Schizophrenia: A Review of Social Risk Factors That Affect Women
Abstract
1. Introduction
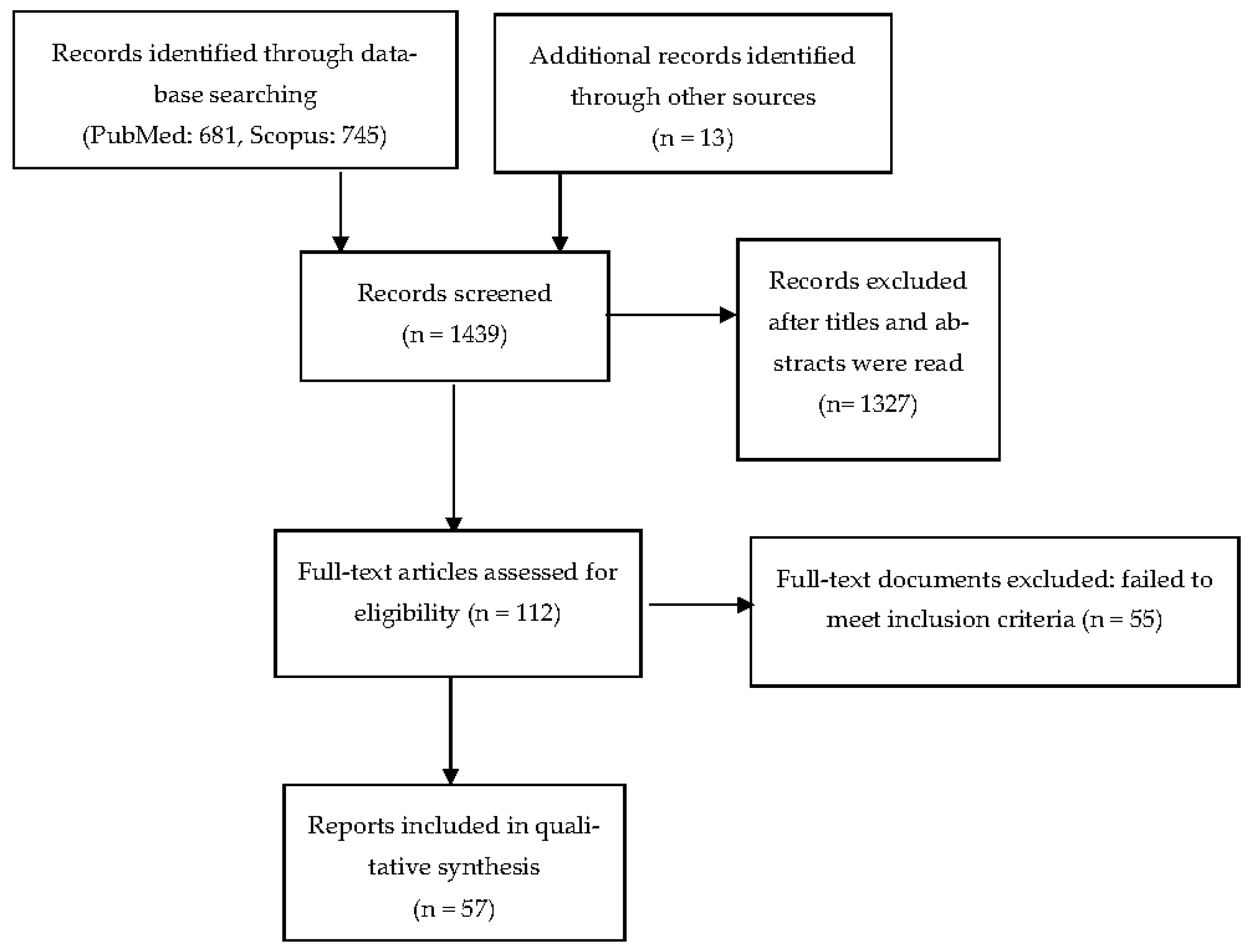
2. Materials and Methods
2.1. Search Strategy
2.2. Inclusion and Exclusion Criteria
2.3. Data Collection and Extraction
3. Results
3.1. The Role of Social Capital and Social Defeat in Schizophrenia
3.2. The Role of Employment/Unemployment
3.3. The Role of Socioeconomic Status
3.4. The Role of Housing and Homelessness
3.5. The Role of Social Networks
3.6. The Role of Stigma and Discrimination
3.7. The Role of Emigration, Immigration, and Acculturation
3.8. The Role of Urbanicity
| Social Risk Factors | Influence on Mental Health | Male/Female Influence on Schizophrenia | Study Design | Refs |
|---|---|---|---|---|
| Social capital and social defeat | Membership in a cohesive group positively influences mental health | Men react with defeat to loss of status; woman are more likely to react to relationship loss | Prospective quality study | [13] |
| Employment/unemployment | Employment improves objective quality of life and mental health | Women cope better with unemployment than men, and jobs for women may be easier to find | Nationwide population registry, cross-sectional (qualitative and quantitative) | [20,21,22,23,24,25,26] |
| Socioeconomic status | Low income correlates with low quality of life and health | Higher parental SES correlates with decreased symptom severity in women, but not always in men | Cross-sectional (part of larger projects) | [31,32] |
| Housing | Homelessness and neighborhood disadvantage correlates with vulnerability to violence, marginalization, and exploitation | Homelessness in women correlates with sexual victimization. Women’s and men’s housing needs differ | Multi-center studies, cross-sectional | [39,40,41] |
| Social network | Individuals with SMI are frequently single, living alone, and unemployed | Schizophrenia is associated with small social networks, more so in men than in women | Population survey (self-report), cross-sectional | [42,43,44,45,46] |
| Discrimination | Perceived “otherness” and discrimination lead to isolation and social marginalization | Reasons for discrimination differ in women and men with schizophrenia | Cross-sectional | [23,49,50] |
| Immigration | Processes of emigration, immigration, and acculturation are major stressors | New immigration is especially difficult for men | Register study | [51,52] |
| Urbanicity | The higher the degree of urbanicity, the higher the risk for schizophrenia | Urbanicity and socioeconomic disadvantage are risks for men and women | National survey study, population-based study | [53,54,55] |
3.9. The Role of Abuse/Trauma
3.9.1. Prevalence and Incidence of Childhood Adversities in Women with Schizophrenia
3.9.2. Association of Adult Trauma and Psychopathological Symptoms in Women with Schizophrenia
3.10. The Role of Intimate Partner Violence
| Social Risk Factors | Relevant Findings | Study Design | Reference |
|---|---|---|---|
| Adverse childhood experiences | Adverse events in childhood are associated with later suicidal behavior and auditory hallucinations. | Cross-sectional | [56] |
| Association with hallucinatory symptoms are more commonly found in women than in men with schizophrenia. | Cross-sectional (part of a genomic psychiatry cohort study) | [60] | |
| Childhood physical and emotional abuse are most commonly reported by women with schizophrenia. | Cross-sectional | [57,59] | |
| Sexual trauma in adulthood | Positive association was found between sexual harassment and hallucinations and affective lability. | Cross-sectional | [62] |
| Women are prone to suffer re-victimization. | Prospective, longitudinal | [63] | |
| Intimate partner violence | Sexual assault and verbal and physical abuse are associated with a higher severity of psychotic symptoms. | Cross-sectional | [65] |
| Verbal abuse is the most frequent type of intimate partner violence. | Cross-sectional | [66] | |
| Nearly half of pregnant women with schizophrenia experience intimate partner violence. | Population-based cohort study | [68] |
4. How Do Social Factors Act Biologically and What Works to Prevent or Reduce This Effect?
5. Discussion
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Jeste, D.V.; Malaspina, D.; Bagot, K.; Cole, S.; Dickerson, F.; Dilmore, A.; Ford, C.L.; Karcher, N.R.; Luby, J.; Rajoo, T.; et al. Review of major social determinants of health in schizophrenia-spectrum psychotic disorders: III. Biology. Schizophr. Bull. 2023, 49, 867–880. [Google Scholar] [CrossRef] [PubMed]
- Jester, D.J.; Thomas, M.L.; Sturm, E.T.; Harvey, P.D.; Keshavan, M.; Davis, B.J.; Saxena, S.; Tampi, R.; Leutwyler, H.; Compton, M.T.; et al. Review of major social determinants of health in schizophrenia-spectrum psychotic disorders: I. Clinical outcomes. Schizophr. Bull. 2023, 49, 837–850. [Google Scholar] [CrossRef] [PubMed]
- Malaspina, D. What social determinants can tell us about schizophrenia. Schizophr. Res. 2023, 256, 114–116. [Google Scholar] [CrossRef] [PubMed]
- Sturm, E.T.; Thomas, M.L.; Sares, A.G.; Dave, S.; Baron, D.; Compton, M.T.; Palmer, M.T.; Jester, D.J.; Jeste, D.V. Review of major social determinants of health in schizophrenia-spectrum disorders: II. Assessments. Schizophr. Bull. 2023, 49, 851–866. [Google Scholar] [CrossRef] [PubMed]
- Huggard, L.; Murphy, R.; O’Connor, C.; Nearchou, F. The social determinants of mental illness: A rapid review of systematic reviews. Issues Ment. Health Nurs. 2023, 44, 302–312. [Google Scholar] [CrossRef] [PubMed]
- Gnanapragasam, S.; Astill Wright, L.; Pemberton, M.; Bhugra, D. Outside/inside: Social determinants of mental health. Ir. J. Psychol. Med. 2021, 40, 63–73. [Google Scholar] [CrossRef]
- Lund, C.; Brooke-Sumner, C.; Baingana, F.; Baron, E.C.; Breuer, E.; Chandra, P.; Haushofer, J.; Herrman, H.; Jordans, M.; Kieling, C.; et al. Social determinants of mental disorders and the Sustainable Development Goals: A systematic review of reviews. Lancet Psychiatry 2018, 5, 357–369. [Google Scholar] [CrossRef]
- Mao, W.; Agyapong, V.I.O. The role of social determinants in mental health and resilience after disasters: Implications for public health policy and practice. Front. Public Health 2021, 9, 658528. [Google Scholar] [CrossRef]
- Boyce, W.T.; Sokolowski, M.B.; Robinson, G.E. Toward a new biology of social adversity. Proc. Natl. Acad. Sci. USA 2012, 109 (Suppl. S2), 17143–17148. [Google Scholar] [CrossRef]
- Landecker, H.; Panofsky, A. From social structure to gene regulation, and back: A critical introduction to environmental epigenetics for sociology. Annu. Rev. Sociol. 2013, 39, 333–357. [Google Scholar] [CrossRef]
- Meaney, M.J. Epigenetics and the biological definition of gene x environment interactions. Child. Dev. 2010, 81, 41–79. [Google Scholar] [CrossRef] [PubMed]
- De Silva, M.J.; McKenzie, K.; Harpham, T.; Huttly, S.R. Social capital and mental illness: A systematic review. J. Epidemiol. Commun. Health 2005, 59, 619–627. [Google Scholar] [CrossRef] [PubMed]
- Eliacin, J. Social capital, narratives of fragmentation, and schizophrenia: An ethnographic exploration of factors shaping African-Caribbeans’ social capital and mental health in a north London community. Cult. Med. Psychiatry 2013, 37, 465–487. [Google Scholar] [CrossRef]
- Selten, J.P.; van der Ven, E.; Rutten, B.P.; Cantor-Graae, E. The social defeat hypothesis of schizophrenia: An update. Schizophr. Bull. 2013, 39, 1180–1186. [Google Scholar] [CrossRef] [PubMed]
- Haslam, C.; Cruwys, T.; Haslam, S.A.; Jetten, J. Social Connectedness and Health. In Encyclopedia of Geropsychology; Pachana, N., Ed.; Springer: Singapore, 2015. [Google Scholar] [CrossRef]
- Luo, P.X.; Manning, C.E.; Fass, J.N.; Williams, A.V.; Hao, R.; Campi, K.L.; Trainor, B.C. Sex-specific effects of social defeat stress on miRNA expression in the anterior BNST. Behav. Brain. Res. 2021, 401, 113084. [Google Scholar] [CrossRef] [PubMed]
- Bjorkqvist, K. Social defeat as a stressor in humans. Physiol. Behav. 2001, 73, 435–442. [Google Scholar] [CrossRef]
- Luhrmann, T.M. Social defeat and the culture of chronicity: Or, why schizophrenia does so well over there and so badly here. Cult. Med. Psychiatry 2017, 31, 135–172. [Google Scholar] [CrossRef]
- Erim, B.R.; Boztas, H.; Yıldız, M.; Uygun, E. The factors affecting the relationship between remission status and employment in chronic schizophrenia patients. Psychiatry. Investig. 2019, 16, 860–867. [Google Scholar] [CrossRef]
- Holm, M.; Taipale, H.; Tanskanen, A.; Tiihonen, J.; Mitterdorfer-Rutz, E. Employment among people with schizophrenia or bipolar disorder: A population-based study using nationwide registers. Acta Psychiatry Scand. 2021, 143, 61–71. [Google Scholar] [CrossRef]
- Khalid, A.; Syed, J. A relational perspective of schizophrenia at work. Equality Diversity Inclusion. Equal. Divers. Incl. 2023, 42, 321–345. [Google Scholar] [CrossRef]
- Ponting, C.; Delgadillo, D.; Rivera-Olmedo, N.; Yarris, K.E. A qualitative analysis of gendered experiences of schizophrenia in an outpatient psychiatric hospital in Mexico. Int. Perspect. Psychol. Res. Pract. Consult. 2020, 9, 159–175. [Google Scholar] [CrossRef]
- Loganathan, S.; Murthy, S. Living with schizophrenia in India: Gender perspectives. Transcult. Psychiatry 2011, 48, 569–584. [Google Scholar] [CrossRef]
- Marcotte, D.E.; Wilcox-Gök, V. Estimating the employment and earnings costs of mental illness: Recent developments in the United States. Soc. Sci. Med. 2001, 53, 21–27. [Google Scholar] [CrossRef]
- Mubarak, A.R. Employment status, psychiatric disability and quality of life: Comparison of men and women with schizophrenia in Malaysia. Int. J. Soc. Welf. 2006, 15, 240–246. [Google Scholar] [CrossRef]
- Goodsmith, N.; Cohen, A.N.; Pedersen, E.R.; Evans, E.; Young, A.; Hamilton, A.B. Predictors of functioning and recovery among men and women veterans with schizophrenia. Commun. Ment. Health J. 2023, 59, 110–121. [Google Scholar] [CrossRef]
- Ravindran, T.K. Universal access: Making health systems work for women. BMC Public Health 2012, 12 (Suppl. S1), S4. [Google Scholar] [CrossRef] [PubMed]
- Prokosch, C.; Fertig, A.R.; Ojebuoboh, A.R.; Trofholz, A.C.; Baird, M.; Young, M.; de Brito, J.N.; Kunin-Batson, A.; Berge, J.M. Exploring associations between social determinants of health and mental health outcomes in families from socioeconomically and racially and ethnically diverse households. Prev. Med. 2022, 161, 107150. [Google Scholar] [CrossRef] [PubMed]
- Jeste, D.V.; Pender, V.B. Social Determinants of mental health: Recommendations for research, training, practice, and policy. JAMA. Psychiatry 2022, 79, 283–284. [Google Scholar] [CrossRef] [PubMed]
- Vijayalakshmi, P.; Ramachandra; Reddemma, K.; Math, S.B. Impact of socio-economic status in meeting the needs of people with mental illness; human rights perspective. Commun. Ment. Health J. 2014, 50, 245–250. [Google Scholar] [CrossRef]
- Parrott, B.; Lewine, R. Socioeconomic status of origin and the clinical expression of schizophrenia. Schizophr. Res. 2005, 75, 417–424. [Google Scholar] [CrossRef]
- Lewine, R.; Shriner, B. Work expectations, cultural sensitivity, schizophrenia, and suicide risk in male patients. J. Nerv. Ment. Dis. 2009, 197, 239–243. [Google Scholar] [CrossRef]
- Shah, N.; Walker, I.F.; Naik, Y.; Rajan, S.; O’Hagan, K.; Black, M.; Cartwright, C.; Tillmann, T.; Pearce-Smith, N.; Stansfield, J. National or population level interventions addressing the social determinants of mental health—An umbrella review. BMC Public Health 2021, 21, 2118. [Google Scholar] [CrossRef]
- Seeman, M.V. Sex differences in schizophrenia relevant to clinical care. Expert. Rev. Neurother. 2021, 21, 443–453. [Google Scholar] [CrossRef] [PubMed]
- McEwen, C.A.; McEwen, B.S. Social structure, adversity, toxic stress, and intergenerational poverty: An early childhood model. Annu. Rev. Sociol. 2017, 43, 445–472. [Google Scholar] [CrossRef]
- Carmona-Derqui, D.; Torres-Tellez, J.; Montero-Soler, A. Effects of housing deprivation on health: Empirical evidence from Spain. Int. J. Environ. Res. Public Health 2023, 20, 2405. [Google Scholar] [CrossRef]
- Singh, A.; Daniel, L.; Baker, E.; Bentley, R. Housing disadvantage and poor mental health: A systematic review. Am. J. Prev. Med. 2019, 57, 262–272. [Google Scholar] [CrossRef]
- Bentley, R.; Baker, E.; Mason, K. Cumulative exposure to poor housing affordability and its association with mental health in men and women. J. Epidem. Ment. Health 2012, 66, 761–766. [Google Scholar] [CrossRef] [PubMed]
- Tinland, A.; Zemmour, K.; Auquier, P.; Boucekine, M.; Girard, V.; Loubière, S.; Fond, G.; Boyer, L.; French Housing First Study Group. Homeless women with schizophrenia reported lower adherence to their medication than men: Results from the French Housing First experience. Soc. Psychiatry Psychiatry Epidemiol. 2017, 52, 1113–1122. [Google Scholar] [CrossRef]
- Tinland, A.; Boyer, L.; Loubière, S.; Greacen, T.; Girard, V.; Boucekine, M.; Fond, G.; Auquier, P. Victimization and posttraumatic stress disorder in homeless women with mental illness are associated with depression, suicide, and quality of life. NeuroPsychiatry Dis. Treat. 2018, 14, 2269–2279. [Google Scholar] [CrossRef]
- Opler, L.A.; White, L.; Caton, C.L.; Dominguez, B.; Hirshfield, S.; Shrout, P.E. Gender differences in the relationship of homelessness to symptom severity, substance abuse, and neuroleptic noncompliance in schizophrenia. J. Nerv. Ment. Dis. 2001, 189, 449–456. [Google Scholar] [CrossRef]
- Galletly, C.; Suetani, S.; Hahn, L.; McKellar, D.; Castle, D. Ageing with psychosis—Fifty and beyond. Aust. N. Z. J. Psychiatry 2022, 56, 39–49. [Google Scholar] [CrossRef] [PubMed]
- Lee, M.H.; Seo, M.K. Community integration of persons with mental disorders compared with the general population. Int. J. Environ. Res. Public Health 2020, 17, 1596. [Google Scholar] [CrossRef] [PubMed]
- Harfush, S.E.E.; El-Nabi Moussa, A.A.; Mabrook Elnehrawy, S. Association between community integration and mental health recovery among patients with psychiatric disorders. Tanta. Sci. Nurs. J. 2022, 24, 11–34. [Google Scholar]
- Yanos, P.T.; Stefanic, A.; Tsemberis, S. Psychological community integration among people with psychiatric disabilities and nondisabled community members. J. Commun. Psychol. 2011, 39, 390–401. [Google Scholar] [CrossRef]
- Yanos, P.T.; Stefancic, A.; Tsemberis, S. Objective community integration of mental health consumers living in supported housing and of others in the community. Psychiatry Serv. 2012, 63, 438–444. [Google Scholar] [CrossRef]
- Amsalem, D.; Jankowski, S.E.; Pagdon, S.; Valeri, L.; Smith, S.; Yang, L.H.; Markowitz, J.C.; Lewis-Fernández, R.; Dixon, L.B. “It is hard to be a woman with schizophrenia”: Randomized controlled trial of a brief video intervention to reduce public stigma in young adults. J. Clin. Psychiatry 2022, 84, 22m14534. [Google Scholar] [CrossRef]
- González-Rodríguez, A.; Guàrdia, A.; Álvarez Pedrero, A.; Betriu, M.; Cobo, J.; Acebillo, S.; Monreal, J.A.; Seeman, M.V.; Palao, D.; Labad, J. Women with schizophrenia over the life span: Health promotion, treatment and outcomes. Int. J. Environ. Res. Public Health 2020, 17, 5594. [Google Scholar] [CrossRef]
- Farrelly, S.; Clement, S.; Gabbidon, J.; Jeffery, D.; Dockery, L.; Lassman, F.; Brohan, E.; Henderson, R.C.; Williams, P.; Howard, L.M.; et al. Anticipated and experienced discrimination amongst people with schizophrenia, bipolar disorder and major depressive disorder: A cross sectional study. BMC Psychiatry 2014, 14, 157. [Google Scholar] [CrossRef]
- West, M.L.; Yanos, P.T.; Smith, S.M.; Roe, D.; Lysaker, P.H. Prevalence of internalized stigma among persons with severe mental illness. Stigma Res. Action. 2011, 1, 3–10. [Google Scholar] [CrossRef]
- Iversen, V.C.; Morken, G. Acute admissions among immigrants and asylum seekers to a psychiatric hospital in Norway. Soc. Psychiatry Psychiatry Epidemiol. 2003, 38, 515–519. [Google Scholar] [CrossRef]
- Pence, A.Y.; Pries, L.-K.; Ferrara, M.; Rutten, B.P.F.; van Os, J.; Guloksuz, S. Gender differences in the association between environment and psychosis. Schizophr. Res. 2022, 243, 120–137. [Google Scholar] [CrossRef] [PubMed]
- Luo, Y.; Pang, L.; Guo, C.; Zhang, L.; Zheng, X. Association of urbanicity with schizophrenia and related mortality in China. Can. J. Psychiatry 2021, 66, 385–394. [Google Scholar] [CrossRef] [PubMed]
- Yang, L.H.; Phillips, M.R.; Li, X.; Yu, G.; Zhang, J.; Shi, Q.; Song, Z.; Ding, Z.; Pang, S.; Susser, E. Marriage outcome and relationship with urban versus rural context for individuals with psychosis in a population-based study in China. Soc. Psychiatry Psychiatry Epidemiol. 2015, 50, 1501–1509. [Google Scholar] [CrossRef]
- Pillay, A.L.; Sargent, C. Descriptive profile of sex and psychiatric diagnosis among rural and peri-urban clinic attenders in South Africa. Psychol. Rep. 2003, 92, 595–598. [Google Scholar] [CrossRef] [PubMed]
- Prokopez, C.R.; Vallejos, M.; Farinola, R.; Alberio, G.; Caporusso, G.B.; Cozzarin, L.G.; Chiapella, L.C.; Fuentes, P.; Daray, F.M. The history of multiple adverse childhood experiences in patients with schizophrenia is associated with more severe symptomatology and suicidal behavior with gender-specific characteristics. Psychiatry Res. 2020, 293, 113411. [Google Scholar] [CrossRef] [PubMed]
- Jangam, K.; Muralidharan, K.; Tansa, K.A.; Raj, E.A.; Bhowmick, P. Incidence of childhood abuse among women with psychiatric disorders compared with healthy women: Data from a tertiary care centre in India. Child. Abuse. Negl. 2015, 50, 67–75. [Google Scholar] [CrossRef]
- Braehler, C.; Valiquette, L.; Holowka, D.; Malla, A.K.; Joober, R.; Ciampi, A.; Pawliuk, N.; King, S. Childhood trauma and dissociation in first-episode psychosis, chronic schizophrenia and community controls. Psychiatry Res. 2013, 210, 36–42. [Google Scholar] [CrossRef]
- Kelly, D.L.; Rowland, L.M.; Patchan, K.M.; Sullivan, K.; Earl, A.; Raley, H.; Liu, F.; Feldman, S.; McMahon, R.P. Schizophrenia clinical symptom differences in women vs. men with and without a history of childhood physical abuse. Child. Adolesc. Psychiatry Ment. Health 2016, 10, 5. [Google Scholar] [CrossRef]
- Levit, J.; Valderrama, J.; Georgakopoulos, P.; Hansen, S.K.; Salisu, M.; Fanous, A.; Bigdeli, T.; Knowles, J.; Pato, C.; Pato, M.; et al. Childhood trauma and psychotic symptomatology in ethnic minorities with schizophrenia. Schizophr. Bull. Open 2021, 2, sgaa068. [Google Scholar] [CrossRef]
- Gayer-Anderson, C.; Reininghaus, U.; Paetzold, I.; Hubbard, K.; Beards, S.; Mondelli, V.; Di Forti, A.; Murray, R.M.; Pariante, C.M.; Dazzan, P.; et al. A comparison between self-report and interviewer-rated retrospective reports of childhood abuse among individuals with first-episode psychosis and population-based controls. J. Psychiatry Res. 2020, 123, 145–150. [Google Scholar] [CrossRef]
- Yildirim, M.H.; Yildirim, E.A.; Kaser, M.; Guduk, M.; Fistikci, N.; Cinar, O.; Yuksel, S. The relationship between adulthood traumatic experiences and psychotic symptoms in female patients with schizophrenia. Compr. Psychiatry 2014, 55, 1847–1854. [Google Scholar] [CrossRef]
- Aakre, J.M.; Brown, C.H.; Benson, K.M.; Drapalski, A.L.; Gearon, J.S. Trauma exposure and PTSD in women with schizophrenia and coexisting substance use disorders: Comparisons to women with severe depression and substance use disorders. Psychiatry Res. 2014, 220, 840–845. [Google Scholar] [CrossRef]
- Gearon, J.S.; Kaltman, S.I.; Brown, C.; Bellack, A.S. Traumatic life events and PTSD among women with substance use disorders and schizophrenia. Psychiatry Serv. 2003, 54, 523–528. [Google Scholar] [CrossRef]
- Afe, T.O.; Emedoh, T.C.; Ogunsemi, O.O.; Adegohun, A.A. Socio-demographic characteristics, partner characteristics, socioeconomic variables, and intimate partner violence in women with schizophrenia in south-South Nigeria. J. Health Care. Poor Underserved 2017, 28, 707–720. [Google Scholar] [CrossRef] [PubMed]
- Afe, T.O.; Emedoh, T.C.; Ogunsemi, O.; Adegbohun, A.A. Intimate partner violence, psychopathology and the women with schizophrenia in an outpatient clinic South-South, Nigeria. BMC Psychiatry 2016, 16, 197. [Google Scholar] [CrossRef] [PubMed]
- Suparare, L.; Watson, S.J.; Binns, R.; Frayne, J.; Galbally, M. Is intimate partner violence more common in pregnant women with severe mental illness? A retrospective study. Int. J. Soc. Psychiatry 2020, 66, 225–231. [Google Scholar] [CrossRef] [PubMed]
- Leslie, K.; Barker, L.C.; Brown, H.K.; Chen, S.; Dennis, C.L.; Ray, J.G.; Saunders, N.; Taylor, C.; Vigod, S. Risk of interpersonal violence during and after pregnancy among people with schizophrenia: A population-based cohort study. CMAJ 2023, 195, E322–E329. [Google Scholar] [CrossRef] [PubMed]
- Lim, C.; Chong, S.-A.; Keefe, R.S.E. Psychosocial factors in the neurobiology of schizophrenia: A selective review. Ann. Acad. Med. Singap. 2009, 38, 402–407. [Google Scholar] [CrossRef] [PubMed]
- Almuqrin, A.; Georgiades, A.; Mouhitzadeh, K.; Rubinic, P.; Mechelli, A.; Tognin, S. The association between psychosocial stress, interpersonal sensitivity, social withdrawal and psychosis relapse: A systematic review. Schizophrenia 2023, 9, 22. [Google Scholar] [CrossRef]
- McCutcheon, R.A.; Keefe, R.S.E.; McGuire, P.K. Cognitive impairment in schizophrenia: Aetiology, pathophysiology, and treatment. Mol. Psychiatry 2023. [Google Scholar] [CrossRef]
- Tomassi, S.; Tosato, S. Epigenetics and gene expression profile in first-episode psychosis: The role of childhood trauma. Neurosci. Biobehav. Rev. 2017, 83, 226–237. [Google Scholar] [CrossRef] [PubMed]
- Solmi, M.; Croatto, G.; Piva, G.; Rosson, S.; Fusar-Poli, P.; Rubio, J.M.; Carvalho, A.F.; Vieta, E.; Arango, C.; DeTore, N.R.; et al. Efficacy and acceptability of psychosocial interventions in schizophrenia: Systematic overview and quality appraisal of the meta-analytic evidence. Mol. Psychiatry 2023, 28, 354–368. [Google Scholar] [CrossRef] [PubMed]
- Rincón-Cortés, M.; Herman, J.P.; Lupien, S.; Maguire, J.; Shansky, R.M. Stress: Influence of sex, reproductive status and gender. Neurobiol. Stress 2019, 10, 100155. [Google Scholar] [CrossRef] [PubMed]
- Handa, R.J.; Sheng, J.A.; Castellanos, E.A.; Templeton, H.N.; McGivern, R.F. Sex differences in acute neuroendocrine responses to stressors in rodents and humans. Cold Spring Harb. Perspect. Biol. 2022, 14, a039081. [Google Scholar] [CrossRef]
- Watson, J.; Fossey, E.; Harvey, C. A home but how to connect with others? A qualitative meta-synthesis of experiences of people with mental illness living in supported housing. Health Soc. Care. Community 2019, 27, 546–564. [Google Scholar] [CrossRef]
- Harries, C.I.; Smith, D.M.; Gregg, L.; Wittkowski, A. Parenting and serious mental illness (SMI): A systematic review and metasynthesis. Clin. Child Fam. Psychol. Rev. 2023, 26, 303–342. [Google Scholar] [CrossRef]
- Sanders, M.R.; Kirby, J.N.; Tellegen, C.L.; Day, J.J. The Triple P-Positive Parenting Program: A systematic review and meta-analysis of a multi-level system of parenting support. Clin. Psychol. Rev. 2014, 34, 337–357. [Google Scholar] [CrossRef]
- Coates, D.; Phelan, R.; Heap, J.; Howe, D. Being in a group with others who have mental illness makes all the difference: The views and experiences of parents who attended a mental health parenting program. Child. Youth. Serv. Rev. 2017, 78, 104–111. [Google Scholar] [CrossRef]
- Kaplan, K.; Solomon, P.; Salzer, M.S.; Brusilovskiy, E. Assessing an Internet-based parenting intervention for mothers with a serious mental illness: A randomized controlled trial. Psychiatry Rehabil. J. 2014, 37, 222–231. [Google Scholar] [CrossRef]
- Schrank, B.; Moran, K.; Borgh, C.; Priebe, S. How to support patients with severe mental illness in their parenting role with children aged over 1 year? A systematic review of interventions. Soc. Psychiatry Psychiatry Epidemiol. 2015, 50, 1765–1783. [Google Scholar] [CrossRef]
- Campbell, L.; Poon, A.W.C. Parenting Challenges for Persons with a Serious Mental Illness. In Mental Health and Social Work; Ow, R., Poon, A.W.C., Eds.; Springer Nature: Singapore, 2020; Chapter 22. [Google Scholar] [CrossRef]
- van der Stouwe, E.C.D.; Steenhuis, L.A.; Pijnenborg, G.H.M.; de Vries, B.; Pharmacotherapy and outcome survey (PHAMOUS)-investigators; Bartels-Velthuis, A.A.; Castelein, S.; Veling, W.; Visser, E.; van Busschbach, J.T. Gender differences in characteristics of violent and sexual victimization in patients with psychosis: A cross-sectional study. BMC Psychiatry 2021, 21, 541. [Google Scholar] [CrossRef] [PubMed]
- Hodgins, S. Could expanding and investing in first-episode psychosis services prevent aggressive behaviour and violent crime? Front. Psychiatry 2022, 13, 821760. [Google Scholar] [CrossRef] [PubMed]
- Balon, R. Complexity of reducing the stigma of mental illness. Acad. Psychiatry 2023, 47, 95–97. [Google Scholar] [CrossRef]
- Dobson, K.S.; Stuart, H. (Eds.) The Stigma of Mental Illness: Models and Methods of Stigma Reduction; Oxford University Press: New York, NY, USA, 2021; p. 260. ISBN 9780197572597. [Google Scholar]
- Sideli, L.; Murray, R.M.; Schimmenti, A.; Corso, M.; La Barbera, D.; Trotta, A.; Fisher, H.L. Childhood adversity and psychosis: A systematic review of bio-psycho-social mediators and moderators. Psychol. Med. 2020, 50, 1761–1782. [Google Scholar] [CrossRef]
- Latimer, E.A.; Rabouin, D.; Cao, Z.; Ly, A.; Powell, G.; Aubry, T.; Distasio, J.; Hwang, S.W.; Somers, J.M.; Bayoumi, A.M.; et al. Cost-effectiveness of housing first with assertive community treatment: Results from the Canadian at Home/Chez Soi Trial. Psychiatry Serv. 2020, 71, 1020–1030. [Google Scholar] [CrossRef]
- Latkin, C.A.; Knowlton, A.R. Social network assessments and interventions for health behavior change: A critical review. Behav. Med. 2015, 41, 90–97. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
González-Rodríguez, A.; Natividad, M.; Seeman, M.V.; Paolini, J.P.; Balagué, A.; Román, E.; Izquierdo, E.; Pérez, A.; Vallet, A.; Salvador, M.; et al. Schizophrenia: A Review of Social Risk Factors That Affect Women. Behav. Sci. 2023, 13, 581. https://doi.org/10.3390/bs13070581
González-Rodríguez A, Natividad M, Seeman MV, Paolini JP, Balagué A, Román E, Izquierdo E, Pérez A, Vallet A, Salvador M, et al. Schizophrenia: A Review of Social Risk Factors That Affect Women. Behavioral Sciences. 2023; 13(7):581. https://doi.org/10.3390/bs13070581
Chicago/Turabian StyleGonzález-Rodríguez, Alexandre, Mentxu Natividad, Mary V. Seeman, Jennipher Paola Paolini, Ariadna Balagué, Eloïsa Román, Eduard Izquierdo, Anabel Pérez, Anna Vallet, Mireia Salvador, and et al. 2023. "Schizophrenia: A Review of Social Risk Factors That Affect Women" Behavioral Sciences 13, no. 7: 581. https://doi.org/10.3390/bs13070581
APA StyleGonzález-Rodríguez, A., Natividad, M., Seeman, M. V., Paolini, J. P., Balagué, A., Román, E., Izquierdo, E., Pérez, A., Vallet, A., Salvador, M., & Monreal, J. A. (2023). Schizophrenia: A Review of Social Risk Factors That Affect Women. Behavioral Sciences, 13(7), 581. https://doi.org/10.3390/bs13070581








