Patient Power and Empowerment: Mitigating Elements of Valuable Patient Participation in Healthcare Collaboratives
Abstract
1. Introduction
2. Literature Review
2.1. Stakeholder Involvement in Healthcare Systems
2.2. Collaboration and Value Co-Creation
2.3. Power and Empowerment
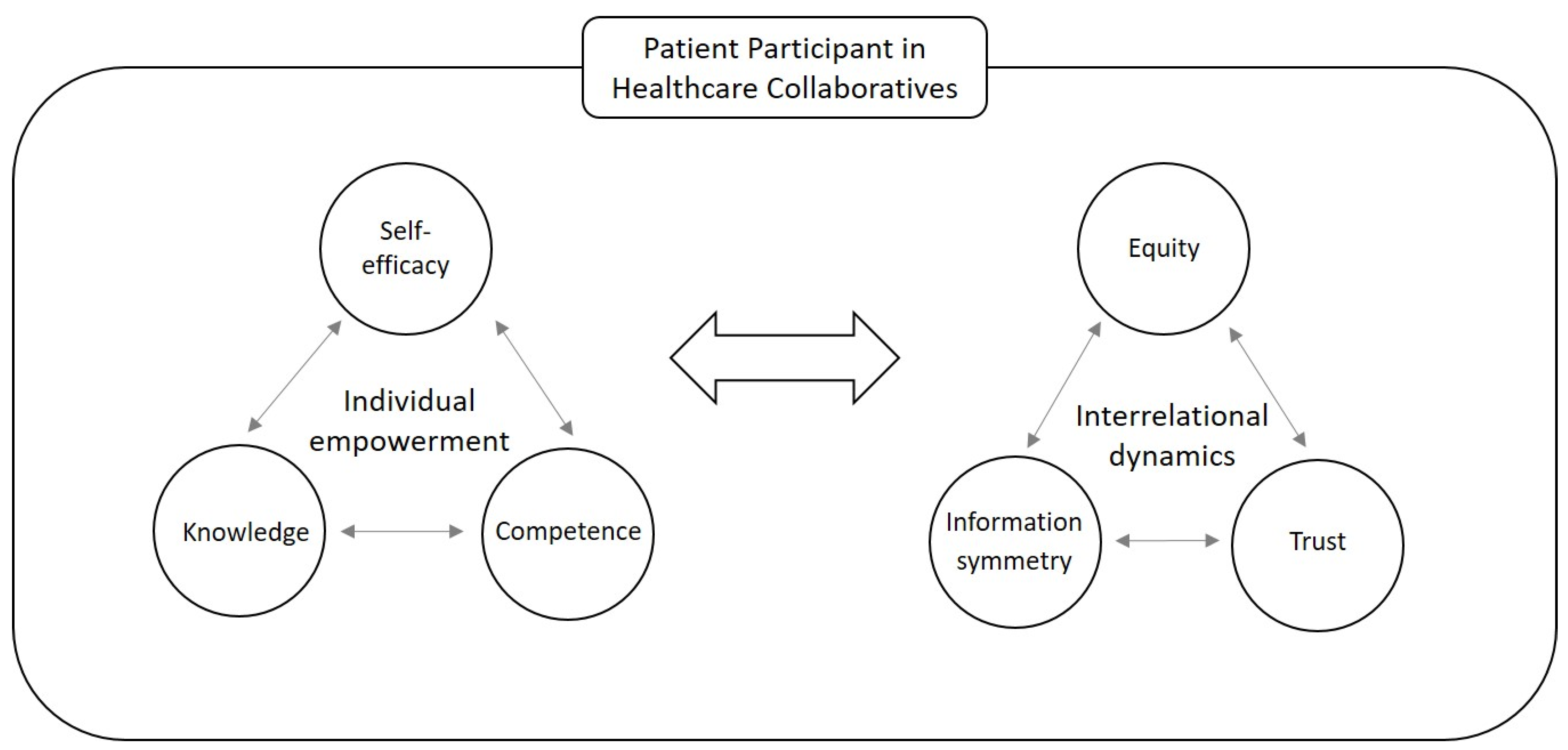
2.4. Conceptual Model
3. Methods
3.1. Research Design
3.2. Data Collection
3.3. Data Analysis
4. Results
4.1. Case 1: Individually Empowered Patient Participant in a Consolidated Collaborative
4.2. Case 2: Individually Empowered Patient Participant in a Newly Established Collaborative
4.3. Case 3: Individually Empowered Patient Participant in a Mature Collaborative
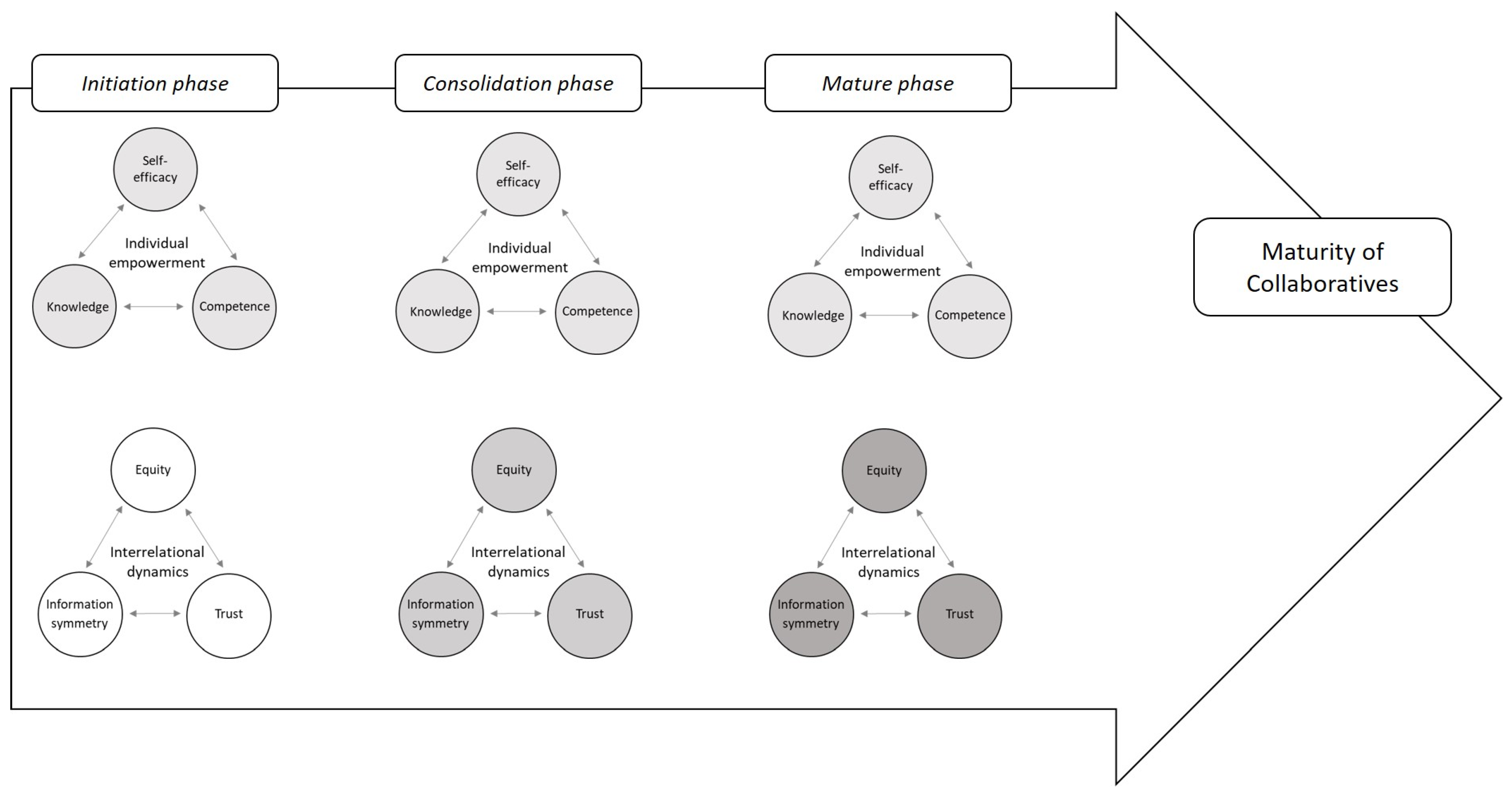
5. Discussion
5.1. Individual Empowerment
5.2. Interrelational Dynamics
5.3. Maturity/Context of Collaboratives
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- de Vries, J.; Huijsman, R. Supply chain management in health services: An overview. Supply Chain Manag. Int. J. 2011, 16, 159–165. [Google Scholar] [CrossRef]
- de Vries, J.; Huijsman, R.; Meijboom, B.; Schmidt-Bakx, S.; Westert, G. Supply chain management practices for improving patient-oriented care. Supply Chain. Manag. Int. J. 2011, 16, 166–175. [Google Scholar] [CrossRef]
- Sharma, S.; Conduit, J. Cocreation Culture in Health Care Organizations. J. Serv. Res. 2016, 19, 438–457. [Google Scholar] [CrossRef]
- Polese, F.; Tartaglione, A.M.; Cavacece, Y. Patient empowerment for healthcare service quality improvements: A value co-creation view. In 19th Toulon-Verona International Conference Excellence in Services; University of Huelva: Huelva, Spain, 2016. [Google Scholar]
- World Health Organization Regional Office for Europe. Health 2020: A European Policy Framework and Strategy for the 21st Century; World Health Organization: Copenhagen, Denmark, 2013.
- Fumagalli, L.P.; Radaelli, G.; Lettieri, E.; Bertele, P.; Masella, C. Patient Empowerment and its neighbours: Clarifying the boundaries and their mutual relationships. Health Policy 2015, 119, 384–394. [Google Scholar] [CrossRef] [PubMed]
- Tanenbaum, J.; Cebul, R.D.; Votruba, M.; Einstadter, D. Association of A Regional Health Improvement Collaborative with Ambulatory Care-Sensitive Hospitalizations. Health Aff. 2018, 37, 266–274. [Google Scholar] [CrossRef] [PubMed]
- McColl-Kennedy, J.R.; Vargo, S.L.; Dagger, T.S.; Sweeney, J.C.; van Kasteren, Y. Health Care Customer Value Cocreation Practice Styles. J. Serv. Res. 2012, 15, 370–389. [Google Scholar] [CrossRef]
- Ewert, B.; Evers, A. An ambiguous concept: On the meanings of co-production for health care users and user organizations? Volunt. Int. J. Volunt. Nonprofit Organ. 2014, 25, 425–442. [Google Scholar] [CrossRef]
- Lambert, D.M.; Garcia-Dastugue, S.J.; Croxton, K.L. Implementing supply chain management. Supply Chain. Manag. Process. Partnersh. Perform. 2006, 41, 217–235. [Google Scholar]
- Thakur, R.; Hsu, S.H.; Fontenot, G. Innovation in healthcare: Issues and future trends. J. Bus. Res. 2011, 65, 562–569. [Google Scholar] [CrossRef]
- WHO Commission on Social Determinants of Health; World Health Organization. Closing the Gap in a Generation: Health Equity through Action on the Social Determinants of Health: Commission on Social Determinants of Health Final Report; World Health Organization: Geneva, Switzerland, 2008.
- Sharma, S.; Conduit, J.; Hill, S.R. Organisational Capabilities for Customer Participation in Health Care Service Innovation. Australas. Mark. J. 2014, 22, 179–188. [Google Scholar] [CrossRef]
- Freeman, R.E. Divergent stakeholder theory. Acad. Manag. Rev. 1999, 24, 233–236. [Google Scholar] [CrossRef]
- Concannon, T.W.; Meissner, P.; Grunbaum, J.A.; McElwee, N.; Guise, J.-M.; Santa, J.; Conway, P.H.; Daudelin, D.; Morrato, E.H.; Leslie, L.K. A New Taxonomy for Stakeholder Engagement in Patient-Centered Outcomes Research. J. Gen. Intern. Med. 2012, 27, 985–991. [Google Scholar] [CrossRef] [PubMed]
- Tummers, L.; Teo, S.; Brunetto, Y.; Palumbo, R. Contextualizing co-production of health care: A systematic literature review. Int. J. Public Sect. Manag. 2016, 29, 72–90. [Google Scholar]
- Lengnick-Hall, C.A. Customer contributions to quality: A different view of the customer-oriented firm. Acad. Manag. Rev. 1996, 21, 791–824. [Google Scholar] [CrossRef]
- Yi, Y.; Gong, T. Customer value co-creation behavior: Scale development and validation. J. Bus. Res. 2013, 66, 1279–1284. [Google Scholar] [CrossRef]
- Morgan, R.M.; Hunt, S.D. The commitment-trust theory of relationship marketing. J. Mark. 1994, 58, 20–38. [Google Scholar] [CrossRef]
- Engdahl, E.; Lidskog, R. Risk, communication and trust: Towards an emotional understanding of trust. Public Underst. Sci. 2012, 23, 703–717. [Google Scholar] [CrossRef]
- Adams, J.S.; Rosenbaum, W. The relationship of worker productivity to Adams, JS. Toward an Understanding of Inequity. J. Abnorm. Soc. Psychol. 1963, 67, 422–436. [Google Scholar] [CrossRef]
- Ross, S.M.; Kapitan, S. Balancing self/collective-interest: Equity theory for prosocial consumption. Eur. J. Mark. 2018, 52, 528–549. [Google Scholar] [CrossRef]
- Reimann, F.; Ketchen, D.J., Jr. Power in supply chain management. J. Supply Chain. Manag. 2017, 53, 3–9. [Google Scholar] [CrossRef]
- Djellouli, N.; Jones, L.; Barratt, H.; Ramsay, A.I.; Towndrow, S.; Oliver, S. Involving the public in decision-making about large-scale changes to health services: A scoping review. Health Policy 2019, 123, 635–645. [Google Scholar] [CrossRef]
- Brito, R.P.; Miguel, P.L.S. Power, Governance, and Value in Collaboration: Differences between Buyer and Supplier Perspectives. J. Supply Chain Manag. 2017, 53, 61–87. [Google Scholar] [CrossRef]
- Ansell, C.; Gash, A. Collaborative Governance in Theory and Practice. J. Public Adm. Res. Theory 2007, 18, 543–571. [Google Scholar] [CrossRef]
- Zimmerman, M.A. Psychological empowerment: Issues and illustrations. Am. J. Community Psychol. 1995, 23, 581–599. [Google Scholar] [CrossRef] [PubMed]
- Damen, H.; Veerman, J.W.; Vermulst, A.A.; Nieuwhoff, R.; de Meyer, R.E.; Scholte, R.H.J. Parental Empowerment: Construct Validity and Reliability of a Dutch Empowerment Questionnaire (EMPO). J. Child Fam. Stud. 2016, 26, 424–436. [Google Scholar] [CrossRef]
- Cattaneo, L.B.; Chapman, A.R. The process of empowerment: A model for use in research and practice. Am. Psychol. 2010, 65, 646–659. [Google Scholar] [CrossRef] [PubMed]
- Locke, E.A.; Latham, G.P. Building a practically useful theory of goal setting and task motivation: A 35-year odyssey. Am. Psychol. 2002, 57, 705–717. [Google Scholar] [CrossRef] [PubMed]
- Stajkovic, A.D.; Luthans, F. Social cognitive theory and self-efficacy: Goin beyond traditional motivational and behavioral approaches. Organ. Dyn. 1998, 26, 62–74. [Google Scholar] [CrossRef]
- Luthans, F.; Avolio, B.J.; Avey, J.B.; Norman, S.M. positive psychological capital: Measurement and relationship with performance and satisfaction. Pers. Psychol. 2007, 60, 541–572. [Google Scholar] [CrossRef]
- Chronister, K.M.; McWhirter, E.H. An experimental examination of two career interventions for battered women. J. Couns. Psychol. 2006, 53, 151–164. [Google Scholar] [CrossRef]
- Speer, P.W. Intrapersonal and interactional empowerment: Implications for theory. J. Community Psychol. 2000, 28, 51–61. [Google Scholar] [CrossRef]
- Webler, T. “Right” discourse in citizen participation: An evaluative yardstick. In Fairness and Competence in Citizen Participation; Springer: Dordrecht, Germany, 1995; pp. 35–86. [Google Scholar]
- Stephens, K.J.; Fulk, J.; Monge, P.R. Constrained choices in alliance formations: Cupids and organizational marriages. Hum. Relat. 2009, 62, 501–536. [Google Scholar] [CrossRef]
- Saunders, M.; Lewis, P.; Thornhill, A. Research Methods for Business Students, 4th ed.; Pearson Education: London, UK, 2011. [Google Scholar]
- Barasa, E.W.; Molyneux, S.; English, M.; Cleary, S. Setting healthcare priorities in hospitals: A review of empirical studies. Health Policy Plan. 2014, 30, 386–396. [Google Scholar] [CrossRef] [PubMed]
- Gibson, J.L.; Martin, D.K.; Singer, P.A. Priority setting in hospitals: Fairness, inclusiveness, and the problem of institutional power differences. Soc. Sci. Med. 2005, 61, 2355–2362. [Google Scholar] [CrossRef] [PubMed]
- Wallerstein, N. What is the Evidence on Effectiveness of Empowerment to Improve Health; World Health Organization, Regional Office for Europe: Copenhagen, Denmark, 2006; p. 37.
- Kuntz, J.R.C.; Malinen, S.; Näswall, K. Employee resilience: Directions for resilience development. Consult. Psychol. J. Pract. Res. 2017, 69, 223–242. [Google Scholar] [CrossRef]
- Su, H.Y.; Fang, S.C.; Young, C.S. Influences of relationship transparency from intellectual capital reporting on supply chain partnerships with suppliers: A field experiment. Supply Chain. Manag. Int. J. 2013, 18, 178–193. [Google Scholar] [CrossRef]
- Gibbert, M.; Ruigrok, W. The ‘‘what’’and ‘‘how’’of case study rigor: Three strategies based on published work. Organ. Res. Methods 2010, 13, 710–737. [Google Scholar] [CrossRef]
- Yin, R.K. How to do better case studies. SAGE Handb. Appl. Soc. Res. Methods 2009, 2, 254–282. [Google Scholar]
- Mann, C.; Chilcott, S.; Plumb, K.; Brooks, E.; Man, M.S. Reporting and appraising the context, process and impact of PPI on contributors, researchers and the trial during a randomised controlled trial-the 3D study. Res. Involv. Engagem. 2018, 4, 15. [Google Scholar] [CrossRef]
- Groenewegen, P.P.; Hansen, J.; de Jong, J.D. Trust in times of health reform. Health Policy 2019, 123, 281–287. [Google Scholar] [CrossRef]
- Brett, J.O.; Staniszewska, S.; Mockford, C.; Herron-Marx, S.; Hughes, J.; Tysall, C.; Suleman, R. A Systematic Review of the Impact of Patient and Public Involvement on Service Users, Researchers and Communities. Patient-Patient-Cent. Outcomes Res. 2014, 7, 387–395. [Google Scholar] [CrossRef] [PubMed]
- Schruijer, S.G. Developing collaborative interorganizational relationships: An action research approach. Team Perform. Manag. Int. J. 2020, 26, 17–28. [Google Scholar] [CrossRef]
- Lucero, J.; Wallerstein, N.; Duran, B.; Alegria, M.; Greene-Moton, E.; Israel, B.; Kastelic, S.; Magarati, M.; Oetzel, J.; Pearson, C.; et al. Development of a Mixed Methods Investigation of Process and Outcomes of Community-Based Participatory Research. J. Mix. Methods Res. 2016, 12, 55–74. [Google Scholar] [CrossRef] [PubMed]
- Christens, B.D. Toward relational empowerment. Am. J. Community Psychol. 2012, 50, 114–128. [Google Scholar] [CrossRef]
- Jagosh, J.; Macaulay, A.C.; Pluye, P.; Salsberg, J.; Bush, P.; Henderson, J.; Sirett, E.; Wong, G.; Cargo, M.; Herbert, C.P.; et al. Uncovering the Benefits of Participatory Research: Implications of a Realist Review for Health Research and Practice. Milbank Q. 2012, 90, 311–346. [Google Scholar] [CrossRef] [PubMed]
- Romsland, G.I.; Milosavljevic, K.L.; Andreassen, T.A. Facilitating non-tokenistic user involvement in research. Res. Involv. Engag. 2019, 5, 18. [Google Scholar] [CrossRef]
- De Wit, M.P.T.; Kvien, T.K.; Gossec, L. Patient participation as an integral part of patient-reported outcomes development ensures the representation of the patient voice: A case study from the field of rheumatology. RMD Open 2015, 1, e000129. [Google Scholar] [CrossRef]
- Allen, M.L.; Salsberg, J.; Knot, M.; LeMaster, J.W.; Felzien, M.; Westfall, J.M.; Herbert, C.P.; Vickery, K.; Culhane-Pera, K.; Ramsden, V.R.; et al. Engaging with communities, engaging with patients: Amendment to the NAPCRG 1998 Policy Statement on Responsible Research with Communities: Table 1. Fam. Pract. 2016, 34, 313–321. [Google Scholar] [CrossRef]
- Watson, E.R.; Foster-Fishman, P.G. The Exchange Boundary Framework: Understanding the Evolution of Power within Collaborative Decision-Making Settings. Am. J. Community Psychol. 2012, 51, 151–163. [Google Scholar] [CrossRef]
- Banner, D.; Bains, M.; Carroll, S.; Kandola, D.K.; Rolfe, D.E.; Wong, C.; Graham, I.D. Patient and public engagement in integrated knowledge translation research: Are we there yet? Res. Involv. Engagem. 2019, 5, 8. [Google Scholar] [CrossRef]
| RHIC | Total of Stakeholders Present (n) | Project Manager (n) | Health Insurance Representative (n) | Health Professional (n) | Patient Participant (n) |
|---|---|---|---|---|---|
| Case 1 | 6 | 1 | 2 | 2 | 2 * |
| Case 2 | 11 | 2 | 2 | 6 | 2 * |
| Case 3 | 14 | 1 | 2 | 9 | 2 ** |
| Observation Objectives | Case 1 (n) | Case 2 (n) | Case 3 (n) |
|---|---|---|---|
| Knowledge sharing/collaboration | |||
| All information shared | 12 | 3 | 12 |
| Participation | 47 | 127 | 180 |
| Health literacy | |||
| Language/technical jargon | 0 | 2 | 1 |
| Explanation | 15 | 18 | 14 |
| Role leadership | |||
| Project manager behaviour | 7 | 19 | 25 |
| Other members behaviour | 0 | 16 | 22 |
| Personal skills | |||
| Time spoken | 1 | 3 | 0 |
| Use voice | 6 | 7 | 5 |
| Responsibility | |||
| Prepared | 3 | 1 | 5 |
| Willing to execute tasks | 1 | 4 | 0 |
| Relationship | |||
| Shakes hand | 2 | 6 | 2 |
| Makes eye contact | 13 | 23 | 22 |
| Interrupts speaker | 0 | 7 | 4 |
| Sitting position | 16 | 11 | 9 |
| Private talk/business talk | 1/1 | 5/7 | 10/16 |
| Other non-verbal signs | 38 | 93 | 84 |
| Interview Objectives | Case 1 | Case 2 | Case 3 |
|---|---|---|---|
| Self-efficacy | |||
| Motivation | 3 | 2 | 5 |
| Believe in oneself | 12 | 4 | 6 |
| Emotional involvement | 5 | 11 | 8 |
| Sensemaking | 5 | 5 | 2 |
| Knowledge | |||
| Critical awareness | 4 | 7 | 6 |
| Leadership | 4 | 4 | 3 |
| Action | 4 | 3 | 5 |
| Competence | |||
| Decision making | 1 | 1 | 1 |
| Problem solving | 4 | 5 | 3 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Minheere, A.; Lambrechts, W.; Mampaey, J.; Stough, T.; Caniëls, M.C.J.; Semeijn, J. Patient Power and Empowerment: Mitigating Elements of Valuable Patient Participation in Healthcare Collaboratives. Behav. Sci. 2023, 13, 347. https://doi.org/10.3390/bs13040347
Minheere A, Lambrechts W, Mampaey J, Stough T, Caniëls MCJ, Semeijn J. Patient Power and Empowerment: Mitigating Elements of Valuable Patient Participation in Healthcare Collaboratives. Behavioral Sciences. 2023; 13(4):347. https://doi.org/10.3390/bs13040347
Chicago/Turabian StyleMinheere, Anja, Wim Lambrechts, Jelle Mampaey, Talia Stough, Marjolein C. J. Caniëls, and Janjaap Semeijn. 2023. "Patient Power and Empowerment: Mitigating Elements of Valuable Patient Participation in Healthcare Collaboratives" Behavioral Sciences 13, no. 4: 347. https://doi.org/10.3390/bs13040347
APA StyleMinheere, A., Lambrechts, W., Mampaey, J., Stough, T., Caniëls, M. C. J., & Semeijn, J. (2023). Patient Power and Empowerment: Mitigating Elements of Valuable Patient Participation in Healthcare Collaboratives. Behavioral Sciences, 13(4), 347. https://doi.org/10.3390/bs13040347







