The Measure of an Outcome: Comparing Norming and Stacking to Benchmark the Effectiveness of Brain Injury Rehabilitation Services
Abstract
:1. Introduction
2. Materials and Methods
2.1. Ethical Considerations
2.2. Study Design
2.3. Participants
2.4. Setting
2.5. Measures
2.6. Data Analysis
3. Results
3.1. Patient Characteristics
3.2. Rehabilitation Outcomes
3.2.1. Stacking by Time
3.2.2. Stacking by Clinical Stream
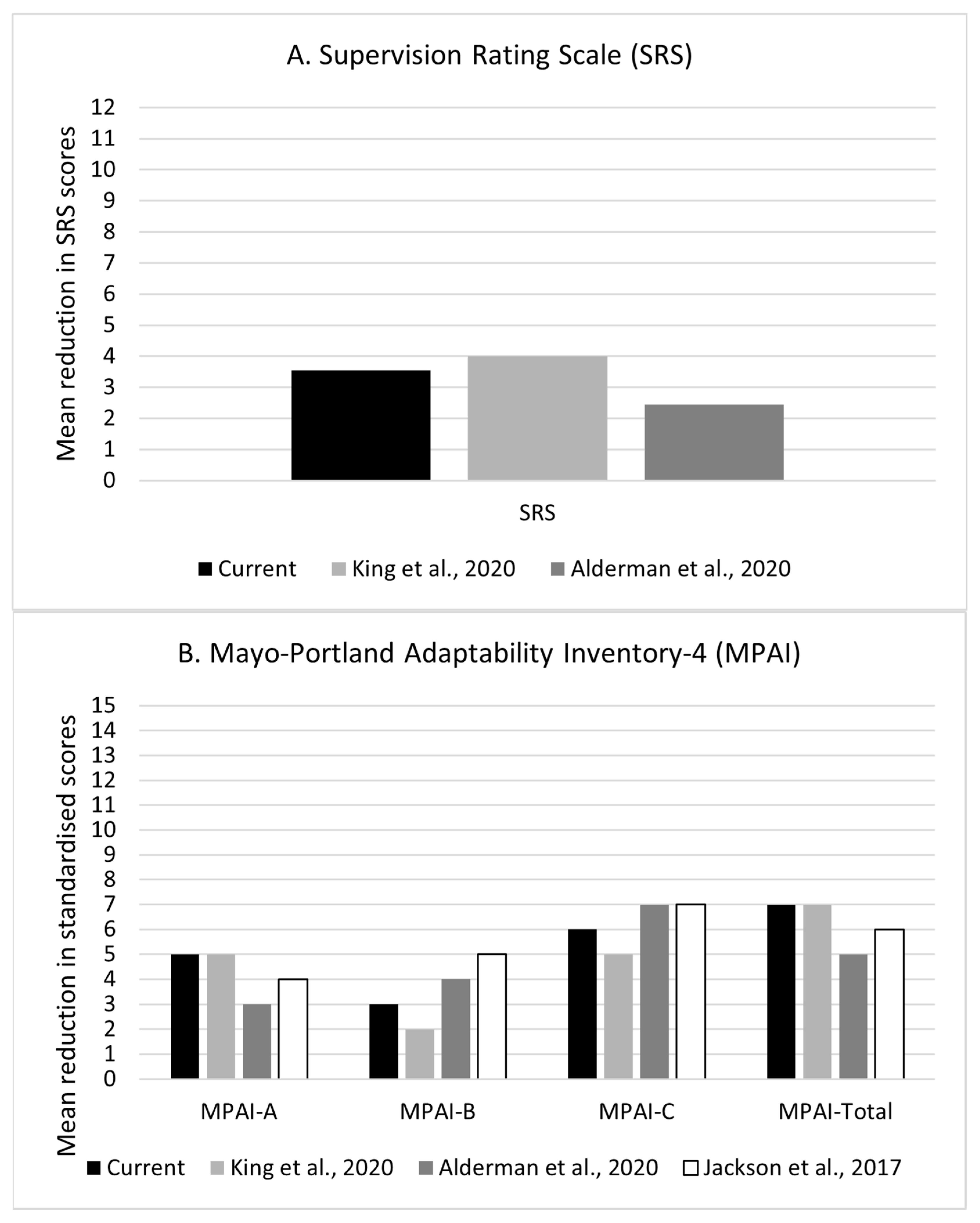
3.2.3. Norming
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Evans, R.W. Postacute neurorehabilitation: Roles and responsibilities within a national information system. Arch. Phys. Med. Rehabil. 1997, 78, S17–S25. [Google Scholar] [CrossRef] [PubMed]
- Mccarthy, M. Purchasing neurorehabilitation in the UK National Health Service. Neuropsychol. Rehabil. 1999, 9, 295–303. [Google Scholar] [CrossRef]
- McMillan, T.M. Outcome of rehabilitation for neurobehavioural disorders. NeuroRehabilitation 2013, 32, 791–801. [Google Scholar] [CrossRef]
- Willmington, C.; Belardi, P.; Murante, A.M.; Vainieri, M. The contribution of benchmarking to quality improvement in healthcare. A systematic literature review. BMC Health Serv. Res. 2022, 22, 139. [Google Scholar] [CrossRef] [PubMed]
- Covington, N.V.; Duff, M.C. Heterogeneity Is a Hallmark of Traumatic Brain Injury, Not a Limitation: A New Perspective on Study Design in Rehabilitation Research. Am. J. Speech Lang. Pathol. 2021, 30, 974–985. [Google Scholar] [CrossRef] [PubMed]
- Vázquez-Guimaraens, M.; Caamaño-Ponte, J.L.; Seoane-Pillado, T.; Cudeiro, J. Factors related to greater functional recovery after suffering a stroke. Brain Sci. 2021, 11, 802. [Google Scholar] [CrossRef]
- Salvadori, E.; Papi, G.; Insalata, G.; Rinnoci, V.; Donnini, I.; Martini, M.; Falsini, C.; Hakiki, B.; Romoli, A.; Barbato, C.; et al. Comparison between ischemic and hemorrhagic strokes in functional outcome at discharge from an intensive rehabilitation hospital. Diagnostics 2020, 11, 38. [Google Scholar] [CrossRef]
- Dickens, G.; Sugarman, P. Key performance indicators and HoNOS. Br. J. Healthcare Manag. 2010, 16, 431–435. [Google Scholar] [CrossRef]
- Alderman, N.; Pink, A.E.; Williams, C.; da Silva Ramos, S.; Oddy, M.; Knight, C.; Jenkins, K.G.; Barnes, M.P.; Hayward, C. Optimizing measurement for neurobehavioural rehabilitation services: A multisite comparison study and response to UKROC. Neuropsychol. Rehabil. 2020, 30, 1318–1347. [Google Scholar] [CrossRef]
- Altan, D.; Ahuja, V.; Kelleher, C.M.; Chang, D.C. Look in the mirror, not out the window. Ann. Surg. Open 2022, 3, e184. [Google Scholar] [CrossRef]
- Shvyrkov, V.V.; Davis, A.C. The homogeneity problem in statistics. Qual. Quant. 1987, 21, 21–36. [Google Scholar] [CrossRef]
- Wilczek, F. Einstein’s Parable of Quantum Insanity. Quanta Magazine. 2015. Available online: https://www.scientificamerican.com/article/einstein-s-parable-of-quantum-insanity/ (accessed on 18 August 2023).
- Dixon, N. Guide to Managing Ethical Issues in Quality Improvement or Clinical Audit Projects; Healthcare Quality Improvement Partnership, Ltd., (HQIP): London, UK, 2021. [Google Scholar]
- Health Research Authority. UK Policy Framework for Health and Social Care Research; Health Research Authority: London, UK, 2020. [Google Scholar]
- Data Protection Act. 2018. c. 12. Available online: https://www.legislation.gov.uk/ukpga/2018/12/contents/enacted (accessed on 18 August 2023).
- Coetzer, R.; Ramos, S.S. A neurobehavioral therapy approach to the rehabilitation and support of persons with brain injury: Practice-based evidence from a UK charitable rehabilitation provider. Front. Rehab. Sci. 2022, 3, 902702. [Google Scholar] [CrossRef] [PubMed]
- National Institute for Health and Care Excellence (NICE). Stroke Rehabilitation in Adults: Clinical Guideline [CG162]. 2013. Available online: https://www.nice.org.uk/guidance/cg162/chapter/Update-information (accessed on 18 August 2023).
- Boake, C. Supervision rating scale: A measure of functional outcome from brain injury. Arch. Phys. Med. Rehabil. 1996, 77, 765–772. [Google Scholar] [CrossRef] [PubMed]
- Malec, J.; Lezak, M. MPAI-4 Manual. 2003. Available online: http://www.tbims.org/combi/mpai/manual.pdf (accessed on 18 August 2023).
- Lowe, J.R.; Wallace, S.J.; Sam, S.; Young, A. Minimum data and core outcomes for subacute rehabilitation: A scoping review. Clin. Rehabil. 2022, 36, 388–406. [Google Scholar] [CrossRef]
- van Heugten, C.; Caldenhove, S.; Crutsen, J.; Winkens, I. An overview of outcome measures used in neuropsychological rehabilitation research on adults with acquired brain injury. Neuropsychol. Rehabil. 2020, 30, 1598–1623. [Google Scholar] [CrossRef]
- Honan, C.A.; McDonald, S.; Tate, R.; Ownsworth, T.; Togher, L.; Fleming, J.; Anderson, V.; Morgan, A.; Catroppa, C.; Douglas, J.; et al. Outcome instruments in moderate-to-severe adult traumatic brain injury: Recommendations for use in psychosocial research. Neuropsychol. Rehabil. 2019, 29, 896–916. [Google Scholar] [CrossRef]
- Benge, J.F.; Caroselli, J.S.; Reed, K.; Zgaljardic, D.J. Changes in supervision needs following participation in a residential post-acute brain injury rehabilitation programme. Brain Inj. 2010, 24, 844–850. [Google Scholar] [CrossRef]
- High, W.M.; Roebuck-Spencer, T.; Sander, A.M.; Struchen, M.A.; Sherer, M. Early Versus Later Admission to Postacute Rehabilitation: Impact on Functional Outcome After Traumatic Brain Injury. Arch. Phys. Med. Rehabil. 2006, 87, 334–342. [Google Scholar] [CrossRef]
- King, R.; Seeger, T.; Wang, M.; Li Pi Shan, R.; McGovern, C.; Knox, J.; Patel, L.; Fung, T.; Sajobi, T.; Debert, C. Early Supported Discharge for Neurorehabilitation Following Acquired Brain Injury. Front. Neurol. 2020, 11, 596526. [Google Scholar] [CrossRef]
- Jackson, D.; Seaman, K.; Sharp, K.; Singer, R.; Wagland, J.; Turner-Stokes, L. Staged residential post-acute rehabilitation for adults following acquired brain injury: A comparison of functional gains rated on the UK Functional Assessment Measure (UK FIM+FAM) and the Mayo-Portland Adaptability Inventory (MPAI-4). Brain Inj. 2017, 31, 1405–1413. [Google Scholar] [CrossRef]
- Banks, R.; Bush, A.; Baker, P.; Bradshaw, J.; Carpenter, P.; Deb, S.; Joyce, T.; Mansell, J.; Xenitidis, K. Challenging Behaviour: A Unified Approach; Royal College of Psychiatrists, British Psychological Society and Royal College of Speech and Language Therapists: London, UK, 2007; pp. 1–79. [Google Scholar]
- MedCalc Software. MedCalc for Windows, Version 16.8. Available online: https://www.medcalc.org/calc/index.php (accessed on 18 August 2023).
- Worthington, A.; Melia, Y.; Oddy, M.; Matthews, S. Cost benefits associated with social outcome from neurobehavioural rehabilitation. Brain Inj. 2006, 20, 947–957. [Google Scholar] [CrossRef] [PubMed]
- Oddy, M.; Ramos, S.D.S. The clinical and cost-benefits of investing in neurobehavioural rehabilitation: A multi-centre study. Brain Inj. 2013, 27, 1500–1507. [Google Scholar] [CrossRef] [PubMed]
- Wood, R.L.; McCrea, J.D.; Wood, L.M.; Merriman, R.N. Clinical and cost effectiveness of post-acute neurobehavioural rehabilitation. Brain Inj. 1999, 13, 69–88. [Google Scholar] [CrossRef]
- Giles, G.M. Assessing adaptive behaviour in the post-acute setting following traumatic brain injury: Initial reliability and validity of the Adaptive Behaviour and Community Competency Scale (ABCCS). Brain Inj. 2007, 21, 521–529. [Google Scholar] [CrossRef] [PubMed]
| Current | Last | Historical | |
|---|---|---|---|
| Characteristic | (N = 166) | (N = 214) | (N = 770) |
| Age (M, SD) | 57 (18) | 57 (16) | 48 (15) ‡ |
| Sex | |||
| Male | 102 (61%) | 139 (65%) | 556 (72%) |
| Female | 65 (39%) | 75(35%) | 214 (28%) ‡ |
| Diagnosis | |||
| TBI | 58 (35%) | 72 (34%) | 318 (42%) |
| Stroke | 76 (46%) | 102 (48%) | 251 (33%) ‡ |
| Other | 32 (19%) | 38 (18%) | 192 (25%) |
| Months since injury | |||
| m (IQR) | 2 (1–5) | 1 (1–5) | 4 (2–10) ‡ |
| Comorbidities | |||
| Schizophrenia | 4 (3%) | 6 (4%) | 10 (3%) |
| Drug misuse | 8 (7%) | 13 (9%) | 50 (16%) ‡ |
| Alcohol misuse | 19 (16%) | 37 (25%) | 124 (38%) ‡ |
| Multiple trauma | 7 (8%) | 13 (11%) | 73 (24%) ‡ |
| Other medical conditions | 48 (59%) | 67 (64%) | 137 (50%) |
| Current | Last | Historical | ||||
|---|---|---|---|---|---|---|
| Characteristic | (N = 137) | (N = 167) | (N = 647) | |||
| Weeks in service | ||||||
| m (IQR) | 16 (11–34) | 16 (10–39) | 24 (13–49) | |||
| A | D | A | D | A | D | |
| Supervision Rating Scale | ||||||
| N | 94 | 94 | 135 | 135 | 448 | 448 |
| m (IQR) | 9 (8–11) | 6 (2–8) | 9 (8–11) | 5 (1–8) | 9 (8–11) | 6 (2–8) |
| MPAI-4 Ability | ||||||
| N | 82 | 82 | 141 | 141 | 383 | 383 |
| M (SD) | 53 (11) | 48 (11) | 52 (8) | 46 (11) | 52 (9) | 47 (9) |
| % above MCI threshold | - | 52% | - | 61% | - | 59% |
| MPAI-4 Adjustment | ||||||
| N | 83 | 83 | 147 | 147 | 420 | 420 |
| M (SD) | 54 (10) | 51 (10) | 52(9) | 48 (12) | 53 (8) | 48 (9) |
| % above MCI threshold | - | 47% | - | 54% | - | 59% |
| MPAI-4 Participation | ||||||
| N | 83 | 83 | 144 | 144 | 433 | 433 |
| M (SD) | 59(13) | 52 (13) | 57(11) | 51 (11) | 57 (10) | 49 (10) |
| % above MCI threshold | - | 55% | - | 56% | - | 68% † |
| MPAI-4 Total | ||||||
| N | 79 | 79 | 138 | 138 | 348 | 348 |
| M (SD) | 61 (14) | 55 (15) | 58 (10) | 51 (13) | 58 (10) | 51 (11) |
| % above MCI threshold | - | 53% † | - | 66% | - | 68% |
| Restoration | Compensation | Support | ||||
|---|---|---|---|---|---|---|
| Characteristic | (N = 434) | (N = 356) | (N = 145) | |||
| Weeks in service | ||||||
| m (IQR) | 12 (8–21) | 21 (12–40) ‡ | 31 (16–57) ‡ | |||
| A | D | A | D | A | D | |
| Supervision Rating Scale | ||||||
| N | 359 | 359 | 284 | 284 | 110 | 110 |
| m (IQR) | 8 (6–11) | 5 (1–7) | 9 (7–11) | 5 (2–8) | 10 (8–11) | 8 (7–10) |
| MPAI-4 Ability | ||||||
| N | 350 | 350 | 275 | 275 | 104 | 104 |
| Mean (SD) | 51 (9) | 45 (10) | 50 (8) | 44 (10) | 52 (10) | 53 (8) |
| % above MCI threshold | - | 64% | - | 59% | - | 55% |
| MPAI-4 Adjustment | ||||||
| N | 359 | 359 | 281 | 281 | 106 | 106 |
| M (SD) | 51 (9) | 45 (11) | 54 (8) | 49 (10) | 57 (9) | 53 (10) |
| % above MCI threshold | - | 56% | - | 55% | - | 53% |
| MPAI-4 Participation | ||||||
| N | 360 | 360 | 279 | 279 | 111 | 111 |
| M (SD) | 54(10) | 47 (11) | 56(10) | 50 (10) | 65 (10) | 58 (11) |
| % above MCI threshold | - | 63% | - | 61% | - | 61% |
| MPAI-4 Total | ||||||
| N | 334 | 334 | 264 | 264 | 96 | 96 |
| M (SD) | 56 (11) | 47 (12) | 57 (10) | 50 (12) | 67 (12) | 59 (13) |
| % above MCI threshold | - | 69% † | - | 64% | - | 59% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ramos, S.D.S.; Coetzer, R. The Measure of an Outcome: Comparing Norming and Stacking to Benchmark the Effectiveness of Brain Injury Rehabilitation Services. Behav. Sci. 2023, 13, 705. https://doi.org/10.3390/bs13090705
Ramos SDS, Coetzer R. The Measure of an Outcome: Comparing Norming and Stacking to Benchmark the Effectiveness of Brain Injury Rehabilitation Services. Behavioral Sciences. 2023; 13(9):705. https://doi.org/10.3390/bs13090705
Chicago/Turabian StyleRamos, Sara D. S., and Rudi Coetzer. 2023. "The Measure of an Outcome: Comparing Norming and Stacking to Benchmark the Effectiveness of Brain Injury Rehabilitation Services" Behavioral Sciences 13, no. 9: 705. https://doi.org/10.3390/bs13090705
APA StyleRamos, S. D. S., & Coetzer, R. (2023). The Measure of an Outcome: Comparing Norming and Stacking to Benchmark the Effectiveness of Brain Injury Rehabilitation Services. Behavioral Sciences, 13(9), 705. https://doi.org/10.3390/bs13090705




