Abstract
Background: Health science students in post-secondary institutions experience high levels of depression and anxiety due to increased stress levels, workload, low socioeconomic status, and history of family mental illness, among other factors. Given the significant negative impact that depression and anxiety can have on undergraduate health science students, it is essential to understand the prevalence and correlation of these conditions in this population. In light of this, this scoping review aims to identify, document, and analyze the literature on the prevalence and determinants of anxiety and depression among undergraduate health sciences students and identify gaps in knowledge for future research. Methods: This scoping review was planned and executed using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for the Scoping Reviews statement. A comprehensive and systematic search was carried out for five databases, namely MEDLINE, Scopus, EMBASE, CINAHL, and PubMed. Results: From the literature identified by our search strategy, the lowest prevalence for anxiety was 5.8%, and the highest was 82.6%, with a median of 44.25%. The prevalence of depression ranged from a high of 88.8% to a low of 2.1%, with a median value of 34.8%. Our analysis revealed that correlates of anxiety and depression among health science students include sociodemographic factors such as age, sex, gender, relationships, ethnicity, and family history, personal health conditions, and academic and socioeconomic issues. Conclusions: With the high incidence of anxiety and depression among health science students, there is an increasing need to find practical remedies to support these students. It is also essential for policymakers and university authorities to implement interventions such as supportive text messages and other strategies geared toward providing support and improving the psychological well-being of health science students.
1. Introduction
Anxiety and depression are globally common aspects of mental illness, affecting millions of individuals every year [1]. Depression (major depressive disorder or clinical depression) can be defined as a common, but serious, mood disorder associated with negative feelings which affects how you feel, the way you think, and how you act. Individuals suffering from depression experience persistent feelings of hopelessness, sadness and loss of interest in things they usually enjoy [2]. Similarly, anxiety can be described as a normal reaction to stress whilst anxiety disorders involve excessive fear or anxiety. Anxiety disorders are the most common of mental disorders [3]. The impact of these conditions on quality of life is significant. They are associated with decreased productivity, social isolation, and, in severe cases, suicide [4,5]. Among undergraduate health science students, the prevalence of depression and anxiety is exceptionally high, likely due to the demanding academic curriculum, clinical rotations, and personal stressors [6,7]. University students are often confronted with psychological challenges, which have emerged as a public health concern [6,8]. Published reports indicate increased mental health problems among university students, including symptoms of depression and anxiety [9,10,11]. Anxiety and depression are often comorbid, and the presence of one typically increases the risk of the other occurring over time [12]. A survey conducted in the United States reported that nearly half of college students met the criteria for a mental health condition in the past year [9]. Similarly, in 2011, a survey in Alberta, Canada, showed that about 800 students reported a feeling of hopelessness and anxiety, while 34.2% felt depressed during the 12 months prior to survey participation [8].
The prevalence of depression and anxiety reported among university students varies by over 20% [10,11,13]. A cross-sectional study reported that 45.3% of university students, including health science students in North America, had symptoms of depression, and 48.1% had anxiety [14]. In another study conducted in Asia, 66.86% of participants had a diagnosis of depression, and 57.39% had anxiety [15]. An African study conducted among medical students found that 88.8% of participants experienced depression, while 82.6% of participants experienced anxiety [6]. Moreover, higher estimates of anxiety (75.5%) [16] and depression (84.4%) were reported in a cross-sectional survey of medical students [17].
Most studies have focused on common psychiatric conditions, including anxiety and depression among medical students [18,19,20], and emphasize the magnitude of mental health challenges in this context. Published research indicates that health science students, including students studying medicine, pharmacy, nursing, physiotherapy, occupational therapy, and clinical psychology, experience a high level of depression and anxiety due to increased workload [21] and other factors such as the intensity of the course work and exams [21,22,23,24]. The literature also suggests that female health sciences students experience more depression and anxiety than their male counterparts [19]. In addition, a history of family mental illness, low family income, and stress levels affected depression and anxiety among medical students [25,26]. This scoping review aims to identify, document, and analyze the literature on the prevalence and determinants of anxiety and depression among health sciences students and identify gaps in knowledge for future research.
The focus on health sciences students was deemed valuable given their distinct risk profiles, the implications of poor mental health on their clinical practice, and the utility of this analysis in guiding supportive reforms in medical education. Existing research indicates health science students face exceptionally high rates of depression and anxiety due to demanding academics, clinical rotations, personal stressors, and other unique pressures [27]. The psychological wellbeing of future healthcare professionals is particularly crucial given its impacts on quality of care, empathy, and medical errors. Hence it is a significant public health concern. Understanding variables linked to adverse mental health outcomes in health sciences students can inform tailored interventions and policy changes in their academic training environments. While there is substantial literature on mental health issues among general university students [28], synthesized evidence specifically among health sciences students is lacking. The research question we aim to answer is “what are the prevalence and correlates of anxiety and depression among health science students in different countries?”
2. Methods
This scoping review followed the standards of Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) extension for scoping reviews [29] and Arksey and O’Malley’s five-stage approach to scoping reviews. Arksey and O’Malley’s five stages are researching questions, searching for relevant studies, study selection, charting the data, and collating, summarizing, and reporting the results [30]. A comprehensive search strategy ensured transparency, replicability, and reliability.
Scoping reviews are optimal for mapping research areas that have not yet been extensively reviewed or exhibit complex, heterogeneous evidence. This approach aligned well with the broad research question examining the prevalence and correlations across diverse geographic settings. Scoping reviews allow the inclusion of all study designs, rather than just clinical trials as in systematic reviews [31]. This enabled a comprehensive overview of the observational epidemiological research on this public health issue among students. Considering the methodological and population variations across studies, the scoping review methodology enabled maximum inclusivity of prevalent literature from disparate global contexts and was optimally suited to broadly map the research area and inform future systematic investigations.
2.1. Searching for Relevant Studies
Relevant terms were used to identify and choose articles in databases: MEDLINE (Medical Literature Analysis and Retrieval System Online; Ovid MEDLINE ALL), PubMed, EMBASE (Excerpta Medica Database; Ovid interface), CINAHL (Cumulative Index of Nursing and Allied Health Literature; EBSCOhost interface), and Scopus Elsevier. These databases were selected to cover the key literatures in medical, health, nursing, allied health and broader scientific fields. They represent leading databases indexing research output globally across these disciplines and student populations. The search was limited to English language original studies, peer-reviewed quantitative articles as they aligned with the study eligibility criteria. Keywords representing the concepts of depression and anxiety among university or college students and their correlates and prevalence were applied in the search. Appendix A shows the specific MeSH terms, keywords and descriptors included in the search. The database search was completed on 20 December 2022.
2.2. Study Selection
Studies were deemed eligible for inclusion in this scoping review if they addressed the prevalence and correlates of depression or anxiety among health science students. The search was limited to English language original studies, peer-reviewed quantitative articles, and studies in which study participants were not tertiary, university, college, or medical students. Papers were also excluded if they were case reports, meta-analyses, systematic reviews, interventional studies or outcomes, commentaries, editorials, opinion pieces, or grey literature, including graduate student theses, non-peer-reviewed studies, non-research articles or conference reports or opinion pieces, commentaries, and editorials. The search was limited by publication year, from 2017 to 2022. This 6-year timeframe was selected to provide a contemporary overview of recent evidence while ensuring a sufficient volume of literature to map key prevalence and correlates. Two researchers independently reviewed citations during the title, abstract screening, and full-text review phases, and conflict was resolved through discussion and consensus. A total of 276 articles were initially identified for full-text review. After a thorough assessment, 205 articles were excluded, including 86 non health science students leaving a final selection of 71 articles for the comprehensive review. The PRISMA flow diagram summarizes this information in detail (Figure 1).
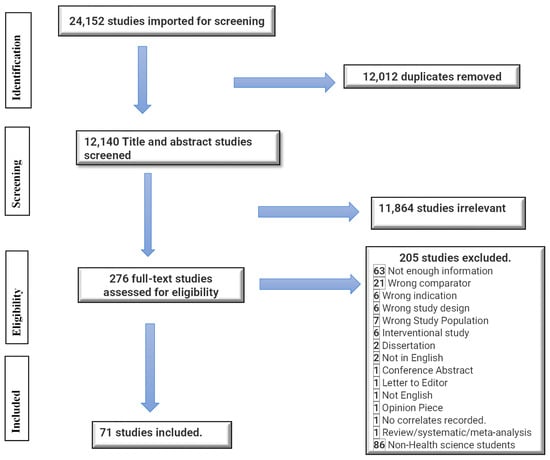
Figure 1.
PRISMA flow chart.
2.3. Data Charting and Extraction Process
Data were extracted for each article based on the following domains: author(s) name, year of publication, country of study, population/sample size [N], study design, assessment tools used, age, main findings, and conclusions.
2.4. Collating, Summarizing, and Reporting the Results
This scoping review gives an overview of existing evidence on the prevalence and the correlates of anxiety and depression among health sciences students. All relevant data were organized into tables and validated by at least two team members. The characteristics and results reported in each included article were summarized.
3. Results
3.1. Study Characteristics
The search strategy identified 24,152 citations. The Covidence software [32] was used to automatically remove 12,012 duplicates. Two hundred and seventy-six studies remained for full-text screening, and 157 of these were eligible for inclusion. This paper focuses on the seventy-one studies on health sciences students. This included a total of 36,271 participants, who were all health science-related students. The sample size for the individual article from Table 1 and Table 2 ranged from 77 to 2798 participants, with an age range from 16 years to 54 years. The minimum response rate was 9.4%, and the maximum was 100%, with a median response rate of 76.4%. The articles included studies from 2017 to 2022. Most of the studies were conducted in Asia (58%), followed by Europe (13%), North America (12%), and Africa (12%). In contrast, South American studies represented 5%, as shown in Figure 2.

Table 1.
Summary of studies reporting on the prevalence and correlates of anxiety and depression among health sciences students.

Table 2.
Continuation of summary of studies reporting on the prevalence and correlates of anxiety and depression among health sciences students.
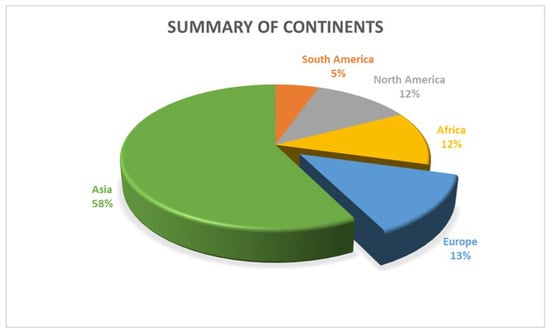
Figure 2.
Summary of continents.
3.2. Number of Studies and Scales Used
Health science students reported in our study includes students in medicine, health sciences, pharmacy, dentistry, nursing, and allied health sciences, midwifery and health management, veterinary, physiotherapy, speech therapy, and occupational therapy, optometry, social work, dietetics and kinesiology. Overall, 43 reported on the prevalence and correlates of anxiety whilst 62 studies reported on the prevalence and correlates of depression. Thirty-one studies focused on both anxiety and depression prevalence and correlates. The Beck Anxiety Inventory Scale was used in eight studies; the Beck Depression Inventory Scale was used in 19 studies, whilst the Hospital Anxiety Scale was used in 10 studies. The Hospital Depression Scale was used in 10 studies, the Patient Health Questionnaire 9 (PHQ) was used in 17 studies, and the Depression, Anxiety, and Stress Scale was used in 13 studies. The Generalized Anxiety Disorder Scale was used in five studies, and the Center for Epidemiological Studies Depression (CESD-R) was used in three studies. The following scales were used in one study: Personality Inventory, Profile of Mood States Short Form, Visual Analog Scale, Positive Orientation Scale, Courtauld Emotional Scale, Subjective Happiness Scale, COVID-induced Anxiety Scale, and State-Trait Anxiety Inventory for Adults (STAI).
3.3. Prevalence and Correlates of Anxiety and Depression
Anxiety and depression are usually comorbid, and the presence of one normally increases the risk of the other occurring over time [12]. Table 1 and Table 2 indicate that the highest prevalence of anxiety was 82.6% [6], and the lowest prevalence was 5.8% [19], with a median of 44.25%. The highest prevalence of anxiety was reported among the Asian ethnic groups and the lowest among the Igbo ethnic group of West Africa [47]. The prevalence of depression ranged from a low of 2.1% for severe depressive symptoms [63] to a high of 88.8% depression [6], with a median for depression was 34.8%. In terms of gender, the median prevalence of anxiety among female health science students was 48.1%, which is slightly higher than the median found in the general health science student population of 44.25%. For studies from 2017 to 2019, the prevalence of depression ranged from 4.4% severe or extreme depression to 66% depression [34,48,57]. Similarly, the prevalence of anxiety reported in our study from 2017 to 2019 range from 5.8% moderate to severe anxiety to 74% anxiety [37,60]. Some correlates of depression for studies between 2017 and 2019 includes academic burnout, academic incompetency, female gender, breakups in relationships, perceived financial burden, poor academic performance or lower academic achievement, poor relationship with peers, the pressure of passing exams, fear of stepping into the real world of medicine, third-year student, moderate or poor socioeconomic status and being married [20,23,38,60,67,74,79,80]. The rates of depression were highest in year two and year three and lowest in year one and year four [57]. Burnout plays a significant role in the rate of depression experienced by health science students. For instance, an increase in burnout increased depression, when there is low burnout the prevalence of depression was 13%, for intermediate burnout the prevalence of depression was 38%,and for those in the high burnout category the prevalence of depression was 66% [48]. Correlates of anxiety for the 2017 to 2019 studies included poor relationship with peers, the pressure of passing exams, fear of stepping into the real world of medicine, low optimism, poor academic performance, female gender, year of study, studying all night before the exam, extensive course load, and low grade point average [54,60,67,70,84]. Satisfaction with faculty and peer relationships also affected both depression and anxiety prevalence among dental students [41]. History of major trauma or psychiatric events increased the possibility of depression among medical school participants [34].
Most of the studies in our scoping review were conducted from 2020 to 2022. The prevalence of depression was ranged from 2.12% of students with severe depressive symptoms or 5.5% with depression to 88.8% [6,63,77]. The prevalence of anxiety ranged from 11.8% to 82.6% [6,77]. The common correlates of anxiety from 2020 to 2022 included dissatisfaction with the course, being in the exam period, female gender, age, students in lower years of study, perceived poor academic performance, history of a mental problem and concurrent physical illness, possible COVID-19 exposure, depression, personal burnout, lower grade point average, experience of COVID-19 symptoms, teaching and learning-related stressors [15,24,39,68,72,77]. Similarly, the correlates of depression from the 2020 to 2022 studies included students in lower years of study, perceived poor academic performance, history of a mental problem and concurrent physical illness, possible COVID-19 exposure, family history of depression, female gender, older age, student academic year, high emotional exhaustion, high cynicism, burnout, age, financial crisis in family, preclinical years (first and second year) compared to third, fourth, and final year), anxiety, personal burnout, work-related burnout, lower grade point average, and experience of COVID-19 symptoms [15,18,33,36,39,46,68,72,77,81].
4. Discussion
4.1. Prevalence and Correlates of Anxiety and Depression among Health Science Students
Anxiety symptoms are common among health sciences students, with a significant proportion of undergraduate medical students being anxious [49,89]. Published research reports that about one in three medical students globally have anxiety, and this prevalence rate is reportedly higher than the general population [90]. The prevalence of anxiety among the health science students in this scoping review ranged from 5.8% to 82.6% [6,19], with a median of 44.25%.
The disproportionately higher volume of evidence from Asian countries compared to other regions reveals some key implications. It likely reflects underlying variability in mental health awareness and research prioritization across regions. Cultural differences in stigma and openness regarding psychological issues may also contribute to more recognized cases in some societies. Nevertheless, the underrepresentation of Western and African contexts is concerning given their significant student populations. It suggests the need to direct more attention toward understanding depression/anxiety prevalence and relationships in these settings through systematic studies with consistent methodologies. As medical education globalizes, a balanced geographic distribution of mental health research across student communities will be increasingly beneficial. Ultimately a nuanced, culturally aware analysis accounting for societal variances underpinning any geographic differences can help inform customized interventions to support student wellness.
The huge variance between prevalence reported in our scoping review may be attributed to the methodological differences between studies or differences in clinical scales used in the measurement of anxiety and the time the research was conducted [91,92]. It is also worth mentioning that the scoping review search strategy was limited by the year of publication which may contribute to the huge disparity in the prevalence. Our scoping review also reported a median of 44.25% which is higher than the global prevalence of anxiety reported in a meta-analysis 33.8% (95% Confidence Interval: 29.2–38.7%) [90] This shows that health science students may experience increased anxiety compared to other university students. The prevalence of depression ranged from a low of 2.1% for severe depressive symptoms [63] to a high depression rate of 88.8% [6], with a median for depression was 34.8%.
4.2. Sociodemographic Correlates of Anxiety and Depression among Health Science Students
In terms of gender, the median prevalence of anxiety among female health science students was 48.1%, which is slightly higher than the median found in the general health science student population of 44.25%. This suggests that anxiety among female health science students may be higher than their male counterparts. This is consistent with what was reported by one study, which showed that female medical students experience more anxiety than their male counterparts [19]. Another study among medical undergraduates [89] also reported that females have higher anxiety scores than their male counterparts. This is in line with other reviews [93] which suggest that females are twice as likely to develop an anxiety disorder compared to males. Other studies have also suggested that biological factors such as stress responsiveness significantly contribute to the gender differentiation in some expressions of both depression and anxiety with female being affected substantially [94]. The prevalence of anxiety symptoms among college students remained relatively high [95]. Some studies reported that the prevalence of depression is higher among female health science students compared to their male counterparts [6,80]. The higher prevalence of depression among female health sciences students is consistent with the prevalence of depression reported among the general public [96]. Furthermore, more generally, in the health sector, women have been reported to have a higher risk of experiencing both anxiety and depression compared to men [97]. With respect to age, one study among the public reported that older participants had a significantly lower anxiety score than their younger counterparts [98]. The study also suggested that age might moderate the effects of anxiety since maturity and experience associated with aging may cause a reduction in anxiety [98]. However, in this scoping review, a relatively lower prevalence of anxiety, 11.8% to 66.86% [15,50,77], was reported among health science students who were aged 20–25 years.
Among the female gender, relationships with peers in the year of study slightly reduced anxiety (51%) [67]. On the contrary, some studies have suggested that relationship status does not independently predict mental health issues [5,99]. Other general relationships, such as satisfaction with faculty and peer relationships, still led to a considerably high prevalence of anxiety (66.8%), with dissatisfaction with administration leading to even higher anxiety at 74% [60]. With respect to ethnicity, one study reported that anxiety is prevalent among medical students from the Middle East and Asia [90], with the highest prevalence reported among the Asian ethnic groups and the lowest anxiety prevalence (25%) reported among the Igbo ethnic group [47]. Another study reported that racial/ethnic minority health science students are generally less likely to report less anxiety than Whites [100]. As reported for anxiety, ethnic minority health science students are generally less likely to report depression relative to Whites, although there is variability in the prevalence of depression among ethnic minorities ranging from as low as 14.3% among the Igbo group 14.3% [47] to as high as 40.0% among the Arab group [67,82].
4.3. Personal and Health Conditions as Correlates of Anxiety and Depression
Physical health activities, including exercise, are usually associated with good general health. In one study, 63% of medical students who lack physical activities were classified as having high state anxiety and contributory factors such as living off-campus, sleeping five hours or less and smoking [71]. On the other hand, a slightly lower anxiety prevalence (41.7%) was reported in another study where students had reduced engagement in physical and other leisure activities, poor sleep quality, and poor self-perceived mental health [88]. Another study identified that a history of mental health problems, use of psychotropic drugs, stressors in schools, and perceived stress correlated with the presence of moderate to high anxiety among medical students [77]. Furthermore, another study identified that participants who reported less than seven hours of sleep per night, worse general health, higher stress, or perceived lack of control had higher rates of anxiety [51]. Other studies have reported that medical students who smoke [65,71] and those with high consumption of energy drinks [66] have higher rates of anxiety. These cohorts may be struggling with managing academic work or other unmanaged stressors leading to reduced sleep, contributing to increased anxiety. According to one study, sleep deprivation, whether total or not, significantly increased state anxiety levels [101]. With respect to the personal and health conditions which are predictors of depression, smoking is often linked to depression [102], and a higher prevalence of depression has been reported among health science students who smoke [6]. Other studies have also reported a higher prevalence of depression among students who smoke and use psychotropic medications [26], those who use alcohol [65], and those who have a history of psychiatric disorders or attempted suicide [7,77]. Furthermore, other studies reported higher depression prevalence in health science students with a history of mental health problems [66], a history of trauma [34], and living with personal chronic disease [42,81].
The onset of the COVID pandemic affected healthcare workers and the general public alike. During the initial peak phase of COVID-19, more than 60% of US medical students screened positive for pandemic-related anxiety [61]. The highest prevalence of both anxiety and depression among medical students was 82.6% and 88.8%, respectively, reported in our study was during the COVID-19 crisis [6].
4.4. Academic-Related Issues as Predictors of Anxiety and Depression
Teaching and learning-related stressors and high academic distress have been correlated with moderate to high anxiety [86,87]. Stressors related to high academic achievement are some of the most challenging problems experienced by health science students, resulting in high anxiety [55,67]. Several studies suggest that the pressure to succeed and pass exams during the time of assessment contributes to heightened anxiety (72% to 82.6% prevalence) in health science students, especially during the third year [6,38,49]. Extensive coursework coupled with studying all night before exams increases anxiety prevalence [54]. One study suggests that students in their final year may experience slightly less anxiety 40% [103], whilst another study suggests that those in first or second-year educational level experience increased anxiety 51.3% [59]. Finally, medical students’ burnout may lead to anxiety [72]. Depression prevalence can vary depending on the year of study or academic achievement [57]. For example, lower depression prevalence (15.1% to 29.2%) has been reported during the lower year of study or in preclinical students [19,80] compared to the prevalence of 53.0% in the senior academic years [66]. However, when students are in a lower year of study but have poor performance, depression prevalence increases significantly to about 44.6% [39]. Other studies have reported that students’ academic achievement and low academic grades increased depression to between 40% and 45.9% [55,67], with the highest prevalence of depression of 88.8% resulting from low achievement scores [6]. Related to these, academic burnout has been reported to contribute significantly to a higher prevalence of depression among health science students [79].
4.5. Limitations of the Scoping Review
This scoping review has several limitations. The search strategy was limited by the year of publication. We focused the search on only English language databases, which may lead to some older studies and some relevant studies in other languages that may not have been included. In addition, the search strategy may have been biased towards health and sciences databases, and there is the probability that searching other bibliographic databases may have resulted in additional relevant studies. Again, different studies included in this scoping review used different screening tools, which may have implications for the prevalence of anxiety and depression [92]. Finally, study characteristics, there are significance differences in terms of study characteristics like the range of response rates, differences in year of study, and potential overrepresentation of certain age groups which may affect the prevalences of depression and anxiety reported.
Notwithstanding these limitations, this scoping review gives a significant perspective on the prevalence and correlates of anxiety and depression among health science students.
5. Conclusions and Implications for Future Research
This scoping review has identified the prevalence and determinants of anxiety and depression among health science students. Health science students face many clinical requirements, pressure to pass exams, and family expectations [60]. The wide range of prevalence of anxiety and depression highlights the potential multifactorial predictors and impact of these problems among health science students. It also highlights the need for further research to understand better the prevalence and correlates of anxiety and depression among health science students and to identify the factors unique to certain populations which contribute to higher or lower prevalence of anxiety and depression. Health science training programs need to be designed to reduce the stressors which culminate into anxiety and depression among the students. University authorities, educationists and policy leaders should come together to review strategies for assessment, which removes the focus from examinations and high academic achievements and rather focus on professionalism, competence, good clinical judgement, and student wellbeing. Interventions and programs which provide cognitive behavioral therapy may also help reduce anxiety and depression and help improve mental health literacy and coping skills of health science students. Innovative interventions which are readily accessible and inexpensive may be developed, assessed, and offered to this cohort, especially those affected by anxiety and depression to improve their psychological well-being. Given that almost all health science students may be conversant with mobile technology, particularly texting and email messaging, these modes of healthcare delivery present a unique opportunity to offer support for their mental health [104]. One such program, ResilienceNHope, is an evidence-based text and email messaging innovation. It may be an appropriate mechanism for reaching and supporting college students to close the existing psychological treatment gap and improve their mental health literacy. In addition, several interventions have been reported to reduce psychological symptoms including mindfulness-based interventions alone or in combination with yoga, Cognitive Behavioral Therapy (CBT), and sport-based physical activity [105]. These can also be explored and adopted among health science students to improve their mental well-being. Considering the high prevalence of both anxiety and depression among the health science students, implementing such interventions will have potential long-term benefits for both the health science students and the broader healthcare field.
Health science students should be encouraged through advocacy groups to seek help when feeling stressed or overwhelmed to reduce the possibility of burnout or subsequent anxiety or depression. The huge disproportion in the number of studies published in different continents helps to appreciate that more research on depression and anxiety among health science students are conducted in Asia, but only 5% of research on this topic occurs in South America. This also beckon on researchers in these countries to refocus their attention on these cohorts. Considering the limitations of a scoping review, future studies may consider a systematic review with metanalysis.
Author Contributions
Conceptualization, G.A.-O.; software and validation, G.A.-O., B.A. and G.O.-D.; methodology and formal analysis, G.A.-O. and B.A.; data curation, G.A.-O., B.A. and G.O.-D.; investigation, G.A.-O. and B.A.; writing—original draft preparation, G.A.-O.; writing—review and editing, G.A.-O., B.A., G.O.-D. and E.E.; supervision, E.E. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by Alberta Mental Health Foundation. The funder did not participate in the study design or conduct; collection, management, analysis, data interpretation, review, writing, or approval of the manuscript; or the submission of the results for publication.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Appendix A
The specific MeSH terms, keyword and descriptors included in the search.: (depress* OR depression OR “depressive disorder” OR “depressive symptoms” OR “major depressive disorder”) OR (anxiety OR “anxiety disorder” OR “generalized anxiety disorder”), (predictors OR risk factors OR correlates OR predisposition OR determinants OR cause), AND (prevalence OR incidence OR epidemiology OR frequency OR occurrence OR statistics)AND (university student* OR undergraduate student* OR tertiary students” OR “higher education students” OR “college students” OR “post-secondary students”).
| depress*.mp.KL | |
| limit 1 to yr | 2017–2022 |
| anxiety*.mp. | |
| limit 3 to yr | 2017–2022 |
| 2 or 4 | |
| college student*.mp. | |
| limit 6 to yr | 2017–2022 |
| university student*.mp. | |
| limit 8 to yr | 2017–2022 |
| undergraduate student*.mp. | |
| limit 10 to yr | 2017–2022 |
| post-secondary student*.mp. | |
| limit 12 to yr | 2017–2022 |
| tertiary student*.mp. | |
| limit 14 to yr | 2017–2022 |
| 7 or 9 or 11 or 13 or 15 | |
| prevalence*.mp. | |
| limit 17 to yr | 2017–2022 |
| correlate*.mp. | |
| limit 19 to yr | 2017–2022 |
| determinant*.mp. | |
| limit 21 to yr | 2017–2022 |
| relat*.mp. | |
| limit 23 to yr | 2017–2022 |
| incidence*.mp. | |
| limit 25 to yr | 2017–2022 |
| 18 or 20 or 22 or 24 or 26 | |
| 5 and 16 and 2 |
References
- Richards, D.; Duffy, D.; Blackburn, B.; Earley, C.; Enrique, A.; Palacios, J.; Franklin, M.; Clarke, G.; Sollesse, S.; Connell, S.; et al. Digital IAPT: The effectiveness & cost-effectiveness of internet-delivered interventions for depression and anxiety disorders in the Improving Access to Psychological Therapies programme: Study protocol for a randomised control trial. BMC Psychiatry 2018, 18, 59. [Google Scholar]
- American Psychiatric Association. What Is Depression? APA: Washington, DC, USA, 2023. [Google Scholar]
- American Psychiatric Association. What Are Anxiety Disorders? APA: Washington, DC, USA, 2023. [Google Scholar]
- Langlois, S.; Morrison, P. Suicide deaths and suicide attempts. Health Rep. 2002, 13, 9–22. [Google Scholar]
- Agyapong, B.; Shalaby, R.; Eboreime, E.; Wei, Y.; Agyapong, V.I.O. Self-Reported Alcohol Abuse and the Desire to Receive Mental Health Counselling Predict Suicidal Thoughts/Thoughts of Self-Harm among Female Residents of Fort McMurray. Int. J. Env. Res. Public Health 2022, 19, 13620. [Google Scholar] [CrossRef]
- Abed, H.A.; Abd-Elraouf, M.S.E.D. Stress, Anxiety, Depression Among Medical Undergraduate Students at Benha University and Their Socio-Demographic Correlates. Egypt. J. Hosp. Med. 2022, 86, 27–32. [Google Scholar] [CrossRef]
- Shawahna, R.; Hattab, S.; Al-Shafei, R.; Tab’ouni, M. Prevalence and factors associated with depressive and anxiety symptoms among Palestinian medical students. BMC Psychiatry 2020, 20, 244. [Google Scholar] [CrossRef]
- Regehr, C.; Glancy, D.; Pitts, A. Interventions to reduce stress in university students: A review and meta-analysis. J. Affect. Disord. 2013, 148, 1–11. [Google Scholar] [CrossRef]
- Macaskill, A. The mental health of university students in the United Kingdom. Br. J. Guid. Couns. 2013, 41, 426–441. [Google Scholar] [CrossRef]
- Hakami, R.M. Prevalence of Psychological Distress among Undergraduate Students at Jazan University: A Cross-Sectional Study. Saudi J. Med. Med. Sci. 2018, 6, 82–88. [Google Scholar] [CrossRef]
- Yadav, R.; Gupta, S.; Malhotra, A.K. A cross sectional study on depression, anxiety and their associated factors among medical students in Jhansi, Uttar Pradesh, India. Int. J. Community Med. Public Health 2016, 3, 1209–1214. [Google Scholar] [CrossRef]
- Axelson, D.A.; Birmaher, B. Relation between anxiety and depressive disorders in childhood and adolescence. Depress. Anxiety 2001, 14, 67–78. [Google Scholar] [CrossRef]
- Ramón-Arbués, E.; Gea-Caballero, V.; Granada-López, J.M.; Juárez-Vela, R.; Pellicer-García, B.; Antón-Solanas, I. The prevalence of depression, anxiety and stress and their associated factors in college students. Int. J. Environ. Res. Public Health 2020, 17, 7001. [Google Scholar] [CrossRef]
- Gupta, P.B.K.A.; Ramakrishna, K. Prevalence of Depression and Anxiety Among Medical Students and House Staff During the COVID-19 Health-Care Crisis. Acad. Psychiatry 2021, 45, 575–580. [Google Scholar] [CrossRef]
- Ahad, A.; Chahar, P.; Haque, E.; Bey, A.; Jain, M.; Raja, W. Factors affecting the prevalence of stress, anxiety, and depression in undergraduate Indian dental students. J. Educ. Health Promot. 2021, 10, 266. [Google Scholar] [PubMed]
- Nebhinani, M.; Parihar, A.; Kumar, A.A.G.; Nebhinani, N.; Rani, R. COVID-19-induced anxiety and protective behaviour among nursing students: A survey from western India. J. Family Med. Prim. Care 2021, 10, 4483–4488. [Google Scholar] [CrossRef]
- Boolani, A.; Yager, C.; Reid, J.; Lackman, J.; Smith, M.L. Correlates of depressive mood among graduate-level allied health students: An exploratory study examining trait energy and fatigue. J. Am. Coll. Health 2021, 71, 1685–1695. [Google Scholar] [CrossRef]
- Adhikari, A.; Sujakhu, E.; GC, S.; Zoowa, S. Depression among Medical Students of a Medical College in Nepal during COVID-19 Pandemic: A Descriptive Cross-sectional Study. JNMA J. Nepal. Med. Assoc. 2021, 59, 645–648. [Google Scholar] [CrossRef]
- Adhikari, A.; Dutta, A.; Sapkota, S.; Chapagain, A.; Aryal, A.; Pradhan, A. Prevalence of poor mental health among medical students in Nepal: A cross-sectional study. BMC Med. Educ. 2017, 17, 232. [Google Scholar] [CrossRef]
- Shrestha, N.; Shrestha, N.; Khanal, S.; Dahal, S.; Lama, R.; Simkhada, P.; Pradhan, S.N. Prevalence of Depression among Medical Students of a Tertiary Care Teaching Hospital. JNMA J. Nepal. Med. Assoc. 2019, 57, 403–407. [Google Scholar] [CrossRef]
- Nezam, S.; Golwara, A.K.; Jha, P.C.; Khan, S.A.; Singh, S.; Tanwar, A.S. Comparison of prevalence of depression among medical, dental, and engineering students in Patna using Beck’s Depression Inventory II: A cross-sectional study. J. Fam. Med. Prim. Care 2020, 9, 3005–3009. [Google Scholar]
- Bresolin, J.Z.; Dalmolin, G.d.L.; Vasconcellos, S.J.L.; Barlem, E.L.D.; Andolhe, R.; Magnago, T.S.B.S. Depressive symptoms among healthcare undergraduate students. Rev. Lat. Am. Enferm. 2020, 28, e3239. [Google Scholar] [CrossRef]
- Ramakrishnan, D.; Raghunathan, D.; Valsan, K.I.; Ambika, S. Prevalence of Depression among Students of a Dental Tertiary Care Center in Kerala. Indian J. Community Med. 2019, 44 (Suppl. S1), S14–S18. [Google Scholar] [CrossRef]
- Alves, J.V.d.S.; Paula, W.d.; Netto, P.R.R.; Godman, B.; Nascimento, R.C.R.M.d.; Coura-Vital, W. Prevalence and factors associated with anxiety among university students of health sciences in Brazil: Findings and implications. J. Bras. De Psiquiatr. 2021, 70, 99–107. [Google Scholar] [CrossRef]
- Yusof, N.S.M.; Zainal, Z.A.; Huri, H.Z.; Jacob, S.A.; Alwi, M.N.M.; Hassan, Y.; Ghazali, L.N. Prevalence of depression among undergraduate pharmacy students in Malaysia. Int. J. Pharm. Res. 2020, 12, 09752366. [Google Scholar]
- Basheti, I.A.; Mhaidat, Q.N.; Mhaidat, H.N. Prevalence of anxiety and depression during COVID-19 pandemic among healthcare students in Jordan and its effect on their learning process: A national survey. PLoS ONE 2021, 16, e0249716. [Google Scholar] [CrossRef]
- Meng, J.; Gao, C.; Tang, C.; Wang, H.; Tao, Z. Prevalence of hypochondriac symptoms among health science students in China: A systematic review and meta-analysis. PLoS ONE 2019, 14, e0222663. [Google Scholar] [CrossRef]
- Shaffique, S.; Farooq, S.S.; Anwar, H.; Asif, H.M.; Akram, M.; Jung, S.K. Meta-analysis of prevalence of depression, anxiety and stress among University Students. RADS J. Biol. Res. Appl. Sci. 2020, 11, 27–32. [Google Scholar] [CrossRef]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Straus, S.E. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef]
- Arksey, H.; O’Malley, L. Scoping studies: Towards a methodological framework. Int. J. Soc. Res. Methodol. 2005, 8, 19–32. [Google Scholar] [CrossRef]
- Munn, Z.; Peters, M.D.J.; Stern, C.; Tufanaru, C.; McArthur, A.; Aromataris, E. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med. Res. Methodol. 2018, 18, 143. [Google Scholar] [CrossRef]
- Covidence. Covidence: Better Systematic Review Management. 2020. Available online: https://www.covidence.org/ (accessed on 8 March 2022).
- Al-Maashani, M.; Al-Balushi, N.; Al-Alawi, M.; Mirza, H.; Al-Huseini, S.; Al-Balushi, M.; Obeid, Y.; Jose, S.; Al-Sibani, N.; Al-Adawi, S. Prevalence and Correlates of Depressive Symptoms among Medical Students: A Cross-sectional Single-centre Study. East Asian Arch. Psychiatry 2020, 30, 28–31. [Google Scholar] [CrossRef]
- Albajjar, M.A.; Bakarman, M.A. Prevalence and correlates of depression among male medical students and interns in Albaha University, Saudi Arabia. J. Fam. Med. Prim. Care 2019, 8, 1889–1894. [Google Scholar]
- AlShamlan, N.A.; AlShamlan, R.A.; AlShamlan, A.A.; AlOmar, R.S.; AlAmer, N.A.; Darwish, M.A.; Sebiany, A.M. Prevalence of depression and its associated factors among clinical-year medical students in Eastern Province, Saudi Arabia. Postgrad Med. J. 2020, 96, 343–348. [Google Scholar] [CrossRef]
- Alkhamees, A.A.; Alaqil, N.S.; Alsoghayer, A.S.; Alharbi, B.A. Prevalence and determinants of burnout syndrome and depression among medical students at Qassim University, Saudi Arabia. Saudi Med. J. 2020, 41, 1375–1380. [Google Scholar] [CrossRef]
- Azad, N.; Shahid, A.; Abbas, N.; Shaheen, A.; Munir, N. Anxiety and Depression in Medical Students of a Private Medical College. J. Ayub Med. Coll. Abbottabad 2017, 29, 123–127. [Google Scholar] [PubMed]
- Azim, S.R.; Baig, M. Frequency and perceived causes of depression, anxiety and stress among medical students of a private medical institute in Karachi: A mixed method study. J. Pak. Med. Assoc. 2019, 69, 840–845. [Google Scholar] [PubMed]
- Aluh, D.O.; Abba, A.; Afosi, A.B. Prevalence and correlates of depression, anxiety and stress among undergraduate pharmacy students in Nigeria. Pharm. Educ. 2020, 20, 236–248. [Google Scholar] [CrossRef]
- Bertani, D.E.; Mattei, G.; Ferrari, S.; Pingani, L.; Galeazzi, G.M. Anxiety, depression and personality traits in Italian medical students. Riv. Psichiatr. 2020, 55, 342–348. [Google Scholar] [PubMed]
- Basudan, S.; Binanzan, N.; Alhassan, A. Depression, anxiety and stress in dental students. Int. J. Med. Educ. 2017, 8, 179–186. [Google Scholar] [CrossRef]
- Bert, F.; Moro, G.L.; Corradi, A.; Acampora, A.; Agodi, A.; Brunelli, L.; Chironna, M.; Cocchio, S.; Cofini, V.; D’errico, M.M.; et al. Prevalence of depressive symptoms among Italian medical students: The multicentre cross-sectional “PRIMES” study. PLoS ONE 2020, 15, e0231845. [Google Scholar] [CrossRef]
- Biswas, M.; Al Jubayer, A.; Hasan, M.T.; Samir, N.; Alin, S.I.; Homaira, N.; Khatun, M.R.; Anjum, A. The Prevalence and Associated Factors of Depressive Symptoms Among Medical Students in Bangladesh During the COVID-19 Pandemic: A Cross-Sectional Pilot Study. Front. Public Health 2022, 9, 811345. [Google Scholar] [CrossRef]
- Coelho, L.D.S.; Tony, A.C.C.; Laguardia, G.C.A.; Santos, K.B.D.; Friedrich, D.B.C.; Cavalcante, R.B. Are symptoms of depression and anxiety in nursing students associated with their sociodemographic characteristics? Rev. Bras. Enferm. 2021, 74 (Suppl. S3), e20200503. [Google Scholar] [CrossRef]
- Çelik, N.; Ceylan, B.; Ünsal, A.; Çağan, Ö. Depression in health college students: Relationship factors and sleep quality. Psychol. Health Med. 2019, 24, 625–630. [Google Scholar] [CrossRef]
- Elsawy, W.I.H.; Sherif, A.A.R.; Attia, M.S.E.D.; El-Nimr, N.A. Depression among medical students in Alexandria, Egypt. Afr. Health Sci. 2020, 20, 1416–1425. [Google Scholar] [CrossRef]
- Falade, J.; Oyebanji, A.H.; Babatola, A.O.; Falade, O.O.; Olumuyiwa, T.O. Prevalence and correlates of psychiatric morbidity, comorbid anxiety and depression among medical students in public and private tertiary institutions in a Nigerian state: A cross-sectional analytical study. Pan. Afr. Med. J. 2020, 37, 53. [Google Scholar] [CrossRef]
- Fitzpatrick, O.; Biesma, R.; Conroy, R.M.; McGarvey, A. Prevalence and relationship between burnout and depression in our future doctors: A cross-sectional study in a cohort of preclinical and clinical medical students in Ireland. BMJ Open 2019, 9, e023297. [Google Scholar] [CrossRef]
- Fawzy, M.; Hamed, S.A. Prevalence of psychological stress, depression and anxiety among medical students in Egypt. Psychiatry Res. 2017, 255, 186–194. [Google Scholar] [CrossRef]
- Gan, G.G.; Yuen Ling, H. Anxiety, depression and quality of life of medical students in Malaysia. Med. J. Malays. 2019, 74, 57–61. [Google Scholar]
- Hoying, J.; Melnyk, B.M.; Hutson, E.; Tan, A. Prevalence and correlates of depression, anxiety, stress, healthy beliefs, and lifestyle behaviors in first-year graduate health sciences students. Worldviews Evid. Based Nurs. 2020, 17, 49–59. [Google Scholar] [CrossRef]
- Hanoon, Y.; Habib, H. Assessment of depressive symptoms among students at Al-Kindy College of Medicine in Baghdad. Fam. Med. Prim. Care Rev. 2021, 23, 307–312. [Google Scholar] [CrossRef]
- Junaid, M.A.L.; Auf, A.I.; Shaikh, K.; Khan, N.; Abdelrahim, S.A. Correlation between Academic Performance and Anxiety in Medical Students of Majmaah University–KSA. JPMA 2020, 2020, 865–868. [Google Scholar] [CrossRef]
- Khoshhal, K.I.; Khairy, G.A.; Guraya, S.Y.; Guraya, S.S. Exam anxiety in the undergraduate medical students of Taibah University. Med. Teach. 2017, 39 (Suppl. S1), S22–S26. [Google Scholar] [CrossRef]
- Kathem, S.H.; Al-Jumail, A.A.; Noor-Aldeen, M.; Najah, N.; Khalid, D.A. Measuring depression and anxiety prevalence among Iraqi healthcare college students using hospital anxiety and depression scale. Pharm. Pract. 2021, 19, 2303. [Google Scholar] [CrossRef]
- Kumar, S.G.; Kattimani, S.; Sarkar, S.; Kar, S.S. Prevalence of depression and its relation to stress level among medical students in Puducherry, India. Ind. Psychiatry J. 2017, 26, 86–90. [Google Scholar] [CrossRef]
- Killinger, S.L.; Flanagan, S.; Castine, E.; Howard, K.A. Stress and Depression among Veterinary Medical Students. J. Vet. Med. Educ. 2017, 44, 3–8. [Google Scholar] [CrossRef]
- Kupcewicz, E.; Mikla, M.; Kadučáková, H.; Grochans, E.; Valcarcel, M.D.R.; Cybulska, A.M. Correlation between Positive Orientation and Control of Anger, Anxiety and Depression in Nursing Students in Poland, Spain and Slovakia during the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2022, 19, 2482. [Google Scholar] [CrossRef]
- Kebede, M.A.; Anbessie, B.; Ayano, G. Prevalence and predictors of depression and anxiety among medical students in Addis Ababa, Ethiopia. Int. J. Ment. Health Syst. 2019, 13, 30. [Google Scholar] [CrossRef]
- Kumar, B.; Shah, M.A.A.; Kumari, R.; Kumar, A.; Kumar, J.; Tahir, A. Depression, Anxiety, and Stress Among Final-year Medical Students. Cureus 2019, 11, e4257. [Google Scholar] [CrossRef]
- Lee, C.M.; Juarez, M.; Rae, G.; Jones, L.; Rodriguez, R.M.; Davis, J.A.; Boysen-Osborn, M.; Kashima, K.J.; Krane, N.K.; Kman, N.; et al. Anxiety, PTSD, and stressors in medical students during the initial peak of the COVID-19 pandemic. PLoS ONE 2021, 16, e0255013. [Google Scholar] [CrossRef]
- López, R.B.; Navarro, N.M.; Astorga, A.C. Relationship between personality organization and the prevalence of symptoms of depression, anxiety and stress among university students in health careers in the Region of Coquimbo, Chile. Rev. Colomb. Psiquiatr. 2017, 46, 203–208. [Google Scholar] [CrossRef]
- Lu, L.; Wang, X.; Wang, X.; Guo, X.; Pan, B. Association of Covid-19 pandemic-related stress and depressive symptoms among international medical students. BMC Psychiatry 2022, 22, 20. [Google Scholar] [CrossRef]
- Milić, J.; Škrlec, I.; Milić Vranješ, I.; Podgornjak, M.; Heffer, M. High levels of depression and anxiety among Croatian medical and nursing students and the correlation between subjective happiness and personality traits. Int. Rev. Psychiatry 2019, 31, 653–660. [Google Scholar] [CrossRef]
- Melaku, L.; Bulcha, G.; Worku, D. The prevalence and severity of depression, anxiety, and stress among medical undergraduate students of Arsi University and their association with substance use, Southeast Ethiopia. Educ. Res. Int. 2021, 2021, 1–12. [Google Scholar] [CrossRef]
- Mirza, A.A.; Milaat, W.A.; Ramadan, I.K.; Baig, M.; Elmorsy, S.A.; Beyari, G.M.; Halawani, M.A.; Azab, R.A.; Zahrani, M.T.; Khayat, N.K. Depression, anxiety and stress among medical and non-medical students in Saudi Arabia: An epidemiological comparative cross-sectional study. Neurosciences 2021, 26, 141–151. [Google Scholar] [CrossRef]
- Mahroon, Z.A.; Borgan, S.M.; Kamel, C.; Maddison, W.; Royston, M.; Donnellan, C. Factors Associated with Depression and Anxiety Symptoms Among Medical Students in Bahrain. Acad. Psychiatry 2018, 42, 31–40. [Google Scholar] [CrossRef]
- Nakhostin-Ansari, A.; Sherafati, A.; Aghajani, F.; Khonji, M.S.; Aghajani, R.; Shahmansouri, N. Depression and Anxiety among Iranian Medical Students during COVID-19 Pandemic. Iran. J. Psychiatry 2020, 15, 228–235. [Google Scholar] [CrossRef]
- Fata Nahas, A.R.M.; Elkalmi, R.M.; Al-Shami, A.M.; Elsayed, T.M. Prevalence of Depression Among Health Sciences Students: Findings From a Public University in Malaysia. J. Pharm. Bioallied Sci. 2019, 11, 170–175. [Google Scholar] [CrossRef]
- Nahar, V.K.; Davis, R.E.; Dunn, C.; Layman, B.; Johnson, E.C.; Dascanio, J.J.; Johnson, J.W.; Sharma, M. The prevalence and demographic correlates of stress, anxiety, and depression among veterinary students in the Southeastern United States. Res. Vet. Sci. 2019, 125, 370–373. [Google Scholar] [CrossRef]
- Otim, M.; Al Marzouqi, A.M.; Subu, M.; Damaj, N.; Al-Harbawi, S. Prevalence of Generalised Anxiety Disorders Among Clinical Training Students at the University of Sharjah. J. Multidiscip. Healthc. 2021, 14, 1863–1872. [Google Scholar] [CrossRef]
- Pokhrel, N.B.; Khadayat, R.; Tulachan, P. Depression, anxiety, and burnout among medical students and residents of a medical school in Nepal: A cross-sectional study. BMC Psychiatry 2020, 20, 298. [Google Scholar] [CrossRef]
- Pukas, L.; Rabkow, N.; Keuch, L.; Ehring, E.; Fuchs, S.; Stoevesandt, D.; Sapalidis, A.; Pelzer, A.; Rehnisch, C.; Watzke, S. Prevalence and predictive factors for depressive symptoms among medical students in Germany—A cross-sectional study. GMS J. Med. Educ. 2022, 39, Doc13. [Google Scholar]
- Pham, T.; Bui, L.; Nguyen, A.; Nguyen, B.; Tran, P.; Vu, P.; Dang, L. The prevalence of depression and associated risk factors among medical students: An untold story in Vietnam. PLoS ONE 2019, 14, e0221432. [Google Scholar] [CrossRef]
- Patelarou, A.; Mechili, E.A.; Galanis, P.; Zografakis-Sfakianakis, M.; Konstantinidis, T.; Saliaj, A.; Bucaj, J.; Alushi, E.; Carmona-Torres, J.M.; Cobo-Cuenca, A.I.; et al. Nursing students, mental health status during COVID-19 quarantine: Evidence from three European countries. J. Ment. Health 2021, 30, 164–169. [Google Scholar] [CrossRef]
- Patten, E.V.; Vaterlaus, J.M. Prevalence of Depression, Anxiety, and Stress in Undergraduate Dietetics Students. J. Nutr. Educ. Behav. 2021, 53, 67–74. [Google Scholar] [CrossRef]
- Risal, A.; Shikhrakar, S.; Mishra, S.; Kunwar, D.; Karki, E.; Shrestha, B.; Holen, A. Anxiety and Depression during COVID-19 Pandemic among Medical Students in Nepal. Kathmandu Univ. Med. J. (KUMJ) 2020, 18, 333–339. [Google Scholar] [CrossRef]
- Santangelo, O.E.; Provenzano, S.; Armetta, F.; Pesco, G.; Allegro, A.; Lampasona, M.; Pantaleo, L.; Terranova, A. Prevalence of depressive symptomatology among nursing students during the COVID-19 pandemic. Ann. Ig. 2022, 34, 227–235. [Google Scholar] [PubMed]
- Silva, V.; Costa, P.; Pereira, I.; Faria, R.; Salgueira, A.P.; Costa, M.J.; Sousa, N.; Cerqueira, J.J.; Morgado, P. Depression in medical students: Insights from a longitudinal study. BMC Med. Educ. 2017, 17, 184. [Google Scholar] [CrossRef]
- Umar, M.U.; Suraj, S.S.; Umar, B.I.; Gajida, A.U. Prevalence and factors associated with depression among medical students in Nigeria. Niger Postgrad Med. J. 2021, 28, 198–203. [Google Scholar] [CrossRef]
- Solanki, H.K.; Awasthi, S.; Kaur, A.; Pamei, G. Depression, its correlates and quality of life of undergraduate medical students in the Kumaon region of Uttarakhand state, India. Indian J. Community Health 2021, 33, 357–363. [Google Scholar] [CrossRef]
- Tayefi, B.; Eftekhar, M.; Tayefi, M.; Darroudi, S.; Khalili, N.; Mottaghi, A.; Shanjani, Z.H.; Nojomi, M. Prevalence and Socio-Demographic Correlates of Mental Health Problems Among Iranian Health Sciences Students. Acad. Psychiatry 2020, 44, 73–77. [Google Scholar] [CrossRef]
- Bahçecioğlu Turan, G.; Özer, Z.; Çiftçi, B. Analysis of anxiety levels and attitudes of nursing students toward the nursing profession during the COVID-19 pandemic. Perspect. Psychiatr. Care 2021, 57, 1913–1921. [Google Scholar] [CrossRef]
- Van Venrooij, L.T.; Barnhoorn, P.C.; Giltay, E.J.; van Noorden, M.S. Burnout, depression and anxiety in preclinical medical students: A cross-sectional survey. Int. J. Adolesc. Med. Health 2017, 29, 20170077. [Google Scholar] [CrossRef]
- Van der Walt, S.; Mabaso, W.S.; Davids, E.L.; De Vries, P.J. The burden of depression and anxiety among medical students in South Africa: A cross-sectional survey at the University of Cape Town. South Afr. Med. J. 2020, 110, 69–79. [Google Scholar] [CrossRef]
- Yuan, L.L.; Lu, L.; Wang, X.H.; Guo, X.X.; Ren, H.; Gao, Y.Q.; Pan, B.-C. Prevalence and Predictors of Anxiety and Depressive Symptoms Among International Medical Students in China During COVID-19 Pandemic. Front. Psychiatry 2021, 12, 761964. [Google Scholar] [CrossRef]
- Zakeri, M.; De La Cruz, A.; Wallace, D.; Sansgiry, S.S. General Anxiety, Academic Distress, and Family Distress Among Doctor of Pharmacy Students. Am. J. Pharm. Educ. 2021, 85, 8522. [Google Scholar] [CrossRef]
- Zeng, Y.; Wang, G.; Xie, C.; Hu, X.; Reinhardt, J.D. Prevalence and correlates of depression, anxiety and symptoms of stress in vocational college nursing students from Sichuan, China: A cross-sectional study. Psychol. Health Med. 2019, 24, 798–811. [Google Scholar] [CrossRef]
- Iqbal, S.; Gupta, S.; Venkatarao, E. Stress, anxiety and depression among medical undergraduate students and their socio-demographic correlates. Indian J. Med. Res. 2015, 141, 354–357. [Google Scholar] [PubMed]
- Tian-Ci Quek, T.; Wai-San Tam, W.X.; Tran, B.; Zhang, M.; Zhang, Z.; Su-Hui Ho, C.; Chun-Man Ho, R. The global prevalence of anxiety among medical students: A meta-analysis. Int. J. Environ. Res. Public Health 2019, 16, 2735. [Google Scholar] [CrossRef]
- Gradus, J.L. Epidemiology of PTSD; National Center for PTSD (United States Department of Veterans Affairs): White River Junction, VT, USA, 2007. [Google Scholar]
- Agyapong, B.; Obuobi-Donkor, G.; Burback, L.; Wei, Y. Stress, Burnout, Anxiety and Depression among Teachers: A Scoping Review. Int. J. Environ. Res. Public Health 2022, 19, 10706. [Google Scholar] [CrossRef]
- Catuzzi, J.E.; Beck, K.D. Anxiety vulnerability in women: A two-hit hypothesis. Exp. Neurol. 2014, 259, 75–80. [Google Scholar] [CrossRef]
- Parker, G.; Brotchie, H. Gender differences in depression. Int. Rev. Psychiatry 2010, 22, 429–436. [Google Scholar] [CrossRef]
- Chang, J.J.; Ji, Y.; Li, Y.H.; Pan, H.F.; Su, P.Y. Prevalence of anxiety symptom and depressive symptom among college students during COVID-19 pandemic: A meta-analysis. J. Affect. Disord. 2021, 292, 242–254. [Google Scholar] [CrossRef]
- Gorman, J.M. Gender differences in depression and response to psychotropic medication. Gend. Med. 2006, 3, 93–109. [Google Scholar] [CrossRef]
- Serpytis, P.; Navickas, P.; Lukaviciute, L.; Navickas, A.; Aranauskas, R.; Serpytis, R.; Deksnyte, A.; Glaveckaite, S.; Petrulioniene, Z.; Samalavicius, R. Gender-Based Differences in Anxiety and Depression Following Acute Myocardial Infarction. Arq. Bras. Cardiol. 2018, 111, 676–683. [Google Scholar] [CrossRef]
- Moustafa, A.A.; Tindle, R.; Frydecka, D.; Misiak, B. Impulsivity and its relationship with anxiety, depression and stress. Compr. Psychiatry 2017, 74, 173–179. [Google Scholar] [CrossRef]
- Bertolote, J.M. Preventing Suicide a Resource for General Physicians; Health DoM, Ed.; World Health Organization: Geneva, Switzerland, 2020. [Google Scholar]
- Liu, C.H.; Stevens, C.; Wong, S.H.M.; Yasui, M.; Chen, J.A. The prevalence and predictors of mental health diagnoses and suicide among U.S. college students: Implications for addressing disparities in service use. Depress. Anxiety 2019, 36, 8–17. [Google Scholar] [CrossRef]
- Pires, G.N.; Bezerra, A.G.; Tufik, S.; Andersen, M.L. Effects of acute sleep deprivation on state anxiety levels: A systematic review and meta-analysis. Sleep Med. 2016, 24, 109–118. [Google Scholar] [CrossRef]
- Mathew, A.R.; Hogarth, L.; Leventhal, A.M.; Cook, J.W.; Hitsman, B. Cigarette smoking and depression comorbidity: Systematic review and proposed theoretical model. Addiction 2017, 112, 401–412. [Google Scholar] [CrossRef]
- Shaukat, N.; Ali, D.M.; Razzak, J. Physical and mental health impacts of COVID-19 on healthcare workers: A scoping review. Int. J. Emerg. Med. 2020, 13, 40. [Google Scholar] [CrossRef]
- Agyapong, B.; Shalaby, R.; Wei, Y.; Agyapong, V.I. Can ResilienceNhope, an evidence-based text and email messaging innovative suite of program help to close the psychological treatment and mental health literacy gaps in college students? Front. Public Health 2022, 10, 890131. [Google Scholar] [CrossRef]
- Agyapong, B.; Brett-MacLean, P.; Burback, L.; Agyapong, V.I.O.; Wei, Y. Interventions to Reduce Stress and Burnout among Teachers: A Scoping Review. Int. J. Environ. Res. Public Health 2023, 20, 5625. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).