Examination of Congruity between Subjective and Objective Working Memory in Veterans with Mild TBI and Relation to Psychiatric Symptoms and Childhood Trauma
Abstract
1. Introduction
2. Materials and Methods
2.1. Inclusion and Exclusion Criteria
2.2. Evaluation and Clinical/Psychiatric Measures
2.3. Subjective and Objective Neurocognitive Measures
2.4. Statistical Analysis
3. Results
3.1. Patient Characteristics
3.2. Primary Aims
Concordance of Subjective and Objective Working Memory, Accounting for mTBI Severity, PTSD, and Childhood Trauma
3.3. Additional Aims
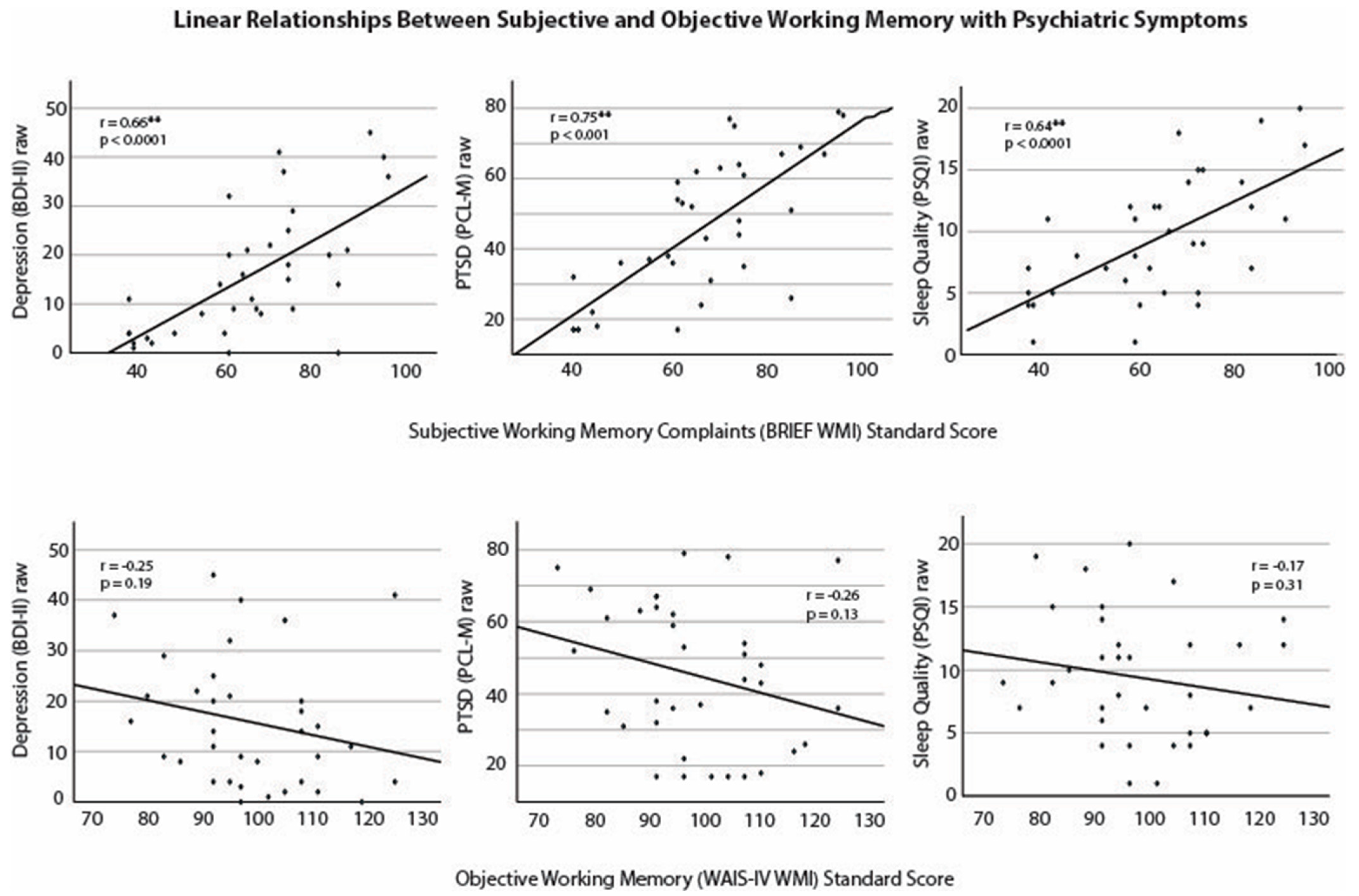
Relationships between Subjective and Objective Working Memory with PTSD Symptoms, Depression Symptoms, Sleep Quality, mTBI Severity, and Childhood Trauma
4. Discussion
4.1. Concordance between Subjective and Objective Working Memory
4.2. Subjective, and Not Objective, Working Memory Was Related to PTSD, Depression, and Sleep Symptoms
4.3. Possible Explanations for Subjective-Objective Cognitive Incongruity
4.4. Childhood Trauma and Subjective Cognitive Concerns
4.5. Importance of Continued Examination of Subjective Cognitive Complaints
4.6. Clinical Implications
4.7. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Terrio, H.; Brenner, L.A.; Ivins, B.J.; Cho, J.M.; Helmick, K.; Schwab, K.; Scally, K.; Bretthauer, R.; Warden, D. Traumatic brain injury screening: Preliminary findings in a US Army Brigade Combat Team. J. Head Trauma Rehabil. 2009, 24, 14–23. [Google Scholar] [CrossRef] [PubMed]
- Hoge, C.W.; McGurk, D.; Thomas, J.L.; Cox, A.L.; Engel, C.C.; Castro, C.A. Mild Traumatic brain injury in U.S. soldiers returning from Iraq. N. Engl. J. Med. 2008, 358, 453–463. [Google Scholar] [CrossRef] [PubMed]
- Schneiderman, A.I.; Braver, E.R.; Kang, H.K. Understanding sequelae of injury mechanisms and mild traumatic brain injury incurred during the conflicts in Iraq and afghanistan: Persistent postconcussive symptoms and posttraumatic stress disorder. Am. J. Epidemiol. 2008, 167, 1446–1452. [Google Scholar] [CrossRef] [PubMed]
- Lindquist, L.K.; Love, H.C.; Elbogen, E.B. Traumatic Brain Injury in Iraq and Afghanistan Veterans: New Results From a National Random Sample Study. J. Neuropsychiatry 2017, 29, 254–259. [Google Scholar] [CrossRef]
- Carlson, K.F.; Kehle, S.M.; Meis, L.A.; Greer, N.; MacDonald, R.; Rutks, I.; Sayer, N.A.; Dobscha, S.K.; Wilt, T.J. Prevalence, assessment, and treatment of mild traumatic brain injury and posttraumatic stress disorder: A systematic review of the evidence. J. Head Trauma Rehabil 2011, 26, 103–115. [Google Scholar] [CrossRef]
- Dieter, J.N.; Engel, S.D. Traumatic Brain Injury and Posttraumatic Stress Disorder: Comorbid Consequences of War. Neurosci. Insights 2019, 14, 1179069519892933. [Google Scholar] [CrossRef]
- Hayes, J.P. PTSD and TBI Comorbidity. PTSD Res. Q. 2019, 30. Available online: https://www.ptsd.va.gov/publications/rq_docs/V30N2.pdf (accessed on 1 April 2024).
- Tanev, K.S.; Pentel, K.Z.; Kredlow, M.A.; Charney, M.E. PTSD and TBI co-morbidity: Scope, clinical presentation and treatment options. Brain Inj. 2014, 28, 261–270. [Google Scholar] [CrossRef]
- Jackson, C.E.; Green, J.D.; Bovin, M.J.; Vasterling, J.J.; Holowka, D.W.; Ranganathan, G.; Rosen, R.C.; Keane, T.M.; Marx, B.P. Mild Traumatic Brain Injury, PTSD, and Psychosocial Functioning Among Male and Female U.S. OEF/OIF Veterans. J. Trauma. Stress. 2016, 29, 309–316. [Google Scholar] [CrossRef]
- Pietrzak, R.H.; Johnson, D.C.; Goldstein, M.B.; Malley, J.C.; Southwick, S.M. Posttraumatic stress disorder mediates the relationship between mild traumatic brain injury and health and psychosocial functioning in veterans of operations enduring freedom and Iraqi freedom. J. Nerv. Ment. Dis. 2009, 197, 748–753. [Google Scholar] [CrossRef]
- Vasterling, J.J.; Brailey, K.; Proctor, S.P.; Kane, R.; Heeren, T.; Franz, M. Neuropsychological outcomes of mild traumatic brain injury, post-traumatic stress disorder and depression in Iraq-deployed US Army soldiers. Br. J. Psychiatry 2012, 201, 186–192. [Google Scholar] [CrossRef] [PubMed]
- Owens, G.P.; Dashevsky, B.; Chard, K.M.; Mohamed, S.; Haji, U.; Heppner, P.S.; Baker, D.G. The Relationship Between Childhood Trauma, Combat Exposure, and Posttraumatic Stress Disorder in Male Veterans. Mil. Psychol. 2009, 21, 114–125. [Google Scholar] [CrossRef]
- Zaidi, L.Y.; Foy, D.W. Childhood abuse experiences and combat-related PTSD. J. Trauma. Stress. 1994, 7, 33–42. [Google Scholar] [CrossRef] [PubMed]
- Van Voorhees, E.E.; Dedert, E.A.; Calhoun, P.S.; Brancu, M.; Runnals, J.; Beckham, J.C.; VA Mid-Atlantic MIRECC Workgroup. Childhood trauma exposure in Iraq and Afghanistan war era veterans: Implications for posttraumatic stress disorder symptoms and adult functional social support. Child Abuse Negl. 2012, 36, 423–432. [Google Scholar] [CrossRef] [PubMed]
- Gillespie, C.F.; Phifer, J.; Bradley, B.; Ressler, K.J. Risk and resilience: Genetic and environmental influences on development of the stress response. Depress. Anxiety 2009, 26, 984–992. [Google Scholar] [CrossRef]
- Koenen, K.C. Developmental epidemiology of PTSD: Self-regulation as a central mechanism. Ann N. Y. Acad Sci. 2006, 1071, 255–266. [Google Scholar] [CrossRef]
- Snowden, T.M.; Hinde, A.K.; Reid, H.M.; Christie, B.R. Does Mild Traumatic Brain Injury Increase the Risk for Dementia? A Systematic Review and Meta-Analysis. J. Alzheimer’s Dis. 2020, 78, 757–775. [Google Scholar] [CrossRef]
- Lee, Y.-K.; Hou, S.-W.; Lee, C.-C.; Hsu, C.-Y.; Huang, Y.-S.; Su, Y.-C. Increased risk of dementia in patients with mild traumatic brain injury: A nationwide cohort study. PLoS ONE 2013, 8, e62422. [Google Scholar] [CrossRef]
- Barnes, D.E.; Byers, A.L.; Gardner, R.C.; Seal, K.H.; Boscardin, W.J.; Yaffe, K. Association of Mild Traumatic Brain Injury With and Without Loss of Consciousness With Dementia in US Military Veterans. JAMA Neurol. 2018, 75, 1055–1061. [Google Scholar] [CrossRef]
- Raza, Z.; Hussain, S.F.; Ftouni, S.; Spitz, G.; Caplin, N.; Foster, R.G.; Gomes, R.S.M. Dementia in military and veteran populations: A review of risk factors-traumatic brain injury, post-traumatic stress disorder, deployment, and sleep. Mil. Med. Res. 2021, 8, 55. [Google Scholar] [CrossRef]
- Pattinson, C.L.; Gill, J.M. Risk of dementia after TBI—A cause of growing concern. Nat. Rev. Neurol. 2018, 14, 511–512. [Google Scholar] [CrossRef] [PubMed]
- Günak, M.M.; Billings, J.; Carratu, E.; Marchant, N.L.; Favarato, G.; Orgeta, V. Post-traumatic stress disorder as a risk factor for dementia: Systematic review and meta-analysis. Br. J. Psychiatry 2020, 217, 600–608. [Google Scholar] [CrossRef] [PubMed]
- Yaffe, K.; Vittinghoff, E.; Lindquist, K.; Barnes, D.; Covinsky, K.E.; Neylan, T.; Kluse, M.; Marmar, C. Posttraumatic stress disorder and risk of dementia among US veterans. Arch. Gen. Psychiatry 2010, 67, 608–613. [Google Scholar] [CrossRef]
- Xie, Z.; Li, M.; Sun, H.; Zhou, C.; Fu, C.; Wang, Q.; Dong, C.; Hao, W.; Zhen, X.; Zhu, D. Childhood, adulthood, and cumulative traumatic events experienced from childhood to adulthood and dementia risk. J. Public Health 2023, 1–11. [Google Scholar] [CrossRef]
- Abouelmagd, M.E.; AbdelMeseh, M.; Elrosasy, A.; Eldeeb, H.A.; Nabil, Y. Adverse childhood experiences and risk of late-life dementia: A systematic review and meta-analysis. Soc. Psychiatry Psychiatr Epidemiol. 2024, 1–11. [Google Scholar] [CrossRef]
- Vespa, J. Aging Veterans: America’s Veteran Population in Later Life. In American Community Survey Reports; United States Census Bureau: Suitland, MD, USA, 2023. [Google Scholar]
- Wang, X.-T.; Wang, Z.-T.; Hu, H.-Y.; Qu, Y.; Wang, M.; Shen, X.-N.; Xu, W.; Dong, Q.; Tan, L.; Yu, J.-T. Association of Subjective Cognitive Decline with Risk of Cognitive Impairment and Dementia: A Systematic Review and Meta-Analysis of Prospective Longitudinal Studies. J. Prev. Alzheimer’s Dis. 2021, 8, 277–285. [Google Scholar] [CrossRef]
- Ávila-Villanueva, M.; Rebollo-Vázquez, A.; de León, J.M.R.-S.; Valentí, M.; Medina, M.; Fernández-Blázquez, M.A. Clinical Relevance of Specific Cognitive Complaints in Determining Mild Cognitive Impairment from Cognitively Normal States in a Study of Healthy Elderly Controls. Front. Aging Neurosci. 2016, 8, 233. [Google Scholar] [CrossRef]
- Dubois, B.; Hampel, H.; Feldman, H.H.; Scheltens, P.; Aisen, P.; Andrieu, S.; Bakardjian, H.; Benali, H.; Bertram, L.; Blennow, K.; et al. Preclinical Alzheimer’s disease: Definition, natural history, and diagnostic criteria. Alzheimers Dement 2016, 12, 292–323. [Google Scholar] [CrossRef]
- Jessen, F.; Amariglio, R.E.; Van Boxtel, M.; Breteler, M.; Ceccaldi, M.; Chételat, G.; Dubois, B.; Dufouil, C.; Ellis, K.A.; Van Der Flier, W.M.; et al. A conceptual framework for research on subjective cognitive decline in preclinical Alzheimer’s disease. Alzheimers Dement 2014, 10, 844–852. [Google Scholar] [CrossRef]
- Jessen, F.; Amariglio, R.E.; Buckley, R.F.; van der Flier, W.M.; Han, Y.; Molinuevo, J.L.; Rabin, L.; Rentz, D.M.; Rodriguez-Gomez, O.; Saykin, A.J.; et al. The characterisation of subjective cognitive decline. Lancet Neurol. 2020, 19, 271–278. [Google Scholar] [CrossRef]
- Jonker, C.; Geerlings, M.I.; Schmand, B. Are memory complaints predictive for dementia? A review of clinical and population-based studies. Int. J. Geriatr. Psychiatry 2000, 15, 983–991. [Google Scholar] [CrossRef] [PubMed]
- Reid, L.M.; MacLullich, A.M. Subjective memory complaints and cognitive impairment in older people. Dement. Geriatr. Cogn. Disord. 2006, 22, 471–485. [Google Scholar] [CrossRef] [PubMed]
- Stewart, R. Mild cognitive impairment—The continuing challenge of its “real-world” detection and diagnosis. Arch Med. Res. 2012, 43, 609–614. [Google Scholar] [CrossRef] [PubMed]
- Amick, M.M.; Meterko, M.; Fortier, C.B.; Fonda, J.R.; Milberg, W.P.; McGlinchey, R.E. The Deployment Trauma Phenotype and Employment Status in Veterans of the Wars in Iraq and Afghanistan. J. Head. Trauma. Rehabil. 2018, 33, E30–E40. [Google Scholar] [CrossRef] [PubMed]
- Seal, K.H.; Bertenthal, D.; Samuelson, K.; Maguen, S.; Kumar, S.; Vasterling, J.J. Association between mild traumatic brain injury and mental health problems and self-reported cognitive dysfunction in Iraq and Afghanistan Veterans. J. Rehabil. Res. Dev. 2016, 53, 185–198. [Google Scholar] [CrossRef] [PubMed]
- Purri, R.; Brennan, L.; Rick, J.; Xie, S.X.; Deck, B.L.; Chahine, L.M.; Dahodwala, N.; Chen-Plotkin, A.; Duda, J.E.; Morley, J.F.; et al. Subjective Cognitive Complaint in Parkinson’s Disease Patients With Normal Cognition: Canary in the Coal Mine? Mov. Disord 2020, 35, 1618–1625. [Google Scholar] [CrossRef]
- Siciliano, M.; Trojano, L.; De Micco, R.; Sant’elia, V.; Giordano, A.; Russo, A.; Passamonti, L.; Tedeschi, G.; Chiorri, C.; Tessitore, A. Correlates of the discrepancy between objective and subjective cognitive functioning in non-demented patients with Parkinson’s disease. Neurol 2021, 268, 3444–3455. [Google Scholar] [CrossRef]
- Thomas, G.A.; Riegler, K.E.; Bradson, M.L.; O’shea, D.U.; Arnett, P.A. Relationship between subjective report and objective assessment of neurocognitive functioning in persons with multiple sclerosis. J. Int. Neuropsychol. Soc. 2023, 29, 266–273. [Google Scholar] [CrossRef]
- Srisurapanont, M.; Suttajit, S.; Eurviriyanukul, K.; Varnado, P. Discrepancy between objective and subjective cognition in adults with major depressive disorder. Sci. Rep. 2017, 7, 3901. [Google Scholar] [CrossRef]
- Burmester, B.; Leathem, J.; Merrick, P. Subjective Cognitive Complaints and Objective Cognitive Function in Aging: A Systematic Review and Meta-Analysis of Recent Cross-Sectional Findings. Neuropsychol. Rev. 2016, 26, 376–393. [Google Scholar] [CrossRef]
- Crumley, J.J.; Stetler, C.A.; Horhota, M. Examining the relationship between subjective and objective memory performance in older adults: A meta-analysis. Psychol. Aging 2014, 29, 250–263. [Google Scholar] [CrossRef] [PubMed]
- Merritt, V.C.; Jurick, S.M.; Crocker, L.D.; Sullan, M.J.; Sakamoto, M.S.; Davey, D.K.; Hoffman, S.N.; Keller, A.V.; Jak, A.J. Associations Between Multiple Remote Mild TBIs and Objective Neuropsychological Functioning and Subjective Symptoms in Combat-Exposed Veterans. Arch. Clin. Neuropsychol. 2020, 35, 491–505. [Google Scholar] [CrossRef] [PubMed]
- Neale, A.C.; Aase, D.M.; Soble, J.R.; Baker, J.C.; Phan, K.L. Disentangling subjective symptom complaints and objective cognitive performance in veterans: Impact of posttraumatic stress disorder and lifetime traumatic brain injury burden. Appl. Neuropsychol. Adult 2022, 31, 948–963. [Google Scholar] [CrossRef] [PubMed]
- Scott, T.; Spellman, J.; Walker, N.; Rivera, J.; Waltzman, D.; Mcnerney, M.; Madore, M. A-09 The Relationship Between Subjective Cognitive Complaints, Depression, and Executive Functioning in TBI Veterans. Arch. Clin. Neuropsychol. 2020, 35, 782. [Google Scholar] [CrossRef]
- Shwartz, S.K.; Roper, B.L.; Arentsen, T.J.; Crouse, E.M.; Adler, M.C. The Behavior Rating Inventory of Executive Function(R)-Adult Version is Related to Emotional Distress, Not Executive Dysfunction, in a Veteran Sample. Arch Clin. Neuropsychol. 2020, 35, 701–716. [Google Scholar] [CrossRef]
- Donnelly, K.; Donnelly, J.P.; Warner, G.C.; Kittleson, C.J.; King, P.R. Longitudinal study of objective and subjective cognitive performance and psychological distress in OEF/OIF Veterans with and without traumatic brain injury. Clin. Neuropsychol. 2017, 32, 436–455. [Google Scholar] [CrossRef]
- Clark, J.M.R.; Mahmood, Z.; Jak, A.J.; Huckans, M.; O’Neil, M.E.; Roost, M.S.; Williams, R.M.; Turner, A.P.; Pagulayan, K.F.; Storzbach, D.; et al. Neuropsychological Performance and Functional Capacity Following Mild Traumatic Brain Injury in Veterans. J. Head. Trauma. Rehabil. 2022, 37, E488–E495. [Google Scholar] [CrossRef]
- Clausen, A.N.; Bouchard, H.C.; Workgroup, V.M.-A.M.; Welsh-Bohmer, K.A.; Morey, R.A. Assessment of Neuropsychological Function in Veterans With Blast-Related Mild Traumatic Brain Injury and Subconcussive Blast Exposure. Front. Psychol. 2021, 12, 686330. [Google Scholar] [CrossRef]
- Geuze, E.; Vermetten, E.; de Kloet, C.S.; Hijman, R.; Westenberg, H.G.M. Neuropsychological performance is related to current social and occupational functioning in veterans with posttraumatic stress disorder. Depress. Anxiety 2009, 26, 7–15. [Google Scholar] [CrossRef]
- Koso, M.; Hansen, S. Executive function and memory in posttraumatic stress disorder: A study of Bosnian war veterans. Eur. Psychiatry 2006, 21, 167–173. [Google Scholar] [CrossRef]
- Esopenko, C.; de Souza, N.L.M.; Jia, Y.; Parrott, J.S.; Merkley, T.L.; Dennis, E.L.; Hillary, F.G.; Velez, C.M.; Cooper, D.B.; Kennedy, J.; et al. Latent Neuropsychological Profiles to Discriminate Mild Traumatic Brain Injury and Posttraumatic Stress Disorder in Active-Duty Service Members. J. Head. Trauma. Rehabil. 2022, 37, E438–E448. [Google Scholar] [CrossRef] [PubMed]
- Jagger-Rickels, A.; Rothlein, D.; Stumps, A.; Evans, T.C.; Bernstein, J.; Milberg, W.; McGlinchey, R.; DeGutis, J.; Esterman, M. An executive function subtype of PTSD with unique neural markers and clinical trajectories. Transl. Psychiatry 2022, 12, 262. [Google Scholar] [CrossRef] [PubMed]
- Jurick, S.M.; Crocker, L.D.; Merritt, V.C.; Sanderson-Cimino, M.E.; Keller, A.V.; Glassman, L.H.; Twamley, E.W.; Rodgers, C.S.; Schiehser, D.M.; Aupperle, R.L.; et al. Independent and Synergistic Associations Between TBI Characteristics and PTSD Symptom Clusters on Cognitive Performance and Postconcussive Symptoms in Iraq and Afghanistan Veterans. J. Neuropsychiatry Clin. Neurosci. 2021, 33, 98–108. [Google Scholar] [CrossRef] [PubMed]
- Karr, J.E.; Rau, H.K.; Shofer, J.B.; Hendrickson, R.C.; Peskind, E.R.; Pagulayan, K.F. Variables associated with subjective cognitive change among Iraq and Afghanistan war Veterans with blast-related mild traumatic brain injury. J. Clin. Exp. Neuropsychol. 2019, 41, 680–693. [Google Scholar] [CrossRef] [PubMed]
- Mattson, E.K.; Nelson, N.W.; Sponheim, S.R.; Disner, S.G. The Impact of PTSD and mTBI on the Relationship between Subjective and Objective Cognitive Deficits in Combat-Exposed Veterans. Neuropsychology 2019, 33, 913–921. [Google Scholar] [CrossRef] [PubMed]
- Pagulayan, K.F.; Petrie, E.C.; Cook, D.G.; Hendrickson, R.C.; Rau, H.; Reilly, M.; Mayer, C.; Meabon, J.S.; Raskind, M.A.; Peskind, E.R.; et al. Effect of blast-related mTBI on the working memory system: A resting state fMRI study. Brain Imaging Behav. 2020, 14, 949–960. [Google Scholar] [CrossRef]
- Brown, M.J.; Kaur, A.; James, T.; Avalos, C.; Addo, P.N.O.; Crouch, E.; Hill, N.L. Adverse Childhood Experiences and Subjective Cognitive Decline in the US. J. Appl. Gerontol. 2022, 41, 1090–1100. [Google Scholar] [CrossRef]
- Terry, R.M.; Schiffmacher, S.E.; Dutcher, A.A.; Croff, J.M.; Jelley, M.J.; Hartwell, M.L. Adverse childhood experience categories and subjective cognitive decline in adulthood: An analysis of the Behavioral Risk Factor Surveillance System. J. Am. Osteopat. Assoc. 2023, 123, 125–133. [Google Scholar] [CrossRef]
- Baiden, P.; Cassidy, J.; Panisch, L.S.; LaBrenz, C.A.; Onyeaka, H.K. Association of adverse childhood experiences with subjective cognitive decline in adulthood: Findings from a population-based study. Aging Ment. Health 2021, 26, 2214–2222. [Google Scholar] [CrossRef]
- Madigan, S.; Deneault, A.; Racine, N.; Park, J.; Thiemann, R.; Zhu, J.; Dimitropoulos, G.; Williamson, T.; Fearon, P.; Cénat, J.M.; et al. Adverse childhood experiences: A meta-analysis of prevalence and moderators among half a million adults in 206 studies. World Psychiatry 2023, 22, 463–471. [Google Scholar] [CrossRef]
- Blosnich, J.R.; Dichter, M.E.; Cerulli, C.; Batten, S.V.; Bossarte, R.M. Disparities in adverse childhood experiences among individuals with a history of military service. JAMA Psychiatry 2014, 71, 1041–1048. [Google Scholar] [CrossRef] [PubMed]
- Aronson, K.R.; Perkins, D.F.; Morgan, N.R.; Bleser, J.A.; Vogt, D.; Copeland, L.A.; Finley, E.P.; Gilman, C.L. The impact of adverse childhood experiences (ACEs) and combat exposure on mental health conditions among new post-9/11 veterans. Psychol Trauma 2020, 12, 698–706. [Google Scholar] [CrossRef] [PubMed]
- Giano, Z.; Wheeler, D.L.; Hubach, R.D. The frequencies and disparities of adverse childhood experiences in the U.S. BMC Public Health 2020, 20, 1327. [Google Scholar] [CrossRef] [PubMed]
- Weathers, F.; Huska, J.; Keane, T. The PTSD Checklist Military Version (PCL-M); National Center for PTSD: Boston, MA, USA, 1991. [Google Scholar]
- Blanchard, E.B.; Jones-Alexander, J.; Buckley, T.C.; Forneris, C.A. Psychometric properties of the PTSD checklist (PCL). Behav. Res. Ther. 1996, 34, 669. [Google Scholar] [CrossRef] [PubMed]
- Beck, A.T.; Steer, R.A.; Brown, G.K. Manual for the Beck Depression Inventory-II; Psychological Corporation: San Antonio, TX, USA, 1996. [Google Scholar]
- Buysse, D.J.; Reynolds, C.F.; Monk, T.H.; Hoch, C.C.; Yeager, A.L.; Kupfer, D.J. Quantification of subjective sleep quality in healthy elderly men and women using the pittsburgh sleep quality index (PSQI). Sleep 1991, 14, 331–338. [Google Scholar] [CrossRef]
- Gioia, G.A.; Isquith, P.K.; Guy, S.C.; Kenworthy, L. The Behavior Rating Inventory of Executive Function; Psychological Assessment Resources: Lutz, FL, USA, 2000. [Google Scholar]
- Hill, N.L.; Mogle, J.; Wion, R.; Munoz, E.; DePasquale, N.; Yevchak, A.M.; Parisi, J.M. Subjective Cognitive Impairment and Affective Symptoms: A Systematic Review. Gerontologist 2016, 56, e109–e127. [Google Scholar] [CrossRef]
- Caplan, B.; Bogner, J.; Brenner, L.; Malec, J.; Hromas, G.A.; Houck, Z.M.; Bauer, R.M. Making a difference: Affective distress explains discrepancy between objective and subjective cognitive functioning after mild traumatic brain injury. J. Head Trauma Rehabil. 2021, 36, 186–195. [Google Scholar]
- Karr, J.E.; Hakun, J.G.; Elbich, D.B.; Pinheiro, C.N.; Schmitt, F.A.; Segerstrom, S.C. Detecting cognitive decline in high-functioning older adults: The relationship between subjective cognitive concerns, frequency of high neuropsychological test scores, and the frontoparietal control network. J. Int. Neuropsychol. Soc. 2024, 30, 220–231. [Google Scholar] [CrossRef]
- Lista, S.; Molinuevo, J.L.; Cavedo, E.; Rami, L.; Amouyel, P.; Teipel, S.J.; Garaci, F.; Toschi, N.; Habert, M.-O.; Blennow, K.; et al. Evolving Evidence for the Value of Neuroimaging Methods and Biological Markers in Subjects Categorized with Subjective Cognitive Decline. J. Alzheimer’s Dis. 2015, 48 (Suppl. S1), S171–S191. [Google Scholar] [CrossRef]
- Madison, A.A.; Andridge, R.; Kantaras, A.H.; Renna, M.E.; Bennett, J.M.; Alfano, C.M.; Povoski, S.P.; Agnese, D.M.; Lustberg, M.; Wesolowski, R.; et al. Depression, Inflammation, and Intestinal Permeability: Associations with Subjective and Objective Cognitive Functioning throughout Breast Cancer Survivorship. Cancers 2023, 15, 4414. [Google Scholar] [CrossRef]
- Holiday, K.A.; Clark, A.L.; Merritt, V.C.; Nakhla, M.Z.; Sorg, S.; Delano-Wood, L.; Schiehser, D.M. Response inhibition in Veterans with a history of mild traumatic brain injury: The role of self-reported complaints in objective performance. J. Clin. Exp. Neuropsychol. 2020, 42, 556–568. [Google Scholar] [CrossRef] [PubMed]
- Majer, M.; Nater, U.M.; Lin, J.-M.S.; Capuron, L.; Reeves, W.C. Association of childhood trauma with cognitive function in healthy adults: A pilot study. BMC Neurol. 2010, 10, 61. [Google Scholar] [CrossRef]
- Dodaj, A.; Krajina, M.; Sesar, K.; Šimić, N. The Effects of Maltreatment in Childhood on Working Memory Capacity in Adulthood. Eur. J. Psychol. 2017, 13, 618–632. [Google Scholar] [CrossRef] [PubMed]
- McGlinchey, R.E.; Milberg, W.P.; Fonda, J.R.; Fortier, C.B. A methodology for assessing deployment trauma and its consequences in OEF/OIF/OND veterans: The TRACTS longitudinal prospective cohort study. Int. J. Methods Psychiatr. Res. 2017, 26, e1556. [Google Scholar] [CrossRef] [PubMed]
- Dyball, D.; Evans, S.; Boos, C.J.; Stevelink, S.A.M.; Fear, N.T. The association between PTSD and cardiovascular disease and its risk factors in male veterans of the Iraq/Afghanistan conflicts: A systematic review. Int. Rev. Psychiatry 2019, 31, 34–48. [Google Scholar] [CrossRef]
- Mitchell, A.J.; Beaumont, H.; Ferguson, D.; Yadegarfar, M.; Stubbs, B. Risk of dementia and mild cognitive impairment in older people with subjective memory complaints: Meta-analysis. Acta Psychiatr. Scand. 2014, 130, 439–451. [Google Scholar] [CrossRef]
- Pike, K.E.; Cavuoto, M.G.; Li, L.; Wright, B.J.; Kinsella, G.J. Subjective Cognitive Decline: Level of Risk for Future Dementia and Mild Cognitive Impairment, a Meta-Analysis of Longitudinal Studies. Neuropsychol. Rev. 2022, 32, 703–735. [Google Scholar] [CrossRef]
- An, R.; Gao, Y.; Huang, X.; Yang, Y.; Yang, C.; Wan, Q. Predictors of progression from subjective cognitive decline to objective cognitive impairment: A systematic review and meta-analysis of longitudinal studies. Int. J. Nurs. Stud. 2024, 149, 104629. [Google Scholar] [CrossRef]
- Ly, M.T.; Merritt, V.C.; Ozturk, E.D.; Clark, A.L.; Hanson, K.L.; Delano-Wood, L.M.; Sorg, S.F. Subjective memory complaints are associated with decreased cortical thickness in Veterans with histories of mild traumatic brain injury. Clin. Neuropsychol. 2023, 37, 1745–1765. [Google Scholar] [CrossRef]
- Levine, T.F.; Dessenberger, S.J.; Allison, S.L.; Head, D.; Initiative, T.A.D.N. Alzheimer disease biomarkers are associated with decline in subjective memory, attention, and spatial navigation ability in clinically normal adults. J. Int. Neuropsychol. Soc. 2024, 30, 313–327. [Google Scholar] [CrossRef]
- Hill, N.L.; McDermott, C.; Mogle, J.; Munoz, E.; DePasquale, N.; Wion, R.; Whitaker, E. Subjective cognitive impairment and quality of life: A systematic review. Int. Psychogeriatr. 2017, 29, 1965–1977. [Google Scholar] [CrossRef] [PubMed]
- Roehr, S.; Luck, T.; Pabst, A.; Bickel, H.; König, H.-H.; Lühmann, D.; Fuchs, A.; Wolfsgruber, S.; Wiese, B.; Weyerer, S.; et al. Subjective cognitive decline is longitudinally associated with lower health-related quality of life. Int. Psychogeriatr. 2017, 29, 1939–1950. [Google Scholar] [CrossRef] [PubMed]
- Wojcik, B.E.; Stein, C.R.; Bagg, K.; Humphrey, R.J.; Orosco, J. Traumatic brain injury hospitalizations of U.S. army soldiers deployed to afghanistan and Iraq. Am. J. Prev. Med. 2010, 38 (Suppl. S1), S108–S116. [Google Scholar] [CrossRef] [PubMed]
| M (SD) or n (%) | |
|---|---|
| Age | 44 (14) |
| Gender | |
| Male | 31 (87%) |
| Female | 4 (11%) |
| Race | |
| White | 24 (69%) |
| Black | 4 (11%) |
| Asian | 2 (6%) |
| American Indian/Alaska Native | 1 (3%) |
| Native Hawaiian/Pacific Islander | 2 (6%) |
| Prefers not to answer | 1 (3%) |
| Other | 1 (3%) |
| Ethnicity | |
| Hispanic or Latino | 25 (72%) |
| Non-Hispanic | 8 (23%) |
| Unknown | 2 (6%) |
| Education (years) | 14 (2) |
| HS graduate or less | 3 (9%) |
| Some college | 18 (51%) |
| College graduate | 12 (34%) |
| Post college | 2 (6%) |
| Handedness | |
| Right | 30 (86%) |
| Left | 3 (9%) |
| Amidexterous | 2 (6%) |
| PTSD a | |
| No PTSD | 18 (51%) |
| PTSD | 17 (49%) |
| Depression (BDI-II) | 15 (13) |
| Sleep Quality | 9 (5) |
| PTSD Checklist | 45 (20) |
| WAIS WMI | 98 (13) |
| BRIEF WMI | 65 (17) |
| Variable | B | SE | β | t | Sig. |
|---|---|---|---|---|---|
| (Intercept) | 1.33 | 18.80 | 0.07 | 0.94 | |
| Objective working memory (WAIS WMI) | 0.30 | 0.16 | 0.23 | 1.85 | 0.07 |
| PTSD (PCL-M) | 0.64 | 0.10 | 0.78 | 6.49 | <0.0001 ** |
| mTBI severity | −0.60 | 1.16 | −0.07 | −0.52 | 0.61 |
| Childhood trauma | 3.18 | 1.33 | 0.30 | 2.40 | 0.02 * |
| R | R-sq. | F | Sig. | ||
| DV: Subjective working memory (BRIEF WMI) | 0.80 | 0.53 | 13.14 | <0.0001 ** |
| Full mTBI Sample (N = 35) | mTBI + PTSD a (n = 18) | mTBI + no PTSD a (n = 17) | ||
|---|---|---|---|---|
| Objective Working Memory | n (%) | n (%) | n (%) | |
| WAIS-IV WMI | ||||
| Low | 0 (0%) | 0 (0%) | 0 (0%) | |
| Normal | 5 (14%) | 4 (22%) | 1 (6%) | |
| High | 30 (86%) | 14 (78%) | 16 (94%) | |
| Subjective Working Memory | ||||
| BRIEF WMI | ||||
| Low | 3 (9%) | 0 (0%) | 3 (18%) | |
| Normal | 8 (23%) | 0 (0%) | 8 (47%) | |
| High | 24 (69%) | 18 (100%) | 6 (35%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cruz, L.N.; Walker, N.C.; Rehman, S.S.; McNerney, M.W.; Madore, M.R. Examination of Congruity between Subjective and Objective Working Memory in Veterans with Mild TBI and Relation to Psychiatric Symptoms and Childhood Trauma. Behav. Sci. 2024, 14, 932. https://doi.org/10.3390/bs14100932
Cruz LN, Walker NC, Rehman SS, McNerney MW, Madore MR. Examination of Congruity between Subjective and Objective Working Memory in Veterans with Mild TBI and Relation to Psychiatric Symptoms and Childhood Trauma. Behavioral Sciences. 2024; 14(10):932. https://doi.org/10.3390/bs14100932
Chicago/Turabian StyleCruz, Lisa N., Nicole C. Walker, Sonia S. Rehman, M. Windy McNerney, and Michelle R. Madore. 2024. "Examination of Congruity between Subjective and Objective Working Memory in Veterans with Mild TBI and Relation to Psychiatric Symptoms and Childhood Trauma" Behavioral Sciences 14, no. 10: 932. https://doi.org/10.3390/bs14100932
APA StyleCruz, L. N., Walker, N. C., Rehman, S. S., McNerney, M. W., & Madore, M. R. (2024). Examination of Congruity between Subjective and Objective Working Memory in Veterans with Mild TBI and Relation to Psychiatric Symptoms and Childhood Trauma. Behavioral Sciences, 14(10), 932. https://doi.org/10.3390/bs14100932





