, J.L. Multiple symptoms, functioning, and general health perception in people with severe copd over time. Appl. Nurs. Res. (ANR) 2016, 29, 76–82. [Google Scholar] [CrossRef] [PubMed]
- Orbell, S.; Lidierth, P.; Henderson, C.J.; Geeraert, N.; Uller, C.; Uskul, A.K.; Kyriakaki, M. Social-cognitive beliefs, alcohol, and tobacco use: A prospective community study of change following a ban on smoking in public places. Health Psychol. 2009, 28, 753–761. [Google Scholar] [CrossRef] [PubMed]
- Ritland, R.; Rodriguez, L. The influence of antiobesity media content on intention to eat healthily and exercise: A test of the ordered protection motivation theory. J. Obes. 2014, 2014, 954784. [Google Scholar] [CrossRef] [PubMed]
- Kara, M.; van der Bijl, J.J.; Shortridge-Baggett, L.M.; Asti, T.; Erguney, S. Cross-cultural adaptation of the diabetes management self-efficacy scale for patients with type 2 diabetes mellitus: Scale development. Int. J. Nurs. Stud. 2006, 43, 611–621. [Google Scholar] [CrossRef] [PubMed]
- Larsson, H.; Tegern, M.; Monnier, A.; Skoglund, J.; Helander, C.; Persson, E.; Malm, C.; Broman, L.; Aasa, U. Content validity index and intra- and inter-rater reliability of a new muscle strength/endurance test battery for Swedish soldiers. PLoS ONE 2015, 10, e0132185. [Google Scholar] [CrossRef] [PubMed]
- Najimi, A.; Golshiri, P. Knowledge, beliefs and preventive behaviors regarding influenza a in students: A test of the health belief model. J. Educ. Health Promot. 2013, 2, 23. [Google Scholar] [CrossRef] [PubMed]
- Cioe, P.A.; Crawford, S.L.; Stein, M.D. Cardiovascular risk-factor knowledge and risk perception among HIV-infected adults. J. Assoc. Nurses AIDS Care (JANAC) 2014, 25, 60–69. [Google Scholar] [CrossRef] [PubMed]
| Part of Questionnaire | No. of Items | Mean Item CVI |
|---|---|---|
| NCD knowledge | 25 | 0.947 |
| Threat appraisal | 50 | 1.000 |
| Coping appraisal | 47 | 0.915 |
| Intention to practice | 10 | 0.900 |
| Disease | No. of Items | Difficulty |
|---|---|---|
| T2DM Knowledge | 5 | 0.54–0.80 |
| HT knowledge | 5 | 0.35–0.77 |
| CVD knowledge | 5 | 0.34–0.70 |
| Colon cancer knowledge | 5 | 0.57–0.90 |
| COPD and lung cancer knowledge | 5 | 0.32–0.94 |
| Part of Questionnaire | No. of Items | Reliability Test |
|---|---|---|
| Knowledge * | ||
| -T2DM. | 5 | 0.793 |
| -HT | 5 | 0.799 |
| -CVD | 5 | 0.786 |
| -Colon cancer | 5 | 0.747 |
| -COPD and Lung cancer | 5 | 0.648 |
| Threat appraisal (severity & vulnerability) ** | ||
| -T2DM. | 10 | 0.706 |
| -HT | 10 | 0.816 |
| -CVD | 10 | 0.824 |
| -Colon cancer | 10 | 0.843 |
| -COPD and Lung cancer | 10 | 0.817 |
| Coping appraisal (response efficacy & self-efficacy) ** | ||
| -Response efficacy | 12 | 0.805 |
| -Self efficacy | 35 | 0.799 |
| Intention to practice health behaviors | 10 | 0.729 |
| Characteristics | T2DM Cases (n = 50) | Controls (n = 50) | p-Value |
|---|---|---|---|
| Age in years ( | 57.94 ± 9.61 | 52.0 ± 8.359 | 0.002 * |
| Female | 70% | 76% | 0.457 |
| Body mass index ( | 27.05 ± 9.16 | 25.18 ± 3.07 | 0.407 |
| Primary school education | 70% | 50% | 0.281 |
| Scores | T2DM cases (n = 50) | Controls (n = 50) | p-Value |
|---|---|---|---|
| Knowledge scores | Median (IQR) | Median (IQR) | |
| -T2DM | 4.5 (2.0) | 4.0 (3.0) | 0.003 * |
| -HT | 4.0 (2.0) | 3.0 (2.75) | 0.005 * |
| -CVD | 3.0 (4.0) | 3.0 (3.0) | 0.158 |
| -Colon cancer | 3.0 (2.75) | 4.0 (3.0) | 0.739 |
| -COPD and Lung cancer | 3.0 (3.0) | 3.0 (2.0) | 0.779 |
| Threat appraisal scores | |||
| -T2DM | 28.0 (3.0) | 28.0 (4.75) | 0.105 |
| -HT | 28.0 (4.0) | 27.0 (3.0) | 0.021 * |
| -CVD | 29.0 (4.0) | 27.5 (4.75) | 0.032 * |
| -Colon cancer | 27.0 (6.0) | 26.0 (6.0) | 0.085 |
| -COPD & Lung cancer | 29.0 (4.0) | 29.0 (3.0) | 0.383 |
| Coping appraisal scores | |||
| -Response efficacy | 35.5 (4.0) | 36.0 (2.0) | 0.357 |
| -Self efficacy | 86.5 (14.5) | 88.0 (12.75) | 0.597 |
| Intention to practice scores | 30.0(0) | 30.0 (1.0) | 0.270 |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chamroonsawasdi, K.; Chottanapund, S.; Tunyasitthisundhorn, P.; Phokaewsuksa, N.; Ruksujarit, T.; Phasuksathaporn, P. Development and Validation of a Questionnaire to Assess Knowledge, Threat and Coping Appraisal, and Intention to Practice Healthy Behaviors Related to Non-Communicable Diseases in the Thai Population. Behav. Sci. 2017, 7, 20. https://doi.org/10.3390/bs7020020
Chamroonsawasdi K, Chottanapund S, Tunyasitthisundhorn P, Phokaewsuksa N, Ruksujarit T, Phasuksathaporn P. Development and Validation of a Questionnaire to Assess Knowledge, Threat and Coping Appraisal, and Intention to Practice Healthy Behaviors Related to Non-Communicable Diseases in the Thai Population. Behavioral Sciences. 2017; 7(2):20. https://doi.org/10.3390/bs7020020
Chicago/Turabian StyleChamroonsawasdi, Kanittha, Suthat Chottanapund, Pravich Tunyasitthisundhorn, Nawaphan Phokaewsuksa, Tassanee Ruksujarit, and Pawarat Phasuksathaporn. 2017. "Development and Validation of a Questionnaire to Assess Knowledge, Threat and Coping Appraisal, and Intention to Practice Healthy Behaviors Related to Non-Communicable Diseases in the Thai Population" Behavioral Sciences 7, no. 2: 20. https://doi.org/10.3390/bs7020020
APA StyleChamroonsawasdi, K., Chottanapund, S., Tunyasitthisundhorn, P., Phokaewsuksa, N., Ruksujarit, T., & Phasuksathaporn, P. (2017). Development and Validation of a Questionnaire to Assess Knowledge, Threat and Coping Appraisal, and Intention to Practice Healthy Behaviors Related to Non-Communicable Diseases in the Thai Population. Behavioral Sciences, 7(2), 20. https://doi.org/10.3390/bs7020020





