Patient Safety Incidents in Inpatient Psychiatric Settings: An Expert Opinion Survey
Abstract
1. Introduction
2. Material and Methods
2.1. Step 1: Comprehensive Knowledge Synthesis
2.1.1. Step 1A: Framework Identification
2.1.2. Step 1B: Literature Review
2.2. Step 2: Questionnaire Design
2.3. Step 3: Sample Size
2.4. Step 4: Expert Identification
2.5. Step 5: Online Survey
2.6. Step 6: Data Quality
2.7. Step 7: Data Analysis and Interpretation
3. Results
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| ICPS | International classification for patient safety |
| PSI | Patient safety incident |
| ITC | Incident type category |
| ICC2K | Two-way random, average score intraclass correlation |
References
- World Health Organization. Global Patient Safety Report 2024; World Health Organization: Geneva, Switzerland, 2024. [Google Scholar]
- Thibaut, B.; Dewa, L.H.; Ramtale, S.C.; D’Lima, D.; Adam, S.; Ashrafian, H.; Darzi, A.; Archer, S. Patient safety in inpatient mental health settings: A systematic review. BMJ Open 2019, 9, e030230. [Google Scholar] [CrossRef] [PubMed]
- Berg, S.H.; Rørtveit, K.; Aase, K. Suicidal patients’ experiences regarding their safety during psychiatric in-patient care: A systematic review of qualitative studies. BMC Health Serv. Res. 2017, 17, 73. [Google Scholar] [CrossRef] [PubMed]
- Karlin, B.E.; Zeiss, R.A. Best Practices: Environmental and Therapeutic Issues in Psychiatric Hospital Design: Toward Best Practices. Psychiatr. Serv. 2006, 57, 1376–1378. [Google Scholar] [CrossRef] [PubMed]
- Stavropoulou, C.; Doherty, C.; Tosey, P. How Effective Are Incident-Reporting Systems for Improving Patient Safety? A Systematic Literature Review. Milbank Q. 2015, 93, 826–866. [Google Scholar] [CrossRef]
- Benevento, M.; Nicolì, S.; Mandarelli, G.; Ferorelli, D.; Cicolini, G.; Marrone, M.; Dell’Erba, A.; Solarino, B. Strengths and weaknesses of the incident reporting system: An Italian experience. J. Patient Saf. Risk Manag. 2023, 28, 15–20. [Google Scholar] [CrossRef]
- Macrae, C. The problem with incident reporting. BMJ Qual. Saf. 2016, 25, 71–75. [Google Scholar] [CrossRef]
- Reilly, C.A.; Cullen, S.W.; Watts, B.V.; Mills, P.D.; Paull, D.E.; Marcus, S.C. How Well Do Incident Reporting Systems Work on Inpatient Psychiatric Units? Jt. Comm. J. Qual. Patient Saf. 2019, 45, 63–69. [Google Scholar] [CrossRef]
- Archer, S.; Thibaut, B.I.; Dewa, L.H.; Ramtale, C.; D’Lima, D.; Simpson, A.; Murray, K.; Adam, S.; Darzi, A. Barriers and facilitators to incident reporting in mental healthcare settings: A qualitative study. J. Psychiatr. Ment. Health Nurs. 2020, 27, 211–223. [Google Scholar] [CrossRef]
- Thompson, A.D.; Ramasamy, R.S.; Simmons, S.; Gurtovenko, K.; Caufield, S.; Sasser, T.; Beauchamp, B.; O’Brien, M. What Do We Do When Things Fall Apart? Rapid Creation of a Pilot Psychiatric Intensive Care Unit in Response to Increased Acuity on a Psychiatric Inpatient Unit for Children and Adolescents. Evid.-Based Pract. Child Adolesc. Ment. Health 2021, 6, 435–446. [Google Scholar] [CrossRef]
- Jenkin, G.; Quigg, S.; Paap, H.; Cooney, E.; Peterson, D.; Every-Palmer, S. Places of safety? Fear and violence in acute mental health facilities: A large qualitative study of staff and service user perspectives. PLoS ONE 2022, 17, e0266935. [Google Scholar] [CrossRef]
- Vanhaecht, K.; Seys, D.; Russotto, S.; Strametz, R.; Mira, J.; Sigurgeirsdóttir, S.; Wu, A.W.; Põlluste, K.; Popovici, D.G.; Sfetcu, R.; et al. An Evidence and Consensus-Based Definition of Second Victim: A Strategic Topic in Healthcare Quality, Patient Safety, Person-Centeredness and Human Resource Management. Int. J. Environ. Res. Public Health 2022, 19, 16869. [Google Scholar] [CrossRef] [PubMed]
- Cousins, M.; Parmley, E.J.; Greer, A.L.; Neiterman, E.; Lambraki, I.A.; Graells, T.; Léger, A.; Henriksson, P.J.G.; Troell, M.; Wernli, D.; et al. Is scientific evidence enough? Using expert opinion to fill gaps in data in antimicrobial resistance research. PLoS ONE 2023, 18, e0290464. [Google Scholar] [CrossRef] [PubMed]
- Dy, S.M.; Taylor, S.L.; Carr, L.H.; Foy, R.; Pronovost, P.J.; Ovretveit, J.; Wachter, R.M.; Rubenstein, L.V.; Hempel, S.; McDonald, K.M.; et al. A framework for classifying patient safety practices: Results from an expert consensus process. BMJ Qual. Saf. 2011, 20, 618–624. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Brickell, T.A.; McLean, C. Emerging Issues and Challenges for Improving Patient Safety in Mental Health: A Qualitative Analysis of Expert Perspectives. J. Patient Saf. 2011, 7, 39–44. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Conceptual Framework for the International Classification for Patient Safety; World Health Organization: Geneva, Switzerland, 2009. [Google Scholar]
- Taheri Moghadam, S.; Hooman, N.; Sheikhtaheri, A. Patient safety classifications, taxonomies and ontologies: A systematic review on development and evaluation methodologies. J. Biomed. Inform. 2022, 133, 104150. [Google Scholar] [CrossRef]
- Marcus, S.C.; Hermann, R.C.; Cullen, S.W. Defining Patient Safety Events in Inpatient Psychiatry. J. Patient Saf. 2021, 17, e1452–e1457. [Google Scholar] [CrossRef]
- Reis, H.T. Why bottom-up taxonomies are unlikely to satisfy the quest for a definitive taxonomy of situations. J. Personal. Soc. Psychol. 2018, 114, 489–492. [Google Scholar] [CrossRef]
- Hennink, M.; Kaiser, B.N. Sample sizes for saturation in qualitative research: A systematic review of empirical tests. Soc. Sci. Med. 2022, 292, 114523. [Google Scholar] [CrossRef]
- Hennink, M.M.; Kaiser, B.N.; Marconi, V.C. Code Saturation Versus Meaning Saturation: How Many Interviews Are Enough? Qual. Health Res. 2017, 27, 591–608. [Google Scholar] [CrossRef]
- ISQua—The International Society for Quality in Health Care. Available online: https://isqua.org/ (accessed on 5 September 2024).
- ERNST—COST Action CA19113—The European Researchers’ Network Working on Second Victims. 2024. Available online: https://cost-ernst.eu/ (accessed on 5 September 2024).
- Ward, M.; Meade, A.W. Dealing with Careless Responding in Survey Data: Prevention, Identification, and Recommended Best Practices. Annu. Rev. Psychol. 2023, 74, 577–596. [Google Scholar] [CrossRef]
- Tavakol, M.; Dennick, R. Making sense of Cronbach’s alpha. Int. J. Med. Educ. 2011, 2, 53–55. [Google Scholar] [CrossRef] [PubMed]
- Passerini, G.; Macchi, L.; Bagassi, M. A methodological approach to ratio bias. Judgm. Decis. Mak. 2012, 7, 602–617. [Google Scholar] [CrossRef]
- Strametz, R.; Fendel, J.C.; Koch, P.; Roesner, H.; Zilezinski, M.; Bushuven, S.; Raspe, M. Prevalence of Second Victims, Risk Factors, and Support Strategies among German Nurses (SeViD-II Survey). Int. J. Environ. Res. Public Health 2021, 18, 10594. [Google Scholar] [CrossRef] [PubMed]
- De Feijter, J.M.; De Grave, W.S.; Muijtjens, A.M.; Scherpbier, A.J.J.A.; Koopmans, R.P. A Comprehensive Overview of Medical Error in Hospitals Using Incident-Reporting Systems, Patient Complaints and Chart Review of Inpatient Deaths. PLoS ONE 2012, 7, e31125. [Google Scholar] [CrossRef] [PubMed]
- Kepner, S.; Jones, R. Patient Safety Trends in 2023: An Analysis of 287,997 Serious Events and Incidents From the Nation’s Largest Event Reporting Database. Patient Saf. 2024, 6. [Google Scholar] [CrossRef]
- Göttems, L.B.D.; Santos, M.D.L.G.D.; Carvalho, P.A.; Amorim, F.F. A study of cases reported as incidents in a public hospital from 2011 to 2014. Rev. Esc. Enferm. USP 2016, 50, 861–867. [Google Scholar] [CrossRef]
- Pham, J.C.; Story, J.L.; Hicks, R.W.; Shore, A.D.; Morlock, L.L.; Cheung, D.S.; Kelen, G.D.; Pronovost, P.J. National Study on the Frequency, Types, Causes, and Consequences of Voluntarily Reported Emergency Department Medication Errors. J. Emerg. Med. 2011, 40, 485–492. [Google Scholar] [CrossRef]
- Thomas, A.N.; Panchagnula, U. Medication-related patient safety incidents in critical care: A review of reports to the UK National Patient Safety Agency. Anaesthesia 2008, 63, 726–733. [Google Scholar] [CrossRef]
- Cottell, M.; Wätterbjörk, I.; Hälleberg Nyman, M. Medication-related incidents at 19 hospitals: A retrospective register study using incident reports. Nurs. Open 2020, 7, 1526–1535. [Google Scholar] [CrossRef]
- McElroy, L.M.; Woods, D.M.; Yanes, A.F.; Skaro, A.I.; Daud, A.; Curtis, T.; Wymore, E.; Holl, J.L.; Abecassis, M.M.; Ladner, D.P. Applying the WHO conceptual framework for the International Classification for Patient Safety to a surgical population. Int. J. Qual. Health Care 2016, 28, 166–174. [Google Scholar] [CrossRef]
- Mitchell, R.; Faris, M.; Lystad, R.; Fajardo Pulido, D.; Norton, G.; Baysari, M.; Clay-Williams, R.; Hibbert, P.; Carson-Stevens, A.; Hughes, C. Using the WHO International Classification of patient safety framework to identify incident characteristics and contributing factors for medical or surgical complication deaths. Appl. Ergon. 2020, 82, 102920. [Google Scholar] [CrossRef] [PubMed]
- Mishina, K.; Berg, J.; Vainila, V.; Korte, M.; Lahti, M. Safety Incidents in Psychiatric Inpatient Care: A Qualitative Content Analysis of Safety Incident Reports. Perspect. Psychiatr. Care 2023, 2023, 1–11. [Google Scholar] [CrossRef]
- Xu, H.; Cao, X.; Jin, Q.; Wang, R.; Zhang, Y.; Chen, Z. Distress, support and psychological resilience of psychiatric nurses as second victims after violence: A cross-sectional study. J. Nurs. Manag. 2022, 30, 1777–1787. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Li, J.; Thornicroft, G.; Huang, Y. Levels of stigma among community mental health staff in Guangzhou, China. BMC Psychiatry 2014, 14, 231. [Google Scholar] [CrossRef]
- Uibu, E.; Põlluste, K.; Lember, M.; Toompere, K.; Kangasniemi, M. Planned improvement actions based on patient safety incident reports in Estonian hospitals: A document analysis. BMJ Open Qual. 2023, 12, e002058. [Google Scholar] [CrossRef]
- Maidment, I.D.; Lelliott, P.; Paton, C. Medication errors in mental healthcare: A systematic review. Qual. Saf. Health Care 2006, 15, 409–413. [Google Scholar] [CrossRef]
- Procyshyn, R.M.; Barr, A.M.; Brickell, T.; Honer, W.G. Medication Errors in Psychiatry: A Comprehensive Review. CNS Drugs 2010, 24, 595–609. [Google Scholar] [CrossRef]
- Ayre, M.J.; Lewis, P.J.; Keers, R.N. Understanding the medication safety challenges for patients with mental illness in primary care: A scoping review. BMC Psychiatry 2023, 23, 417. [Google Scholar] [CrossRef]
- Jayaram, G.; Doyle, D.; Steinwachs, D.; Samuels, J. Identifying and Reducing Medication Errors in Psychiatry: Creating a Culture of Safety Through the Use of an Adverse Event Reporting Mechanism. J. Psychiatr. Pract. 2011, 17, 81–88. [Google Scholar] [CrossRef]
- Holmes, S.; Baumhover, M.; Lockwood, J. Safety Unseen: Leveraging Design to Improve Inpatient Mental Health-Care Practices. Creat. Nurs. 2020, 26, 048–055. [Google Scholar] [CrossRef]
- Bodryzlova, Y.; Lemieux, A.J.; Dufour, M.; Côté, A.; Lalancette, S.; Crocker, A.G. Hospital design for inpatient psychiatry: A realistic umbrella review. J. Psychiatr. Res. 2024, 178, 94–106. [Google Scholar] [CrossRef] [PubMed]
- Marsall, M.; Hornung, T.; Bäuerle, A.; Weigl, M. Quality of care transition, patient safety incidents, and patients’ health status: A structural equation model on the complexity of the discharge process. BMC Health Serv. Res. 2024, 24, 576. [Google Scholar] [CrossRef] [PubMed]
- Tyler, N.; Wright, N.; Waring, J. Interventions to improve discharge from acute adult mental health inpatient care to the community: Systematic review and narrative synthesis. BMC Health Serv. Res. 2019, 19, 883. [Google Scholar] [CrossRef] [PubMed]
- Simms, A.; Fear, N.T.; Greenberg, N. The impact of having inadequate safety equipment on mental health. Occup. Med. 2020, 70, 278–281. [Google Scholar] [CrossRef] [PubMed]
- Prossor, D.; Constantinescu, S.; Stubbs, C.; Stewart, N.; Johansson, F. Medical Emergency Equipment Medication (MEEM) Training: A Quality Improvement Project Focusing on Transforming the Emergency Response to Inpatient Psychiatric Medical Emergencies. BJPsych Open 2024, 10, S171. [Google Scholar] [CrossRef]
- Varpula, J.; Välimäki, M.; Lantta, T.; Berg, J.; Lahti, M. Nurses’ perceptions of risks for occupational hazards in patient seclusion and restraint practices in psychiatric inpatient care: A focus group study. Int. J. Ment. Health Nurs. 2020, 29, 703–715. [Google Scholar] [CrossRef]
- Rowell, A.; Long, C.; Chance, L.; Dolley, O. Identification of nutritional risk by nursing staff in secure psychiatric settings: Reliability and validity of St Andrew’s Nutrition Screening Instrument. J. Psychiatr. Ment. Health Nurs. 2012, 19, 722–728. [Google Scholar] [CrossRef]
- Faulkner, G.E.J.; Gorczynski, P.F.; Cohn, T.A. Psychiatric Illness and Obesity: Recognizing the “Obesogenic” Nature of an Inpatient Psychiatric Setting. Psychiatr. Serv. 2009, 60, 538–541. [Google Scholar] [CrossRef]
- Flint, K.; Matthews-Rensch, K.; Flaws, D.; Mudge, A.; Young, A. Mealtime care and dietary intake in older psychiatric hospital inpatient: A multiple case study. J. Adv. Nurs. 2021, 77, 1490–1500. [Google Scholar] [CrossRef]
- Houben, F.; Van Hensbergen, M.; Den Heijer, C.D.J.; Dukers-Muijrers, N.H.T.M.; Hoebe, C.J.P.A. Barriers and facilitators to infection prevention and control in Dutch psychiatric institutions: A theory-informed qualitative study. BMC Infect. Dis. 2022, 22, 243. [Google Scholar] [CrossRef]
- Demler, T.L.; Mulcahy, K.B. Implications of infection and trends of antibiotic prescribing in hospitalized patients diagnosed with serious mental illness. Int. Clin. Psychopharmacol. 2018, 33, 49–55. [Google Scholar] [CrossRef] [PubMed]
- Ott, M.; French, R. Hand Hygiene Compliance Among Health Care Staff and Student Nurses in a Mental Health Setting. Issues Ment. Health Nurs. 2009, 30, 702–704. [Google Scholar] [CrossRef] [PubMed]
- Piai-Morais, T.H.; Fortaleza, C.M.C.B.; Figueiredo, R.M.D. Good Practices For Infection Prevention and Control at a Psychiatric Hospital in Brazil. Issues Ment. Health Nurs. 2015, 36, 513–517. [Google Scholar] [CrossRef] [PubMed]
- Rajamaki, B.; Hartikainen, S.; Tolppanen, A.M. Psychotropic Drug-Associated Pneumonia in Older Adults. Drugs Aging 2020, 37, 241–261. [Google Scholar] [CrossRef]
- Vossoughi, S.; Perez, G.; Whitaker, B.I.; Fung, M.K.; Rajbhandary, S.; Crews, N.; Stotler, B. Safety incident reports associated with blood transfusions. Transfusion 2019, 59, 2827–2832. [Google Scholar] [CrossRef]
- Osborn, D.A. Errors in blood transfusion. BMJ 1967, 4, 550–551. [Google Scholar] [CrossRef][Green Version]
- Kilbourne, A.M.; Beck, K.; Spaeth-Rublee, B.; Ramanuj, P.; O’Brien, R.W.; Tomoyasu, N.; Pincus, H.A. Measuring and improving the quality of mental health care: A global perspective. World Psychiatry 2018, 17, 30–38. [Google Scholar] [CrossRef]
- Averill, P.; Vincent, C.; Reen, G.; Henderson, C.; Sevdalis, N. Conceptual and practical challenges associated with understanding patient safety within community-based mental health services. Health Expect. 2022, 26, 51–63. [Google Scholar] [CrossRef]
- Ramírez, E.; Martín, A.; Villán, Y.; Lorente, M.; Ojeda, J.; Moro, M.; Vara, C.; Avenza, M.; Domingo, M.J.; Alonso, P.; et al. Effectiveness and limitations of an incident-reporting system analyzed by local clinical safety leaders in a tertiary hospital: Prospective evaluation through real-time observations of patient safety incidents. Medicine 2018, 97, e12509. [Google Scholar] [CrossRef]
- Noble, D.J.; Pronovost, P.J. Underreporting of Patient Safety Incidents Reduces Health Care’s Ability to Quantify and Accurately Measure Harm Reduction. J. Patient Saf. 2010, 6, 247–250. [Google Scholar] [CrossRef]
- Vargas, E.A.; Brassel, S.T.; Cortina, L.M.; Settles, I.H.; Johnson, T.R.; Jagsi, R. #MedToo: A Large-Scale Examination of the Incidence and Impact of Sexual Harassment of Physicians and Other Faculty at an Academic Medical Center. J. Women’s Health 2020, 29, 13–20. [Google Scholar] [CrossRef]

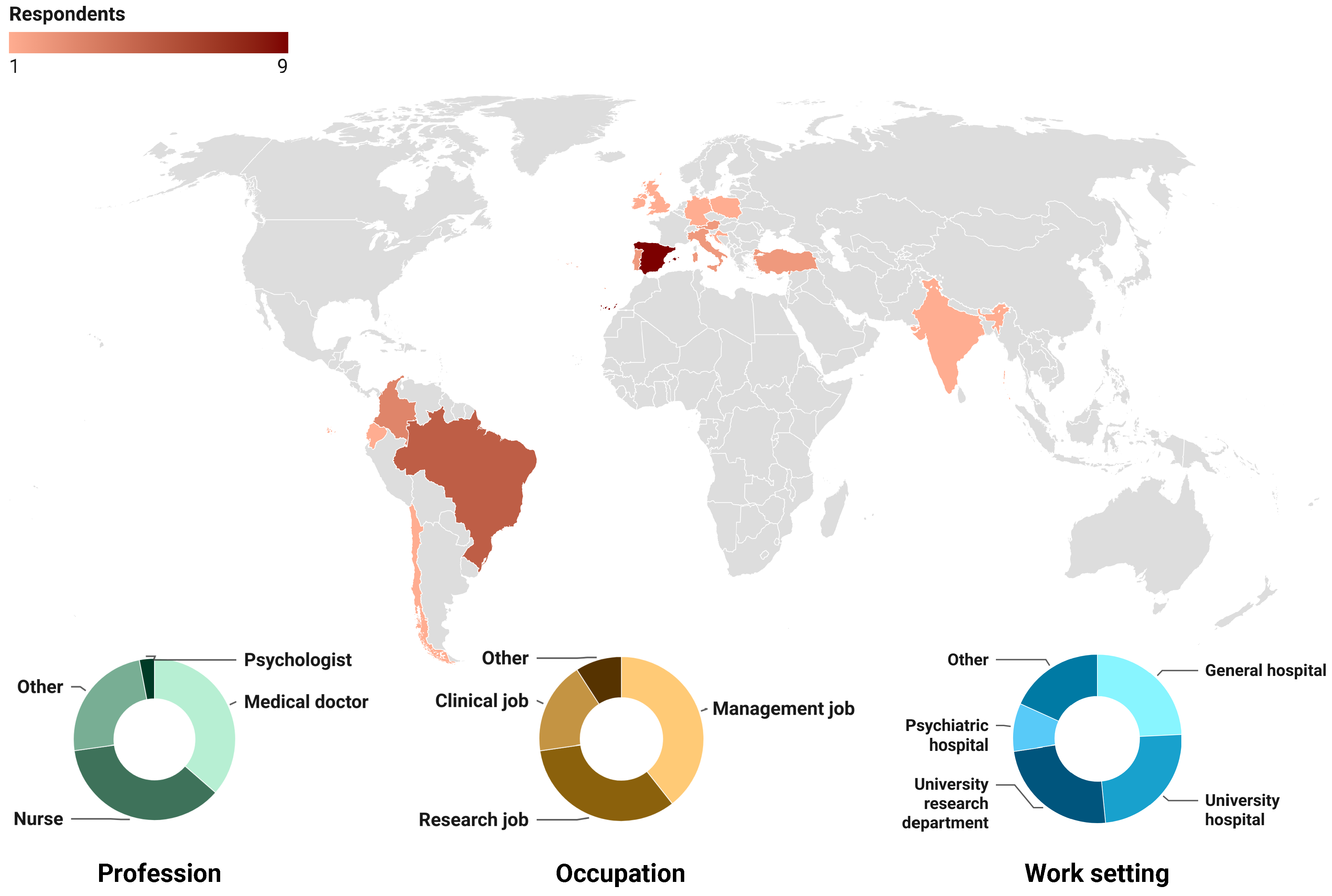
| Gender (n, %) | |
|---|---|
| Female | 23 (69.7) |
| Male | 10 (30.3) |
| Other | 0 (0.0) |
| Country (n, %) | |
| Austria | 2 (6.1) |
| Brazil | 5 (15.2) |
| Chile | 1 (3.0) |
| Colombia | 3 (9.1) |
| Croatia | 1 (3.0) |
| Ecuador | 1 (3.0) |
| Germany | 1 (3.0) |
| India | 1 (3.0) |
| Ireland | 1 (3.0) |
| Italy | 2 (6.1) |
| Portugal | 2 (6.1) |
| Poland | 1 (3.0) |
| Spain | 9 (27.3) |
| Turkey | 2 (6.1) |
| United Kingdom | 1 (3.0) |
| Work setting (n, %) | |
| General hospital | 8 (24.2) |
| Non-university research structure | 2 (6.1) |
| Non-clinical healthcare institutions and bodies | 1 (3.0) |
| Primary care | 1 (3.0) |
| Psychiatric hospital | 3 (9.1) |
| University hospital | 8 (24.2) |
| University research department | 8 (24.2) |
| Other | 2 (6.1) |
| Occupation (n, %) | |
| Clinical job | 6 (18.2) |
| Management job | 13 (39.4) |
| Research job | 11 (33.3) |
| Other | 3 (9.1) |
| Profession (n, %) | |
| Medical doctor | 12 (36.4) |
| of which psychiatrist | 2 (6.1) |
| Nurse | 12 (36.4) |
| of which psychiatric nurse | 0 (0) |
| Psychologist | 1 (3.0) |
| Other | 8 (24.2) |
| Working time spent on patient safety activities (n, %) | |
| Full time | 7 (21.2) |
| Most of my working time | 7 (21.2) |
| Half time | 5 (15.2) |
| Less than half | 10 (30.3) |
| No time | 4 (12.1) |
| Official patient safety appointment (n, %) | 20 (60.7) |
| Considers PSI list not exhaustive (n, %) | 7 (21.2) |
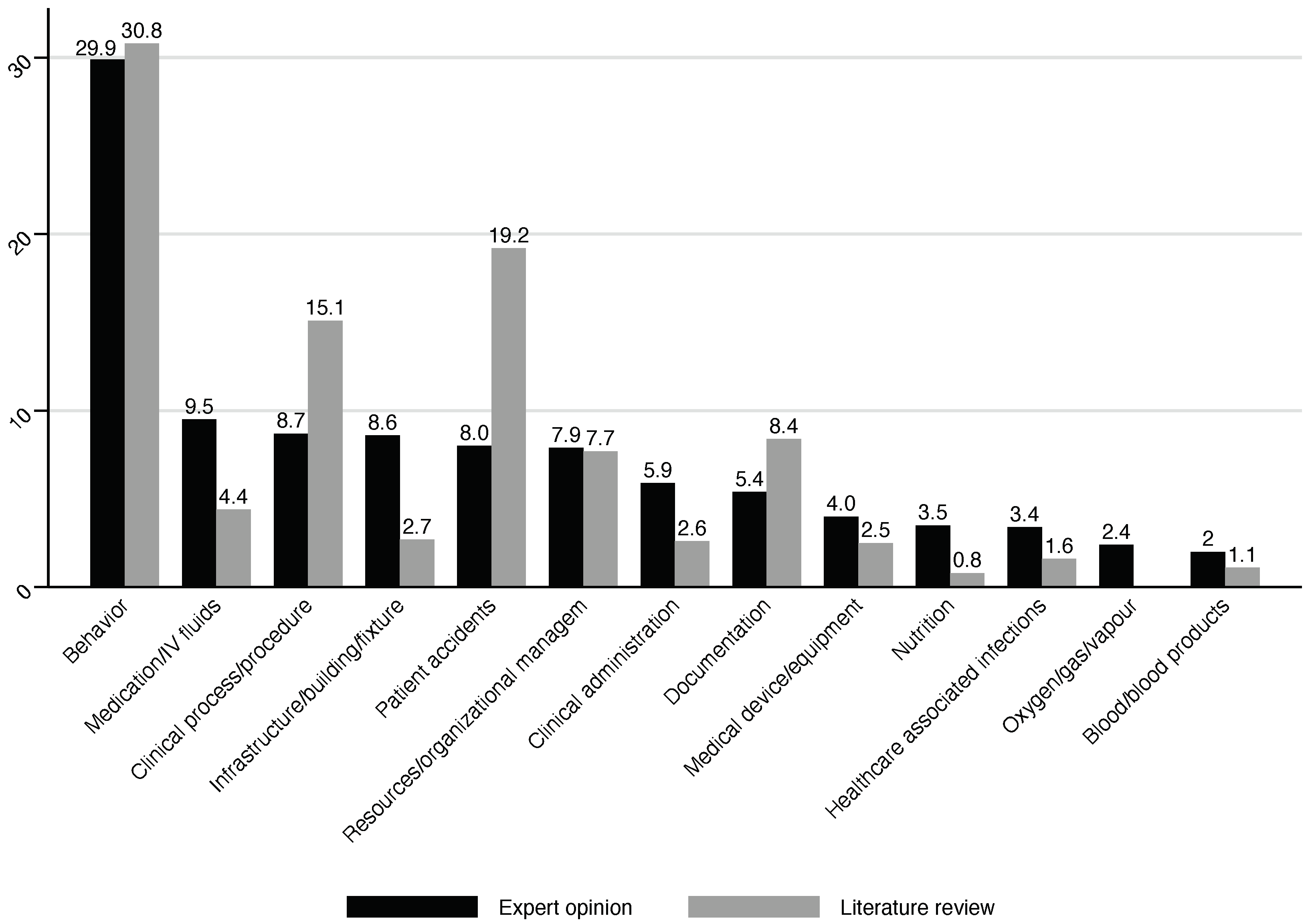
| Incident Type Category | Expert Opinion (Mean %, SD, ICC2K) | Literature Review (%) |
|---|---|---|
| Behavior | 29.9 (17.9, 0.91) | 30.8 |
| Medication/IV Fluids | 9.5 (11.6, 0.90) | 4.4 |
| Clinical Process/Procedure | 8.7 (6.6, 0.93) | 15.1 |
| Infrastructure/Building/Fixtures | 8.6 (7.2, 1.00) | 2.7 |
| Patient Accidents | 8.0 (8.1, 0.95) | 19.2 |
| Resources/Organizational Management | 7.9 (5.7, 0.89) | 7.7 |
| Clinical Administration | 5.9 (5.4, 0.89) | 2.6 |
| Documentation | 5.4 (3.6, 0.66) | 8.4 |
| Medical Device/Equipment | 4.0 (3.5, 0.86) | 2.5 |
| Nutrition | 3.5 (2.9, 0.90) | 0.8 |
| Healthcare-Associated Infections | 3.4 (2.9, 0.72) | 1.6 |
| Oxygen/Gas/Vapor | 2.4 (1.7, 0.93) | - |
| Blood/Blood Products | 2.0 (1.1, 0.89) | 1.1 |
| Patient Safety Incident | Expert Opinion (%) | Literature Review (%) |
|---|---|---|
| Patient behavior | ||
| Noncompliant/Uncooperative/Obstructive | 4.4 | 3.0 [28] |
| Inconsiderate/Rude/Hostile/Inappropriate | 3.2 | 0.3 [28] |
| Risky/Reckless/Dangerous | 3.1 | 1.5 [28] |
| Problem with Substance Use/Abuse | 3.2 | - |
| Harassment | 1.4 | - |
| Discrimination/Prejudice | 1.2 | 0.5 [28] |
| Wandering/Absconding | 1.4 | 0.5 [28] |
| Intended Self-Harm/Suicide | 3.4 | 0.9 [29] |
| Verbal Aggression | 2.9 | 0.2 [28] |
| Physical Assault | 2.0 | 0.2 [28] |
| Sexual Assault | 0.9 | - |
| Aggression Toward an Inanimate Object | 1.7 | 0.2 [28] |
| Death Threat | 1.1 | - |
| Infrastructure/Building/Fixtures | ||
| Nonexistent/Inadequate | 4.9 | 0 [30] |
| Damaged/Faulty/Worn | 3.8 | 0 [30] |
| Medication/IV Fluids | ||
| Wrong Patient | 0.5 | 0.8 [31] |
| Wrong Drug | 1.1 | 1.2 [29] |
| Wrong Dose/Strength of Frequency | 1.5 | 2.1 [32] |
| Wrong Formulation/Presentation | 0.6 | 2.1 [32] |
| Wrong Route | 0.5 | 0.5 [31] |
| Wrong Quantity | 0.7 | 3.4 [31] |
| Wrong Dispensing Label/Instruction | 0.5 | 0.2 [33] |
| Contraindication | 0.7 | 0.6 [31] |
| Wrong Storage | 0.5 | 1.0 [32] |
| Omitted Medicine or Dose | 1.0 | 0.3 [29] |
| Expired Medicine | 0.3 | 0.1 [33] |
| Adverse Drug Reaction | 0.9 | 2.5 [29] |
| Patient Accidents | ||
| Blunt Force | 0.7 | - |
| Piercing/Penetrating Force | 0.7 | 0.9 [34] |
| Other Mechanical Force | 0.7 | - |
| Thermal Mechanism | 1.3 | 0.3 [29] |
| Threat to Breathing | 1.2 | 0.9 [34] |
| Exposure to Chemical or Other Substance | 0.6 | - |
| Other Specified Mechanism of Injury | 0.5 | - |
| Exposure to/Effect of wWather, Natural Disaster, or Other Force of Nature | 0.7 | - |
| Falls | 2.2 | 11.3 [29] |
| Resources/Organizational management | ||
| Matching of Workload Management | 1.7 | 4.0 [34] |
| Bed/Service Availability/Adequacy | 1.3 | 0.3 [28] |
| Human Resource/Staff Availability/Adequacy | 1.9 | 2.8 [28] |
| Organization of Teams/People | 1.5 | 0.0 [28] |
| Protocols/Policy/Procedure/Guideline Availability/Adequacy | 1.5 | 0.5 [28] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Russotto, S.; Conti, A.; Vanhaecht, K.; Mira, J.J.; Panella, M. Patient Safety Incidents in Inpatient Psychiatric Settings: An Expert Opinion Survey. Behav. Sci. 2024, 14, 1116. https://doi.org/10.3390/bs14111116
Russotto S, Conti A, Vanhaecht K, Mira JJ, Panella M. Patient Safety Incidents in Inpatient Psychiatric Settings: An Expert Opinion Survey. Behavioral Sciences. 2024; 14(11):1116. https://doi.org/10.3390/bs14111116
Chicago/Turabian StyleRussotto, Sophia, Andrea Conti, Kris Vanhaecht, José Joaquín Mira, and Massimiliano Panella. 2024. "Patient Safety Incidents in Inpatient Psychiatric Settings: An Expert Opinion Survey" Behavioral Sciences 14, no. 11: 1116. https://doi.org/10.3390/bs14111116
APA StyleRussotto, S., Conti, A., Vanhaecht, K., Mira, J. J., & Panella, M. (2024). Patient Safety Incidents in Inpatient Psychiatric Settings: An Expert Opinion Survey. Behavioral Sciences, 14(11), 1116. https://doi.org/10.3390/bs14111116









