Anxious-Withdrawal and Sleep Problems during Adolescence: The Moderating Role of Peer Difficulties
Abstract
:1. Introduction
1.1. Anxious-Withdrawal and Sleep
1.2. The Role of Peer Difficulties
1.3. The Present Study
2. Materials and Methods
2.1. Participants and Procedures
2.2. Measures
2.2.1. School Measures (T1)
2.2.2. Laboratory Measures (T1, T2)
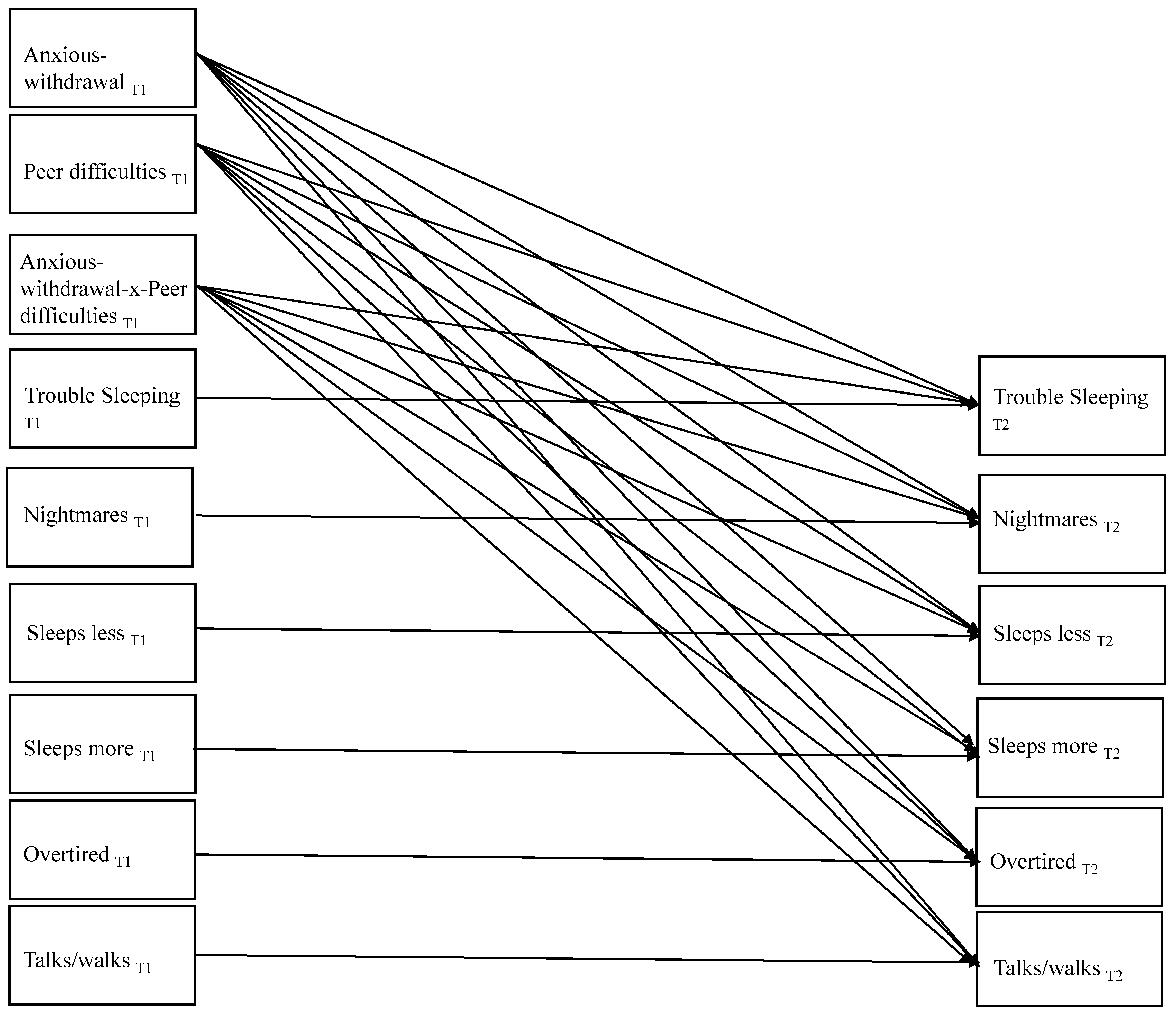
2.3. Data Analysis
3. Results
3.1. Preliminary Analyses
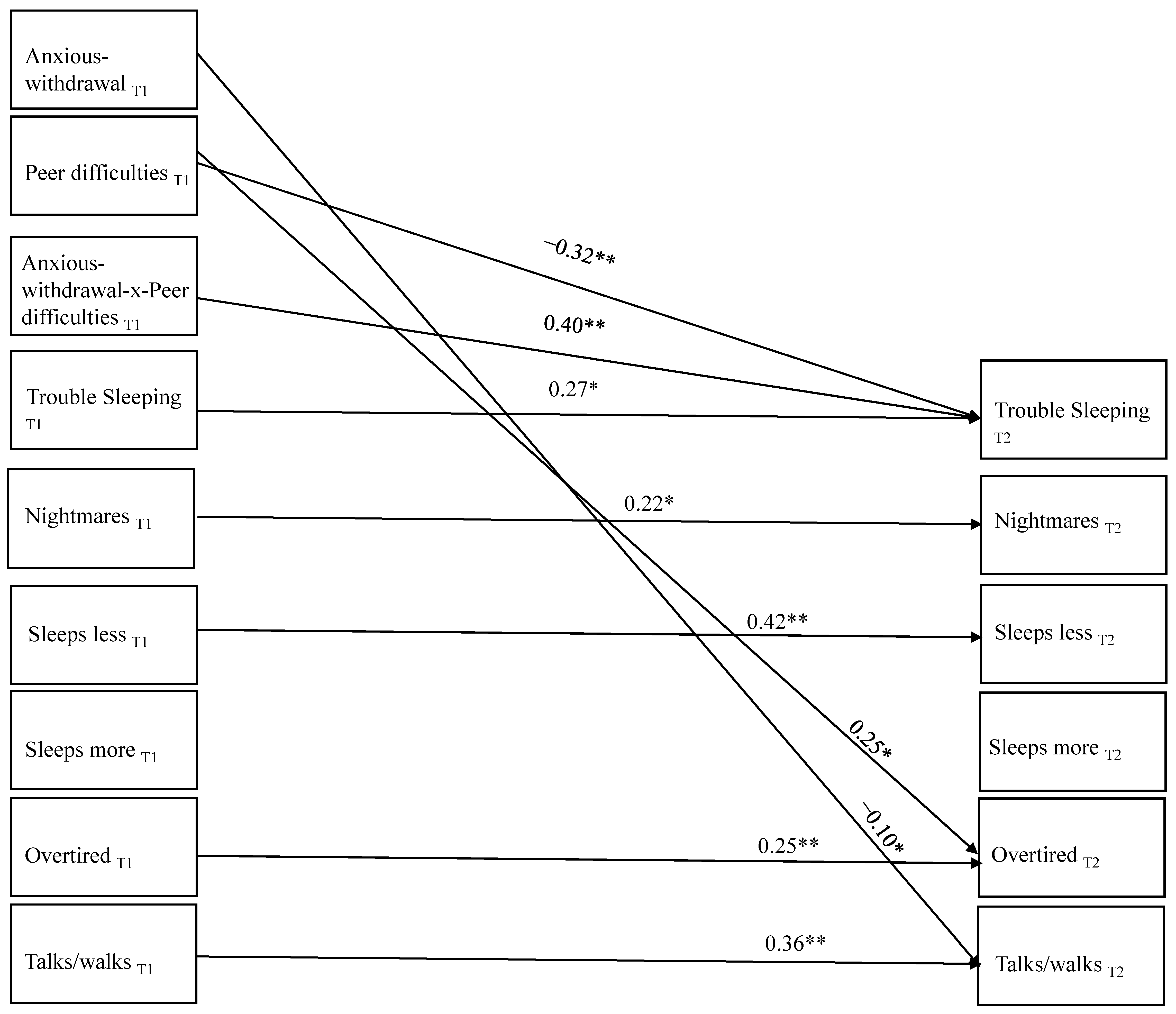
3.2. Primary Analyses
3.3. Exploratory Analyses
3.3.1. Evaluation of Sex Differences
3.3.2. Youth Self-Reports of Sleep Difficulties
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Rubin, K.H.; Chronis-Tuscano, A. Perspectives on social withdrawal in childhood: Past, present, and prospects. Child Dev. Perspect. 2021, 15, 160–167. [Google Scholar] [CrossRef] [PubMed]
- Gazelle, H.; Ladd, G.W. Anxious solitude and peer exclusion: A diathesis-stress model of internalizing trajectories in childhood. Child Dev. 2003, 74, 257–278. [Google Scholar] [CrossRef] [PubMed]
- Boivin, M.; Hymel, S.; Bukowski, W.M. The roles of social withdrawal, peer rejection, and victimization by peers in predicting loneliness and depressed mood in childhood. Dev. Psychopathol. 1995, 7, 765–785. [Google Scholar] [CrossRef]
- Rubin, K.H.; Chen, X.; McDougall, P.; Bowker, A.; McKinnon, J. The Waterloo Longitudinal Project: Predicting adolescent internalizing and externalizing problems from early and mid-childhood. Dev. Psychopathol. 1995, 7, 751–764. [Google Scholar] [CrossRef]
- Alfano, C.A.; Zakem, A.H.; Costa, N.M.; Taylor, L.K.; Weems, C.F. Sleep problems and their relation to cognitive factors, anxiety, and depressive symptoms in children and adolescents. Depress. Anxiety 2009, 26, 503–512. [Google Scholar] [CrossRef] [PubMed]
- Kelly, R.J.; Zeringue, M.M.; El-Sheikh, M. Adolescents’ sleep and adjustment: Reciprocal effects. Child Dev. 2021, 93, 540–555. [Google Scholar] [CrossRef] [PubMed]
- Palmer, C.A.; Oosterhoff, B.; Bower, J.L.; Kaplow, J.B.; Alfano, C.A. Associations among adolescent sleep problems, emotion regulation, and affective disorders: Findings from a nationally representative sample. J. Psychiatr. Res. 2018, 96, 1–8. [Google Scholar] [CrossRef]
- Kann, L.; McManus, T.; Harris, W.A.; Shanklin, S.L.; Flint, K.H.; Queen, B.; Lowry, R.; Chyen, D.; Whittle, L.; Thornton, J.; et al. Youth risk behavior surveillance—United States, 2017. MMWR Surveill. Summ. 2018, 67, 1–114. [Google Scholar] [CrossRef]
- Dikeos, D.; Georgantopoulos, G. Medical comorbidity of sleep disorders. Curr. Opin. Psychiatry 2011, 24, 346–354. [Google Scholar] [CrossRef]
- Freeman, D.; Sheaves, B.; Waite, F.; Harvey, A.G.; Harrison, P.J. Sleep disturbance and psychiatric disorders. Lancet Psychiatry 2020, 7, 628–637. [Google Scholar] [CrossRef]
- Orchard, F.; Gregory, A.M.; Gradisar, M.; Reynolds, S. Self-reported sleep patterns and quality amongst adolescents: Cross-sectional and prospective associations with anxiety and depression. J. Child Psychol. Psychiatry 2020, 61, 1126–1137. [Google Scholar] [CrossRef]
- Berger, R.H.; Diaz, A.; Valiente, C.; Eisenberg, N.; Sprinrad, T.L.; Thompson, M.S.; Hernandez, M.M.; VanSchyndel, S.K.; Southworth, J. Sleep duration moderates the association between children’s temperament and academic achievement. Early Educ. Dev. 2018, 29, 624–640. [Google Scholar] [CrossRef] [PubMed]
- Simola, P.; Liukkonen, K.; Pitkaranta, A.; Pirinen, T.; Aronen, E.T. Psychosocial and somatic outcomes of sleep problems in children: A 4-year follow-up study. Child Care Health Dev. 2012, 40, 60–67. [Google Scholar] [CrossRef]
- Oh, W.; Rubin, K.H.; Bowker, J.C.; Booth-LaForce, C.L.; Rose-Krasnor, L.; Laursen, B. Trajectories of social withdrawal from middle childhood to early adolescence. J. Abnorm. Child Psychol. 2008, 36, 553–556. [Google Scholar] [CrossRef]
- Lamoureux, V.A.; Glenn, A.L.; Ling, S.; Raine, A.; Ang, R.P.; Fung, D. The role of anxiety and callous-unemotional traits in the relationship between externalizing behaviors and sleep problems in clinic-referred youth. Clin. Child Psychol. Psychiatry 2023, 28, 654–667. [Google Scholar] [CrossRef] [PubMed]
- Alfano, C.A.; Ginsburg, G.S.; Kingery, J.N. Sleep-related problems among children and adolescents with anxiety disorder. J. Am. Acad. Child Adolesc. Psychiatry 2007, 46, 224–232. [Google Scholar] [CrossRef]
- McMakin, D.L.; Alfano, C.A. Sleep and anxiety in late childhood and early adolescence. Curr. Opin. Psychiatry 2015, 28, 483–489. [Google Scholar] [CrossRef]
- Gazelle, H.; Workman, J.O.; Allan, W. Anxious solitude and clinical disorder in middle childhood: Bridging developmental and clinical approaches to childhood social anxiety. J. Abnorm. Child Psychol. 2010, 38, 1–17. [Google Scholar] [CrossRef]
- Hom, M.A.; Chu, C.; Rogers, M.L.; Joiner, T.E. A meta-analysis of the relationship between sleep problems and loneliness. Clin. Psychol. Sci. 2020, 8, 799–824. [Google Scholar] [CrossRef]
- Cacioppo, J.T.; Hawkley, L.C.; Berntson, G.G.; Ernst, J.M.; Gibbs, A.C.; Stickgold, R.; Hobson, J.A. Do lonely days invade the nights? Potential social modulation of sleep efficiency. Psychol. Sci. 2002, 13, 384–387. [Google Scholar] [CrossRef]
- Peng, A.; Tang, Y.; He, S.; Ji, S.; Dong, B.; Chen, L. Association between loneliness, sleep behavior and quality: A propensity-score-matched case-control study. Sleep Med. 2021, 86, 19–24. [Google Scholar] [CrossRef] [PubMed]
- Matthews, T.; Danese, A.; Gregory, A.M.; Caspi, A.; Moffitt, T.E.; Arseneault, L. Sleeping with one eye open: Loneliness and sleep quality in young adults. Psychol. Med. 2017, 47, 2177–2186. [Google Scholar] [CrossRef] [PubMed]
- Eccles, A.M.; Qualter, P.; Madsen, K.R.; Holstein, B.E. Loneliness in the lives of Danish adolescents: Associations with health and sleep. Scand. J. Public Health 2020, 48, 877–887. [Google Scholar] [CrossRef] [PubMed]
- Markovic, A.; Bowker, J.C. Friends also matter: Examining friendship adjustment indices as moderators of anxious-withdrawal and trajectories of change in psychological maladjustment. Dev. Psychol. 2017, 53, 1462. [Google Scholar] [CrossRef] [PubMed]
- Azizi-Zeinalhajlou, A.; Mirghafourvand, M.; Nadrian, H.; Sis, S.S.; Matlabi, H. The contribution of social isolation and loneliness to sleep disturbances among older adults: A systematic review. Sleep Biol. Rhythm. 2022, 20, 153–163. [Google Scholar] [CrossRef]
- Richardson, C.; Oar, E.; Fardouly, J.; Magson, N.; Johnco, C.; Forbes, M.; Rapee, R. The moderating role of sleep in the relationship between social isolation and internalising problems in adolescence. Child Psychiatry Hum. Dev. 2019, 50, 1011–1020. [Google Scholar] [CrossRef]
- Pilcher, J.J.; Dorsey, L.L.; Galloway, S.M.; Erikson, D.N. Social isolation and sleep: Manifestation during COVID-19 quarantines. Front. Psychol. 2022, 12, 6476. [Google Scholar] [CrossRef]
- Cacioppo, J.T.; Hawkley, L.C. Social isolation and health, with an emphasis on underlying mechanisms. Perspect. Biol. Med. 2003, 46, S39–S52. [Google Scholar] [CrossRef]
- Palmer, C.A.; Powell, S.L.; Deutchman, D.R.; Tintzman, C.; Poppler, A.; Oosterhoff, B. Sleepy and secluded: Sleep disturbances are associated with connectedness in early adolescent social networks. J. Res. Adolesc. 2022, 32, 756–768. [Google Scholar] [CrossRef]
- Weissbluth, M. Sleep-loss stress and temperamental difficultness: Psychobiological processes and practical considerations. In Temperament in Childhood; Kohnstamm, G.A., Bates, J.E., Rothbart, M.K., Eds.; John Wiley & Sons: Hoboken, NJ, USA, 1989; pp. 357–375. [Google Scholar]
- Bowker, J.C.; White, H.I. Studying peers in research on social withdrawal: Why broader assessments of peers are needed. Child Dev. Perspect. 2021, 15, 90–95. [Google Scholar] [CrossRef]
- Bowker, J.C.; Ooi, L.L.; Coplan, R.J.; Etkin, R.G. When is it okay to be alone? Gender differences in normative beliefs about social withdrawal in emerging adulthood. Sex Roles 2020, 82, 482–492. [Google Scholar] [CrossRef]
- Rubin, K.H.; Wojslawowicz, J.C.; Rose-Krasnor, L.; Booth-LaForce, C.; Burgess, K.B. The best friendships of shy/withdrawn children: Prevalence, stability, and relationship quality. J. Abnorm. Child Psychol. 2006, 34, 139–153. [Google Scholar] [CrossRef] [PubMed]
- De Lise, F.; Bacaro, V.; Crocetti, E. The social side of sleep: A systematic review of the longitudinal associations between peer relationships and sleep quality. Int. J. Environ. Res. Public Health 2023, 20, 2017. [Google Scholar] [CrossRef] [PubMed]
- Tu, K.M.; Spencer, C.W.; El-Sheikh, M.; Erath, S.A. Peer victimization predicts sleep problems in early adolescence. J. Early Adolesc. 2019, 39, 67–80. [Google Scholar] [CrossRef]
- Van Geel, M.; Goemans, A.; Vedder, P.H. The relation between peer victimization and sleeping problems: A meta-analysis. Sleep Med. Rev. 2016, 27, 89–95. [Google Scholar] [CrossRef]
- LaFontana, K.M.; Cillessen, A.H. Developmental changes in the priority of perceived status in childhood and adolescence. Soc. Dev. 2010, 19, 130–147. [Google Scholar] [CrossRef]
- Cillessen, A.H.N. Sociometric methods. In Handbook of Peer Interactions, Relationships, and Groups; Rubin, K.H., Bukowski, W.M., Laursen, B., Eds.; The Guilford Press: New York, NY, USA, 2009; pp. 82–99. [Google Scholar]
- Achenbach, T.M. Manual for Child Behavior Checklist/4–18 and 1991 Profile; University of Vermont Department of Psychiatry: Burlington, VT, USA, 1991. [Google Scholar]
- Achenbach, T.M.; Rescorla, L.A. Manual for the ASEBA School-Age Forms & Profiles; University of Vermont, Research Center for Children, Youth, & Families: Burlington, VT, USA, 2001. [Google Scholar]
- Muthén, L.K.; Muthén, B.O. Mplus User’s Guide, 6th ed.; Muthén & Muthén: Los Angeles, CA, USA, 2010. [Google Scholar]
- Rosenberger, M.E.; Fulton, J.E.; Buman, M.P.; Troiano, R.P.; Grandner, M.A.; Buchner, D.M.; Haskell, W.L. The 24-hour activity cycle: A new paradigm for physical activity. Med. Sci. Sports Exerc. 2019, 51, 454. [Google Scholar] [CrossRef]
- McGowan, N.M.; Saunders, K.E. The emerging circadian phenotype of borderline personality disorder: Mechanisms, opportunities and future directions. Curr. Psychiatry Rep. 2021, 23, 30. [Google Scholar] [CrossRef]
- Kingsbury, M.; Coplan, R.J.; Rose-Krasnor, L. Shy but getting by? An examination of the complex links among shyness, coping, and socioemotional functioning in childhood. Soc. Dev. 2013, 22, 126–145. [Google Scholar] [CrossRef]
- Gazelle, H.; Rudolph, K.D. Moving toward and away from the world: Social approach and avoidance trajectories in anxious solitary youth. Child Dev. 2004, 75, 829–849. [Google Scholar] [CrossRef]
- Blake, M.J.; Sheeber, L.B.; Youssef, G.J.; Raniti, M.B.; Allen, N.B. Systematic review and meta-analysis of adolescent cognitive–behavioral sleep interventions. Clin. Child Fam. Psychol. Rev. 2017, 20, 227–249. [Google Scholar] [CrossRef]
- Hendricks, M.C.; Ward, C.M.; Grodin, L.K.; Slifer, K.J. Multicomponent cognitive-behavioural intervention to improve sleep in adolescents: A multiple baseline design. Behav. Cogn. Psychother. 2014, 42, 368–373. [Google Scholar] [CrossRef] [PubMed]
- Kodsi, A.; Bullock, B.; Kennedy, G.A.; Tirlea, L. Psychological interventions to improve sleep in young adults: A systematic review and meta-analysis of randomized controlled trials. Behav. Sleep Med. 2022, 20, 125–142. [Google Scholar] [CrossRef]
- Nguyen, V.V.; Zainal, N.H.; Newman, M.G. Why sleep is key: Poor sleep quality is a mechanism for the bidirectional relationship between major depressive disorder and generalized anxiety disorder across 18 years. J. Anxiety Disord. 2022, 90, 102601. [Google Scholar] [CrossRef] [PubMed]
- Song, Y.; Sznajder, K.; Cui, C.; Yang, Y.; Li, Y.; Yang, X. Anxiety and its relationship with sleep disturbance and problematic smartphone use among Chinese medical students during COVID-19 home confinement—A structural equation model analysis. J. Affect. Disord. 2022, 296, 315–321. [Google Scholar] [CrossRef]
- Chellappa, S.L.; Aeschbach, D. Sleep and anxiety: From mechanisms to interventions. Sleep Med. Rev. 2022, 61, 101583. [Google Scholar] [CrossRef]
- Kim, H.; Kim, S.H.; Jang, S.I.; Park, E.C. Association between sleep quality and anxiety in Korean adolescents. J. Prev. Med. Public Health 2022, 55, 173. [Google Scholar] [CrossRef]
- Chen, Y.; Zhu, J. Longitudinal associations between cybervictimization and adolescent sleep problems: The role of anxiety and depressive symptoms. J. Interpers. Violence 2023, 38, 2806–2827. [Google Scholar] [CrossRef] [PubMed]
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Anxious-withdrawal T1 | ||||||||||||||
| 2. Exclusion/Victimization T1 | 0.320 ** | |||||||||||||
| 3. Nightmares T1 | 0.122 * | 0.127 * | ||||||||||||
| 4. Overtired T1 | 0.101 | 0.071 | 0.119 * | |||||||||||
| 5. Sleeps less T1 | 0.039 | 0.037 | 0.112 * | 0.262 ** | ||||||||||
| 6. Sleeps more T1 | 0.175 ** | 0.055 | 0.134 ** | 0.104 * | 0.013 | |||||||||
| 7. Talks/walks T1 | −0.052 | −0.054 | 0.173 ** | 0.034 | −0.005 | 0.082 | ||||||||
| 8. Trouble sleeping T1 | 0.198 ** | 0.175 ** | 0.288 ** | 0.210 ** | 0.301 ** | 0.08 | 0.181 ** | |||||||
| 9. Nightmares T2 | 0.089 | 0.068 | 0.244 ** | 0.057 | −0.059 | 0.004 | 0.186 * | 0.053 | ||||||
| 10. Overtired T2 | 0.1 | 0.275 ** | 0.232 ** | 0.300 ** | 0.15 | 0.097 | 0.021 | 0.212 ** | 0.261 ** | |||||
| 11. Sleeps less T2 | 0.008 | 0.008 | 0.015 | 0.007 | 0.436 ** | 0.026 | −0.074 | 0.128 | 0.036 | 0.187 * | ||||
| 12. Sleeps more T2 | 0.194 * | 0.081 | 0.023 | −0.002 | 0.048 | 0.202 ** | 0.018 | 0.245 ** | 0.066 | 0.388 ** | 0.272 ** | |||
| 13. Talks/walks T2 | −0.145 | −0.115 | 0.011 | −0.006 | −0.055 | 0.008 | 0.433 ** | −0.028 | 0.297 ** | 0.054 | −0.142 | 0.071 | ||
| 14. Trouble sleeping T2 | 0.225 * | 0.247 ** | 0.178 * | 0.208 ** | 0.222 ** | 0.15 | 0.074 | 0.374 ** | 0.311 ** | 0.451 ** | 0.307 ** | 0.163 * | −0.019 | |
| M | −0.016 | −0.005 | 0.168 | 0.223 | 0.168 | 0.097 | 0.112 | 0.125 | 0.138 | 0.204 | 0.174 | 0.078 | 0.133 | 0.156 |
| SD | 0.837 | 0.605 | 0.381 | 0.463 | 0.425 | 0.344 | 0.34 | 0.394 | 0.379 | 0.446 | 0.439 | 0.29 | 0.374 | 0.38 |
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Anxious-withdrawal T1 | ||||||||||||
| 2. Exclusion/Victimization T1 | 0.320 ** | |||||||||||
| 3. Nightmares T1 | 0.122 * | 0.127 * | ||||||||||
| 4. Overtired T1 | 0.101 | 0.071 | 0.119 * | |||||||||
| 5. Sleeps less T1 | 0.039 | 0.037 | 0.112 * | 0.262 * | ||||||||
| 6. Sleeps more T1 | 0.175 ** | 0.055 | 0.134 ** | 0.104 * | 0.013 | |||||||
| 7. Trouble sleeping T1 | 0.198 ** | 0.175 ** | 0.288 ** | 0.210 ** | 0.301 ** | 0.08 | ||||||
| 8. Nightmares T2 | 0.019 | 0.166 | 0.167 * | 0.043 | 0.026 | −0.023 | −0.042 | |||||
| 9. Overtired T2 | 0.009 | 0.088 | −0.006 | 0.067 | 0.095 | 0.197 ** | 0.065 | 0.231 ** | ||||
| 10. Sleeps less T2 | −0.106 | −0.09 | −0.088 | 0.027 | 0.162 * | −0.047 | −0.007 | 0.092 | 0.206 ** | |||
| 11. Sleeps more T2 | −0.042 | 0.017 | −0.122 | −0.076 | −0.114 | 0.008 | −0.067 | −0.019 | 0.065 | −0.053 | ||
| 12. Trouble sleeping T2 | −0.08 | −0.084 | 0.022 | 0.038 | 0.211 ** | 0.089 | 0.116 | 0.171 * | 0.429 ** | 0.408 ** | −0.089 | |
| M | −0.016 | −0.005 | 0.168 | 0.223 | 0.168 | 0.097 | 0.125 | 0.477 | 0.465 | 0.465 | 0.269 | 0.374 |
| SD | 0.837 | 0.605 | 0.381 | 0.463 | 0.425 | 0.344 | 0.394 | 0.577 | 0.652 | 0.643 | 0.562 | 0.614 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bowker, J.C.; Gurbacki, J.N.; Richard, C.L.; Rubin, K.H. Anxious-Withdrawal and Sleep Problems during Adolescence: The Moderating Role of Peer Difficulties. Behav. Sci. 2023, 13, 740. https://doi.org/10.3390/bs13090740
Bowker JC, Gurbacki JN, Richard CL, Rubin KH. Anxious-Withdrawal and Sleep Problems during Adolescence: The Moderating Role of Peer Difficulties. Behavioral Sciences. 2023; 13(9):740. https://doi.org/10.3390/bs13090740
Chicago/Turabian StyleBowker, Julie C., Jessica N. Gurbacki, Chloe L. Richard, and Kenneth H. Rubin. 2023. "Anxious-Withdrawal and Sleep Problems during Adolescence: The Moderating Role of Peer Difficulties" Behavioral Sciences 13, no. 9: 740. https://doi.org/10.3390/bs13090740
APA StyleBowker, J. C., Gurbacki, J. N., Richard, C. L., & Rubin, K. H. (2023). Anxious-Withdrawal and Sleep Problems during Adolescence: The Moderating Role of Peer Difficulties. Behavioral Sciences, 13(9), 740. https://doi.org/10.3390/bs13090740





