Preoperative Biopsychosocial Assessment and Length of Stay in Orthopaedic Surgery Admissions of Youth with Cerebral Palsy
Abstract
1. Introduction
Background
2. Materials and Methods
2.1. Biopsychosocial Assessment
2.2. Statistical Analysis
3. Results
3.1. Group Analysis
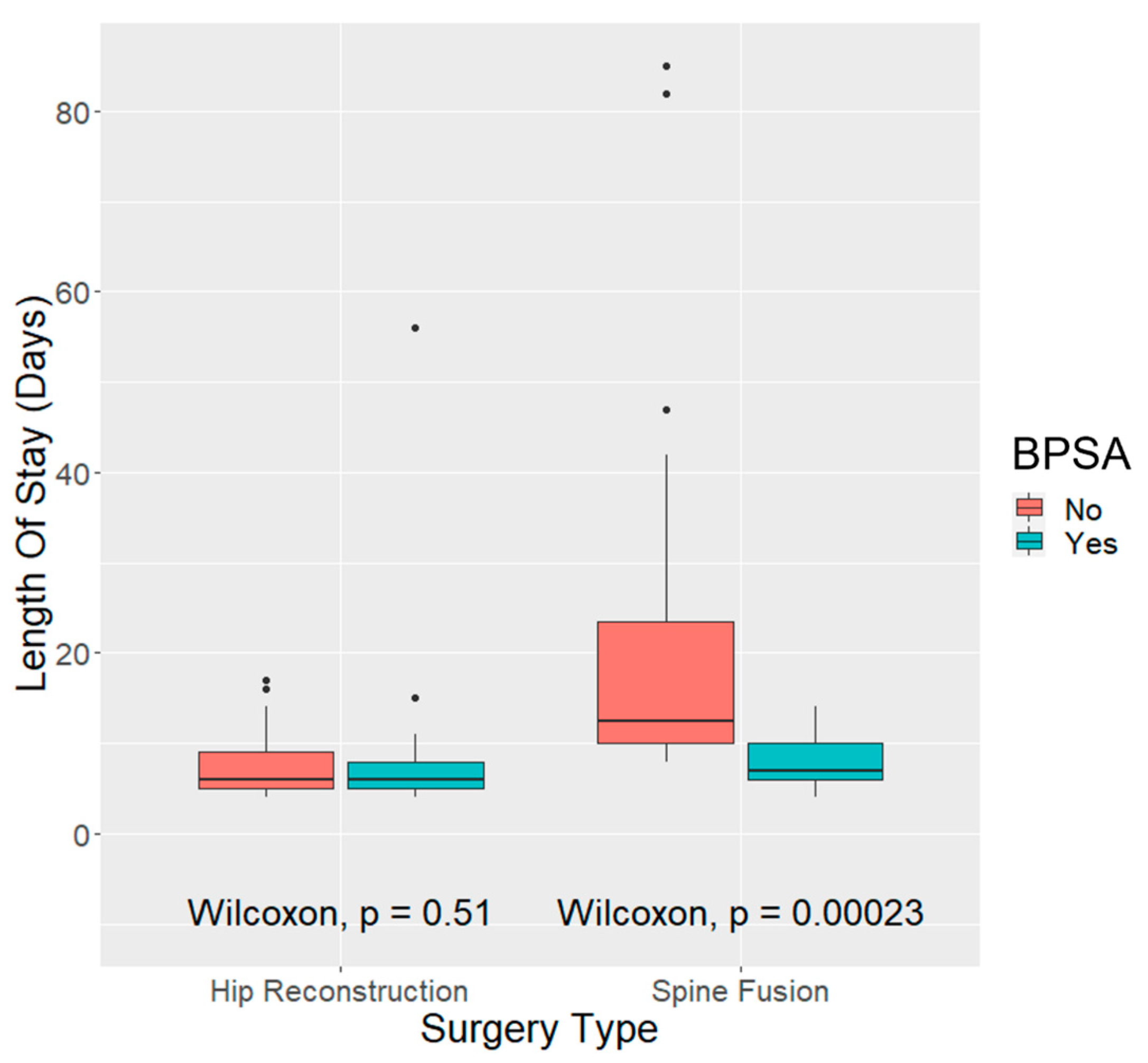
3.1.1. Length of Stay
3.1.2. Extended Length of Stay
3.1.3. Thirty-Day Readmission
3.2. Multivariate Analyses
3.2.1. Length of Stay
3.2.2. Extended Length of Stay
3.2.3. Thirty-Day Readmission
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Centers for Disease Control and Prevention. Cerebral Palsy. Available online: http://www.cdc.gov/ncbddd/dd/ddcp.htm (accessed on 30 November 2021).
- Graham, H.K.; Rosenbaum, P.; Paneth, N.; Dan, B.; Lin, J.P.; Damiano, D.L.; Becher, J.G.; Gaebler-Spira, D.; Colver, A.; Reddihough, D.S.; et al. Cerebral palsy. Nat. Rev. Dis. Primers 2016, 2, 15082. [Google Scholar] [CrossRef]
- Palisano, R.; Rosenbaum, P.; Walter, S.; Russell, D.; Wood, E.; Galuppi, B. Development and reliability of a system to classify gross motor function in children with cerebral palsy. Dev. Med. Child Neurol. 1997, 39, 214–223. [Google Scholar] [CrossRef] [PubMed]
- Wimalasundera, N.; Stevenson, V.L. Cerebral palsy. Pract. Neurol. 2016, 16, 184–194. [Google Scholar] [CrossRef] [PubMed]
- Davis, E.; Shelly, A.; Waters, E.; Boyd, R.; Cook, K.; Davern, M.; Reddihough, D. The impact of caring for a child with cerebral palsy: Quality of life for mothers and fathers. Child Care Health Dev. 2010, 36, 63–73. [Google Scholar] [CrossRef]
- Brehaut, J.C.; Kohen, D.E.; Raina, P.; Walter, S.D.; Russell, D.J.; Swinton, M.; O’Donnell, M.; Rosenbaum, P. The health of primary caregivers of children with cerebral palsy: How does it compare with that of other Canadian caregivers? Pediatrics 2004, 114, e182–e191. [Google Scholar] [CrossRef]
- Guillamón, N.; Nieto, R.; Pousada, M.; Redolar, D.; Muñoz, E.; Hernández, E.; Boixadós, M.; Gómez-Zúñiga, B. Quality of life and mental health among parents of children with cerebral palsy: The influence of self-efficacy and coping strategies. J. Clin. Nurs. 2013, 22, 1579–1590. [Google Scholar] [CrossRef]
- Parkes, J.; Caravale, B.; Marcelli, M.; Franco, F.; Colver, A. Parenting stress and children with cerebral palsy: A European cross-sectional survey. Dev. Med. Child Neurol. 2011, 53, 815–821. [Google Scholar] [CrossRef]
- Svedberg, L.E.; Englund, E.; Malker, H.; Stener-Victorin, E. Comparison of impact on mood, health, and daily living experiences of primary caregivers of walking and non-walking children with cerebral palsy and provided community services support. Eur. J. Paediatr. Neurol. 2010, 14, 239–246. [Google Scholar] [CrossRef]
- Britner, P.A.; Morog, M.C.; Pianta, R.C.; Marvin, R.S. Stress and coping: A comparison of self-report measures of functioning in families of young children with cerebral palsy or no medical diagnosis. J. Child Fam. Stud. 2003, 12, 335–348. [Google Scholar] [CrossRef]
- Lee, M.H.; Matthews, A.K.; Park, P. Determinants of health-related quality of life among mothers of children with cerebral palsy. J. Pediatr. Nurs. 2019, 44, 1–8. [Google Scholar] [CrossRef]
- Tseng, M.H.; Chen, K.L.; Shieh, J.Y.; Lu, L.; Huang, C.Y.; Simeonsson, R.J. Child characteristics, caregiver characteristics, and environmental factors affecting the quality of life of caregivers of children with cerebral palsy. Disabil. Rehabil. 2016, 38, 2374–2382. [Google Scholar] [CrossRef] [PubMed]
- Healthy People 2030. U.S. Department of Health and Human Services. Office of Disease Prevention and Health Promotion. Social Determinants of Health. Available online: https://health.gov/healthypeople/priority-areas/social-determinants-health (accessed on 12 December 2022).
- Pruszczynski, B.; Sees, J.; Miller, F. Risk factors for hip displacement in children with cerebral palsy: Systematic review. J. Pediatr. Orthop. 2016, 36, 829–833. [Google Scholar] [CrossRef] [PubMed]
- McGinley, J.L.; Dobson, F.; Ganeshalingam, R.; Shore, B.J.; Rutz, E.; Graham, H.K. Single-event multilevel surgery for children with cerebral palsy: A systematic review. Dev. Med. Child Neurol. 2012, 54, 117–128. [Google Scholar] [CrossRef] [PubMed]
- Miller, D.J.; Flynn, J.J.M.; Pasha, S.; Yaszay, B.; Parent, S.; Asghar, J.; Abel, M.F.; Pahys, J.M.; Samdani, A.; Hwang, S.W.; et al. Improving health-related quality of life for patients with nonambulatory cerebral palsy: Who stands to gain from scoliosis surgery? J. Pediatr. Orthop. 2020, 40, e186–e192. [Google Scholar] [CrossRef] [PubMed]
- Hosseinzadeh, P.; Baldwin, K.; Minaie, A.; Miller, F. Management of hip disorders in patients with cerebral palsy. JBJS Rev. 2020, 8, e0148. [Google Scholar] [CrossRef] [PubMed]
- Koop, S.E. Scoliosis in cerebral palsy. Dev. Med. Child Neurol. 2009, 51 (Suppl. S4), 92–98. [Google Scholar] [CrossRef]
- Iversen, A.S.; Graue, M.; Clare, J. Parents’ perspectives of surgery for a child who has cerebral palsy. J. Pediatr. Health Care 2009, 23, 165–172. [Google Scholar] [CrossRef]
- Park, M.S.; Chung, C.Y.; Lee, K.M.; Sung, K.H.; Choi, I.H.; Kim, T.W. Parenting stress in parents of children with cerebral palsy and its association with physical function. J. Pediatr. Orthop. B 2012, 21, 452–456. [Google Scholar] [CrossRef]
- Vessey, J.A.; DiFazio, R.L.; Strout, T.D.; Snyder, B.D. Impact of non-medical out-of-pocket expenses on families of children with cerebral palsy following orthopaedic surgery. J. Pediatr. Nurs. 2017, 37, 101–107. [Google Scholar] [CrossRef]
- Shanske, S.; Arnold, J.; Carvalho, M.; Rein, J. Social workers as transition brokers: Facilitating the transition from pediatric to adult medical care. Soc. Work Health Care 2012, 51, 279–295. [Google Scholar] [CrossRef]
- Jain, A.; Sponseller, P.D.; Shah, S.A.; Samdani, A.; Cahill, P.J.; Yaszay, B.; Njoku, D.B.; Abel, M.F.; Newton, P.O.; Marks, M.C.; et al. Subclassification of GMFCS level-5 cerebral palsy as a predictor of complications and health-related quality of life after spinal arthrodesis. J. Bone Jt. Surg. Am. 2016, 98, 1821–1828. [Google Scholar] [CrossRef] [PubMed]
- National Association of Social Workers (NASW). NASW Standards for Social Work Practice in Health Care Settings. Washington, DC: NASW. Available online: https://www.socialworkers.org/LinkClick.aspx?fileticket=fFnsRHX-4HE%3d&portalid=0 (accessed on 19 December 2022).
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2021; Available online: https://www.R-project.org/ (accessed on 19 December 2022).
| Variable | BPSA | p Value | Test | ||
|---|---|---|---|---|---|
| No | Yes | ||||
| Age | Median (CI) | 10.6 (0.94) | 10.9 (0.97) | 0.72 | Wilcoxon |
| Race | Asian | 1 | 0 | 0.68 | Chi-squared |
| Asian Indian | 1 | 0 | |||
| Black or African American | 13 | 13 | |||
| Guamanian or Chamorro | 0 | 1 | |||
| Some other race | 3 | 4 | |||
| White or Caucasian | 28 | 28 | |||
| GMFCS | IV | 16 | 17 | 0.83 | Chi-squared |
| V | 30 | 29 | |||
| Surgery type | Hip | 28 | 28 | 1 | Chi-squared |
| Spine | 18 | 18 | |||
| Range of medical issues | None = 0 | 6 | 8 | 0.84 | Chi-squared |
| Small = 1.2 | 24 | 23 | |||
| Large = 3.4 | 16 | 15 | |||
| Surgery Type | BPSA | Comorbidities | n | LOS Days | 30-Day Readmission | ||
|---|---|---|---|---|---|---|---|
| Median | IQR | CI | |||||
| Hip | No | None | 4 | 5.5 | 1.75 | 2.72 | 0 |
| Hip | No | Small | 16 | 6.5 | 4 | 1.76 | 2 |
| Hip | No | Large | 8 | 6.5 | 7.75 | 4.07 | 2 |
| Spine | No | None | 2 | 11 | 3 | 38.1 | 1 |
| Spine | No | Small | 8 | 11 | 2.5 | 21.2 | 0 |
| Spine | No | Large | 8 | 21 | 31 | 21.8 | 0 |
| Hip | Yes | None | 6 | 6 | 1.5 | 21.6 | 0 |
| Hip | Yes | Small | 16 | 5.5 | 2.25 | 1.06 | 1 |
| Hip | Yes | Large | 6 | 8 | 1.5 | 3.8 | 0 |
| Spine | Yes | None | 2 | 9 | 1 | 12.7 | 0 |
| Spine | Yes | Small | 7 | 10 | 5 | 3.16 | 1 |
| Spine | Yes | Large | 9 | 7 | 1 | 1.96 | 2 |
| Subject Number | Surgery | Reason for 30-Day Readmission |
|---|---|---|
| 1 | HR | Oropharyngeal dysphagia, diabetes insipidus |
| 2 | HR | Postoperative pain management |
| 3 | HR | Vomiting, constipation |
| 4 | HR | Decubitus ulcer |
| 5 | PSF | Urinary retention |
| 6 | HR | Wound infection |
| 7 | PSF | Urinary tract infection |
| 8 | PSF | Wound infection |
| 9 | PSF | Wound infection |
| Length of Stay Models Fit | ||||
|---|---|---|---|---|
| PSF | ||||
| χ2 (5) | 186.96 | |||
| p | 0.00 | |||
| Pseudo-R2 (McFadden) | 0.29 | |||
| Standard errors: MLE | ||||
| Est. | S.E. | z val. | p | |
| (Intercept) | 0.17 | 0.64 | 0.27 | 0.78 |
| BPSA (yes) | −1.08 | 0.10 | 11.16 | <0.001 |
| additional comorbidities (small) | 0.37 | 0.17 | 2.16 | 0.03 |
| additional comorbidities (large) | 0.63 | 0.19 | 3.27 | <0.001 |
| Age | 0.05 | 0.02 | 1.90 | 0.06 |
| GMFCS | 0.41 | 0.12 | 3.48 | 0.005 |
| Hip Reconstruction | ||||
| χ2 (3) | 22.56 | |||
| p | 0.00 | |||
| Pseudo-R2 (McFadden) | 0.06 | |||
| Standard errors: MLE | ||||
| Est. | S.E. | z val. | p | |
| (Intercept) | 2.23 | 0.12 | 19.24 | 0.00 |
| Additional comorbidities (small) | −0.46 | 0.12 | −3.89 | <0.001 |
| Additional comorbidities (large) | −0.13 | 0.13 | −1.03 | 0.30 |
| Sex (male) | 0.23 | 0.1 | 2.34 | 0.019 |
| Extended Length of Stay Models Fit | ||||
|---|---|---|---|---|
| PSF | ||||
| χ2 (1) | 9.77 | |||
| p | 0.00 | |||
| Pseudo-R2 (McFadden) | 0.20 | |||
| Standard errors: MLE | ||||
| Est. | S.E. | z val. | p | |
| (Intercept) | 0.69 | 0.5 | 1.39 | 0.17 |
| BPSA (Yes) | −2.3 | 0.81 | −2.86 | 0.004 |
| Hip Reconstruction | ||||
| χ2 (3) | 11.66 | |||
| p | 0.01 | |||
| Pseudo-R2 (McFadden) | 0.22 | |||
| Standard errors: MLE | ||||
| Est. | S.E. | z val. | p | |
| (Intercept) | −13.99 | 6.07 | −2.31 | 0.02 |
| BPSA (yes) | −2.16 | 1.01 | −2.13 | 0.03 |
| Sex (male) | 1.96 | 1.02 | 1.92 | 0.05 |
| GMFCS | 2.56 | 1.22 | 2.09 | 0.04 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lennon, N.; Sewell-Roberts, C.; Banjo, T.; Kraft, D.B.; Salazar-Torres, J.J.; Church, C.; Shrader, M.W. Preoperative Biopsychosocial Assessment and Length of Stay in Orthopaedic Surgery Admissions of Youth with Cerebral Palsy. Behav. Sci. 2023, 13, 383. https://doi.org/10.3390/bs13050383
Lennon N, Sewell-Roberts C, Banjo T, Kraft DB, Salazar-Torres JJ, Church C, Shrader MW. Preoperative Biopsychosocial Assessment and Length of Stay in Orthopaedic Surgery Admissions of Youth with Cerebral Palsy. Behavioral Sciences. 2023; 13(5):383. https://doi.org/10.3390/bs13050383
Chicago/Turabian StyleLennon, Nancy, Carrie Sewell-Roberts, Tolulope Banjo, Denver B. Kraft, Jose J. Salazar-Torres, Chris Church, and M. Wade Shrader. 2023. "Preoperative Biopsychosocial Assessment and Length of Stay in Orthopaedic Surgery Admissions of Youth with Cerebral Palsy" Behavioral Sciences 13, no. 5: 383. https://doi.org/10.3390/bs13050383
APA StyleLennon, N., Sewell-Roberts, C., Banjo, T., Kraft, D. B., Salazar-Torres, J. J., Church, C., & Shrader, M. W. (2023). Preoperative Biopsychosocial Assessment and Length of Stay in Orthopaedic Surgery Admissions of Youth with Cerebral Palsy. Behavioral Sciences, 13(5), 383. https://doi.org/10.3390/bs13050383







