A Prospective Examination of Mental Health Trajectories of Disaster-Exposed Young Adults in the COVID-19 Pandemic
Abstract
1. Introduction
1.1. Conceptual Foundations: Transactional-Ecological Theory and a Disaster Mental Health Model
1.2. Broad Impacts of the COVID-19 Pandemic
1.3. Young Adult Development and Pre- and During-Pandemic Mental Health
1.4. Current Study
2. Materials and Methods
2.1. Participants
2.2. Measures—Pre-Pandemic Factors
2.3. Measures—Pre- and during Pandemic Mental Health
2.4. Analytic Procedure
3. Results
3.1. Preliminary Analyses
3.2. Hierarchical Linear Modeling Analyses
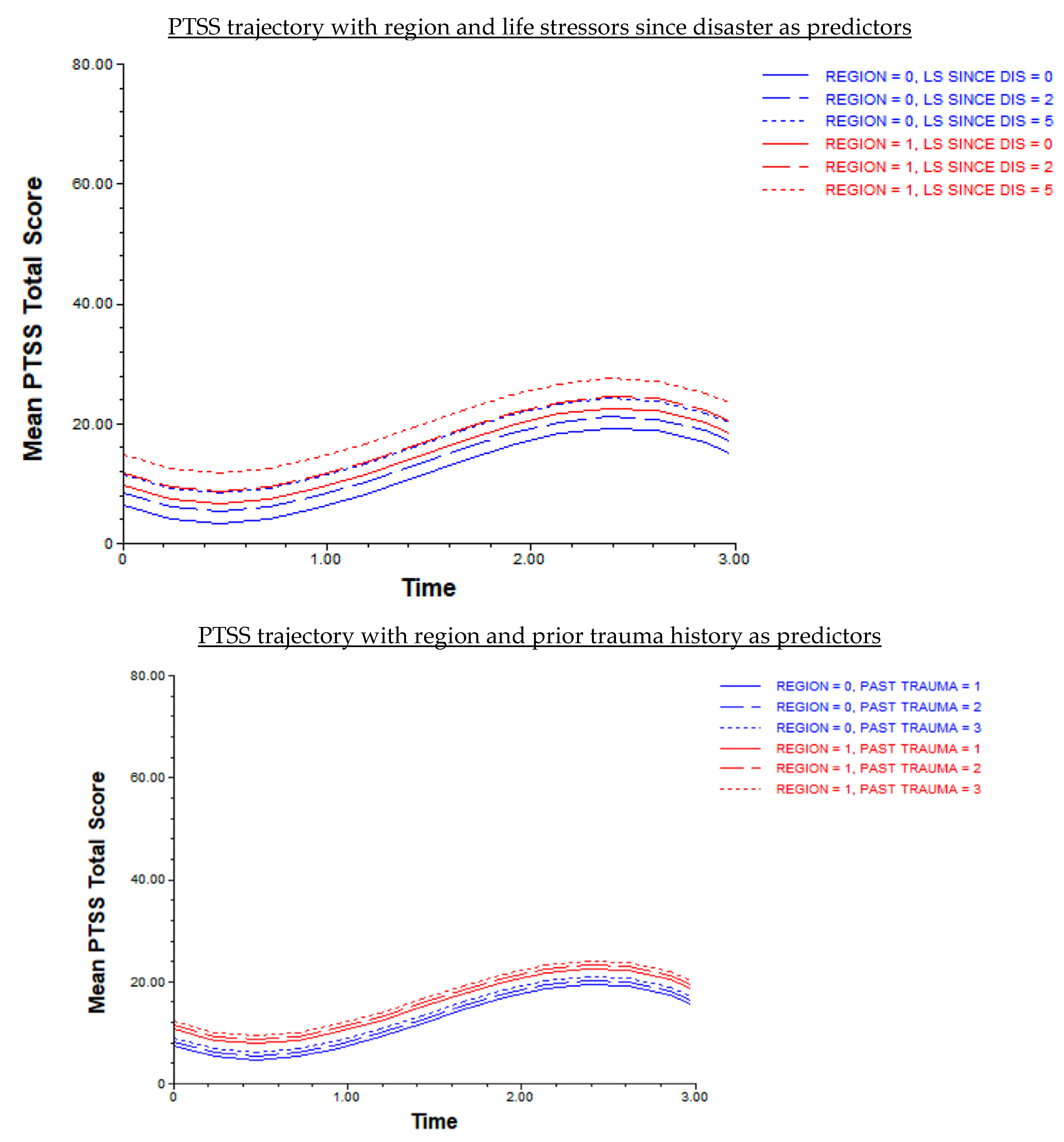
3.3. Post Hoc Analyses
3.4. Summary
4. Discussion
4.1. Mental Health Trends Pre- and during Pandemic
4.1.1. Prior Trauma History and Life Stressors since Disaster
4.1.2. Implications for Practice
4.1.3. Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Beaglehole, B.; Mulder, R.T.; Frampton, C.M.; Boden, J.M.; Newton-Howes, G.; Bell, C.J. Psychological distress and psychiatric disorder after natural disasters: Systematic review and meta-analysis. Br. J. Psychiatry J. Ment. Sci. 2018, 213, 716–722. [Google Scholar] [CrossRef] [PubMed]
- Bonanno, G.A.; Brewin, C.R.; Kaniasty, K.; La Greca, A.M. Weighing the costs of disaster: Consequences, risks, and resilience in individuals, families, and communities. Psychol. Sci. Public Interest 2010, 11, 1–49. [Google Scholar] [CrossRef]
- Leppold, C.; Gibbs, L.; Block, K.; Reifels, L.; Quinn, P. Public health implications of multiple disaster exposures. Lancet Public Health 2022, 7, e274–e286. [Google Scholar] [CrossRef]
- Silver, R.C.; Holman, E.A.; Garfin, D.R. Coping with cascading collective traumas in the United States. Nat. Hum. Behav. 2021, 5, 4–6. [Google Scholar] [CrossRef]
- Garfin, D.R.; Thompson, R.R.; Holman, E.A.; Wong-Parodi, G.; Silver, R.C. Association Between Repeated Exposure to Hurricanes and Mental Health in a Representative Sample of Florida Residents. JAMA Netw. Open 2022, 5, e2217251. [Google Scholar] [CrossRef]
- Acierno, R.; Ruggiero, K.J.; Kilpatrick, D.G.; Resnick, H.S.; Galea, S. Risk and protective factors for psychopathology among older versus younger adults after the 2004 Florida hurricanes. Am. J. Geriatr. Psychiatry 2006, 14, 1051–1059. [Google Scholar] [CrossRef]
- Bonanno, G.A.; Galea, S.; Bucciarelli, A.; Vlahov, D. What predicts psychological resilience after disaster? The role of demographics, resources, and life stress. J. Consult. Clin. Psychol. 2007, 75, 671–682. [Google Scholar] [CrossRef]
- American Psychological Association. Stress in AmericaTM 2020: A National Mental Health Crisis. 2020. Available online: https://www.apa.org/news/press/releases/stress/2020/sia-mental-health-crisis.pdf (accessed on 15 January 2021).
- American Psychological Association. Stress in America™ 2021: Stress and Decision-Making During the Pandemic. 2021. Available online: https://www.apa.org/news/press/releases/stress/2021/decision-making-october-2021.pdf (accessed on 1 November 2021).
- Cameron-Maldonado, S.; Pérez, C.M.; Fernández-Repollet, E.; López-Cepero, A. Age-Related Differences in Anxiety and Depression Diagnosis among Adults in Puerto Rico during the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2023, 20, 5922. [Google Scholar] [CrossRef]
- National Center for Health Statistics. U.S. Census Bureau, Household Pulse Survey, 2020–2021. Anxiety and Depression. 2021. Available online: https://www.cdc.gov/nchs/covid19/pulse/mental-health.htm (accessed on 5 May 2021).
- O’Donohue, K.; Berger, E.; McLean, L.; Carroll, M. Psychological outcomes for young adults after disastrous events: A mixed-methods scoping review. Soc. Sci. Med. 2021, 276, 113851. [Google Scholar] [CrossRef]
- Anderson, K.M.; Manuel, G. Gender differences in reported stress response to the Loma Prieta earthquake. Sex Roles A J. Res. 1994, 30, 725–733. [Google Scholar] [CrossRef]
- Nolen-Hoeksema, S.; Morrow, J. A prospective study of depression and posttraumatic stress symptoms after a natural disaster: The 1989 Loma Prieta Earthquake. J. Personal. Soc. Psychol. 1991, 61, 115–121. [Google Scholar] [CrossRef]
- Parslow, R.A.; Jorm, A.F. Tobacco use after experiencing a major natural disaster: Analysis of a longitudinal study of 2063 young adults. Addiction 2006, 101, 1044–1050. [Google Scholar] [CrossRef] [PubMed]
- Pistoia, F.; Conson, M.; Carolei, A.; Dema, M.G.; Splendiani, A.; Curcio, G.; Sacco, S. Post-earthquake Distress and Development of Emotional Expertise in Young Adults. Front. Behav. Neurosci. 2018, 12, 91. [Google Scholar] [CrossRef] [PubMed]
- Janson, M.; Felix, E.D.; Kaniasty, K.; Lugo-Hernández, E.A.; Rosa-Rodríguez, Y.; Canino, G. Life stressors and posttraumatic stress symptoms mediate the association between disaster exposure and identity-related distress in emerging adults. J. Am. Coll. Health, 2023; 1–10, advance online publication. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.; Bonanno, G.A. Psychological adjustment during the global outbreak of COVID-19: A resilience perspective. Psychol. Trauma Theory Res. Pract. Policy 2020, 12, S51–S54. [Google Scholar] [CrossRef] [PubMed]
- Cicchetti, D.; Lynch, M. Toward an ecological/transactional model of community violence and child maltreatment: Consequences for children’s development. Psychiatry 1993, 56, 96–118. [Google Scholar] [CrossRef]
- La Greca, A.M.; Silverman, W.K.; Vernberg, E.M.; Prinstein, M.J. Symptoms of posttraumatic stress in children after Hurricane Andrew: A prospective study. J. Consult. Clin. Psychol. 1996, 64, 712–723. [Google Scholar] [CrossRef]
- Lynch, M.; Cicchetti, D. An ecological-transactional analysis of children and contexts: The longitudinal interplay among child maltreatment, community violence, and children’s symptomatology. Dev. Psychopathol. 1998, 10, 235–257. [Google Scholar] [CrossRef]
- Furr, J.M.; Comer, J.S.; Edmunds, J.M.; Kendall, P.C. Disasters and youth: A meta-analytic examination of posttraumatic stress. J. Consult. Clin. Psychol. 2010, 78, 765–780. [Google Scholar] [CrossRef]
- Goldmann, E.; Galea, S. Mental health consequences of disasters. Annu. Rev. Public Health 2014, 35, 169–183. [Google Scholar] [CrossRef]
- Vernberg, E.M.; La Greca, A.M.; Silverman, W.K.; Prinstein, M.J. Prediction of posttraumatic stress symptoms in children after Hurricane Andrew. J. Abnorm. Psychol. 1996, 105, 237–248. [Google Scholar] [CrossRef] [PubMed]
- Davidson, T.M.; Price, M.; McCauley, J.L.; Ruggiero, K.J. Disaster impact across cultural groups: Comparison of Whites, African Americans, and Latinos. Am. J. Community Psychol. 2013, 52, 97–105. [Google Scholar] [CrossRef] [PubMed]
- Norris, F.H.; Friedman, M.J.; Watson, P.J. 60, 000 disaster victims speak: Part II. Summary and implications of the disaster mental health research. Psychiatry 2002, 65, 240–260. [Google Scholar] [CrossRef]
- Adepoju, O.E.; Han, D.; Chae, M.; Smith, K.L.; Gilbert, L.; Choudhury, S.; Woodard, L. Health Disparities and Climate Change: The Intersection of Three Disaster Events on Vulnerable Communities in Houston, Texas. Int. J. Environ. Res. Public Health 2021, 19, 35. [Google Scholar] [CrossRef] [PubMed]
- Flores, A.B.; Collins, T.W.; Grineski, S.E.; Griego, A.L.; Mullen, C.; Nadybal, S.M.; Renteria, R.; Rubio, R.; Shaker, Y.; Trego, S.A. Environmental Injustice in the Disaster Cycle: Hurricane Harvey and the Texas Gulf Coast. Environ. Justice 2021, 14, 146–158. [Google Scholar] [CrossRef]
- Grineski, S.E.; Collins, T.W.; Chakraborty, J. Cascading disasters and mental health inequities: Winter Storm Uri, COVID-19 and post-traumatic stress in Texas. Soc. Sci. Med. (1982) 2022, 315, 115523. [Google Scholar] [CrossRef]
- Norris, F.H.; Elrod, C.L. Psychosocial Consequences of Disaster: A Review of Past Research. In Methods for Disaster Mental Health Research; Norris, F.H., Galea, S., Friedman, M.J., Watson, P.J., Eds.; The Guilford Press: New York, NY, USA, 2006; pp. 20–42. [Google Scholar]
- Gruber, J.; Prinstein, M.J.; Clark, L.A.; Rottenberg, J.; Abramowitz, J.S.; Albano, A.M.; Aldao, A.; Borelli, J.L.; Chung, T.; Davila, J.; et al. Mental health and clinical psychological science in the time of COVID-19: Challenges, opportunities, and a call to action. Am. Psychol. 2020, 76, 409–426. [Google Scholar] [CrossRef]
- Pfefferbaum, B.; North, C.S. Mental Health and the Covid-19 Pandemic. N. Engl. J. Med. 2020, 383, 510–512. [Google Scholar] [CrossRef]
- Ettman, C.K.; Abdalla, S.M.; Cohen, G.H.; Sampson, L.; Vivier, P.M.; Galea, S. Prevalence of Depression Symptoms in US Adults Before and During the COVID-19 Pandemic. JAMA Netw. Open 2020, 3, e2019686. [Google Scholar] [CrossRef]
- Holingue, C.; Badillo-Goicoechea, E.; Riehm, K.E.; Veldhuis, C.B.; Thrul, J.; Johnson, R.M.; Fallin, M.D.; Kreuter, F.; Stuart, E.A.; Kalb, L.G. Mental distress during the COVID-19 pandemic among US adults without a pre-existing mental health condition: Findings from American trend panel survey. Prev. Med. 2020, 139, 106231. [Google Scholar] [CrossRef]
- Holman, E.A.; Thompson, R.R.; Garfin, D.R.; Silver, R.C. The unfolding COVID-19 pandemic: A probability-based, nationally representative study of mental health in the United States. Sci. Adv. 2020, 6, eabd5390. [Google Scholar] [CrossRef] [PubMed]
- Jamil, B.; Su, J. Multidimensional social support and associations between COVID-19 stress and depressive/anxiety outcomes among Hispanic/Latinx and White first-year college students. J. Am. Coll. Health, 2024; 1–12, advance online publication. [Google Scholar] [CrossRef] [PubMed]
- Lipson, S.K.; Zhou, S.; Abelson, S.; Heinze, J.; Jirsa, M.; Morigney, J.; Patterson, A.; Singh, M.; Eisenberg, D. Trends in college student mental health and help-seeking by race/ethnicity: Findings from the national healthy minds study, 2013–2021. J. Affect. Disord. 2022, 306, 138–147. [Google Scholar] [CrossRef]
- Pierce, M.; Hope, H.; Ford, T.; Hatch, S.; Hotopf, M.; John, A.; Kontopantelis, E.; Webb, R.; Wessely, S.; McManus, S.; et al. Mental health before and during the COVID-19 pandemic: A longitudinal probability sample survey of the UK population. Lancet. Psychiatry 2020, 7, 883–892. [Google Scholar] [CrossRef]
- Xiong, J.; Lipsitz, O.; Nasri, F.; Lui LM, W.; Gill, H.; Phan, L.; Chen-Li, D.; Iacobucci, M.; Ho, R.; Majeed, A.; et al. Impact of COVID-19 pandemic on mental health in the general population: A systematic review. J. Affect. Disord. 2020, 277, 55–64. [Google Scholar] [CrossRef]
- Arnett, J. Emerging adulthood: A theory of development from the late teens through the twenties. Am. Psychol. 2000, 55, 469–480. [Google Scholar] [CrossRef]
- Arnett, J. Emerging Adulthood: The Winding Road from the Late Teens through the Twenties; Oxford University Press: Oxford, UK, 2004. [Google Scholar] [CrossRef]
- Tanner, J.L.; Arnett, J.J.; Leis, J.A. Emerging adulthood: Learning and development during the first stage of adulthood. In Handbook of Research on Adult Learning and Development; Smith, M.C., DeFrates-Densch, N., Eds.; Routledge/Taylor & Francis Group: Hoboken, NJ, USA, 2009; pp. 34–67. [Google Scholar]
- American Psychological Association. Stress in America: Stress and Current Events. Stress in America™ Survey. 2019. Available online: https://www.apa.org/news/press/releases/stress/2019/stress-america-2019.pdf (accessed on 15 January 2021).
- Auerbach, R.P.; Mortier, P.; Bruffaerts, R.; Alonso, J.; Benjet, C.; Cuijpers, P.; Demyttenaere, K.; Ebert, D.D.; Green, J.G.; Hasking, P.; et al. WHO World Mental Health Surveys International College Student Project: Prevalence and distribution of mental disorders. J. Abnorm. Psychol. 2018, 127, 623–638. [Google Scholar] [CrossRef]
- Twenge, J.M.; Cooper, A.B.; Joiner, T.E.; Duffy, M.E.; Binau, S.G. Age, period, and cohort trends in mood disorder indicators and suicide-related outcomes in a nationally representative dataset, 2005–2017. J. Abnorm. Psychol. 2019, 128, 185–199. [Google Scholar] [CrossRef]
- Twenge, J.M.; Joiner, T.E. U.S. Census Bureau-assessed prevalence of anxiety and depressive symptoms in 2019 and during the 2020 COVID-19 pandemic. Depress. Anxiety 2020, 37, 954–956. [Google Scholar] [CrossRef]
- Duffy, M.E.; Twenge, J.M.; Joiner, T.E. Trends in mood and anxiety symptoms and suicide-related outcomes among U.S. undergraduates, 2007–2018: Evidence from two national surveys. J. Adolesc. Health 2019, 65, 590–598. [Google Scholar] [CrossRef]
- Lipson, S.K.; Lattie, E.G.; Eisenberg, D. Increased Rates of Mental Health Service Utilization by U.S. College Students: 10-Year Population-Level Trends (2007–2017). Psychiatr. Serv. 2019, 70, 60–63. [Google Scholar] [CrossRef] [PubMed]
- Hawes, M.T.; Szenczy, A.K.; Klein, D.N.; Hajcak, G.; Nelson, B.D. Increases in depression and anxiety symptoms in adolescents and young adults during the COVID-19 pandemic. Psychol. Med. 2022, 52, 3222–3230. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.H.; Zhang, E.; Wong GT, F.; Hyun, S.; Hahm, H.C. Factors associated with depression, anxiety, and PTSD symptomatology during the COVID-19 pandemic: Clinical implications for U.S. young adult mental health. Psychiatry Res. 2020, 290, 113172. [Google Scholar] [CrossRef]
- Zimmermann, M.; Bledsoe, C.; Papa, A. Initial impact of the COVID-19 pandemic on college student mental health: A longitudinal examination of risk and protective factors. Psychiatry Res. 2021, 305, 114254. [Google Scholar] [CrossRef] [PubMed]
- Hawes, M.T.; Szenczy, A.K.; Olino, T.M.; Nelson, B.D.; Klein, D.N. Trajectories of depression, anxiety and pandemic experiences; A longitudinal study of youth in New York during the Spring-Summer of 2020. Psychiatry Res. 2021, 298, 113778. [Google Scholar] [CrossRef]
- Shanahan, L.; Steinhoff, A.; Bechtiger, L.; Murray, A.L.; Nivette, A.; Hepp, U.; Ribeaud, D.; Eisner, M. Emotional distress in young adults during the COVID-19 pandemic: Evidence of risk and resilience from a longitudinal cohort study. Psychol. Med. 2022, 52, 824–833. [Google Scholar] [CrossRef]
- Fisher, C.B.; Tao, X.; Yip, T. The effects of COVID-19 victimization distress and racial bias on mental health among AIAN, Asian, Black, and Latinx young adults. Cult. Divers. Ethn. Minor. Psychol. 2023, 29, 119–131. [Google Scholar] [CrossRef]
- Thomeer, M.B.; Moody, M.D.; Yahirun, J. Racial and Ethnic Disparities in Mental Health and Mental Health Care During The COVID-19 Pandemic. J. Racial Ethn. Health Disparities 2023, 10, 961–976. [Google Scholar] [CrossRef]
- Gray, M.J.; Litz, B.T.; Hsu, J.L.; Lombardo, T.W. Psychometric properties of the life events checklist. Assessment 2004, 11, 330–341. [Google Scholar] [CrossRef]
- Felix, E.; Afifi, T.; Kia-Keating, M.; Brown, L.; Afifi, W.; Reyes, G. Family functioning and posttraumatic growth among parents and youth following wildfire disasters. Am. J. Orthopsychiatry 2015, 85, 191–200. [Google Scholar] [CrossRef] [PubMed]
- Felix, E.; Hernández, L.A.; Bravo, M.; Ramirez, R.; Cabiya, J.; Canino, G. Natural disaster and risk of psychiatric disorders in Puerto Rican children. J. Abnorm. Child Psychol. 2011, 39, 589–600. [Google Scholar] [CrossRef] [PubMed]
- Felix, E.D.; Nylund-Gibson, K.; Kia-Keating, M.; Liu, S.R.; Binmoeller, C.; Terzieva, A. The influence of flood exposure and subsequent stressors on youth social-emotional health. Am. J. Orthopsychiatry 2020, 90, 161–170. [Google Scholar] [CrossRef]
- Felix, E.D.; Binmoeller, C.; Nylund-Gibson, K.; Benight, C.C.; Benner, A.D.; Terzieva, A. Addressing disaster exposure measurement issues with latent class analysis. J. Trauma. Stress 2019, 32, 56–66. [Google Scholar] [CrossRef] [PubMed]
- Spitzer, R.L.; Kroenke, K.; Williams, J.B.; Löwe, B. A brief measure for assessing generalized anxiety disorder: The GAD-7. Arch. Intern. Med. 2006, 166, 1092–1097. [Google Scholar] [CrossRef]
- Lee, E.; Kim, Y. Effect of university students’ sedentary behavior on stress, anxiety, and depression. Perspect. Psychiatr. Care 2019, 55, 164–169. [Google Scholar] [CrossRef]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B. The PHQ-9: Validity of a brief depression severity measure. J. Gen. Intern. Med. 2001, 16, 606–613. [Google Scholar] [CrossRef]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B.; Löwe, B. The Patient Health Questionnaire Somatic, Anxiety, and Depressive Symptom Scales: A systematic review. Gen. Hosp. Psychiatry 2010, 32, 345–359. [Google Scholar] [CrossRef]
- Keum, B.T.; Miller, M.J.; Inkelas, K.K. Testing the factor structure and measurement invariance of the PHQ-9 across racially diverse U.S. college students. Psychol. Assess. 2018, 30, 1096–1106. [Google Scholar] [CrossRef]
- Weathers, F.W.; Litz, B.T.; Keane, T.M.; Palmieri, P.A.; Marx, B.P.; Schnurr, P.P. The PTSD Checklist for DSM-5 (PCL-5). National Center for PTSD. 2013. Available online: https://www.ptsd.va.gov/professional/assessment/adult-sr/ptsd-checklist.asp (accessed on 18 May 2020).
- Blevins, C.A.; Weathers, F.W.; Davis, M.T.; Witte, T.K.; Domino, J.L. The Posttraumatic Stress Disorder Checklist for DSM-5 (PCL-5): Development and Initial Psychometric Evaluation. J. Trauma. Stress 2015, 28, 489–498. [Google Scholar] [CrossRef]
- Faul, F.; Erdfelder, E.; Lang, A.G.; Buchner, A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods 2007, 39, 175–191. [Google Scholar] [CrossRef]
- RMASS; Center for Health Statistics, University of Chicago: Chicago, IL, USA, 2006–2015. Available online: http://www.rmass.org (accessed on 26 April 2021).
- Kapur, K.; Jercan, M.; Bhaumik, D.K.; Gibbons, R.D. Repeated Measures and Sample Size (RMASS) Manual. Available online: http://www.rmass.org/RMASS_Manual.pdf (accessed on 26 April 2021).
- IBM SPSS Statistics for Macintosh; ver. 28.0; IBM Corp: Armonk, NY, USA, 2021.
- Anderson, D.R. Hierarchical Linear Modeling (HLM): An Introduction to Key Concepts within Cross-Sectional and Growth Modeling Frameworks; Technical Report No. 1308; Behavioral Research & Teaching, University of Oregon: Eugene, OR, USA, 2012. Available online: https://files.eric.ed.gov/fulltext/ED545279.pdf (accessed on 11 March 2022).
- Raudenbush, S.W.; Bryk, A.S.; Cheong, Y.F.; Congdon, R. HLM 8 for Windows; ver. 8.0; Scientific Software International, Inc.: Skokie, IL, USA, 2019. [Google Scholar]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B.; Monahan, P.O.; Löwe, B. Anxiety disorders in primary care: Prevalence, impairment, comorbidity, and detection. Ann. Intern. Med. 2007, 146, 317–325. [Google Scholar] [CrossRef]
- Bovin, M.J.; Marx, B.P.; Weathers, F.W.; Gallagher, M.W.; Rodriguez, P.; Schnurr, P.P.; Keane, T.M. Psychometric properties of the PTSD Checklist for Diagnostic and Statistical Manual of Mental Disorders-Fifth Edition (PCL-5) in veterans. Psychol. Assess. 2016, 28, 1379–1391. [Google Scholar] [CrossRef] [PubMed]
- Bonanno, G.A. Loss, Trauma, and Human Resilience: Have We Underestimated the Human Capacity to Thrive After Extremely Aversive Events? Am. Psychol. 2004, 59, 20–28. [Google Scholar] [CrossRef] [PubMed]
- Bonanno, G.A.; Galea, S.; Bucciarelli, A.; Vlahov, D. Psychological Resilience After Disaster: New York City in the Aftermath of the September 11th Terrorist Attack. Psychol. Sci. 2006, 17, 181–186. [Google Scholar] [CrossRef]
- Keya, T.A.; Leela, A.; Habib, N.; Rashid, M.; Bakthavatchalam, P. Mental Health Disorders Due to Disaster Exposure: A Systematic Review and Meta-Analysis. Cureus 2023, 15, e37031. [Google Scholar] [CrossRef]
- Daly, M.; MacLachlan, M.; Maguire, R.; Power, J.M.; Nolan, A.; Shevlin, M.; Spikol, E.; Vallières, F.; Hyland, P. Changes in PTSD, depression, and generalized anxiety before and during the COVID-19 pandemic in Ireland. J. Affect. Disord. Rep. 2021, 5, 100184. [Google Scholar] [CrossRef] [PubMed]
- Young, K.S.; Purves, K.L.; Hübel, C.; Davies, M.R.; Thompson, K.N.; Bristow, S.; Krebs, G.; Danese, A.; Hirsch, C.; Parsons, C.E.; et al. Depression, anxiety and PTSD symptoms before and during the COVID-19 pandemic in the UK. Psychol. Med. 2023, 53, 5428–5441. [Google Scholar] [CrossRef]
- Lee, C.M.; Cadigan, J.M.; Rhew, I.C. Increases in Loneliness Among Young Adults During the COVID-19 Pandemic and Association with Increases in Mental Health Problems. J. Adolesc. Health 2020, 67, 714–717. [Google Scholar] [CrossRef]
- Robinson, E.; Sutin, A.R.; Daly, M.; Jones, A. A systematic review and meta-analysis of longitudinal cohort studies comparing mental health before versus during the COVID-19 pandemic in 2020. J. Affect. Disord. 2022, 296, 567–576. [Google Scholar] [CrossRef]
- Garfin, D.R.; Holman, E.A.; Silver, R.C. Cumulative exposure to prior collective trauma and acute stress responses to the Boston marathon bombings. Psychol. Sci. 2015, 26, 675–683. [Google Scholar] [CrossRef]
- Shrira, A.; Palgi, Y.; Hamama-Raz, Y.; Goodwin, R.; Ben-Ezra, M. Previous exposure to the World Trade Center terrorist attack and posttraumatic symptoms among older adults following Hurricane Sandy. Psychiatry 2014, 77, 374–385. [Google Scholar] [CrossRef]
- Usher, K.; Ranmuthugala, G.; Maple, M.; Durkin, J.; Douglas, L.; Coffey, Y.; Bhullar, N. The 2019–2020 bushfires and COVID-19: The ongoing impact on the mental health of people living in rural and farming communities. Int. J. Ment. Health Nurs. 2021, 30, 3–5. [Google Scholar] [CrossRef] [PubMed]
- Nolen-Hoeksema, S. Emotion regulation and psychopathology: The role of gender. Annu. Rev. Clin. Psychol. 2012, 8, 161–187. [Google Scholar] [CrossRef]
- Garriga-Lopez, A.M. Compounded disasters: Puerto Rico confronts COVID-19 under US colonialism. Soc. Anthropol. 2020, 28, 269–270. [Google Scholar] [CrossRef]
- Morgan, M.L.; Zetzer, H.A. Latinx undergraduates’ navigation in the context of covid-19 and racial injustice. Couns. Psychol. 2022, 50, 415–444. [Google Scholar] [CrossRef]
- Vazqueza, M.; Cortina, J. Hispanic/Latinx College Students’ Mental Health During the COVID-19 Pandemic: The Effects of Familismo and Self-Efficacy. J. Lat. Educ. 2023, 23, 1124–1135. [Google Scholar] [CrossRef]
- Raghavan, S.; Sandanapitchai, P. The relationship between cultural variables and resilience to psychological trauma: A systematic review of the literature. Traumatology 2024, 30, 37–51. [Google Scholar] [CrossRef]
- Hermosilla, S.; Forthal, S.; Sadowska, K.; Magill, E.B.; Watson, P.; Pike, K.M. We need to build the evidence: A systematic review of psychological first aid on mental health and well-being. J. Trauma. Stress 2023, 36, 5–16. [Google Scholar] [CrossRef]
- Hamblen, J.L.; Norris, F.H.; Pietruszkiewicz, S.; Gibson, L.E.; Naturale, A.; Louis, C. Cognitive Behavioral Therapy for Postdisaster Distress: A Community Based Treatment Program for Survivors of Hurricane Katrina. Adm. Policy Ment. Health Ment. Health Serv. Res. 2009, 36, 206–214. [Google Scholar] [CrossRef]
- Lopes, A.P.; Macedo, T.F.; Coutinho, E.S.; Figueira, I.; Ventura, P.R. Systematic review of the efficacy of cognitive-behavior therapy related treatments for victims of natural disasters: A worldwide problem. PloS ONE 2014, 9, e109013. [Google Scholar] [CrossRef]
- Semerci, M.; Uzun, S. The effectiveness of post-disaster psychotherapeutic interventions: A systematic review and meta-analysis study. Asian J. Psychiatry 2023, 85, 103615. [Google Scholar] [CrossRef] [PubMed]
- Jaramillo, N.; Felix, E.D. Understanding the psychosocial impact of the COVID-19 pandemic on Latinx emerging adults. Front. Psychol. 2023, 14, 1066513. [Google Scholar] [CrossRef] [PubMed]
- Ahumada, G.; Cantillan, R.; Jara, B. Social capital and individual well-being in the post-disaster period: The case of Hurricane Maria in Puerto Rico. Int. J. Disaster Risk Reduct. 2024, 103, 104308. [Google Scholar] [CrossRef]


| n | % | |
|---|---|---|
| Sex | ||
| Female | 177 | 86.3 |
| Male | 28 | 13.7 |
| Ethnicity | ||
| Asian | 24 | 11.7 |
| Black | 9 | 4.4 |
| Latinx | 102 | 49.8 |
| White | 49 | 23.9 |
| Mixed/Other | 21 | 10.3 |
| Missing | 1 | 0.5 |
| Region by Disaster | ||
| Mainland U.S. | ||
| Hurricane | 50 | 24.4 |
| Wildfire | 58 | 28.3 |
| Puerto Rico | ||
| Hurricane | 97 | 47.3 |
| Region | ||
| Mainland U.S. | 108 | 25.7 |
| California | 58 | 28.8 |
| Florida | 42 | 20.5 |
| Texas | 8 | 3.9 |
| Puerto Rico | 97 | 47.3 |
| Wave Participation | ||
| Wave 1 | 205 | - |
| Wave 2 | 162 | 79 |
| Wave 3 | 117 | 57.1 |
| Wave 4 | 97 | 47.3 |
| Attrition Rate | ||
| Waves 1–2 | 43 | 21 |
| Waves 2–3 | 45 | 27.8 |
| Waves 3–4 | 20 | 17.1 |
| W1 University Class | ||
| Freshman | 44 | 21.5 |
| Sophomore | 44 | 21.5 |
| Junior | 28 | 13.7 |
| Senior | 48 | 23.4 |
| Graduate Student | 39 | 19 |
| Missing | 2 | 1 |
| M | SD | |
| W1 Age | 21.38 | 3.27 |
| Model 7 Predictors of PTSS Trajectory | |||||
|---|---|---|---|---|---|
| Fixed Effects | Coeff. | SE | t | df | p-Value |
| Initial Status in Model | |||||
| M of Initial Status | 4.13 | 1.03 | 4.00 | 201 | <0.001 |
| Region | 3.06 | 1.40 | 2.18 | 201 | 0.030 |
| Trauma History | 0.76 | 0.37 | 2.04 | 201 | 0.042 |
| Life Stressors Since Disaster | 0.93 | 0.31 | 3.01 | 201 | 0.003 |
| Change Rate in Model | 199 | ||||
| M of Linear Growth Rate | −12.65 | 2.34 | −5.40 | 204 | <0.001 |
| M of Quadratic Growth Rate | 16.42 | 2.61 | 6.29 | 204 | <0.001 |
| M of Cubic Growth Rate | −3.78 | 0.63 | −6.00 | 204 | <0.001 |
| Random Effects | Variance | df | p-value | ||
| Intercept | 64.00 | 44 | <0.001 | ||
| Linear Growth | 300.57 | 49 | <0.001 | ||
| Quadratic Growth | 452.93 | 49 | <0.001 | ||
| Cubic Growth | 27.68 | 49 | <0.001 | ||
| Deviance Statistic (Parameters) | 4162.76 (19) | ||||
| Comparison | χ2(df) | p-value | |||
| Model 6 | 20.91(13) | 0.070 | |||
| Model 5 | 40.61(3) | <0.001 | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Janson, M.; Felix, E.D.; Jaramillo, N.; Sharkey, J.D.; Barnett, M. A Prospective Examination of Mental Health Trajectories of Disaster-Exposed Young Adults in the COVID-19 Pandemic. Behav. Sci. 2024, 14, 787. https://doi.org/10.3390/bs14090787
Janson M, Felix ED, Jaramillo N, Sharkey JD, Barnett M. A Prospective Examination of Mental Health Trajectories of Disaster-Exposed Young Adults in the COVID-19 Pandemic. Behavioral Sciences. 2024; 14(9):787. https://doi.org/10.3390/bs14090787
Chicago/Turabian StyleJanson, Melissa, Erika D. Felix, Natalia Jaramillo, Jill D. Sharkey, and Miya Barnett. 2024. "A Prospective Examination of Mental Health Trajectories of Disaster-Exposed Young Adults in the COVID-19 Pandemic" Behavioral Sciences 14, no. 9: 787. https://doi.org/10.3390/bs14090787
APA StyleJanson, M., Felix, E. D., Jaramillo, N., Sharkey, J. D., & Barnett, M. (2024). A Prospective Examination of Mental Health Trajectories of Disaster-Exposed Young Adults in the COVID-19 Pandemic. Behavioral Sciences, 14(9), 787. https://doi.org/10.3390/bs14090787







