Abstract
Face washing for trachoma, like most public health improvements, necessitates behaviour change, yet traditional educational interventions frequently fail to achieve this goal. Behavioural science frameworks offer guidance to develop alternative types of interventions, helping to translate formative research and insights about the target population and behavioural determinants into more effective strategies. This paper outlines the outputs and decision-making underlying the five-stage process we followed to translate formative research findings into intervention activities and materials: (1) synthesising formative research findings into a creative brief to guide intervention development; (2) selecting behaviour change techniques (BCTs) to address key behavioural targets; (3) selecting an overarching intervention concept; (4) developing intervention content; and (5) finalising the intervention’s Theory of Change. This paper presents our experiences and reflections on the intervention design process, using a practical example of a face washing intervention for trachoma control. The intervention was designed for delivery in the Stronger SAFE trial in rural Oromia, Ethiopia (ISCRTN 40760473).
1. Introduction
Behaviour change interventions in the Water, Sanitation, and Hygiene (WASH) sector have progressed from educational and community development approaches to incorporate growing insights from behavioural science. A feature of this is the application of structured methods to translate behavioural theory into intervention components (Aunger & Curtis, 2016; Dreibelbis et al., 2013; Michie et al., 2011; Mosler, 2012). A key step in this process is the conduction of formative research, which involves the collection of data to identify the intervention’s target audience and understand their needs, behaviours, and the context in which they operate (Gittelsohn et al., 2006; Glasgow & Linnan, 2008). The main purpose of formative research is to understand the variety of personal, cognitive, social, cultural, and structural factors that influence individual behaviours in a given context and the processes that can be mobilised to develop effective interventions that bring about change in these factors at different levels (e.g., individual, interpersonal, organisational, environmental).
A growing body of WASH literature documents formative research studies rooted in behavioural science, implementation studies through process evaluations, as well as quantitative outcome evaluations following the method of scientific enquiry, often in the form of a randomised controlled trial (Biswas et al., 2021; D’Mello-Guyett et al., 2020; Greenland et al., 2017; Kuhl et al., 2021; Ogutu et al., 2022; Panulo et al., 2022; Sule et al., 2022). However, less attention has been given to the intervention design process, which translates formative research into practical materials and activities for implementation and evaluation through process and outcome evaluation.
Intervention design is a creative process which encompasses both content and delivery strategies. While increasingly informed by formative research and behavioural science frameworks, it is also shaped by prior experience, pragmatic decision-making, researchers’ experiential knowledge, and contextual adaptations, constraints, and opportunities (Tidwell et al., 2019). The limited systematic reporting of this design process hinders experience sharing and learning among behaviour change researchers and practitioners.
This paper addresses the gap between formative research and intervention implementation and evaluation by documenting and reflecting on the creative process of designing a face washing intervention for trachoma control.
Despite widespread implementation of the WHO-endorsed SAFE strategy—Surgery to treat blinding trachoma, Antibiotic mass drug administration, Facial cleanliness, and Environmental improvement to reduce the pool of infection and slow transmission—(World Health Organization, 2020; Taylor et al., 2014), trachoma remains a major public health challenge in Ethiopia, which accounts for a disproportionate 59% of the global at-risk population (World Health Organization, 2024). Facial cleanliness interventions for trachoma prevention have primarily relied on educational approaches (Delea et al., 2018; Freeman et al., 2022); trials of such interventions have not demonstrated a significant impact on trachoma outcomes to date (Abdou et al., 2010; Aragie et al., 2022; Ejere et al., 2015). In this article, we present the creative design process used to translate formative research findings into a face washing intervention for trachoma control in rural Oromia, Ethiopia. We detail five distinct stages of the intervention’s design: Stage 1 involved developing a creative brief by synthesising formative research findings; Stage 2 entailed selecting behaviour change techniques (BCTs) to address behavioural targets; Stage 3 focused on choosing an overarching intervention concept; Stage 4 comprised developing intervention content, including designing, testing, and refining activities and materials; and Stage 5 involved finalising the intervention’s Theory of Change (ToC) (De Silva et al., 2014; Weiss, 1995). For each stage, we describe the outcome and the decision-making process. The Methods section details the decision-making within each stage, while the Results section presents the tangible outputs produced by each creative stage.
2. Materials and Methods
Intervention design was guided by Behaviour Centred Design (BCD) (Aunger & Curtis, 2016; Aunger et al., 2017) and Risk, Attitude, Norm, Ability, and Self-regulation (RANAS) models (Mosler, 2012), which had also guided our formative research. These models have been used to develop successful behaviour change interventions in the WASH sector (Biran et al., 2014; Friedrich et al., 2020; Inauen & Mosler, 2014), and offer complementary, structured frameworks for developing engaging, contextually relevant interventions to address key determinants of behaviour. The following sections detail the methods used and decisions made during each stage of the intervention design process.
2.1. Stage 1—Developing the Creative Brief: Synthesising Formative Research
The design of this face washing intervention was conducted within specific intervention parameters established by the Stronger SAFE cluster-randomised trial (Stronger SAFE, ISCRTN 40760473), which evaluated a comprehensive package of trachoma control interventions. These parameters mandated face-to-face community-based implementation through local health volunteers and community leaders; a structured two-year delivery timeline aligned with the timeframe for the trial; delivery at the garee (sub-village administrative unit) level; employment of multi-modal delivery strategies; integration within existing public health infrastructure; adaptation for low literacy populations with limited mass media access; incorporation of mechanisms for sustained behaviour maintenance; and universal household inclusion within intervention communities.
To inform the intervention design, a series of preliminary and formative research studies were conducted, exploring local determinants of face washing and contextual factors likely to influence intervention implementation (Czerniewska et al., 2020; Greenland et al., 2019, 2022; Last et al., 2020; Shafi Abdurahman et al., 2023).
The ‘creative brief’, the output of the synthesis of data from these studies, provided the foundation for the intervention design process (Aunger et al., 2017). Recognising the overlap between formative research and intervention design, this stage details the synthesis process to provide context for the subsequent intervention development.
The creative brief was developed through a collaborative process involving qualitative synthesis of research findings supplemented by contributions from researchers and key stakeholders with expertise in face washing interventions. We identified key themes and patterns related to face washing behaviour and its determinants and organised these findings according to the five behavioural factors of the RANAS framework (risk, attitude, norm, ability, and self-regulation), i.e. the ’perceptions, thoughts, feelings, and beliefs that influence the practice of a behaviour’ within a specific context (Mosler, 2012). Through this process, we distilled the research findings into actionable insights for the intervention design.
The creative brief served as a roadmap for the intervention design, ensuring that a locally relevant intervention package was developed and all creative efforts were aligned with the intervention’s goals and the pre-defined intervention parameters. It detailed the formative research findings organised by behavioural factor and defined the target behaviour specifying who, when, where, and how face washing should be performed.
2.2. Stage 2—Selecting Behaviour Change Techniques (BCTs)
Stage 2 involved selecting strategies to bring about change in behavioural determinants identified in the brief, known as Behaviour Change Techniques (BCTs). Previous work has listed and categorised these techniques based on reviews of the behaviour change literature and expert opinion, mapping them to specific behaviour change problems they might address (Michie et al., 2013).
To select BCTs, we reformulated the potential determinants of behaviour outlined in the creative brief into specific targets that the intervention would address. We then utilised the RANAS catalogue of BCTs to select techniques for the intervention (Mosler, 2016). (When multiple BCTs were associated with a given factor, several were selected to enhance the likelihood of influencing that given factor. Techniques perceived as coercive, stigmatising (e.g., comparing or shaming neighbours’ behaviours), or reinforcing negative power dynamics were not selected.
2.3. Stage 3—Choosing an Overarching Intervention Concept
Following the BCD approach, we then chose an ‘umbrella’ concept to unify intervention activities under a compelling narrative linked to a motive that resonated with the community (Aunger et al., 2017; Czerniewska et al., 2023). The purpose was to enhance audience adherence to the intervention package, foster audience engagement, and improve the memorability of key intervention messages.
Four potential motives—“pair-bond love”, “nurture”, “status”, and “dignity”—were developed into short narratives and tested in eight focus group discussions (FGDs) with community members (four male groups, four female groups, six to eight participants per group) and five interviews with female primary caregivers. Participants listened to five- to ten-minute Afan Oromo audio recordings of the narratives, individually ranked them by memorability, likeability, and character relatability, and provided qualitative feedback on their rankings. They were also asked to describe daily activities associated with the different motives.
FGD and interview audio recordings were transcribed and analysed alongside field notes, focussing on the investigated attributes and perceived links to personal hygiene behaviours.
2.4. Stage 4—Developing Intervention Content
Intervention activities and materials were designed to integrate selected BCTs within a coherent package aligned with the overarching concept. This was achieved through an iterative process of ideation, prototyping, and refinement, involving stakeholder engagement and community feedback. A local creative agency, Spotlight, was hired to design the visuals and infographics used in intervention activities.
A five-day stakeholder workshop in Shashemene, Ethiopia, generated initial ideas for intervention activities and materials, with participation from federal and local government representatives, local health workers and community members, representatives from other NGOs working in the local areas, our field team, and creatives from a consortium of local and regional agencies. Working in small groups, these stakeholders shortlisted six promising ideas and developed prototypes.
Intervention content was further refined into activities and events through testing in 18 FGDs with children and female caregivers to assess understandability, acceptability, and relatability. Each activity was developed to target the specific intervention targets identified in Stage 2 and integrated one or multiple BCTs. Whenever possible, the “dignity” motive was used to frame activity content and the target behaviour was reinforced at least once during each event. A multi-event format was designed to maximise intensive contact points with the target population, while adhering to the intervention parameters. Local health volunteers, who were respected in the community, were involved in intervention delivery to legitimise it and support implementation. This approach leveraged existing outreach structures, promoting intervention buy-in, especially among community leaders.
The full intervention package was piloted three times under real-world conditions to assess coherence, flow, and pacing. After each round, participant feedback was reviewed, observations were shared, and the intervention package was refined for subsequent piloting.
2.5. Stage 5—Finalising the Intervention’s Theory of Change
A draft Theory of Change (ToC) was developed at the start of the design process outlining the outcomes, intermediate outcomes hypothesised to influence them, and the selected BCTs to drive measurable changes in these intermediate outcomes and ultimately lead to change in the target behaviour (De Silva et al., 2014; Weiss, 1995). This draft ToC was iteratively refined throughout intervention design to ensure intervention content was supported by hypothesised behaviour change pathways. The ToC was finalised after all intervention activities had been developed, piloted, and validated for inclusion in the intervention package. This finalisation incorporated inputs from multiple stakeholders with different expertise in behaviour change interventions, including local and international academics and WASH practitioners.
3. Results
3.1. Stage 1—Developing the Creative Brief: Synthesising Formative Research
Table 1 presents an overview of the insights from the formative research and preliminary studies, illustrating how findings were mapped to the RANAS behavioural factors. Given that face washing was typically limited to the early morning, rarely involved soap, and was unsupervised for young children (who are key in trachoma transmission), the target behaviour was defined as faces (and hands) of the whole family (particularly pre-school children) to be thoroughly washed with soap three times a day: morning after waking, before lunch, and before the evening meal. This definition prioritised pre-school children, increased washing frequency, and emphasised soap use and caregiver supervision for effective discharge removal.

Table 1.
Categorisation of formative research findings on face washing behaviour by RANAS behavioural factors.
Table 1 also highlights key insights from the formative research, including resource limitations such as soap and water, which pointed to the need for accessible and creative solutions operating within these constraints. Drawing on these actionable insights, the creative brief proposed that the face washing intervention delivered in this context should emphasise the benefits of soap while encouraging efficient water usage; establish a daily face washing with soap routine for children; promote the construction of accessible, high-quality wash stations with soap; support caregiver supervision to improve removal of discharge, which is known to transmit trachoma; and shift perceptions of discharge as a trachoma risk, using emotional motivators to drive behaviour change.
3.2. Stage 2—Selecting Behaviour Change Techniques (BCTs)
We identified 20 intervention targets within the five categories of the RANAS approach that represented the specific perceptions, thoughts, feelings, and beliefs that the intervention would need to modify to achieve the desired change in face washing behaviour. ‘Risk’ intervention targets included understanding the importance of face washing for trachoma control and strengthening the perception that ocular and nasal discharge are both disgusting and dangerous to health. Key ‘Attitudinal’ targets included perceptions that soap is important for face washing, wash stations make it easier to wash faces, and the amount of water and soap required for face washing is manageable, and the motivation to prioritise these resources for face washing. Key ‘Normative’ targets included the belief that face washing with soap must be performed several times a day to achieve truly clean faces throughout the year, and that such behaviours were expected by the community. Key ‘Ability’ intervention targets included the ability to construct and maintain a wash station stand, the ability to wash the faces of pre-school children, self-efficacy in acting as a role model, and taking responsibility for young children’s hygiene. Finally, key ‘Self-regulation’ targets were the integration of the target behaviour into daily routine, the consistent provision of water and soap for face washing, and the capacity to trouble-shoot seasonal factors to continue to prioritise these resources.
Table 2 presents these intervention targets along with 29 BCTs from the RANAS catalogue that were mapped to these targets.

Table 2.
RANAS Behaviour Change Techniques (BCTs) mapped against intervention targets.
3.3. Stage 3—Choosing an Overarching Concept
The “pair-bond love” narrative (linking face washing to marital relationships) resonated well with the community. However, we identified potential risks of reinforcing negative gender stereotypes or poor treatment of women using this narrative. The “status” narrative (highlighting social standing with a negative framing around public shaming) was not acceptable in the community. The “nurture” (focused on family well-being) was less engaging, as participants struggled to identify a clear emotional driver.
The “dignity” narrative demonstrated strong performance, with participants viewing dignity as fundamental to gaining respect and social standing, and establishing a credible link to personal hygiene of both adults and children, as illustrated by the following quote:
“Children come from the family, so if the family is dignified the children will be dignified”.(Female caregiver, individual household interview on the concept of dignity, January 2020)
Both the “pair-bond love” and “dignity” narratives scored highly across comprehension, acceptability, reliability, and perceived connection to face washing (Table 3). However, to mitigate potential negative side effects associated with the “pair-bond love” theme, dignity was ultimately chosen as the intervention concept.

Table 3.
Comparative evaluation of motivational narratives for face washing behaviour.
The intervention was named the Faces of Dignity intervention, with the tagline “A clean face is attractive, it is also dignifying”, exemplified by the image of a dignified family, which was refined through multiple rounds of community feedback (Figure 1). This image visually represented the intervention’s central narrative and served as its logo, being easily recognisable, memorable, and aspirational for the audience, reminding them about the target behaviour promoted by the intervention. The logo was displayed on the intervention banner and materials.
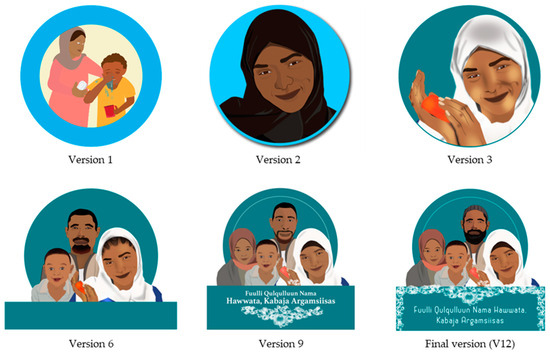
Figure 1.
Evolution of the Faces of Dignity intervention logo. “Fuulli Qulqulluun Nama Hawwata, Kabaja Argamsiisas” translates as “A clean face is attractive, it is also dignifying”.
3.4. Stage 4—Developing Intervention Content
3.4.1. Intervention Activities
Between April 2019 and February 2021, 33 intervention activities were designed based on ideas proposed in the stakeholders’ meeting and refined with community feedback. Figure 2 illustrates the development process of three of these activities, showing how key formative research findings were categorised by RANAS behavioural factors (Stage 1), reformulated into behavioural targets and linked to relevant BCTs (Stage 2), and translated into intervention activities.
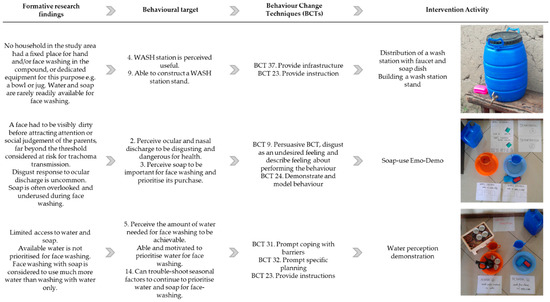
Figure 2.
Three examples illustrating the theory-informed design of intervention activities for the Faces of Dignity intervention. BCT: Behaviour Change Technique.
3.4.2. Intervention Package
The 33 intervention activities were grouped into nine events. The full intervention package of activities and materials is presented in Table 4. The first five events—the Community Event, two Family Fora, and two Household Visits—formed the intensive behaviour change package, which was followed by four Seasonal Reinforcement Events spread out over the two years that the trial was planned to last. Detailed intervention manuals outlining the content and materials required for each event were developed to aid training and ensure intervention fidelity and standardisation throughout implementation (see Supplementary Materials).

Table 4.
Overview of the Faces of Dignity intervention.
The Community Event, designed to engage all residents of the three garees (administrative units of approximately 90 households), involved two actors, local influential leaders, and health volunteers. A 20-min drama with a life-sized child puppet was used to present different face washing scenarios and outcomes, introducing parents as hygiene role models and promoting the target behaviour as a way of maintaining family dignity and social acceptance. The event culminated in a collective pledge led by influential community leaders, following which wash stations with a faucet, soap, and soap dishes were distributed to all households to make face washing easier and cue behaviour.
One trained activator and one health volunteer delivered the two Family Fora, one week apart to groups of five neighbouring households. The first Family Forum aimed to build knowledge, skills, and motivation for face washing, and inspire households to commit to constructing a wash station stand to facilitate face washing and habit formation. The second Family Forum focused on addressing practical challenges and motivation related to wash station (stand) construction and usage.
Household Visits intended to provide more tailored feedback and support to overcome face washing barriers and maintain wash stations, with rewards provided to signal completion of the intensive programme. Two health volunteers and the activator conducted the Household Visits, one and two weeks after the second Family Forum. Using health volunteers who were already known and respected in the community helped to legitimise the intervention. It also leveraged the existing structure for community outreach.
Following this intensive phase, four Seasonal Reinforcement Events targeting groups of 10 households were led by health volunteers. These events aimed to address specific seasonal challenges, provide tips on wash station maintenance, and encourage continuation of new face washing practises, highlighting the key roles played by adults in the family in modelling behaviour and continuously provisioning water and soap at the stations.
3.5. Stage 5—Finalising the Intervention’s Theory of Change
The intervention’s final Theory of Change is presented in Figure 3. The schematic illustrates how intervention activities and associated BCTs are employed to modify specific behavioural targets (intermediate outcomes) which are hypothesised to increase face washing with soap (outcome). This increased face washing, in turn, is expected to reduce oculo-nasal discharge on children’s faces, thereby contributing to a decrease in trachoma transmission within the community.
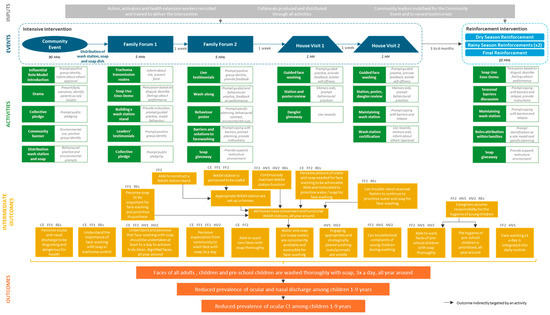
Figure 3.
Theory of Change for the Faces of Dignity intervention. The event that includes activities targeting each intermediate outcome is indicated. CE = Community Event; FF1 = Family Forum 1; FF2 = Family Forum 2; HV1 = House Visit 1; HV2 = House Visit 2; REs = Reinforcement Events.
4. Discussion
This paper describes five key stages in the development of behaviour change interventions, using the example of a face washing intervention to improve the trachoma control strategy in a trachoma-endemic setting, in rural Oromia, Ethiopia.
Intervention design was informed by extensive formative research and grounded in two behaviour (change) theories, the BCD and RANAS approaches, both recognised approaches used to develop WASH behaviour change interventions in low-income countries (De Buck et al., 2017). These intervention design guidelines and theoretical frameworks enabled us to structure the creative process and organise our formative research findings to address a range of behavioural factors likely to drive face washing behaviour in our setting (Michie, 2008), a consideration often overlooked in face washing interventions for trachoma control (Delea et al., 2018).
Although structured into different steps, our creative design process shares similarities with other documented hygiene intervention development frameworks, notably the process outlined by Arriola et al. for designing interventions to improve nutrition and WASH behaviours (Jacob Arriola et al., 2020). A key distinction in our approach is that we treated formative research as a prerequisite rather than an integrated component of the creative process. We initiated our creative process by synthesising research findings into a comprehensive creative brief, which specified intervention parameters, the target behaviour, and behavioural determinants that could be modified by an intervention, elements that Jacob Arriola et al. addressed as a separate second step. The timing of Theory of Change (ToC) development also differed. While Jacob Arriola et al. articulated the ToC early in their process, our ToC model was drafted at the outset and iteratively refined throughout intervention design. While we employed different behaviour change frameworks, both creative processes followed a similar sequence: identifying behavioural targets, selecting behaviour change techniques (BCTs), developing intervention activities, and refining intervention packages using various data collection methods. However, our approach makes two notable contributions to the literature: first, by documenting the selection of an overarching intervention concept aligned with the BCD model; and second, by detailing how intervention activities were derived from formative research, linked to specific behavioural determinants, mapped to relevant BCTs, and translated into concrete activities. This systematic translation process, which provides a clear trail from formative research to implementation, represents an advancement on existing descriptions of intervention design processes.
These variations in intervention design structuring, however, highlight an important reality: despite the availability of frameworks detailing steps needed to be undertaken to translate theory into practical interventions (French et al., 2012; Michie, 2008; Susan Michie et al., 2011; O’Cathain et al., 2019), the design process remains complex and often requires making decisions that depart from established frameworks. Intervention design thus entails a series of decisions, informed by a combination of methodological guidance, empirical evidence, prior knowledge, and professional experience. The principal challenge is the precise documentation of decision-making to ensure transparency, thereby enabling the broader scientific and practitioner community to comprehend and replicate the design process. This documentation is essential for advancing both the theoretical understanding and practical development of behavioural interventions.
A key challenge in documenting intervention design lies in capturing its inherently iterative nature (O’Cathain et al., 2019). Unlike the straightforward linear process that the description in stages might suggest, intervention design is dynamic and continually evolves as new insights and challenges arise. While this iterative approach allows for flexibility and adaptability, it often requires prolonged periods of field testing, ongoing intervention refinement, and, at times, lengthy decision-making processes. The development of the Faces of Dignity intervention took 22 months (during the COVID-19 pandemic). The pandemic did not alter the content of our intervention, but the extended timelines of intervention development might raise concerns about the applicability and timeliness of pre-existing evidence underpinning the design process in a rapidly changing context.
Another important reflection concerns the co-design process. Co-production ensures interventions are culturally relevant, sustainable, and owned by the communities they serve. It creates trust, builds capacity, and increases the likelihood of long-term impact (Vargas et al., 2022). Co-production is relatively uncommon in low-income countries (Singh et al., 2023). The COVID-19 pandemic and local travel restrictions linked to political unrest hindered our ability to engage as closely with communities as we desired. These factors restricted full community involvement in intervention development and feasibility testing. Ideally, a more advanced co-production process would have involved local communities more actively in the selection of intervention priorities from the outset.
One of the key strengths of this work was the development of a robust Theory of Change (De Silva et al., 2014). The Theory of Change provided a clear and comprehensive vision of the intervention activities structured around specific BCTs and the hypothesised causal pathways through which the intervention is expected to influence face washing behaviour. Furthermore, the Theory of Change facilitated the identification of key indicators that were assessed in the later process and outcome evaluations.
Despite identifying water availability as a major barrier to face washing in our formative research, budgetary and logistical constraints prevented direct intervention in water access. Instead, Family Fora activities sought to shift perceptions of water scarcity by demonstrating that face washing with soap requires less water than commonly assumed and providing strategies for conserving water for this purpose. This limitation highlights how interventions are shaped by initial project parameters and contextual constraints, reinforcing that intervention development necessarily involves decisions extending beyond strictly defined scientific methodologies.
To conclude, this paper represents one of few attempts to document the transition from formative research to intervention implementation and evaluation by detailing the intervention design process. It outlines experiences that may benefit other researchers and practitioners attempting to synthesise formative research findings, choose behavioural targets and behaviour change techniques, develop overarching concepts to unify interventions, and develop intervention’s activities and materials, alongside refining the intervention’s Theory of Change. Finally, this paper also highlights the importance of recognising the potential limitations of intervention design processes, which, despite being labelled as theory-based and scientific, still involve significant subjective decision-making, further influenced by contextual and project-specific constraints. We provide a practical example of how a rigorously designed intervention can be developed using explicit behaviour change theory, informed by empirical formative research findings through a transparent decision-making process.
The resulting intensive intervention was delivered over four to six weeks in 34 rural communities between January and April 2022. Reinforcement Events were delivered around the start of the dry and rainy seasons in September 2022, January 2023, September 2023, and January 2024. Results of the process and outcome evaluation are forthcoming.
Supplementary Materials
The following supporting information can be downloaded at https://www.mdpi.com/article/10.3390/bs15030355/s1, Intervention Manuals.
Author Contributions
Conceptualization, K.G.; methodology, K.G., A.B., A.C. and C.C.; validation, K.G., A.C. and C.C.; formal analysis, K.G., C.C. and A.C.; investigation, K.G., C.C., A.C., E.S.E. and O.S.A.; resources, O.S.A., A.A. and W.A.; data curation, C.C., K.G., A.C., E.S.E., D.L., M.G., A.A.M., E.H. and S.D.; writing—original draft preparation, K.G., A.B. and C.C.; writing—review and editing, C.C., A.C., D.L., M.G., A.A.M., A.B., E.S.E., A.A., W.A., S.D., O.S.A., E.H., D.A., A.L., M.J.B. and K.G.; visualisation, C.C. and K.G.; supervision, K.G., C.C., A.B., A.A., E.S.E., A.L. and M.J.B.; project administration, O.S.A. and A.A.; funding acquisition, M.J.B. All authors have read and agreed to the published version of the manuscript.
Funding
This research is supported by a Wellcome Trust Collaborative Award (206275/Z/17/Z) and the Children’s Investment Foundation Fund (102653IR1).
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki. The research is a collaboration between the London School of Hygiene and Tropical Medicine (UK) (sponsor), the Federal Ministry of Health (Ethiopia), the Oromia Regional Health Bureau (Ethiopia), and the Fred Hollows Foundation (Ethiopia and International). Approval for the research conducted in this trial has been obtained from the London School of Hygiene and Tropical Medicine Ethics Committee (UK) (Reference 17494), the Oromia Regional Health Bureau (BEFO/DDFDHU/1-89/3515), the National Research Ethics Review Committee of the Ethiopian Ministry of Science and Higher Education (MOSHE//RD/141/8082/19), and the Ethiopian Food and Drug Authority (02/25/32/206).
Informed Consent Statement
Written informed consent was obtained from adult participants and legal guardians of minors, and assent was provided by children aged 7–17, as required by the ethics committees which approved the study.
Data Availability Statement
The raw data from Focus Group Discussions and Interviews conducted during intervention development that support the conclusions of this article will be made available by the authors on request.
Acknowledgments
We are indebted to the community members who assisted with the development and testing of intervention materials. We are also grateful to the wider Stronger-SAFE team in Shashemene for their assistance with initial testing of the Faces of Dignity intervention activities, providing resources for fieldwork, data management and data storage, and helping with the sourcing of equipment. We would also like to thank Bob Aunger at LSHTM for his helpful suggestions at various stages during intervention design and Bob Aunger and Robert Dreibelbis at LSHTM for their comments on this manuscript. Thanks also go to Spotlight, for developing intervention materials, and the Busara Center for Behavioural Economics and Khanga Rue for their assistance with the narrative testing and early intervention design.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Abdou, A., Munoz, B. E., Nassirou, B., Kadri, B., Moussa, F., Baarè, I., Riverson, J., Opong, E., & West, S. K. (2010). How much is not enough? A community randomized trial of a Water and Health Education programme for Trachoma and Ocular C. trachomatis infection in Niger. Tropical Medicine & International Health, 15(1), 98–104. [Google Scholar] [CrossRef]
- Aragie, S., Wittberg, D. M., Tadesse, W., Dagnew, A., Hailu, D., Chernet, A., Melo, J. S., Aiemjoy, K., Haile, M., Zeru, T., Tadesse, Z., Gwyn, S., Martin, D. L., Arnold, B. F., Freeman, M. C., Nash, S. D., Callahan, E. K., Porco, T. C., Lietman, T. M., & Keenan, J. D. (2022). Water, sanitation, and hygiene for control of trachoma in Ethiopia (WUHA): A two-arm, parallel-group, cluster-randomised trial. The Lancet Global Health, 10(1), e87–e95. [Google Scholar] [CrossRef] [PubMed]
- Aunger, R., & Curtis, V. (2016). Behaviour centred design: Towards an applied science of behaviour change. Health Psychology Review, 10(4), 425–446. [Google Scholar] [CrossRef]
- Aunger, R., White, S., Greenland, K., & Curtis, V. (2017). Behaviour centred design. A practitioner’s manual. Available online: https://www.lshtm.ac.uk/sites/default/files/2017-03/BCD%20Manual.pdf (accessed on 17 September 2020).
- Biran, A., Schmidt, W. P., Varadharajan, K. S., Rajaraman, D., Kumar, R., Greenland, K., Gopalan, B., Aunger, R., & Curtis, V. (2014). Effect of a behaviour-change intervention on handwashing with soap in India (SuperAmma): A cluster-randomised trial. The Lancet Global Health, 2(3), e145–e154. [Google Scholar] [CrossRef]
- Biswas, S. K., Thomas, E. D., Masud, J., Zohura, F., Hasan, T., Parvin, T., Bhuyian, S. I., Minhaj, I., Johura, F., Sultana, M., Tahmina, S., Monira, S., Perin, J., Alam, M., & George, C. M. (2021). Formative research for the design of a baby water, sanitation, and hygiene mobile health program in Bangladesh (CHoBI7 Mobile Health Program). The American Journal of Tropical Medicine and Hygiene, 104(1), 357–371. [Google Scholar] [CrossRef] [PubMed]
- Czerniewska, A., Mwambuli, K., Curtis, V., & Aunger, R. (2023). Intervention design in public health: Adaptive messaging in the Tanzanian National Sanitation Campaign. Health Promotion International, 38(3), daad064. [Google Scholar] [CrossRef]
- Czerniewska, A., Versteeg, A., Shafi, O., Dumessa, G., Aga, M. A., Last, A., MacLeod, D., Sarah, V., Dodson, S., Negussu, N., Sori, B. K., Kirumba, M., Biran, A., Cairncross, S., Burton, M. J., & Greenland, K. (2020). Comparison of face washing and face wiping methods for trachoma control: A pilot study. The American Journal of Tropical Medicine and Hygiene, 102(4), 740–743. [Google Scholar] [CrossRef]
- De Buck, E., Van Remoortel, H., Hannes, K., Govender, T., Naidoo, S., Avau, B., Veegaete, A. V., Musekiwa, A., Lutje, V., Cargo, M., Mosler, H., Vandekerckhove, P., & Young, T. (2017). Approaches to promote handwashing and sanitation behaviour change in low- and middle-income countries: A mixed method systematic review. Campbell Systematic Reviews, 13(1), 1–447. [Google Scholar] [CrossRef]
- Delea, M. G., Solomon, H., Solomon, A. W., & Freeman, M. C. (2018). Interventions to maximize facial cleanliness and achieve environmental improvement for trachoma elimination: A review of the grey literature. PLoS Neglected Tropical Diseases, 12(1), e0006178. [Google Scholar] [CrossRef]
- De Silva, M. J., Breuer, E., Lee, L., Asher, L., Chowdhary, N., Lund, C., & Patel, V. (2014). Theory of Change: A theory-driven approach to enhance the Medical Research Council’s framework for complex interventions. Trials, 15(1), 267. [Google Scholar] [CrossRef]
- D’Mello-Guyett, L., Greenland, K., Bonneville, S., D’Hondt, R., Mashako, M., Gorski, A., Verheyen, D., Bergh, R. V. D., Maes, P., Checchi, F., & Cumming, O. (2020). Distribution of hygiene kits during a cholera outbreak in Kasaï-Oriental, Democratic Republic of Congo: A process evaluation. Conflict and Health, 14(1), 51. [Google Scholar] [CrossRef] [PubMed]
- Dreibelbis, R., Winch, P. J., Leontsini, E., Hulland, K. R. S., Ram, P. K., Unicomb, L., & Luby, S. P. (2013). The integrated behavioural model for water, sanitation, and hygiene: A systematic review of behavioural models and a framework for designing and evaluating behaviour change interventions in infrastructure-restricted settings. BMC Public Health, 13(1), 1015. [Google Scholar] [CrossRef] [PubMed]
- Ejere, H. O., Alhassan, M. B., & Rabiu, M. (2015). Face washing promotion for preventing active trachoma. Cochrane Database of Systematic Reviews, 2015(2), CD003659. [Google Scholar] [CrossRef]
- Freeman, M. C., Delea, M. G., Snyder, J. S., Garn, J. V., Belew, M., Caruso, B. A., Clasen, T. F., Sclar, G. D., Tesfaye, Y., Woreta, M., Zewudie, K., & Gobezayehu, A. G. (2022). The impact of a demand-side sanitation and hygiene promotion intervention on sustained behavior change and health in Amhara, Ethiopia: A cluster-randomized trial. PLoS Global Public Health, 2(1), e0000056. [Google Scholar] [CrossRef] [PubMed]
- French, S. D., Green, S. E., O’Connor, D. A., McKenzie, J. E., Francis, J. J., Michie, S., Buchbinder, R., Schattner, P., Spike, N., & Grimshaw, J. M. (2012). Developing theory-informed behaviour change interventions to implement evidence into practice: A systematic approach using the Theoretical Domains Framework. Implementation Science, 7(1), 38. [Google Scholar] [CrossRef]
- Friedrich, M., Balasundaram, T., Muralidharan, A., Raman, V. R., & Mosler, H.-J. (2020). Increasing latrine use in rural Karnataka, India using the risks, attitudes, norms, abilities, and self-regulation approach: A cluster-randomized controlled trial. Science of the Total Environment, 707, 135366. [Google Scholar] [CrossRef]
- Gittelsohn, J., Steckler, A., Johnson, C. C., Pratt, C., Grieser, M., Pickrel, J., Stone, E. J., Conway, T., Coombs, D., & Staten, L. K. (2006). Formative research in school and community-based health programs and studies: “State of the Art” and the TAAG approach. Health Education & Behavior, 33(1), 25–39. [Google Scholar] [CrossRef]
- Glasgow, R. E., & Linnan, L. (2008). Evaluation of theory-based interventions. In K. Glanz, B. K. Rimer, & K. Viswanath (Eds.), Health behaviour and health education. Theory, Research and Practice. Jossey-Bass. [Google Scholar]
- Greenland, K., Chipungu, J., Chilekwa, J., Chilengi, R., & Curtis, V. (2017). Disentangling the effects of a multiple behaviour change intervention for diarrhoea control in Zambia: A theory-based process evaluation. Globalization and Health, 13(1), 78. [Google Scholar] [CrossRef]
- Greenland, K., Czerniewska, A., Guye, M., Legesse, D., Ahmed Mume, A., Abdurahman, O. S., Aga, M. A., Miecha, H., Bejiga, G. S., Sarah, V., Burton, M., & Last, A. (2022). Seasonal variation in water use for hygiene in Oromia, Ethiopia, and its implications for trachoma control: An intensive observational study. PLoS Neglected Tropical Diseases, 16(5), e0010424. [Google Scholar] [CrossRef]
- Greenland, K., White, S., Sommers, K., Biran, A., Burton, M. J., Sarah, V., & Alemayehu, W. (2019). Selecting behaviour change priorities for trachoma ‘F’ and ‘E’ interventions: A formative research study in Oromia, Ethiopia. PLoS Neglected Tropical Diseases, 13(10), e0007784. [Google Scholar] [CrossRef]
- Inauen, J., & Mosler, H.-J. (2014). Developing and testing theory-based and evidence-based interventions to promote switching to arsenic-safe wells in Bangladesh. Journal of Health Psychology, 19(12), 1483–1498. [Google Scholar] [CrossRef]
- Jacob Arriola, K. R., Ellis, A., Webb-Girard, A., Ogutu, E. A., McClintic, E., Caruso, B., & Freeman, M. C. (2020). Designing integrated interventions to improve nutrition and WASH behaviors in Kenya. Pilot and Feasibility Studies, 6(1), 10. [Google Scholar] [CrossRef] [PubMed]
- Kuhl, J., Bisimwa, L., Thomas, E. D., Williams, C., Ntakirutimana, J., Coglianese, N., Bauler, S., François, R., Sanvura, P., Bisimwa, J. C., Mirindi, P., & George, C. M. (2021). Formative research for the development of baby water, sanitation, and hygiene interventions for young children in the Democratic Republic of the Congo (REDUCE program). BMC Public Health, 21(1), 427. [Google Scholar] [CrossRef] [PubMed]
- Last, A., Versteeg, B., Shafi Abdurahman, O., Robinson, A., Dumessa, G., Abraham Aga, M., Bejiga, G. S., Negussu, N., Greenland, K., Czerniewska, A., Thomson, N., Cairncross, S., Sarah, V., Macleod, D., Solomon, A. W., Logan, J., & Burton, M. J. (2020). Detecting extra-ocular Chlamydia trachomatis in a trachoma-endemic community in Ethiopia: Identifying potential routes of transmission. PLoS Neglected Tropical Diseases, 14(3), e0008120. [Google Scholar] [CrossRef] [PubMed]
- Michie, S. (2008). Designing and implementing behaviour change interventions to improve population health. Journal of Health Services Research & Policy, 13(3_suppl), 64–69. [Google Scholar] [CrossRef]
- Michie, S., Richardson, M., Johnston, M., Abraham, C., Francis, J., Hardeman, W., Eccles, M. P., Cane, J., & Wood, C. E. (2013). The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: Building an international consensus for the reporting of behavior change interventions. Annals of Behavioral Medicine, 46(1), 81–95. [Google Scholar] [CrossRef]
- Michie, S., van Stralen, M. M., & West, R. (2011). The behaviour change wheel: A new method for characterising and designing behaviour change interventions. Implementation Science, 6(1), 42. [Google Scholar] [CrossRef]
- Mosler, H. J. (2012). A systematic approach to behavior change interventions for the water and sanitation sector in developing countries: A conceptual model, a review, and a guideline. International Journal of Environmental Health Research, 22(5), 431–449. [Google Scholar] [CrossRef]
- Mosler, H. J. (2016). Catalog of behavior change techniques (BCTs). ESI 3.1 to a practical guide using the RANAS approach version 1.0, August 2016. Available online: https://76ddba31-385f-4f1b-a8fc-00db654c6cbf.filesusr.com/ugd/accbe3_2540cf86e0e84a779156dd4a58aaab14.pdf (accessed on 17 September 2020).
- O’Cathain, A., Croot, L., Duncan, E., Rousseau, N., Sworn, K., Turner, K. M., Yardley, L., & Hoddinott, P. (2019). Guidance on how to develop complex interventions to improve health and healthcare. BMJ Open, 9(8), e029954. [Google Scholar] [CrossRef]
- Ogutu, E. A., Ellis, A., Rodriguez, K. C., Caruso, B. A., McClintic, E. E., Ventura, S. G., Arriola, K. R. J., Kowalski, A. J., Linabarger, M., Wodnik, B. K., Webb-Girard, A., Muga, R., & Freeman, M. C. (2022). Determinants of food preparation and hygiene practices among caregivers of children under two in Western Kenya: A formative research study. BMC Public Health, 22(1), 1865. [Google Scholar] [CrossRef]
- Panulo, M., Chidziwisano, K., Beattie, T. K., Tilley, E., Kambala, C., & Morse, T. (2022). Process evaluation of “The Hygienic Family” intervention: A community-based water, sanitation, and hygiene project in rural Malawi. International Journal of Environmental Research and Public Health, 19(11), 6771. [Google Scholar] [CrossRef] [PubMed]
- Shafi Abdurahman, O., Last, A., Macleod, D., Habtamu, E., Versteeg, B., Dumessa, G., Guye, M., Nure, R., Adugna, D., Miecha, H., Greenland, K., & Burton, M. J. (2023). Trachoma risk factors in Oromia region, Ethiopia. PLoS Neglected Tropical Diseases, 17(11), e0011679. [Google Scholar] [CrossRef]
- Singh, D. R., Sah, R. K., Simkhada, B., & Darwin, Z. (2023). Potentials and challenges of using co-design in health services research in low- and middle-income countries. Global Health Research and Policy, 8(1), 5. [Google Scholar] [CrossRef]
- Sule, M. N., Mosha, J., Soboka, T. E., Kinung’hi, S. M., Sfynia, C., Rafiq, K., Dower, A., Comparet, M., Bewley, E., Angelo, T., Beshah, F. Z., & Templeton, M. R. (2022). A novel theatre-based behaviour change approach for influencing community uptake of schistosomiasis control measures. Parasites & Vectors, 15(1), 301. [Google Scholar] [CrossRef]
- Taylor, H. R., Burton, M. J., Haddad, D., West, S., & Wright, H. (2014). Trachoma. Lancet, 384(9960), 2142–2152. [Google Scholar] [CrossRef] [PubMed]
- Tidwell, J. B., Chipungu, J., Chilengi, R., Curtis, V., & Aunger, R. (2019). Using a theory-driven creative process to design a peri-urban on-site sanitation quality improvement intervention. BMC Public Health, 19(1), 565. [Google Scholar] [CrossRef] [PubMed]
- Vargas, C., Whelan, J., Brimblecombe, J., & Allendera, S. (2022). Co-creation, co-design and co-production for public health: A perspective on definitions and distinctions. Public Health Research & Practice, 32(2), e3222211. [Google Scholar]
- Weiss, C. (1995). Nothing as practical as a good theory: Exploring theory-based evaluation in complex community initiatives for children and families. In J. Connell, A. Kubisch, L. Schorr, & C. Weiss (Eds.), New approaches to evaluating community initiatives: Volume 1, concepts, methods, and contexts. The Aspen Institute. [Google Scholar]
- World Health Organization. (2020). Ending the neglect to attain the sustainable development goals: A road map for neglected tropical diseases 2021–2030. World Health Organization. [Google Scholar]
- World Health Organization. (2024). WHO alliance for the global elimination of trachoma: Progress report on elimination of trachoma, 2023. Weekly Epidemiological Record, 28(99), 363–380. [Google Scholar]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).