Association between Family Functioning, Child Emotional and Behavioral Problems, and Parental Stress during the COVID-19 Pandemic in Thailand
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Procedures
2.3. Measurements
2.4. Statistical Analysis
3. Results
3.1. Demographic Data of Participants
3.2. Effect of the COVID-19 Pandemic on Children’s Daily Activities
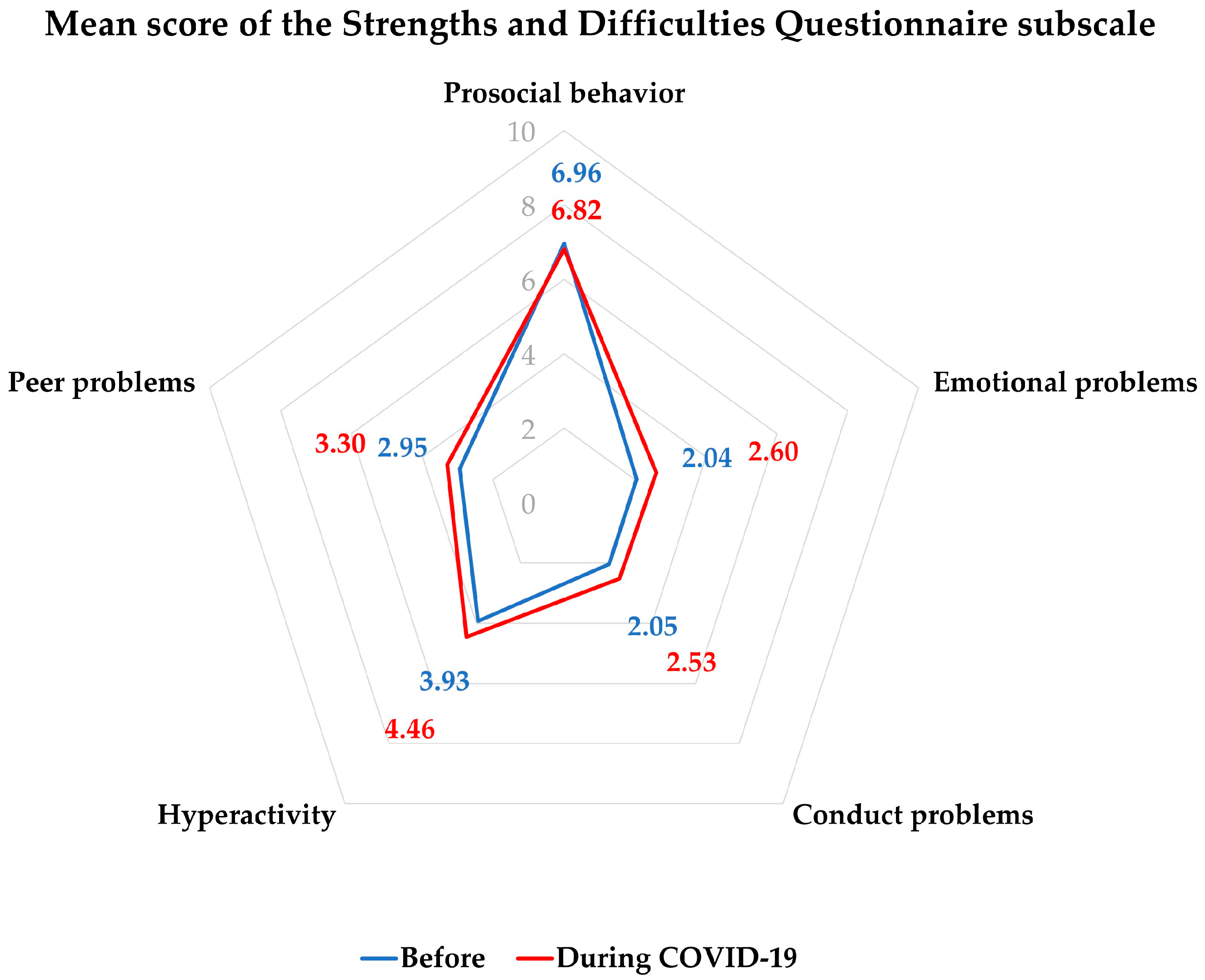
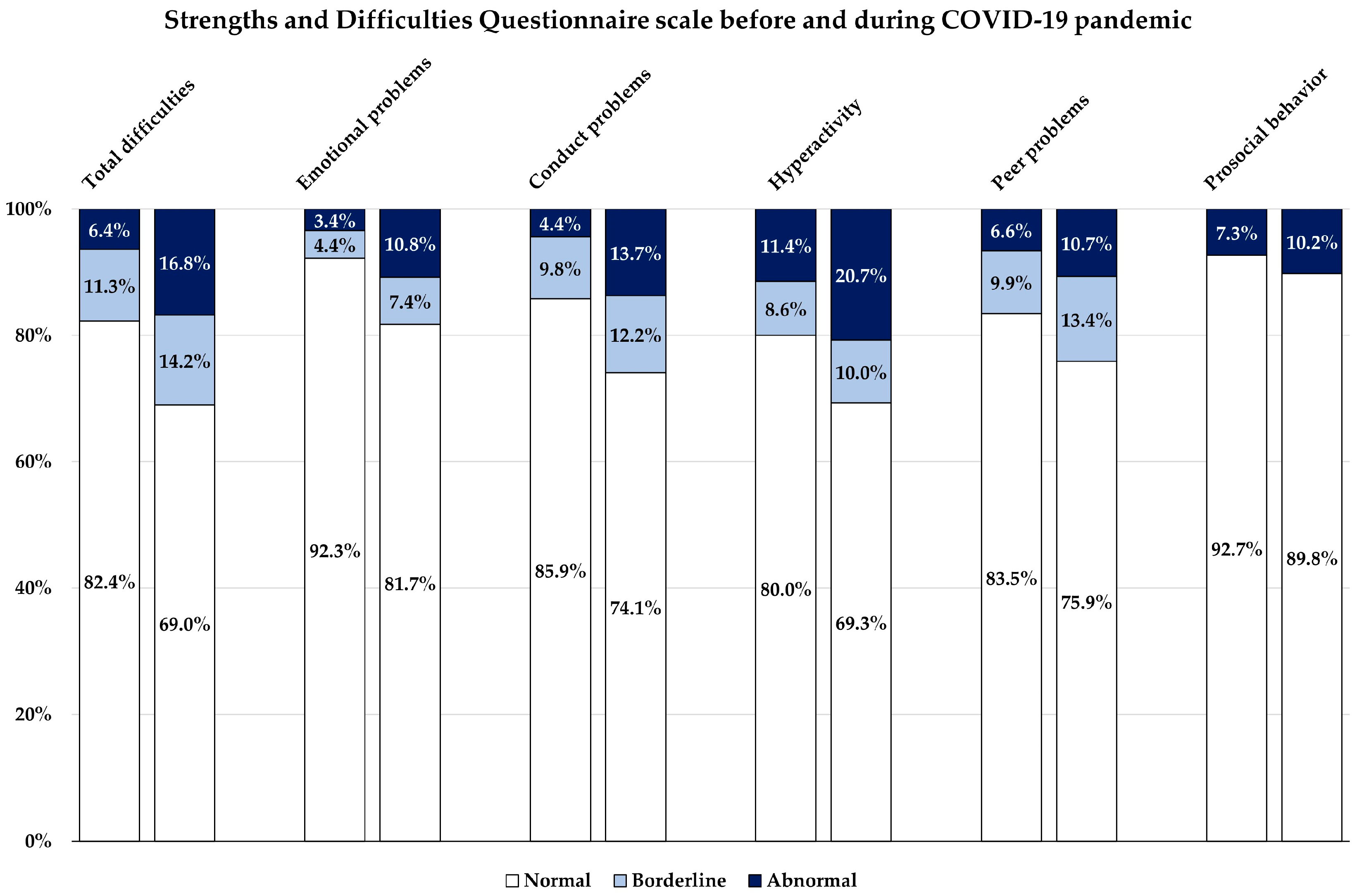
3.3. Emotional and Behavioral Problems Developed Due to the COVID-19 Pandemic
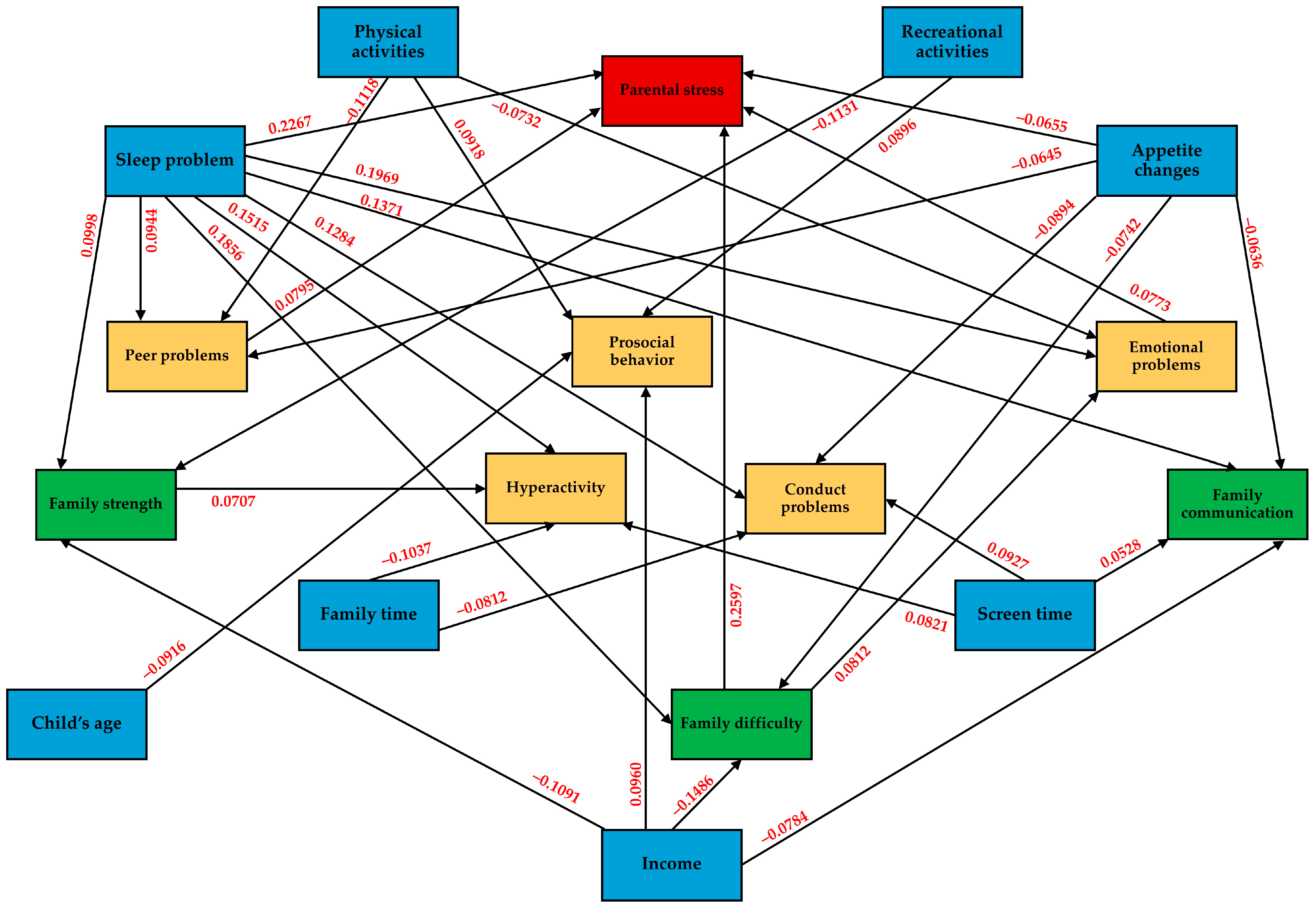
3.4. Association between Parental Stress, Family Functioning, and Children’s Strengths and Difficulties during the COVID-19 Pandemic
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. WHO Director-General’s Opening Remarks at the Media Briefing on COVID-19—11 March 2020. Available online: https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 (accessed on 1 December 2020).
- Cucinotta, D.; Vanelli, M. WHO Declares COVID-19 a Pandemic. Acta Biomed. 2020, 91, 157–160. [Google Scholar] [CrossRef]
- World Health Organization. WHO Coronavirus (COVID-19) Dashboard. Available online: https://covid19.who.int/ (accessed on 1 December 2021).
- Alfano, V.; Ercolano, S. The Efficacy of Lockdown Against COVID-19: A Cross-Country Panel Analysis. Appl. Health Econ. Health Policy 2020, 18, 509–517. [Google Scholar] [CrossRef]
- Trott, M.; Driscoll, R.; Irlado, E.; Pardhan, S. Changes and correlates of screen time in adults and children during the COVID-19 pandemic: A systematic review and meta-analysis. eClinicalMedicine 2022, 48, 101452. [Google Scholar] [CrossRef] [PubMed]
- Meherali, S.; Punjani, N.; Louie-Poon, S.; Abdul Rahim, K.; Das, J.K.; Salam, R.A.; Lassi, Z.S. Mental Health of Children and Adolescents Amidst COVID-19 and Past Pandemics: A Rapid Systematic Review. Int. J. Environ. Res. Public Health 2021, 18, 3432. [Google Scholar] [CrossRef] [PubMed]
- Ren, X.; Huang, W.; Pan, H.; Huang, T.; Wang, X.; Ma, Y. Mental Health During the Covid-19 Outbreak in China: A Meta-Analysis. Psychiatr. Q. 2020, 91, 1033–1045. [Google Scholar] [CrossRef] [PubMed]
- Sameer, A.S.; Khan, M.A.; Nissar, S.; Banday, M.Z. Assessment of Mental Health and Various Coping Strategies among general population living Under Imposed COVID-Lockdown Across world: A Cross-Sectional Study. Ethics Med. Public Health 2020, 15, 100571. [Google Scholar] [CrossRef]
- Anand, P.; Patil, R.S.; Puri, P.; Patil, S. The Psychosocial Effects of Lockdown Due to the COVID-19 Pandemic on Children in 2021. Cureus 2024, 16, e53614. [Google Scholar] [CrossRef]
- Christner, N.; Essler, S.; Hazzam, A.; Paulus, M. Children’s psychological well-being and problem behavior during the COVID-19 pandemic: An online study during the lockdown period in Germany. PLoS ONE 2021, 16, e0253473. [Google Scholar] [CrossRef]
- Panda, P.K.; Gupta, J.; Chowdhury, S.R.; Kumar, R.; Meena, A.K.; Madaan, P.; Sharawat, I.K.; Gulati, S. Psychological and Behavioral Impact of Lockdown and Quarantine Measures for COVID-19 Pandemic on Children, Adolescents and Caregivers: A Systematic Review and Meta-Analysis. J. Trop. Pediatr. 2021, 67, fmaa122. [Google Scholar] [CrossRef]
- Marmor, A.; Cohen, N.; Katz, C. Child Maltreatment During COVID-19: Key Conclusions and Future Directions Based on a Systematic Literature Review. Trauma Violence Abus. 2023, 24, 760–775. [Google Scholar] [CrossRef]
- Viner, R.; Russell, S.; Saulle, R.; Croker, H.; Stansfield, C.; Packer, J.; Nicholls, D.; Goddings, A.L.; Bonell, C.; Hudson, L.; et al. School Closures During Social Lockdown and Mental Health, Health Behaviors, and Well-being Among Children and Adolescents During the First COVID-19 Wave: A Systematic Review. JAMA Pediatr. 2022, 176, 400–409. [Google Scholar] [CrossRef]
- Okuyama, J.; Seto, S.; Fukuda, Y.; Funakoshi, S.; Amae, S.; Onobe, J.; Izumi, S.; Ito, K.; Imamura, F. Mental Health and Physical Activity among Children and Adolescents during the COVID-19 Pandemic. Tohoku J. Exp. Med. 2021, 253, 203–215. [Google Scholar] [CrossRef]
- Chen, M.; Bai, Y.; Fu, M.; Huang, N.; Ahmed, F.; Shahid, M.; Wang, X.; Liu, C.; Feng, X.L.; Guo, J. The Associations Between Parental Burnout and Mental Health Symptoms Among Chinese Parents With Young Children During the COVID-19 Pandemic. Front. Psychiatry 2022, 13, 819199. [Google Scholar] [CrossRef] [PubMed]
- von Suchodoletz, A.; Bélanger, J.; Bryan, C.; Ali, R.; Al Nuaimi, S.R. COVID-19’s shadow on families: A structural equation model of parental stress, family relationships, and child wellbeing. PLoS ONE 2023, 18, e0292292. [Google Scholar] [CrossRef] [PubMed]
- Dayton, L.; Kong, X.; Powell, T.W.; Bowie, J.; Rebok, G.; Strickland, J.C.; Latkin, C. Child Mental Health and Sleep Disturbances During the Early Months of the COVID-19 Pandemic in the United States. Fam. Community Health 2022, 45, 288–298. [Google Scholar] [CrossRef] [PubMed]
- Pudpong, N.; Julchoo, S.; Sinam, P.; Uansri, S.; Kunpeuk, W.; Suphanchaimat, R. Family Health among Families with Primary School Children during the COVID Pandemic in Thailand, 2022. Int. J. Environ. Res. Public Health 2022, 19, 15001. [Google Scholar] [CrossRef] [PubMed]
- Limsuwan, N.; Prachason, T.; Wisajun, P. The changes in family functioning and family happiness during the COVID-19 pandemic: The situation in Thailand. Front. Public Health 2022, 10, 1055819. [Google Scholar] [CrossRef] [PubMed]
- Wongpiromsarn, Y.; Wipulakorn, P.; Nuanmanee, S.; Wolfgang, W.; Mongkol, A. Strengths and Difficulties Questionnaire (SDQ) Thai improved version: Change and administration. J. Ment. Health Thai. 2011, 19, 128–134. [Google Scholar]
- Woerner, W.; Nuanmanee, S.; Becker, A.; Wongpiromsarn, Y.; Mongkol, A. Normative data and psychometric properties of the Thai version of the Strengths and Difficulties Questionnaire (SDQ). J. Ment. Health Thai. 2011, 19, 42–57. [Google Scholar]
- Goodman, R. The Strengths and Difficulties Questionnaire: A research note. J. Child Psychol. Psychiatry 1997, 38, 581–586. [Google Scholar] [CrossRef]
- Carr, A.; Stratton, P. The Score Family Assessment Questionnaire: A Decade of Progress. Fam. Process 2017, 56, 285–301. [Google Scholar] [CrossRef]
- Limsuwan, N.; Prachason, T. Psychometric properties of the SCORE-15 Thai version and its relationship with mental health index. J. Fam. Ther. 2022, 44, 299–312. [Google Scholar] [CrossRef]
- Silpakit, O. Srithanya stress scale. J. Ment. Health Thai. 2012, 16, 177–185. [Google Scholar]
- Schumacker, R.E.; Lomax, R.G. A Beginner’s Guide to Structural Equation Modeling; Psychology Press: London, UK, 2004. [Google Scholar]
- Barrett, P. Structural equation modelling: Adjudging model fit. Personal. Individ. Differ. 2007, 42, 815–824. [Google Scholar] [CrossRef]
- Hu, L.T.; Bentler, P.M. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct. Equ. Model. A Multidiscip. J. 1999, 6, 1–55. [Google Scholar] [CrossRef]
- Dunton, G.F.; Do, B.; Wang, S.D. Early effects of the COVID-19 pandemic on physical activity and sedentary behavior in children living in the U.S. BMC Public Health 2020, 20, 1351. [Google Scholar] [CrossRef] [PubMed]
- Moore, S.A.; Faulkner, G.; Rhodes, R.E.; Brussoni, M.; Chulak-Bozzer, T.; Ferguson, L.J.; Mitra, R.; O’Reilly, N.; Spence, J.C.; Vanderloo, L.M.; et al. Impact of the COVID-19 virus outbreak on movement and play behaviours of Canadian children and youth: A national survey. Int. J. Behav. Nutr. Phys. Act. 2020, 17, 85. [Google Scholar] [CrossRef]
- Carroll, N.; Sadowski, A.; Laila, A.; Hruska, V.; Nixon, M.; Ma, D.W.L.; Haines, J.; On Behalf Of The Guelph Family Health Study. The Impact of COVID-19 on Health Behavior, Stress, Financial and Food Security among Middle to High Income Canadian Families with Young Children. Nutrients 2020, 12, 2352. [Google Scholar] [CrossRef] [PubMed]
- Pfefferbaum, B.; Van Horn, R.L. Physical Activity and Sedentary Behavior in Children During the COVID-19 Pandemic: Implications for Mental Health. Curr. Psychiatry Rep. 2022, 24, 493–501. [Google Scholar] [CrossRef]
- Widyastari, D.A.; Saonuam, P.; Pongpradit, K.; Wongsingha, N.; Choolers, P.; Kesaro, S.; Thangchan, W.; Pongpaopattanakul, P.; Phankasem, K.; Musor, M.E.; et al. Results from the Thailand 2022 report card on physical activity for children and youth. J. Exerc. Sci. Fit. 2022, 20, 276–282. [Google Scholar] [CrossRef]
- Hossain, M.M.; Nesa, F.; Das, J.; Aggad, R.; Tasnim, S.; Bairwa, M.; Ma, P.; Ramirez, G. Global burden of mental health problems among children and adolescents during COVID-19 pandemic: An umbrella review. Psychiatry Res. 2022, 317, 114814. [Google Scholar] [CrossRef] [PubMed]
- Rajatanavin, N.; Tuangratananon, T.; Suphanchaimat, R.; Tangcharoensathien, V. Responding to the COVID-19 second wave in Thailand by diversifying and adapting lessons from the first wave. BMJ Glob. Health 2021, 6, e006178. [Google Scholar] [CrossRef] [PubMed]
- Stiglic, N.; Viner, R.M. Effects of screentime on the health and well-being of children and adolescents: A systematic review of reviews. BMJ Open 2019, 9, e023191. [Google Scholar] [CrossRef]
- Lund, L.; Sølvhøj, I.N.; Danielsen, D.; Andersen, S. Electronic media use and sleep in children and adolescents in western countries: A systematic review. BMC Public Health 2021, 21, 1598. [Google Scholar] [CrossRef]
- Muppalla, S.K.; Vuppalapati, S.; Reddy Pulliahgaru, A.; Sreenivasulu, H. Effects of Excessive Screen Time on Child Development: An Updated Review and Strategies for Management. Cureus 2023, 15, e40608. [Google Scholar] [CrossRef] [PubMed]
- Hosokawa, R.; Katsura, T. Association between mobile technology use and child adjustment in early elementary school age. PLoS ONE 2018, 13, e0199959. [Google Scholar] [CrossRef]
- Vandekerckhove, M.; Wang, Y.L. Emotion, emotion regulation and sleep: An intimate relationship. AIMS Neurosci. 2018, 5, 1–17. [Google Scholar] [CrossRef]
- Werling, A.M.; Walitza, S.; Grünblatt, E.; Drechsler, R. Media use before, during and after COVID-19 lockdown according to parents in a clinically referred sample in child and adolescent psychiatry: Results of an online survey in Switzerland. Compr. Psychiatry 2021, 109, 152260. [Google Scholar] [CrossRef]
- Li, B.; Ng, K.; Tong, X.; Zhou, X.; Ye, J.; Yu, J.J. Physical activity and mental health in children and youth during COVID-19: A systematic review and meta-analysis. Child Adolesc. Psychiatry Ment. Health 2023, 17, 92. [Google Scholar] [CrossRef]
- Wan, Y.; Zhao, Y.; Song, H. Effects of Physical Exercise on Prosocial Behavior of Junior High School Students. Children 2021, 8, 1199. [Google Scholar] [CrossRef]
- Li, J.; Shao, W. Influence of Sports Activities on Prosocial Behavior of Children and Adolescents: A Systematic Literature Review. Int. J. Environ. Res. Public Health 2022, 19, 6484. [Google Scholar] [CrossRef]
- Moulin, F.; Bailhache, M.; Monnier, M.; Thierry, X.; Vandentorren, S.; Côté, S.M.; Falissard, B.; Simeon, T.; Geay, B.; Marchand, L.; et al. Longitudinal impact of psychosocial status on children’s mental health in the context of COVID-19 pandemic restrictions. Eur. Child Adolesc. Psychiatry 2022, 32, 1073–1082. [Google Scholar] [CrossRef]
- Kerr, M.L.; Rasmussen, H.F.; Fanning, K.A.; Braaten, S.M. Parenting During COVID-19: A Study of Parents’ Experiences Across Gender and Income Levels. Fam. Relat. 2021, 70, 1327–1342. [Google Scholar] [CrossRef]
- Riany, Y.E.; Morawska, A. Financial and Work Burden, Psychosocial Functioning, and Family Interactions During the COVID-19 Pandemic in Indonesia: Effects on Child Outcomes. Child. Psychiatry Hum. Dev. 2021, 54, 340–351. [Google Scholar] [CrossRef] [PubMed]
- Adegboye, D.; Williams, F.; Collishaw, S.; Shelton, K.; Langley, K.; Hobson, C.; Burley, D.; van Goozen, S. Understanding why the COVID-19 pandemic-related lockdown increases mental health difficulties in vulnerable young children. JCPP Adv. 2021, 1, e12005. [Google Scholar] [CrossRef] [PubMed]
- Wang, M.T.; Henry, D.A.; Del Toro, J.; Scanlon, C.L.; Schall, J.D. COVID-19 Employment Status, Dyadic Family Relationships, and Child Psychological Well-Being. J. Adolesc. Health 2021, 69, 705–712. [Google Scholar] [CrossRef] [PubMed]
- Sum, K.K.; Cai, S.; Law, E.; Cheon, B.; Tan, G.; Loo, E.; Lee, Y.S.; Yap, F.; Chan, J.K.Y.; Daniel, M.; et al. COVID-19-Related Life Experiences, Outdoor Play, and Long-term Adiposity Changes Among Preschool- and School-Aged Children in Singapore 1 Year After Lockdown. JAMA Pediatr. 2022, 176, 280–289. [Google Scholar] [CrossRef] [PubMed]
- Khanijahani, A.; Iezadi, S.; Gholipour, K.; Azami-Aghdash, S.; Naghibi, D. A systematic review of racial/ethnic and socioeconomic disparities in COVID-19. Int. J. Equity Health 2021, 20, 248. [Google Scholar] [CrossRef] [PubMed]
- Zahry, N.R.; Ling, J.; Robbins, L.B. Mental health and lifestyle behavior changes during COVID-19 among families living in poverty: A descriptive phenomenological study. J. Child Adolesc. Psychiatr. Nurs. 2024, 37, e12447. [Google Scholar] [CrossRef] [PubMed]
- Marcus, S.M.; Marcus, T.S. Infrastructural Inequality and Household COVID-19 Vulnerability in a South African Urban Settlement. J. Urban Health 2022, 99, 571–581. [Google Scholar] [CrossRef]
- Li, W.; Wang, Z.; Wang, G.; Ip, P.; Sun, X.; Jiang, Y.; Jiang, F. Socioeconomic inequality in child mental health during the COVID-19 pandemic: First evidence from China. J. Affect. Disord. 2021, 287, 8–14. [Google Scholar] [CrossRef]
- MacKenzie, N.E.; Keys, E.; Hall, W.A.; Gruber, R.; Smith, I.M.; Constantin, E.; Godbout, R.; Stremler, R.; Reid, G.J.; Hanlon-Dearman, A.; et al. Children’s Sleep During COVID-19: How Sleep Influences Surviving and Thriving in Families. J. Pediatr. Psychol. 2021, 46, 1051–1062. [Google Scholar] [CrossRef]
- Wang, P.; Sun, X.; Li, W.; Wang, Z.; He, S.; Zhai, F.; Xin, Y.; Pan, L.; Wang, G.; Jiang, F.; et al. Mental Health of Parents and Preschool-Aged Children During the COVID-19 Pandemic: The Mediating Role of Harsh Parenting and Child Sleep Disturbances. Front. Psychiatry 2021, 12, 746330. [Google Scholar] [CrossRef]
- Zhao, J.; Xu, J.; He, Y.; Xiang, M. Children and adolescents’ sleep patterns and their associations with mental health during the COVID-19 pandemic in Shanghai, China. J. Affect. Disord. 2022, 301, 337–344. [Google Scholar] [CrossRef]
- Philippe, K.; Chabanet, C.; Issanchou, S.; Monnery-Patris, S. Child eating behaviors, parental feeding practices and food shopping motivations during the COVID-19 lockdown in France: (How) did they change? Appetite 2021, 161, 105132. [Google Scholar] [CrossRef]
- Kamaleddine, A.N.; Antar, H.A.; Ali, B.T.A.; Hammoudi, S.F.; Lee, J.; Lee, T.; Bhang, S.Y.; Chung, S.; Salameh, P. Effect of Screen Time on Physical and Mental Health and Eating Habits During COVID-19 Lockdown in Lebanon. Psychiatry Investig. 2022, 19, 220–228. [Google Scholar] [CrossRef]
- Radwan, A.; Radwan, E.; Radwan, W. Eating habits among primary and secondary school students in the Gaza Strip, Palestine: A cross-sectional study during the COVID-19 pandemic. Appetite 2021, 163, 105222. [Google Scholar] [CrossRef] [PubMed]
- Brakspear, L.; Boules, D.; Nicholls, D.; Burmester, V. The Impact of COVID-19-Related Living Restrictions on Eating Behaviours in Children and Adolescents: A Systematic Review. Nutrients 2022, 14, 3657. [Google Scholar] [CrossRef] [PubMed]
- Juli, M.R.; Juli, R.; Juli, G.; Juli, L. Eating Disorders: The Role of the Family in Development and Maintenance of Children’s Problems in the Pandemic Period. Psychiatr. Danub. 2022, 34, 122–128. [Google Scholar] [PubMed]
- Krom, H.; van Mameren, J.; Remijn, L.; de Nennie, K.; Dumont, E.; van der Gaag, E.; van Leeuwen, M.C.C.; Mulkens, S.; Schakelaar, C.; Kindermann, A. Impact of COVID-19 Pandemic on Young Children With Feeding and Eating Problems and Disorders and Their Families. J. Pediatr. Gastroenterol. Nutr. 2022, 75, 529–534. [Google Scholar] [CrossRef] [PubMed]
- González, L.M.; Lammert, A.; Phelan, S.; Ventura, A.K. Associations between parenting stress, parent feeding practices, and perceptions of child eating behaviors during the COVID-19 pandemic. Appetite 2022, 177, 106148. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Tee, M.; Roy, A.E.; Fardin, M.A.; Srichokchatchawan, W.; Habib, H.A.; Tran, B.X.; Hussain, S.; Hoang, M.T.; Le, X.T.; et al. The impact of COVID-19 pandemic on physical and mental health of Asians: A study of seven middle-income countries in Asia. PLoS ONE 2021, 16, e0246824. [Google Scholar] [CrossRef] [PubMed]
- Bureau of Information and Communication Technology, Ministry of Education. Educational Statistics 2020; Bureau of Information and Communication Technology, Ministry of Education: Bangkok, Thailand, 2021; pp. 38–39.
| Demographic | n (%) or Mean [SD] |
|---|---|
| Caregiver characteristics | |
| Father | 46 (4.9) |
| Mother | 837 (88.9) |
| Others | 59 (6.2) |
| Region (missing = 1) | |
| Central | 687 (73.0) |
| North | 118 (12.5) |
| Northeast | 55 (5.8) |
| South | 81 (8.6) |
| Education level | |
| Undergraduate | 111 (11.8) |
| Bachelor’s degree | 540 (57.3) |
| Higher degree | 291 (30.9) |
| Household income (USD/month) a | |
| <300 | 31 (3.3) |
| 300–900 | 236 (25.1) |
| 901–1500 | 233 (24.7) |
| 1501–3000 | 221 (23.5) |
| >3000 | 221 (23.5) |
| Sex of child | |
| Male | 491 (52.1) |
| Female | 451 (47.9) |
| Type of schools | |
| Private | 567 (60.2) |
| Government | 263 (27.9) |
| Demonstrate | 57 (6.1) |
| International | 50 (5.3) |
| Psychiatric diagnosis of child | |
| Yes | 151 (16.0) |
| No | 791 (84) |
| Age of children (years) [Min = 5, Max = 15] | 8.54 [1.87] |
| Effects | n (%) or Mean [SD] |
|---|---|
| COVID-19 infection | |
| Child infected | 1 (0.1) |
| Parent infected | 1 (0.1) |
| Child quarantined due to being in a high-risk group | 13 (1.4) |
| Parent quarantined due to being in high-risk group | 21 (2.2) |
| Sleep problems | |
| The problem has just presented or with more severity | 243 (25.8) |
| The problem presented before and with equal severity | 113 (12.0) |
| Problem presented before but with less severity | 9 (1.0) |
| Appetite | |
| Decrease | 475 (50.4) |
| Increase | 365 (38.7) |
| Same | 102 (10.8) |
| Physical activities | |
| <1 h/day | 548 (58.2) |
| 1–2 h/day | 303 (32.2) |
| >2 h/day | 91 (9.7) |
| Recreational activities | |
| <1 h/day | 292 (31.0) |
| 1–2 h/day | 351 (37.3) |
| >2 h/day | 299 (31.7) |
| Family time | |
| <1 h/day | 340 (36.1) |
| 1–2 h/day | 337 (35.8) |
| >2 h/day | 265 (28.1) |
| Screen time during COVID-19 pandemic | |
| Increased from before pandemic | 811 (86.1) |
| Decreased from before pandemic | 101 (10.7) |
| Same as before pandemic | 30 (3.2) |
| Duration of screen time | |
| <3 h/day | 291 (30.9) |
| 3–5 h/day | 297 (31.5) |
| >5 h/day | 213 (22.6) |
| >7 h/day | 141 (15.0) |
| Online classes | |
| No | 149 (15.8) |
| 1–3 h/day | 480 (50.9) |
| 3–5 h/day | 238 (25.3) |
| 5–7 h/day | 75 (8) |
| Parental supervision during screen time | |
| No | 48 (5.1) |
| Sometimes | 278 (29.5) |
| Often | 356 (37.8) |
| Always | 260 (27.6) |
| SDQ Scale (Range) | n (%) or Mean [SD] | p-Value a | |
|---|---|---|---|
| Before | After | ||
| Total difficulties (0–40) | 10.98 [4.81] | 12.90 [5.88] | <0.001 * |
| Normal (0–15) | 776 (82.4%) | 650 (69.0%) | <0.001 * |
| Borderline (16–18) | 106 (11.3%) | 134 (14.2%) | |
| Abnormal (19–40) | 60 (6.4%) | 158 (16.8%) | |
| Emotional problems (0–10) | 2.04 [1.69] | 2.60 [2.13] | <0.001 * |
| Normal (0–4) | 869 (92.3%) | 770 (81.7%) | <0.001 * |
| Borderline (5) | 41 (4.4%) | 70 (7.4%) | |
| Abnormal (6–10) | 32 (3.4%) | 102 (10.8%) | |
| Conduct problems (0–10) | 2.05 [1.41] | 2.53 [1.75] | <0.001 * |
| Normal (0–3) | 809 (85.9%) | 698 (74.1%) | <0.001 * |
| Borderline (4) | 92 (9.8%) | 115 (12.2%) | |
| Abnormal (5–10) | 41 (4.4%) | 129 (13.7%) | |
| Hyperactivity (0–10) | 3.93 [2.12] | 4.46 [2.42] | <0.001 * |
| Normal (0–5) | 754 (80.0%) | 653 (69.3%) | <0.001 * |
| Borderline (6) | 81 (8.6%) | 94 (10.0%) | |
| Abnormal (7–10) | 107 (11.4%) | 195 (20.7%) | |
| Peer problems (0–10) | 2.95 [1.61] | 3.30 [1.72] | <0.001 * |
| Normal (0–4) | 787 (83.5%) | 715 (75.9%) | <0.001 * |
| Borderline (5) | 93 (9.9%) | 126 (13.4%) | |
| Abnormal (6–10) | 62 (6.6%) | 101 (10.7%) | |
| Prosocial behavior (0–10) | 6.96 [1.89] | 6.82 [1.98] | <0.001 * |
| Normal (5–10) | 873 (92.7%) | 846 (89.8%) | <0.001 * |
| Abnormal (0–4) | 69 (7.3%) | 97 (10.2%) | |
| Variables | β | (95% CI) | p-Value |
|---|---|---|---|
| Parental stress | |||
| Emotional problems change | 0.0773 | (0.0099, 0.1446) | 0.025 * |
| Conduct problems change | 0.0208 | (−0.0521, 0.0936) | 0.576 |
| Hyperactivity change | 0.0633 | (−0.0059, 0.1326) | 0.073 |
| Peer problems change | 0.0795 | (0.0183, 0.1408) | 0.011 * |
| Family strength | 0.0491 | (−0.0114, 0.1095) | 0.111 |
| Family difficulty | 0.2597 | (0.1867, 0.3327) | <0.001 * |
| Family communication | −0.0364 | (−0.1117, 0.0389) | 0.343 |
| Child’s age | −0.0522 | (−0.1108, 0.0063) | 0.080 |
| Psychiatric diagnosis | 0.0489 | (−0.0077, 0.1054) | 0.090 |
| Sleep problems | 0.2267 | (0.1692, 0.2842) | <0.001 * |
| Appetite changes | −0.0655 | (−0.1224, −0.0086) | 0.024 * |
| Physical activities ≥ 1 h/day | −0.0317 | (−0.0894, 0.0260) | 0.282 |
| Screen time ≥ 3 h/day | 0.0472 | (−0.0118, 0.1061) | 0.117 |
| Emotional problems change | |||
| Family difficulty | 0.0812 | (0.0064, 0.1560) | 0.033 * |
| Family communication | 0.0077 | (−0.0647, 0.0801) | 0.834 |
| Psychiatric diagnosis | 0.0210 | (−0.0324, 0.0743) | 0.441 |
| Sleep problems | 0.1969 | (0.1351, 0.2587) | <0.001 * |
| Appetite changes | −0.0478 | (−0.1102, 0.0145) | 0.133 |
| Physical activities ≥ 1 h/day | −0.0732 | (−0.1355, −0.0109) | 0.021* |
| Recreational activities ≥ 1 h/day | −0.0241 | (−0.0851, 0.0370) | 0.439 |
| Screen time ≥ 3 h/day | 0.0467 | (−0.0146, 0.1081) | 0.136 |
| Conduct problems change | |||
| Family strength | 0.0417 | (−0.0147, 0.0981) | 0.147 |
| Family difficulty | 0.0413 | (−0.0303, 0.1129) | 0.259 |
| Family communication | 0.0070 | (−0.0610, 0.0749) | 0.841 |
| Sleep problems | 0.1284 | (0.0659, 0.1909) | <0.001 * |
| Appetite changes | −0.0894 | (−0.1516, −0.0272) | 0.005 * |
| Physical activities ≥ 1 h/day | −0.0096 | (−0.0735, 0.0543) | 0.769 |
| Recreational activities ≥ 1 h/day | −0.0497 | (−0.1159, 0.0165) | 0.141 |
| Family time ≥ 1 h/day | −0.0812 | (−0.1424, −0.0199) | 0.009 * |
| Screen time ≥ 3 h/day | 0.0927 | (0.0311, 0.1543) | 0.003 * |
| Hyperactivity change | |||
| Family strength | 0.0707 | (0.0134, 0.1280) | 0.016 * |
| Family difficulty | 0.0054 | (−0.0544, 0.0652) | 0.860 |
| Sleep problems | 0.1515 | (0.0893, 0.2138) | <0.001 * |
| Appetite changes | −0.0408 | (−0.1033, 0.0217) | 0.201 |
| Physical activities ≥ 1 h/day | −0.0505 | (−0.1144, 0.0134) | 0.121 |
| Recreational activities ≥ 1 h/day | −0.0186 | (−0.0859, 0.0487) | 0.587 |
| Family time ≥ 1 h/day | −0.1037 | (−0.1678, −0.0396) | 0.002 * |
| Screen time ≥ 3 h/day | 0.0821 | (0.0199, 0.1443) | 0.010 * |
| Peer problems change | |||
| Sleep problems | 0.0944 | (0.0312, 0.1577) | 0.003 * |
| Appetite changes | −0.0645 | (−0.1280, −0.0011) | 0.046 * |
| Physical activities ≥ 1 h/day | −0.1118 | (−0.1743, −0.0493) | <0.001 * |
| Prosocial behavior change | |||
| Income > 900 USD | 0.0960 | (0.0404, 0.1516) | 0.001 * |
| Child’s age | −0.0916 | (−0.1502, −0.0331) | 0.002 * |
| Sleep problems | −0.0566 | (−0.1195, 0.0062) | 0.077 |
| Appetite changes | 0.0610 | (−0.0018, 0.1239) | 0.057 |
| Physical activities ≥ 1 h/day | 0.0918 | (0.0273, 0.1563) | 0.005 * |
| Recreational activities ≥ 1 h/day | 0.0896 | (0.0221, 0.1572) | 0.009 * |
| Family time ≥ 1 h/day | 0.0232 | (−0.0443, 0.0906) | 0.500 |
| Screen time ≥ 3 h/day | −0.0048 | (−0.0682, 0.0586) | 0.882 |
| Family strength | |||
| Income > 900 USD | −0.1091 | (−0.1710, −0.0473) | 0.001 * |
| Sleep problems | 0.0998 | (0.0372, 0.1624) | 0.002 * |
| Appetite changes | −0.0362 | (−0.0995, 0.0270) | 0.261 |
| Physical activities ≥ 1 h/day | −0.0476 | (−0.1087, 0.0134) | 0.126 |
| Recreational activities ≥ 1 h/day | −0.1131 | (−0.1794, −0.0468) | 0.001 * |
| Family time ≥ 1 h/day | −0.0220 | (−0.0890, 0.0450) | 0.521 |
| Screen time ≥ 3 h/day | 0.0234 | (−0.0402, 0.0869) | 0.471 |
| Family difficulty | |||
| Income > 900 USD | −0.1486 | (−0.2092, −0.0880) | <0.001 * |
| Child’s age | −0.0297 | (−0.0792, 0.0199) | 0.241 |
| Psychiatric diagnosis | 0.0423 | (−0.0061, 0.0907) | 0.087 |
| Sleep problems | 0.1856 | (0.1247, 0.2465) | <0.001 * |
| Appetite changes | −0.0742 | (−0.1363, −0.0121) | 0.019 * |
| Recreational activities ≥ 1 h/day | −0.0346 | (−0.0843, 0.0151) | 0.173 |
| Family communication | |||
| Income > 900 USD | −0.0784 | (−0.1409, −0.0159) | 0.014 * |
| Sleep problems | 0.1371 | (0.0745, 0.1996) | <0.001 * |
| Appetite changes | −0.0636 | (−0.1270, −0.0003) | 0.049 * |
| Screen time ≥ 3 h/day | 0.0528 | (0.0027, 0.1028) | 0.039 * |
| RMSEA | 0.017 | ||
| SRMR | 0.019 | ||
| CFI | 0.995 | ||
| TLI | 0.985 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jetiyanuwat, S.; Kawilapat, S.; Narkpongphun, A.; Pojanapotha, P. Association between Family Functioning, Child Emotional and Behavioral Problems, and Parental Stress during the COVID-19 Pandemic in Thailand. Behav. Sci. 2024, 14, 270. https://doi.org/10.3390/bs14040270
Jetiyanuwat S, Kawilapat S, Narkpongphun A, Pojanapotha P. Association between Family Functioning, Child Emotional and Behavioral Problems, and Parental Stress during the COVID-19 Pandemic in Thailand. Behavioral Sciences. 2024; 14(4):270. https://doi.org/10.3390/bs14040270
Chicago/Turabian StyleJetiyanuwat, Sawitree, Suttipong Kawilapat, Assawin Narkpongphun, and Pichaya Pojanapotha. 2024. "Association between Family Functioning, Child Emotional and Behavioral Problems, and Parental Stress during the COVID-19 Pandemic in Thailand" Behavioral Sciences 14, no. 4: 270. https://doi.org/10.3390/bs14040270
APA StyleJetiyanuwat, S., Kawilapat, S., Narkpongphun, A., & Pojanapotha, P. (2024). Association between Family Functioning, Child Emotional and Behavioral Problems, and Parental Stress during the COVID-19 Pandemic in Thailand. Behavioral Sciences, 14(4), 270. https://doi.org/10.3390/bs14040270






