Haptic Nudging Using a Wearable Device to Promote Upper Limb Activity during Stroke Rehabilitation: Exploring Diurnal Variation, Repetition, and Duration of Effect
Abstract
:1. Introduction
2. Materials and Methods
2.1. Dataset
2.2. Study Procedures
- No movement, where no movement was observed;
- Affected upper limb movement, where movement of the affected upper limb alone was observed;
- Unaffected upper limb movement, where movement of the unaffected upper limb alone was observed;
- Bimanual movement, where movement of both upper limbs was observed to perform a common task;
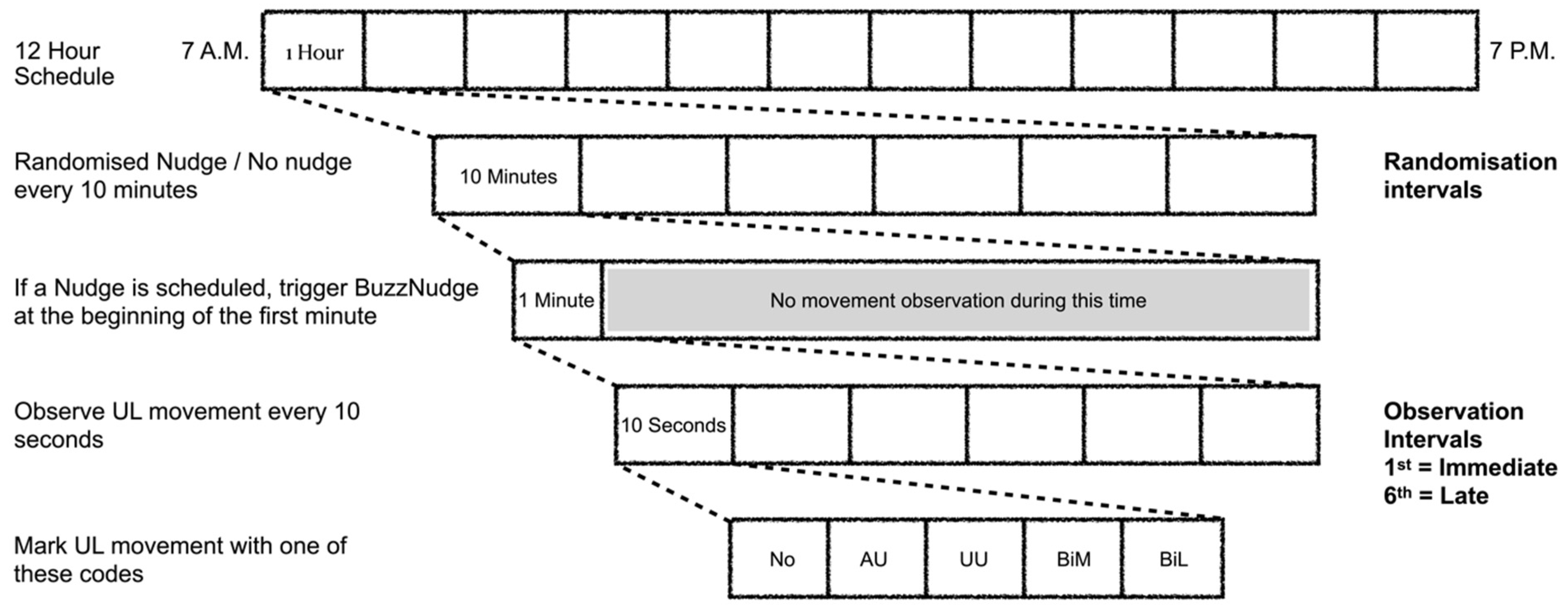
2.3. Haptic Nudge Randomisation Schedule
- Nudge;
- No nudge;
- Nudge-Nudge;
- No nudge-No nudge;
- Nudge-Nudge-Nudge;
- No nudge-No nudge-No nudge.
2.4. Data Analysis
2.4.1. Statistical Analysis
2.4.2. Estimated Effects
3. Results
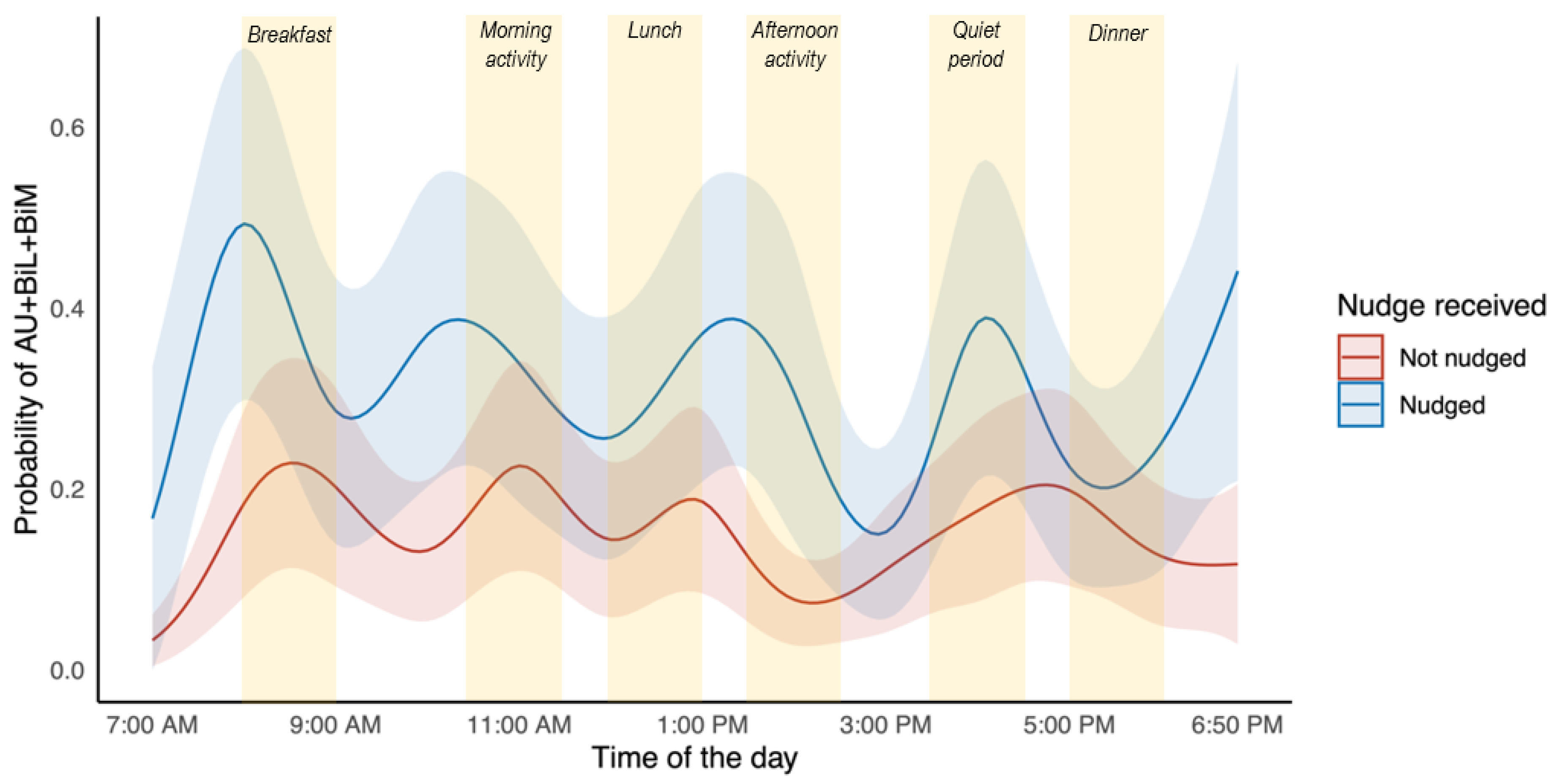
3.1. Is There Diurnal Variation in the Effect of a Haptic Nudge?
3.2. How Long Does the Effect of a Haptic Nudge Last?
3.3. Is the Effect of a Haptic Nudge Dependent on the Repetition of Nudges?
4. Discussion
4.1. Effect of Haptic Nudging
4.1.1. Diurnal Variation
4.1.2. Duration of Effect
4.1.3. Repetition of Nudges
4.2. Limitations
4.3. Future Directions
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Johansson, D.; Malmgren, K.; Alt Murphy, M. Wearable sensors for clinical applications in epilepsy, Parkinson’s disease, and stroke: A mixed-methods systematic review. J. Neurol. 2018, 265, 1740–1752. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.B.; Cadmus-Bertram, L.A.; Natarajan, L.; White, M.M.; Madanat, H.; Nichols, J.F.; Ayala, G.X.; Pierce, J.P. Wearable sensor/device (Fitbit One) and SMS text-messaging prompts to increase physical activity in overweight and obese adults: A randomized controlled trial. Telemed. J. E-Health 2015, 21, 782–792. [Google Scholar] [CrossRef] [PubMed]
- Dowling, A.V.; Fisher, D.S.; Andriacchi, T.P. Gait modification via verbal instruction and an active feedback system to reduce peak knee adduction moment. J. Biomech. Eng. 2010, 132, 071007. [Google Scholar] [CrossRef] [PubMed]
- Jiang, J.; Qin, Y.; Kim, I.; Wang, Y. Towards an IoT-Based Upper Limb Rehabilitation Assessment System. In Proceedings of the 39th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Jeju Island, South Korea, 11–25 July 2017; pp. 2414–2417. [Google Scholar] [CrossRef]
- Laranjo, L.; Ding, D.; Heleno, B.; Kocaballi, B.; Quiroz, J.C.; Tong, H.L.; Chahwan, B.; Neves, A.L.; Gabarron, E.; Dao, K.P.; et al. Do smartphone applications and activity trackers increase physical activity in adults? Systematic review, meta-analysis and metaregression. Br. J. Sports Med. 2021, 55, 422–432. [Google Scholar] [CrossRef]
- Case, M.A.; Burwick, H.A.; Volpp, K.G.; Patel, M.S. Accuracy of smartphone applications and wearable devices for tracking physical activity data. JAMA 2015, 313, 625–626. [Google Scholar] [CrossRef] [PubMed]
- Kao, Y.S.; Nawata, K.; Huang, C.Y. An exploration and confirmation of the factors influencing adoption of IoT-based wearable fitness trackers. Int. J. Environ. Res. Public Health 2019, 16, 3227. [Google Scholar] [CrossRef]
- Dunn, J.; Runge, R.; Synyder, M. Wearables and the medical revolution. Per. Med. 2018, 15, 429–448. [Google Scholar] [CrossRef]
- Krishnamurthi, R.V.; Ikeda, T.; Feigin, V.L. Global, regional and country-specific burden of ischaemic stroke, intracerebral haemorrhage and subarachnoid haemorrhage: A systematic analysis of the Global Burden of Disease Study 2017. Neuroepidemiology 2020, 54, 171–179. [Google Scholar] [CrossRef]
- Veerbeek, J.M.; van Wegen, E.; van Peppen, R.; van der Wees, P.J.; Hendriks, E.; Rietberg, M.; Kwakkel, G. What is the evidence for physical therapy poststroke? A systematic review and meta-analysis. PLoS ONE 2014, 9, e87987. [Google Scholar] [CrossRef]
- Stroke Foundation. Clinical Guidelines for Stroke Management; Stroke Foundation: Melbourne, Australia, 2022. [Google Scholar]
- McLaren, R.; Signal, N.; Lord, S.; Taylor, S.; Henderson, J.; Taylor, D. The volume and timing of upper limb movement in acute stroke rehabilitation: Still room for improvement. Disabil. Rehabil. 2020, 42, 3237–3242. [Google Scholar] [CrossRef]
- Bernhardt, J.; Chan, J.; Nicola, I.; Collier, J.M. Little therapy, little physical activity: Rehabilitation within the first 14 days of organized stroke unit care. J. Rehab. Med. 2007, 39, 43–48. [Google Scholar] [CrossRef]
- Louie, D.R.; Bird, M.; Menon, C.; Eng, J.J. Perspectives on the prospective development of stroke-specific lower extremity wearable monitoring technology: A qualitative focus group study with physical therapists and individuals with stroke. J. NeuroEngineering Rehabil. 2020, 17, 31. [Google Scholar] [CrossRef] [PubMed]
- Lynch, E.A.; Jones, T.M.; Simpson, D.B.; Fini, N.A.; Kuys, S.S.; Borschmann, K.; Kramer, S.; Johnson, L.; Callisaya, M.L.; Mahendran, N.; et al. Activity monitors for increasing physical activity in adult stroke survivors. Cochrane Database Syst. Rev. 2018, 7, CD012543. [Google Scholar] [CrossRef]
- Kanai, M.; Izawa, K.P.; Kobayashi, M.; Onishi, A.; Kubo, H.; Nozoe, M.; Mase, K.; Shimada, S. Effect of accelerometer-based feedback on physical activity in hospitalized patients with ischemic stroke: A randomized controlled trial. Clin. Rehabil. 2018, 32, 1047–1056. [Google Scholar] [CrossRef]
- Mercer, K.; Li, M.; Giangregorio, L.; Burns, C.; Grindrod, K. Behavior change techniques present in wearable activity trackers: A critical analysis. JMIR Mhealth Uhealth 2016, 4, e40. [Google Scholar] [CrossRef] [PubMed]
- Sullivan, A.N.; Lachman, M.E. Behavior change with fitness technology in sedentary adults. A review of the evidence for increasing physical activity. Front. Public Health 2016, 4, 289. [Google Scholar] [CrossRef]
- Peng, W.; Li, L.; Kononova, A.; Cotten, S.; Kamp, K.; Bowen, M. Habit formation in wearable activity tracker use among older adults: Qualitative study. JMIR Mhealth Uhealth 2021, 9, e22488. [Google Scholar] [CrossRef] [PubMed]
- Meske, C.; Amojo, I.; Poncette, A.; Balzer, F. The potential role of digital nudging in the digital transformation of the healthcare industry. In Design, User Experience, and Usability. Application Domains. HCII 2019; Marcus, A., Wang, W., Eds.; Springer: Cham, Switzerland, 2019. [Google Scholar]
- Kwan, Y.H.; Cheng, T.Y.; Yoon, S.; Ho, L.Y.C.; Huang, C.W.; Chew, E.H.; Thumboo, J.; Østbye, T.; Low, L.L. A systematic review of nudge theories and strategies used to influence adult health behaviour and outcome in diabetes management. Diabetes Metab. 2020, 46, 450–460. [Google Scholar] [CrossRef] [PubMed]
- Forberger, S.; Wichmann, F.; Comito, C.N. Nudges used to promote physical activity and to reduce sedentary behaviour in the workplace: Results of a scoping review. Prev. Med. 2022, 155, 106922. [Google Scholar] [CrossRef] [PubMed]
- Ulmer, T.; Baldauf, M. Keep Moving! A Systematic Review of App-Based Behavior Change Techniques and Visualizations for Promoting Everyday Physical Activity. In Proceedings of the Human-Computer Interaction. User Experience and Behavior, HCII 2022, Virtual Event, 26 June–1 July 2022; Springer: Berlin/Heidelberg, Germany, 2022. [Google Scholar]
- Shull, P.B.; Damian, D.D. Haptic wearables as sensory replacement, sensory augmentation and trainer—A review. J. Neuroeng. Rehabil. 2015, 12, 59. [Google Scholar] [CrossRef]
- Chin, L.F.; Hayward, K.S.; Soh, A.J.A.; Tan, C.M.; Wong, C.J.R.; Loh, J.W.; Loke, G.J.H.; Brauer, S. An accelerometry and observational study to quantify upper limb use after stroke during inpatient rehabilitation. Physioth. Res. Int. 2019, 24, e1784. [Google Scholar] [CrossRef] [PubMed]
- Da-Silva, R.H.; Moore, S.A.; Rodgers, H.; Shaw, L.; Sutcliffe, L.; van Wijck, F.; Price, C.I. Wristband accelerometers to motiVate arm exercises after stroke (WAVES): A pilot randomized controlled trial. Clin. Rehabil. 2019, 33, 1391–1403. [Google Scholar] [CrossRef]
- Signal, N.E.J.; McLaren, R.; Rashid, U.; Vandal, A.; King, M.; Almesfer, F.; Henderson, J.; Taylor, D. Haptic Nudges Increase Affected Upper Limb Movement During Inpatient Stroke Rehabilitation: Multiple-Period Randomized Crossover Study. JMIR Mhealth Uhealth 2020, 8, e17036. [Google Scholar] [CrossRef]
- Bernhardt, J.; Dewey, H.; Thrift, A.; Donnan, G. Inactive and alone: Physical activity within the first 14 days of acute stroke unit care. Stroke 2004, 35, 1005–1009. [Google Scholar] [CrossRef]
- Herbert, R.D.; Kasza, J.; Bø, K. Analysis of randomised trials with long-term follow-up. BMC Med. Res. Methodol. 2018, 18, 48. [Google Scholar] [CrossRef] [PubMed]
- Greenland, S.; Robins, J.M. Identifiability, exchangeability and confounding revisited. Epidemiol. Perspect. Innov. 2009, 6, 4. [Google Scholar] [CrossRef] [PubMed]
- Keselman, J.C.; Keselman, H. Analysing unbalanced repeated measures designs. Br. J. Math. Stat. Psychol. 1990, 43, 265–282. [Google Scholar] [CrossRef]
- Fitzmaurice, G.M.; Ravichandran, C. A primer in longitudinal data analysis. Circulation 2008, 118, 2005–2010. [Google Scholar] [CrossRef]
- Donders, A.R.T.; Van Der Heijden, G.J.; Stijnen, T.; Moons, K.G. Review: A gentle introduction to imputation of missing values. J. Clin. Epidemiol. 2006, 59, 1087–1091. [Google Scholar] [CrossRef]
- Bhaskaran, K.; Smeeth, L. What is the difference between missing completely at random and missing at random? Int. J. Epidemiol. 2014, 43, 1336–1339. [Google Scholar] [CrossRef]
- Nagelkerke, N.; Fidler, V.; Bernsen, R.; Borgdorff, M. Estimating treatment effects in randomized clinical trials in the presence of non-compliance. Stat. Med. 2000, 19, 1849–1864. [Google Scholar] [CrossRef] [PubMed]
- Small, D.S.; Ten Have, T.R.; Joffe, M.M.; Cheng, J. Random effects logistic models for analysing efficacy of a longitudinal randomized treatment with non-adherence. Stat. Med. 2006, 25, 1981–2007. [Google Scholar] [CrossRef] [PubMed]
- Bates, D.; Mächler, M.; Bolker, B.; Walker, S. Fitting linear mixed-effects models using lme4. J. Stat. Software 2015, 67, 1–48. [Google Scholar] [CrossRef]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2022; Available online: https://www.R-project.org/ (accessed on 1 December 2023).
- Wickham, H. ggplot2: Elegant Graphics for Data Analysis; Springer-Verlag: New York, NY, USA, 2016. [Google Scholar]
- Kassambara, A. ggpubr: ‘ggplot2’ Based Publication Ready Plots. 2023. Available online: https://CRAN.R-project.org/package=ggpubr (accessed on 1 December 2023).
- Lenth, R.V. emmeans: Estimated Marginal Means, aka Least-Squares Means. 2023. Available online: https://CRAN.R-project.org/package=emmeans (accessed on 1 December 2023).
- Xiao, N. ggsci: Scientific Journal and Sci-Fi Themed Color Palettes for ‘ggplot2’. Available online: https://CRAN.R-project.org/package=ggsci (accessed on 1 December 2023).
- Wickham, H.; François, R.; Henry, L.; Müller, K.; Vaughan, V. dplyr: A Grammar of Data Manipulation. 2023. Available online: https://CRAN.R-project.org/package=dplyr (accessed on 1 December 2023).
- Wickham, H. forcats: Tools for Working with Categorical Variables (Factors). 2023. Available online: https://CRAN.R-project.org/package=forcats (accessed on 1 December 2023).
- Skogestad, I.J.; Kirkevold, M.; Larsson, P.; Borge, C.R.; Indredavik, B.; Gay, C.L.; Lerdal, A. Post-stroke fatigue: An exploratory study with patients and health professionals to develop a patient-reported outcome measure. J. Patient Rep. Outcomes 2021, 5, 35. [Google Scholar] [CrossRef] [PubMed]
- Moore, S.A.; Da Silva, R.; Balaam, M.; Brkic, L.; Jackson, D.; Jamieson, D.; Ploetz, T.; Rodgers, H.; Shaw, L.; van Wijck, F.; et al. Wristband accelerometers to motiVate arm exercise after stroke (WAVES): Study protocol for a pilot randomized controlled trial. Trials 2016, 17, 508. [Google Scholar] [CrossRef]
- Da-Silva, R.H.; van Wijck, F.; Shaw, L.; Rodgers, H.; Balaam, M.; Brkic, L.; Ploetz, T.; Jackson, D.; Ladha, K.; Price, C.I. Prompting arm activity after stroke: A clinical proof of concept study of wrist-worn accelerometers with a vibrating alert function. J. Rehabil. Assist. Technol. Eng. 2018, 5, 2055668318761524. [Google Scholar] [CrossRef] [PubMed]
- Brkic, L.; Shaw, L.; van Wijck, F.; Francis, R.; Price, C.; Forster, A.; Langhorne, P.; Watkins, C.; Rodgers, H. Repetitive arm functional tasks after stroke (RAFTAS): A pilot randomised controlled trial. Pilot Feasibility Stud. 2016, 2, 50. [Google Scholar] [CrossRef]
- Kilbreath, S.L.; Heard, R.C. Frequency of hand use in healthy older persons. Aust. J. Physiother. 2005, 51, 119–122. [Google Scholar] [CrossRef]
- Michielsen, M.E.; Selles, R.W.; Stam, H.J.; Ribbers, G.M.; Bussmann, J.B. Quantifying nonuse in chronic stroke patients: A study into paretic, nonparetic, and bimanual upper-limb use in daily life. Arch. Phys. Med. Rehabil. 2012, 93, 1975–1981. [Google Scholar] [CrossRef]
- Rogers, T.; Frey, E. Changing Behavior Beyond the Here and Now. In Blackwell Handbook of Judgment and Decision Making, 1st ed.; John Wiley & Sons, Ltd.: Oxford, UK; pp. 726–748.
- Kleim, J.A.; Jones, T.A. Principles of experience-dependent neural plasticity: Implications for rehabilitation after brain damage. J. Speech. Lang. Hear. Res. 2008, 51, S225–S239. [Google Scholar] [CrossRef]
- Kwasnicka, D.; Dombrowski, S.U.; White, M.; Sniehotta, F. Theoretical explanations for maintenance of behaviour change: A systematic review of behaviour theories. Health Psychol. Rev. 2016, 10, 277–296. [Google Scholar] [CrossRef]
- Rankin, C.H.; Abrams, T.; Barry, R.J.; Bhatnagar, S.; Clayton, D.F.; Colombo, J.; Coppola, G.; Geyer, M.A.; Glanzman, D.L.; Marsland, S.; et al. Habituation revisited: An updated and revised description of the behavioral characteristics of habituation. Neurobiol. Learn. Mem. 2009, 92, 135–138. [Google Scholar] [CrossRef]

| Participant | Age Range (Years) | Sex | Stroke Classification | Days Since Stroke | Affected UL | Affected UL = Dominant Hand |
|---|---|---|---|---|---|---|
| 1 | 70–79 | Male | LACS-I | 9 | Left | No |
| 2 | 80–89 | Female | TACS-I | 39 | Left | No |
| 3 | 70–79 | Female | TACS-I | 59 | Left | No |
| 4 | 40–49 | Female | LACS-H | 8 | Right | Yes |
| 5 | 60–69 | Female | PACS-I | 5 | Right | Yes |
| 6 | 80–89 | Male | PACS-I | 34 | Left | No |
| 7 | 70–79 | Male | TACS-I | 27 | Right | Yes |
| 8 | 80–89 | Female | PACS-I | 7 | Left | No |
| 9 | 80–89 | Male | TACS-I | 67 | Right | Yes |
| 10 | 60–69 | Male | PACS-I | 36 | Right | Yes |
| 11 | 50–59 | Female | TACS-I | 25 | Left | Yes |
| 12 | 70–79 | Male | LACS-H | 33 | Left | No |
| 13 | 80–89 | Male | PACS-I | 12 | Left | No |
| 14 | 60–69 | Male | LACS-I | 3 | Right | Yes |
| 15 | 70–79 | Male | PACS-H | 40 | Right | Yes |
| 16 | 80–89 | Female | PACS-I | 22 | Right | Yes |
| 17 | 60–69 | Female | PACS-I | 6 | Left | No |
| 18 | 60–69 | Male | POCS-I | 10 | Bilateral | Yes |
| 19 | 80–89 | Male | PACS-I | 9 | Right | Yes |
| 20 | 80–89 | Male | PACS-H | 160 | Right | Yes |
| Time of the Day | Odds Ratio ± SE [95% CI] | Z-Value | p-Value | Pairwise Comparisons against Odds Ratio for ‘Day’ p-Value |
|---|---|---|---|---|
| Day (7.00 a.m.–7.00 p.m.) | 2.37 ± 0.41 [1.68, 3.34] | 4.95 | <0.001 * | |
| Breakfast (8.00–9.00 a.m.) | 2.58 ± 0.66 [1.57, 4.26] | 3.72 | <0.001 * | 0.614 |
| Morning activity (10.30–11.30 a.m.) | 2.01 ± 0.47 [1.27, 3.17] | 2.99 | 0.003 * | 0.354 |
| Lunch (12.00–1.00 p.m.) | 2.17 ± 0.53 [1.35, 3.49] | 3.20 | 0.001 * | 0.617 |
| Afternoon activity (1.30–2.30 p.m.) | 4.63 ± 1.29 [2.67, 8.01] | 5.47 | <0.001 * | 0.001 * |
| Quiet period (3.30–4.30 p.m.) | 2.51 ± 0.67 [1.49, 4.22] | 3.45 | <0.001 * | 0.769 |
| Dinner (5.00–6.00 p.m.) | 1.36 ± 0.32 [0.86, 2.16] | 1.30 | 0.194 | 0.001 * |
| Nudge Pattern | Log Odds/Consecutive Condition ± SE [95% CI] | Z-Value | p-Value |
|---|---|---|---|
| Repetition | −0.1 ± 0.1 [−0.3, 0.1] | −0.9 | 0.4 |
| Delay | −0.4 ± 0.1 [−0.5, −0.2] | −3.6 | 0.0003 * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Signal, N.; Olsen, S.; Rashid, U.; McLaren, R.; Vandal, A.; King, M.; Taylor, D. Haptic Nudging Using a Wearable Device to Promote Upper Limb Activity during Stroke Rehabilitation: Exploring Diurnal Variation, Repetition, and Duration of Effect. Behav. Sci. 2023, 13, 995. https://doi.org/10.3390/bs13120995
Signal N, Olsen S, Rashid U, McLaren R, Vandal A, King M, Taylor D. Haptic Nudging Using a Wearable Device to Promote Upper Limb Activity during Stroke Rehabilitation: Exploring Diurnal Variation, Repetition, and Duration of Effect. Behavioral Sciences. 2023; 13(12):995. https://doi.org/10.3390/bs13120995
Chicago/Turabian StyleSignal, Nada, Sharon Olsen, Usman Rashid, Ruth McLaren, Alain Vandal, Marcus King, and Denise Taylor. 2023. "Haptic Nudging Using a Wearable Device to Promote Upper Limb Activity during Stroke Rehabilitation: Exploring Diurnal Variation, Repetition, and Duration of Effect" Behavioral Sciences 13, no. 12: 995. https://doi.org/10.3390/bs13120995
APA StyleSignal, N., Olsen, S., Rashid, U., McLaren, R., Vandal, A., King, M., & Taylor, D. (2023). Haptic Nudging Using a Wearable Device to Promote Upper Limb Activity during Stroke Rehabilitation: Exploring Diurnal Variation, Repetition, and Duration of Effect. Behavioral Sciences, 13(12), 995. https://doi.org/10.3390/bs13120995








