Devastating Wildfires and Mental Health: Major Depressive Disorder Prevalence and Associated Factors among Residents in Alberta and Nova Scotia, Canada
Abstract
1. Introduction
2. Methodology
2.1. Study Setting
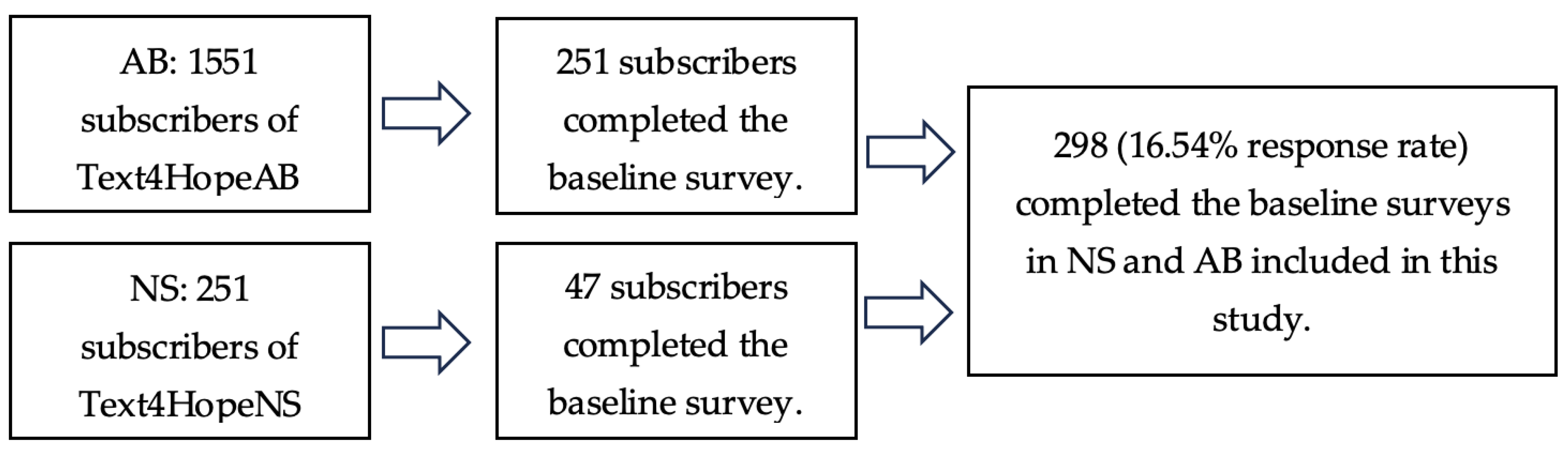
2.2. Study Design, Data Collection, and Ethical Consideration
2.3. Sample Size Estimation
2.4. Statistical Analysis
3. Results
3.1. Univariate Analysis
3.2. Logistic Regression
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Wildfires: Information & Facts. Canadian Red Cross. Available online: https://www.redcross.ca/how-we-help/emergencies-and-disasters-in-canada/types-of-emergencies/wildfires/wildfires-information-facts (accessed on 10 August 2023).
- Hundreds of Fires Are Out of Control in Canada’s Worst-Ever Season. Available online: https://www.bloomberg.com/news/articles/2023-06-07/hundreds-of-fires-are-out-of-control-in-canada-s-worst-ever-season (accessed on 10 August 2023).
- The 7 Largest Wildfires in North American History. Available online: https://www.propertycasualty360.com/2014/07/23/the-7-largest-wildfires-in-north-american-history/?slreturn=20240204223045 (accessed on 10 August 2023).
- It’s Canada’s Worst Fire Season in Modern History, as Smoke Fills Skies. 2023. Available online: https://www.washingtonpost.com/weather/2023/06/26/canada-wildfire-worst-season-quebec-ontario-smoke/ (accessed on 10 August 2023).
- Zimonjic, P. Canada Still Faces a High Risk of Wildfires for the Rest of The summer, Government Warns. 2023. Available online: https://www.cbc.ca/news/politics/federl-wildfire-record-worst-summer-1.6898955 (accessed on 8 August 2023).
- Malekian, S.; Ogao, E.; Beaule, V. Canada Marks Worst Wildfire Season on Record. 2023. Available online: https://abcnews.go.com/International/International/canada-marks-worst-wildfire-season-record/story?id=100474336 (accessed on 8 August 2023).
- Forest Fire Centre Declares 2023 Worst Year Ever for Canadian Wildfires. Available online: https://www.theglobeandmail.com/canada/article-quebec-wildfire-smoke-causes-widespread-smog-warnings-grounds-some/ (accessed on 10 August 2023).
- How Large Are the Canadian Wildfires, and Who Is Suffering the Smoke? Available online: https://www.washingtonpost.com/climate-environment/2023/06/07/canada-wildfires-weather-air-quality/ (accessed on 10 August 2023).
- Grant, E.; Runkle, J.D. Long-term health effects of wildfire exposure: A scoping review. J. Clim. Change Health 2022, 6, 100110. [Google Scholar] [CrossRef]
- Mao, W.; Adu, M.; Eboreime, E.; Shalaby, R.; Nkire, N.; Agyapong, B.; Pazderka, H.; Obuobi-Donkor, G.; Owusu, E.; Oluwasina, F. Post-traumatic stress disorder, major depressive disorder, and wildfires: A fifth-year postdisaster evaluation among residents of Fort McMurray. Int. J. Environ. Res. Public Health 2022, 19, 9759. [Google Scholar] [CrossRef]
- Reid, C.E.; Maestas, M.M. Wildfire smoke exposure under climate change: Impact on respiratory health of affected communities. Curr. Opin. Pulm. Med. 2019, 25, 179. [Google Scholar] [CrossRef]
- Doerr, S.H.; Santín, C. Global trends in wildfire and its impacts: Perceptions versus realities in a changing world. Philos. Trans. R. Soc. B Biol. Sci. 2016, 371, 20150345. [Google Scholar] [CrossRef]
- Cohen, J.R.; Adams, Z.W.; Menon, S.V.; Youngstrom, E.A.; Bunnell, B.E.; Acierno, R.; Ruggiero, K.J.; Danielson, C.K. How should we screen for depression following a natural disaster? An ROC approach to post-disaster screening in adolescents and adults. J. Affect. Disord. 2016, 202, 102–109. [Google Scholar] [CrossRef]
- Association, A.P. What Is Depression? Available online: https://www.psychiatry.org/patients-families/depression/what-is-depression (accessed on 8 August 2023).
- McDermott, B.M.; Lee, E.M.; Judd, M.; Gibbon, P. Posttraumatic stress disorder and general psychopathology in children and adolescents following a wildfire disaster. Can. J. Psychiatry 2005, 50, 137–143. [Google Scholar] [CrossRef]
- Papadatou, D.; Giannopoulou, I.; Bitsakou, P.; Bellali, T.; Talias, M.A.; Tselepi, K. Adolescents’ reactions after a wildfire disaster in Greece. J. Trauma. Stress 2012, 25, 57–63. [Google Scholar] [CrossRef] [PubMed]
- Belleville, G.; Ouellet, M.-C.; Morin, C.M. Post-traumatic stress among evacuees from the 2016 Fort McMurray wildfires: Exploration of psychological and sleep symptoms three months after the evacuation. Int. J. Environ. Res. Public Health 2019, 16, 1604. [Google Scholar] [CrossRef] [PubMed]
- Marshall, G.N.; Schell, T.L.; Elliott, M.N.; Rayburn, N.R.; Jaycox, L.H. Psychiatric disorders among adults seeking emergency disaster assistance after a wildland-urban interface fire. Psychiatr. Serv. 2007, 58, 509–514. [Google Scholar] [CrossRef] [PubMed]
- Tang, B.; Liu, X.; Liu, Y.; Xue, C.; Zhang, L. A meta-analysis of risk factors for depression in adults and children after natural disasters. BMC Public Health 2014, 14, 623. [Google Scholar] [CrossRef] [PubMed]
- Agyapong, V.I.; Ritchie, A.; Brown, M.R.; Noble, S.; Mankowsi, M.; Denga, E.; Nwaka, B.; Akinjise, I.; Corbett, S.E.; Moosavi, S. Long-term mental health effects of a devastating wildfire are amplified by socio-demographic and clinical antecedents in elementary and high school staff. Front. Psychiatry 2020, 11, 448. [Google Scholar] [CrossRef]
- Moosavi, S.; Nwaka, B.; Akinjise, I.; Corbett, S.E.; Chue, P.; Greenshaw, A.J.; Silverstone, P.H.; Li, X.-M.; Agyapong, V.I. Mental health effects in primary care patients 18 months after a major wildfire in Fort McMurray: Risk increased by social demographic issues, clinical antecedents, and degree of fire exposure. Front. Psychiatry 2019, 10, 683. [Google Scholar] [CrossRef]
- Agyapong, V.I.; Hrabok, M.; Juhas, M.; Omeje, J.; Denga, E.; Nwaka, B.; Akinjise, I.; Corbett, S.E.; Moosavi, S.; Brown, M. Prevalence rates and predictors of generalized anxiety disorder symptoms in residents of Fort McMurray six months after a wildfire. Front. Psychiatry 2018, 9, 345. [Google Scholar] [CrossRef]
- Bryant, R.A.; Waters, E.; Gibbs, L.; Gallagher, H.C.; Pattison, P.; Lusher, D.; MacDougall, C.; Harms, L.; Block, K.; Snowdon, E. Psychological outcomes following the Victorian Black Saturday bushfires. Aust. N. Z. J. Psychiatry 2014, 48, 634–643. [Google Scholar] [CrossRef]
- McDermott, B.M.; Palmer, L.J. Postdisaster emotional distress, depression and event-related variables: Findings across child and adolescent developmental stages. Aust. N. Z. J. Psychiatry 2002, 36, 754–761. [Google Scholar] [CrossRef]
- Agyapong, V.I. Coronavirus disease 2019 pandemic: Health system and community response to a text message (Text4Hope) program supporting mental health in Alberta. Disaster Med. Public Health Prep. 2020, 14, e5–e6. [Google Scholar] [CrossRef] [PubMed]
- Agyapong, V.I.O.; Hrabok, M.; Shalaby, R.; Mrklas, K.; Vuong, W.; Gusnowski, A.; Surood, S.; Greenshaw, A.J.; Nkire, N. Closing the COVID-19 psychological treatment gap for cancer patients in Alberta: Protocol for the implementation and evaluation of Text4Hope-Cancer Care. JMIR Res. Protoc. 2020, 9, e20240. [Google Scholar] [CrossRef] [PubMed]
- Census Profile, 2021 Census of Population. 2021. Available online: https://www12.statcan.gc.ca/census-recensement/2021/dp-pd/prof/details/page.cfm?Lang=E&GENDERlist=1&STATISTIClist=1&HEADERlist=0&DGUIDlist=2021A000248&SearchText=Alberta (accessed on 2 August 2023).
- Davidson, R.B.; Harrison, R.O.; Smith, P.; Spalding, D.A.E. Alberta. 2023. Available online: https://www.britannica.com/place/Alberta-province (accessed on 2 August 2023).
- Alberta Could Break Decades-Old Record for Amount of Area Burned during 2023 Wildfire Season. Available online: https://edmonton.ctvnews.ca/alberta-could-break-decades-old-record-for-amount-of-area-burned-during-2023-wildfire-season-1.6438194 (accessed on 10 August 2023).
- Wildfires in Alberta off to an Exponentially Fast Start Compared to Recent Years. Available online: https://edition.cnn.com/2023/05/10/americas/canada-alberta-wildfires/index.html (accessed on 10 August 2023).
- Storring, T. Economics and Statistics. 2023. Available online: https://novascotia.ca/finance/statistics/archive_news.asp?id=18712#:~:text=Nova%20Scotia’s%20population%20was%201%2C037%2C782,%25)%20from%20October%201%2C%202022 (accessed on 2 August 2023).
- More Than 16,000 Evacuated as Wildfire Rages Outside Halifax. Available online: https://www.nytimes.com/2023/05/30/world/canada/wildfire-halifax-nova-scotia.html (accessed on 10 August 2023).
- Harris, P.A.; Taylor, R.; Thielke, R.; Payne, J.; Gonzalez, N.; Conde, J.G. Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. J. Biomed. Inform. 2009, 42, 377–381. [Google Scholar] [CrossRef] [PubMed]
- Levis, B.; Benedetti, A.; Thombs, B.D. Accuracy of Patient Health Questionnaire-9 (PHQ-9) for screening to detect major depression: Individual participant data meta-analysis. BMJ 2019, 365, l1476. [Google Scholar] [CrossRef] [PubMed]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B. The PHQ-9: Validity of a Brief Depression Severity Measure. J. Gen. Intern. Med. 2001, 16, 606–613. [Google Scholar] [CrossRef] [PubMed]
- Shin, C.; Ko, Y.-H.; An, H.; Yoon, H.-K.; Han, C. Normative data and psychometric properties of the Patient Health Questionnaire-9 in a nationally representative Korean population. BMC Psychiatry 2020, 20, 194. [Google Scholar] [CrossRef]
- IBM Corporation. IBM SPSS Statistics for Windows; IBM Corp: Armonk, NY, USA, 2017. [Google Scholar]
- Ying, L.; Wu, X.; Lin, C.; Jiang, L. Traumatic severity and trait resilience as predictors of posttraumatic stress disorder and depressive symptoms among adolescent survivors of the Wenchuan earthquake. PLoS ONE 2014, 9, e89401. [Google Scholar] [CrossRef]
- Nandi, A.; Tracy, M.; Beard, J.R.; Vlahov, D.; Galea, S. Patterns and predictors of trajectories of depression after an urban disaster. Ann. Epidemiol. 2009, 19, 761–770. [Google Scholar] [CrossRef]
- Ritchie, A.; Sautner, B.; Omege, J.; Denga, E.; Nwaka, B.; Akinjise, I.; Corbett, S.E.; Moosavi, S.; Greenshaw, A.; Chue, P. Long-term mental health effects of a devastating wildfire are amplified by sociodemographic and clinical antecedents in college students. Disaster Med. Public Health Prep. 2021, 15, 707–717. [Google Scholar] [CrossRef]
- Silveira, S.; Kornbluh, M.; Withers, M.C.; Grennan, G.; Ramanathan, V.; Mishra, J. Chronic mental health sequelae of climate change extremes: A case study of the deadliest Californian wildfire. Int. J. Environ. Res. Public Health 2021, 18, 1487. [Google Scholar] [CrossRef]
- Nillni, Y.I.; Nosen, E.; Williams, P.A.; Tracy, M.; Coffey, S.F.; Galea, S. Unique and related predictors of major depressive disorder, posttraumatic stress disorder, and their comorbidity following Hurricane Katrina. J. Nerv. Ment. Dis. 2013, 201, 841. [Google Scholar] [CrossRef] [PubMed]
- Goldmann, E.; Galea, S. Mental health consequences of disasters. Annu. Rev. Public Health 2014, 35, 169–183. [Google Scholar] [CrossRef] [PubMed]
- Callegari, C.; Bertù, L.; Caselli, I.; Isella, C.; Ielmini, M.; Bonalumi, C.; Ferrario, M.; Vender, S. Resilience in older adults: Influence of the admission in nursing home and psychopathology. Neuropsychiatry 2016, 6, 117–123. [Google Scholar] [CrossRef]
- Isella, C.; Gasparini, A.; Lucca, G.; Ielmini, M.; Caselli, I.; Poloni, N.; Dajelli Ermolli, C.; Caravati, F.; Castiglioni, B.; De Ponti, R. Resilience, cardiological outcome, and their correlations with anxious-depressive symptoms and quality of life in patients with an implantable cardioverter defibrillator. Front. Psychiatry 2021, 12, 763726. [Google Scholar] [CrossRef] [PubMed]
- Camero, K. 8 Common Triggers of Depression Relapse. Depression 2023. Available online: https://www.everydayhealth.com/hs/major-depression-health-well-being/factors-can-trigger-depression-relapse/ (accessed on 8 August 2023).
- Kinderman, P.; Schwannauer, M.; Pontin, E.; Tai, S. Psychological processes mediate the impact of familial risk, social circumstances and life events on mental health. PLoS ONE 2013, 8, e76564. [Google Scholar] [CrossRef] [PubMed][Green Version]
- McKee-Ryan, F.; Song, Z.; Wanberg, C.R.; Kinicki, A.J. Psychological and physical well-being during unemployment: A meta-analytic study. J. Appl. Psychol. 2005, 90, 53. [Google Scholar] [CrossRef]
- Stankunas, M.; Kalediene, R.; Starkuviene, S.; Kapustinskiene, V. Duration of unemployment and depression: A cross-sectional survey in Lithuania. BMC Public Health 2006, 6, 174. [Google Scholar] [CrossRef] [PubMed]
- Paul, K.I.; Moser, K. Unemployment impairs mental health: Meta-analyses. J. Vocat. Behav. 2009, 74, 264–282. [Google Scholar] [CrossRef]
- Fergusson, D.M.; McLeod, G.F.; Horwood, L.J. Unemployment and psychosocial outcomes to age 30: A fixed-effects regression analysis. Aust. N. Z. J. Psychiatry 2014, 48, 735–742. [Google Scholar] [CrossRef]
- Amiri, S. Unemployment associated with major depression disorder and depressive symptoms: A systematic review and meta-analysis. Int. J. Occup. Saf. Ergon. 2022, 28, 2080–2092. [Google Scholar] [CrossRef]
- Eisenberg, P.; Lazarsfeld, P.F. The psychological effects of unemployment. Psychol. Bull. 1938, 35, 358. [Google Scholar] [CrossRef]
- Keya, T.A.; Leela, A.; Habib, N.; Rashid, M.; Bakthavatchalam, P. Mental health disorders due to disaster exposure: A systematic review and meta-analysis. Cureus 2023, 15, e37031. [Google Scholar] [CrossRef]
- Lim, G.Y.; Tam, W.W.; Lu, Y.; Ho, C.S.; Zhang, M.W.; Ho, R.C. Prevalence of depression in the community from 30 countries between 1994 and 2014. Sci. Rep. 2018, 8, 2861. [Google Scholar] [CrossRef]
- Economou, M.; Peppou, L.E.; Souliotis, K.; Konstantakopoulos, G.; Papaslanis, T.; Kontoangelos, K.; Nikolaidi, S.; Stefanis, N. An association of economic hardship with depression and suicidality in times of recession in Greece. Psychiatry Res. 2019, 279, 172–179. [Google Scholar] [CrossRef]
- Fukuda, Y.; Hiyoshi, A. Influences of income and employment on psychological distress and depression treatment in Japanese adults. Environ. Health Prev. Med. 2012, 17, 10–17. [Google Scholar] [CrossRef]
- Chung, E.K.; McCollum, K.F.; Elo, I.T.; Lee, H.J.; Culhane, J.F. Maternal depressive symptoms and infant health practices among low-income women. Pediatrics 2004, 113, e523–e529. [Google Scholar] [CrossRef] [PubMed]
- Dooley, D.; Catalano, R.; Hough, R. Unemployment and alcohol disorder in 1910 and 1990: Drift versus social causation. J. Occup. Organ. Psychol. 1992, 65, 277–290. [Google Scholar] [CrossRef]
- Lee, A.J.; Crombie, I.K.; Smith, W.C.; Tunstall-Pedoe, H.D. Cigarette smoking and employment status. Soc. Sci. Med. 1991, 33, 1309–1312. [Google Scholar] [CrossRef] [PubMed]
- Björkman, T.; Hansson, L. What do case managers do? An investigation of case manager interventions and their relationship to client outcome. Soc. Psychiatry Psychiatr. Epidemiol. 2000, 35, 43–50. [Google Scholar] [CrossRef] [PubMed]
- Helliwell, J.F.; Putnam, R.D. The social context of well-being. Philos. Trans. R. Soc. Lond. Ser. B Biol. Sci. 2004, 359, 1435–1446. [Google Scholar] [CrossRef]
- Obuobi-Donkor, G.; Eboreime, E.; Shalaby, R.; Agyapong, B.; Oluwasina, F.; Adu, M.; Owusu, E.; Mao, W.; Agyapong, V.I. Evaluating the prevalence and predictors of moderate to severe depression in Fort McMurray, Canada during the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2022, 19, 7090. [Google Scholar] [CrossRef]
- Templeton, L.; Deehan, A.; Taylor, C.; Drummond, C.; Strang, J. Surveying general practitioners: Does a low response rate matter? Br. J. Gen. Pract. 1997, 47, 91–94. [Google Scholar]
| Variables | Living in a Region of Nova Scotia/Alberta That Has Recently Been Impacted by the Wildfires | ||
|---|---|---|---|
| No (Total = 185) n (%) 62.3% | Yes (Total = 113) n (%) 37.7% | Total 297 n (%) | |
| Province | |||
| Nova Scotia | 19 (10.3%) | 28 (24.8%) | 47 (15.8%) |
| Alberta | 166 (89.7%) | 85 (75.2%) | 251(84.2%) |
| Age | |||
| Median | 50.00 | 50.50 | |
| Mean (SD) | 48.62 (14.05) | 47.98 (13.79) | |
| Age categories | |||
| ≥60 year | 48 (25.9%) | 24 (21.4%) | 72 (24.2%) |
| 50–59 | 46 (24.9%) | 34 (30.4%) | 80 (26.9%) |
| 40–49 | 39 (21.1%) | 22 (19.6%) | 61 (20.5%) |
| ≤40 year | 52 (28.1%) | 32 (28.6%) | 84 (28.3%) |
| Gender | |||
| Male | 25 (13.5%) | 13 (11.6%) | 38 (12.8%) |
| Female | 156 (84.3%) | 97 (86.6%) | 253 (85.2%) |
| Other | 4 (2.2%) | 2 (1.8%) | 6 (2.0%) |
| Ethnicity | |||
| Caucasian | 150 (81.1%) | 98 (87.5%) | 248 (83.5%) |
| Indigenous | 12 (6.5%) | 6 (5.4%) | 18 (6.1%) |
| Asian | 10 (5.4%) | 1 (0.9%) | 11 (3.7%) |
| Black/Hispanic | 6 (3.2%) | 3 (2.7%) | 9 (3.0%) |
| Other | 7 (3.8%) | 4 (3.6%) | 11 (3.7%) |
| Education level | |||
| High School or Lower Education | 34 (18.4%) | 17 (15.2%) | 51 (17.2%) |
| Post-secondary Education | 151 (81.6%) | 95 (84.8%) | 246 (82.8%) |
| Relationship status | |||
| Married/Partnered/Common Law/Cohabiting | 106 (57.6%) | 61 (54.5%) | 167 (56.4%) |
| Single | 48 (26.1%) | 27 (24.1%) | 75 (25.3%) |
| Separated or Divorced | 22 (12.0%) | 16 (14.3%) | 38 (12.8%) |
| Widowed | 5 (2.7%) | 7 (6.3%) | 12 (4.1%) |
| Other | 3 (1.6%) | 1 (0.9%) | 4 (1.4%) |
| Employment status | |||
| Employed | 116 (62.7%) | 73 (65.2%) | 189 (63.6%) |
| Unemployed | 30 (16.2%) | 18 (16.1%) | 48 (16.2%) |
| Student | 7 (3.8%) | 5 (4.5%) | 12 (4.0%) |
| Retired | 32 (17.3%) | 16 (14.3%) | 48 (16.2%) |
| Housing status | |||
| Own home | 121 (65.4%) | 79 (70.5%) | 200 (67.3%) |
| Renting accommodation | 44 (23.8%) | 20 (17.9%) | 64 (21.5%) |
| Live with family or friend | 20 (10.8%) | 13 (11.6%) | 33 (11.1%) |
| History of having mental health diagnosis from a health professional * | |||
| Depression | 107 (57.8%) | 61 (54.0%) | 168 (56.4%) |
| Bipolar Disorder | 10 (5.4%) | 6 (5.3%) | 16 (5.4%) |
| Anxiety | 98 (53.0%) | 59 (52.2%) | 157 (52.7%) |
| Alcohol abuse | 11 (5.9%) | 1 (0.9%) | 12 (4.0%) |
| Drug abuse | 8 (4.3%) | 3 (2.7%) | 11 (3.7%) |
| Schizophrenia | 2 (1.1%) | 1 (0.9%) | 3 (1.0%) |
| Personality Disorder | 10 (5.4%) | 10 (8.8%) | 20 (6.7%) |
| PTSD/OCD | 9 (4.9%) | 10 (8.8%) | 19 (6.4%) |
| ADHD | 7 (3.8%) | 7 (6.2%) | 14 (4.7%) |
| Other | 2 (1.1%) | 2 (1.8%) | 4 (1.3%) |
| No mental health diagnosis | 35 (18.9%) | 28 (24.8%) | 63 (21.1%) |
| History of receiving psychotropic medications * | |||
| Antidepressants | 76 (41.1%) | 40 (35.4%) | 116 (38.9%) |
| Antipsychotics | 12 (6.5%) | 9 (8.0%) | 21 (7.0%) |
| Benzodiazepines | 8 (4.3%) | 8 (7.1%) | 16 (5.4%) |
| Mood stabilizers | 16 (8.6%) | 11 (9.7%) | 27 (9.1%) |
| Sleeping tablets | 18 (9.7%) | 15 (13.3%) | 33 (11.1%) |
| Stimulants for ADHD | 6 (3.2%) | 4 (3.5%) | 10 (3.4%) |
| Other | 10 (5.4%) | 0 (0.0%) | 10 (3.4%) |
| On no psychotropic medication | 87 (47.0%) | 61 (54.0%) | 148 (49.7%) |
| Having received MH counselling in the past year | |||
| No | 88 (47.6%) | 97 (52.4%) | 146 (49.2%) |
| Yes | 58 (51.8%) | 54 (48.2%) | 151 (50.8%) |
| Having a wildfire evacuation order issued for the subscriber’s area of residence | |||
| Yes | N/A | 25 (22.1%) | 113 (100%) |
| No | 88 (77.9%) | ||
| Having had to evacuate from your home due to the recent wildfires in AB/NS | |||
| No | N/A | 88 (77.9%) | 113 (100%) |
| Yes | 25 (22.1%) | ||
| Have you lost any property because of the wildfire? | |||
| No | N/A | 109 (96.5%) | 113 (100%) |
| Yes | 4 (3.5%) | ||
| If you lost any property, what kind of property that was lost * | |||
| Home | N/A | 3 (60%) | 4 (100%) |
| Car | 2 (40%) | ||
| Farm | 0 (0%) | ||
| Having received support from family and friends in relation to the recent wildfire | |||
| Absolute support | N/A | 28 (24.8%) | 113 (100%) |
| Some support | 24 (21.2%) | ||
| Only limited support | 18 (15.9%) | ||
| Not at all | 43 (38.1%) | ||
| Having received support from the government of AB/NS in relation to the recent wildfire | |||
| Absolute support | N/A | 6 (5.3%) | 6 (5.3%) |
| Some support | 13 (11.5%) | 13 (11.5%) | |
| Only limited support | 8 (7.1%) | 8 (7.1%) | |
| Not at all | 86 (76.1%) | 86 (76.1%) | |
| Having received support from Red Cross in relation to the recent wildfire | |||
| Absolute support | N/A | 0 | 112 (100%) |
| Some support | 6 (5.4%) | ||
| Only limited support | 4 (3.6%) | ||
| Not at all | 102 (91.1%) | ||
| Frequency of watching television images about the devastation caused by the recent wildfires in AB/NS | |||
| Daily | 64 (34.6%) | 41 (36.6%) | 105 (35.4%) |
| About every other day | 34 (18.4%) | 25 (22.3%) | 59 (19.9%) |
| About once a week | 23 (12.4%) | 8 (7.1%) | 31 (10.4%) |
| Less than once a week | 22 (11.9%) | 16 (14.3%) | 38 (12.8%) |
| Haven’t watched TV images of the devastation | 42 (22.7%) | 22 (19.6%) | 64 (21.5%) |
| Having called the Mental Health Criss line in relation to the recent wildfires in AB/NS | |||
| No | 183 (98.9%) | 110 (97.3%) | 293 (98.3%) |
| Yes | 2 (1.1%) | 3 (2.7%) | 5 (1.7%) |
| Likely depression | |||
| Non to mild depression | 81 (53.3%) | 43 (43.9%) | 124 (49.6%) |
| Moderate to severe depression | 71 (46.7%) | 55 (56.1%) | 126 (50.4%) |
| Variables | Moderate to Severe Depression | ||
|---|---|---|---|
| n (%) | Chi 2 (DF)/Fisher’s Exact | p-Value | |
| Province | |||
| NS | 21 (48.8%) | 0.05 (1) | 0.82 |
| AB | 105 (50.7%) | ||
| Age categories | |||
| ≥60 year | 24 (39.3%) | 6.77 (3) | 0.08 |
| 50–59 | 35 (56.5%) | ||
| 40–49 | 24 (44.4%) | ||
| ≤40 year | 43 (58.9%) | ||
| Gender | |||
| Male | 14 (48.3%) | * | 0.82 |
| Female | 108 (50.2%) | ||
| Other | 4 (66.7%) | ||
| Ethnicity | |||
| Caucasian | 102 (48.6%) | * | 0.15 |
| Indigenous | 11 (68.8%) | ||
| Asian | 4 (40.0%) | ||
| Black/Hispanic | 3 (42.9%) | ||
| Other | 6 (85.7%) | ||
| Education level | |||
| High School or Lower Education | 24 (66.7%) | 4.45 (1) | 0.04 |
| Post-secondary Education | 102 (47.7%) | ||
| Relationship status | |||
| Married/Partnered/Common Law/Cohabiting | 64 (45.1%) | * | 0.11 |
| Single | 36 (59.0%) | ||
| Separated or Divorced | 17 (50.0%) | ||
| Widowed | 8 (80.0%) | ||
| Other | 1 (33.3%) | ||
| Employment status | |||
| Employed | 77 (47.0%) | * | 0.01 |
| Unemployed | 29 (72.5%) | ||
| Student | 6 (66.7%) | ||
| Retired | 14 (37.8%) | ||
| Housing status | |||
| Own home | 73 (44.0%) | 8.17 (2) | 0.02 |
| Renting accommodation | 37 (62.7%) | ||
| Live with family or friend | 16 (64.0%) | ||
| History of having mental health diagnosis from a health professional * | |||
| Depression | 95 (63.8%) | 26.33 (1) | 0.00 |
| Bipolar Disorder | 9 (69.2%) | 1.95 (1) | 0.16 |
| Anxiety | 83 (58.5%) | 8.52 (1) | 0.00 |
| Alcohol abuse | 7 (58.3%) | 0.32 (1) | 0.57 |
| Drug abuse | 5 (45.5%) | 0.11 (1) | 0.74 |
| Schizophrenia | 0 (0.0%) | * | 0.12 |
| Personality Disorder | 13 (72.2%) | 3.70 (1) | 0.06 |
| PTSD/OCD | 12 (66.7%) | 2.05 (1) | 0.15 |
| ADHD | 10 (83.3%) | 5.47 (1) | 0.02 |
| Other | 3 (75.0%) | * | 0.62 |
| No mental health diagnosis | 17 (28.8%) | 14.40 (1) | 0.00 |
| History of receiving psychotropic medications * | |||
| Antidepressants | 65 (63.1%) | 11.31 (1) | 0.00 |
| Antipsychotics | 14 (73.7%) | 4.46 (1) | 0.04 |
| Benzodiazepines | 12 (80.0%) | 5.59 (1) | 0.02 |
| Mood stabilizers | 16 (69.6%) | 3.72 (1) | 0.05 |
| Sleeping tablets | 21 (65.6%) | 3.40 (1) | 0.07 |
| Stimulants for ADHD | 3 (42.9%) | * | 0.72 |
| Other | 5 (55.6%) | * | 1.0 |
| On no psychotropic medication | 49 (40.5%) | 9.20 (1) | 0.00 |
| Having received MH counselling in the past year | |||
| No | 54 (46.6%) | 1.28 (1) | 0.26 |
| Yes | 72 (53.7%) | ||
| Living in a region of AB/NS that has recently been impacted by the wildfires | |||
| No | 71 (46.7%) | 2.11 (1) | 0.15 |
| Yes | 55 (56.1%) | ||
| Having a wildfire evacuation order issued for the subscriber’s area of residence | |||
| Yes | 15 (62.5%) | * | 0.33 |
| No | 38 (56.7%) | ||
| Not applicable | 2 (28.6%) | ||
| Having had to evacuate from your home due to the recent wildfires in AB/NS | |||
| No | 41 (53.2%) | 1.20 (1) | 0.27 |
| Yes | 14 (66.7%) | ||
| Have you lost any property because of the wildfire? | |||
| No | 53 (55.2%) | * | 0.50 |
| Yes | 2 (100.0%) | ||
| Kind of property that was lost | |||
| Home | 2 (100%) | * | 0.50 |
| Car | 0 (0%) | - | - |
| Farm | 0 (0%) | - | - |
| Having received support from family and friends in relation to the recent wildfire | |||
| Some to absolute support | 21 (50.0%) | 1.12 (1) | 0.29 |
| Limited to no support | 34 (60.7%) | ||
| Having received support from the government of AB/NS in relation to the recent wildfire | |||
| Some to absolute support | 8 (53.3%) | 0.06 (1) | 0.81 |
| Limited to no support | 47 (56.6%) | ||
| Having received support from Red Cross in relation to the recent wildfire | |||
| Some to absolute support | 4 (80.0%) | * | 0.38 |
| Limited to no support | 51 (54.8%) | ||
| Frequency of watching television images about the devastation caused by the recent wildfires in AB/NS | |||
| Daily | 41 (47.7%) | 0.79 (4) | 0.94 |
| About every other day | 27 (55.1%) | ||
| About once a week | 12 (48.0%) | ||
| Less than once a week | 16 (50.0%) | ||
| Haven’t watched TV images of the devastation | 30 (51.7%) | ||
| Having called the Mental Health Criss line in relation to the recent wildfires in AB/NS | |||
| No | 125 (50.6%) | * | 0.62 |
| Yes | 1 (33.3%) | ||
| B | S.E. | Wald | df | Sig. | Exp(B) | 95% C.I.for EXP(B) | |||
|---|---|---|---|---|---|---|---|---|---|
| Lower | Upper | ||||||||
| Age | ≥60 year | 2.148 | 3 | 0.542 | |||||
| 50–59 year | 0.484 | 0.463 | 1.090 | 1 | 0.296 | 1.622 | 0.654 | 4.023 | |
| 40–49 year | −0.099 | 0.504 | 0.038 | 1 | 0.845 | 0.906 | 0.337 | 2.433 | |
| <40 year | 0.145 | 0.485 | 0.089 | 1 | 0.765 | 1.156 | 0.447 | 2.990 | |
| Employment status | Employed | 5.664 | 3 | 0.129 | |||||
| Unemployed | 0.899 | 0.427 | 4.429 | 1 | 0.035 | 2.457 | 1.064 | 5.674 | |
| Student | 0.461 | 0.838 | 0.303 | 1 | 0.582 | 1.586 | 0.307 | 8.196 | |
| Retired | −0.358 | 0.518 | 0.476 | 1 | 0.490 | 0.699 | 0.253 | 1.932 | |
| Education | Post-secondary Education | −0.527 | 0.434 | 1.478 | 1 | 0.224 | 0.590 | 0.252 | 1.381 |
| Housing status | Own Home | 1.636 | 2 | 0.441 | |||||
| Rented Accommodation | 0.335 | 0.378 | 0.789 | 1 | 0.375 | 1.398 | 0.667 | 2.931 | |
| Live with Family or Friends | 0.576 | 0.518 | 1.237 | 1 | 0.266 | 1.779 | 0.645 | 4.912 | |
| Previous mental health diagnosis | Depression | ||||||||
| Yes | 1.147 | 0.417 | 7.558 | 1 | 0.006 | 3.150 | 1.390 | 7.138 | |
| Anxiety | |||||||||
| Yes | 0.060 | 0.374 | 0.026 | 1 | 0.872 | 1.062 | 0.510 | 2.210 | |
| Personality Disorder | |||||||||
| Yes | −0.131 | 0.697 | 0.035 | 1 | 0.851 | 0.877 | 0.224 | 3.439 | |
| ADHD | |||||||||
| Yes | 1.232 | 0.858 | 2.060 | 1 | 0.151 | 3.427 | 0.637 | 18.424 | |
| Received no mental health diagnosis | |||||||||
| Yes | 0.284 | 0.545 | 0.271 | 1 | 0.603 | 1.328 | 0.456 | 3.867 | |
| Are you on any of the following medications for a mental health concern? | Antidepressants | ||||||||
| Yes | 0.260 | 0.339 | 0.587 | 1 | 0.443 | 1.297 | 0.667 | 2.519 | |
| Antipsychotics | |||||||||
| Yes | 0.453 | 0.760 | 0.355 | 1 | 0.551 | 1.572 | 0.355 | 6.968 | |
| Benzodiazepines | |||||||||
| Yes | 0.933 | 0.722 | 1.667 | 1 | 0.197 | 2.541 | 0.617 | 10.470 | |
| Mood Stabilizers | |||||||||
| Yes | 0.068 | 0.640 | 0.011 | 1 | 0.916 | 1.070 | 0.305 | 3.755 | |
| Sleeping Tablets | |||||||||
| Yes | 0.292 | 0.475 | 0.377 | 1 | 0.539 | 1.338 | 0.528 | 3.395 | |
| Constant | −0.967 | 0.677 | 2.038 | 1 | 0.153 | 0.380 | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mao, W.; Shalaby, R.; Agyapong, B.; Obuobi-Donkor, G.; Da Luz Dias, R.; Agyapong, V.I.O. Devastating Wildfires and Mental Health: Major Depressive Disorder Prevalence and Associated Factors among Residents in Alberta and Nova Scotia, Canada. Behav. Sci. 2024, 14, 209. https://doi.org/10.3390/bs14030209
Mao W, Shalaby R, Agyapong B, Obuobi-Donkor G, Da Luz Dias R, Agyapong VIO. Devastating Wildfires and Mental Health: Major Depressive Disorder Prevalence and Associated Factors among Residents in Alberta and Nova Scotia, Canada. Behavioral Sciences. 2024; 14(3):209. https://doi.org/10.3390/bs14030209
Chicago/Turabian StyleMao, Wanying, Reham Shalaby, Belinda Agyapong, Gloria Obuobi-Donkor, Raquel Da Luz Dias, and Vincent I. O. Agyapong. 2024. "Devastating Wildfires and Mental Health: Major Depressive Disorder Prevalence and Associated Factors among Residents in Alberta and Nova Scotia, Canada" Behavioral Sciences 14, no. 3: 209. https://doi.org/10.3390/bs14030209
APA StyleMao, W., Shalaby, R., Agyapong, B., Obuobi-Donkor, G., Da Luz Dias, R., & Agyapong, V. I. O. (2024). Devastating Wildfires and Mental Health: Major Depressive Disorder Prevalence and Associated Factors among Residents in Alberta and Nova Scotia, Canada. Behavioral Sciences, 14(3), 209. https://doi.org/10.3390/bs14030209







