Resilience in Mild Cognitive Impairment (MCI): Examining the Level and the Associations of Resilience with Subjective Wellbeing and Negative Affect in Early and Late-Stage MCI
Abstract
1. Introduction
1.1. Mild Cognitive Impairment
1.2. Psychological Resilience
1.3. Resilience and Subjective Wellbeing in Older Adults
1.4. Resilience and Negative Psychological Outcomes in Older Adults
1.5. Aim and Hypotheses of the Study
2. Methods
2.1. Participants
2.2. Procedure
2.3. Ethics
2.4. Measures
2.4.1. Screening Tests
MoCA
Doors and People: Subtest Shapes
2.4.2. Main Research Tools
Brief Resilience Scale
The PERMA Profiler
DASS-21
Demographic Variables
2.5. Statistics
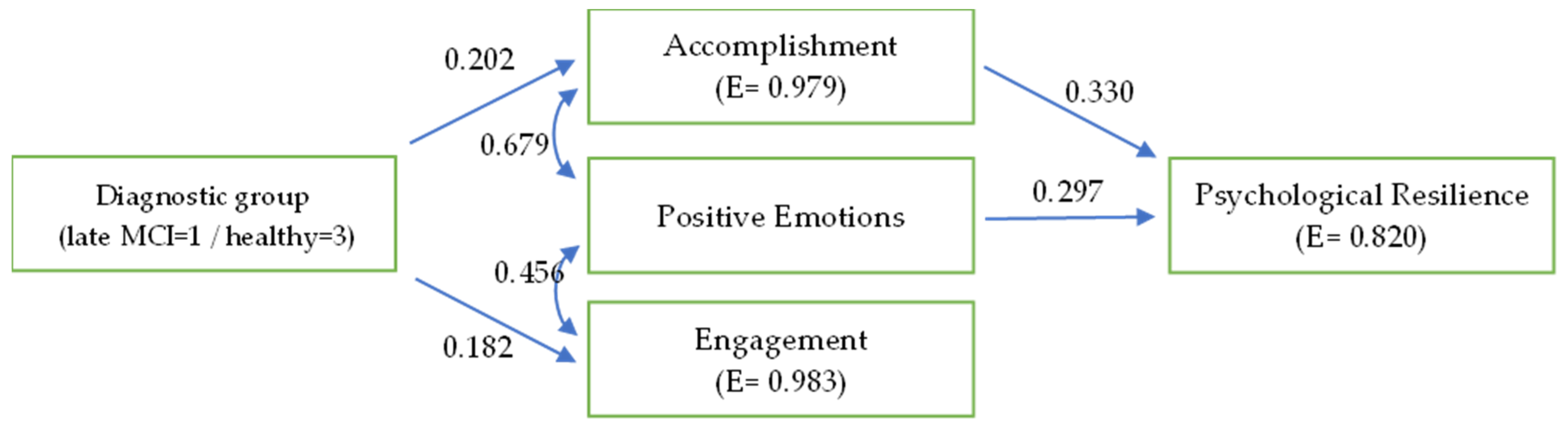
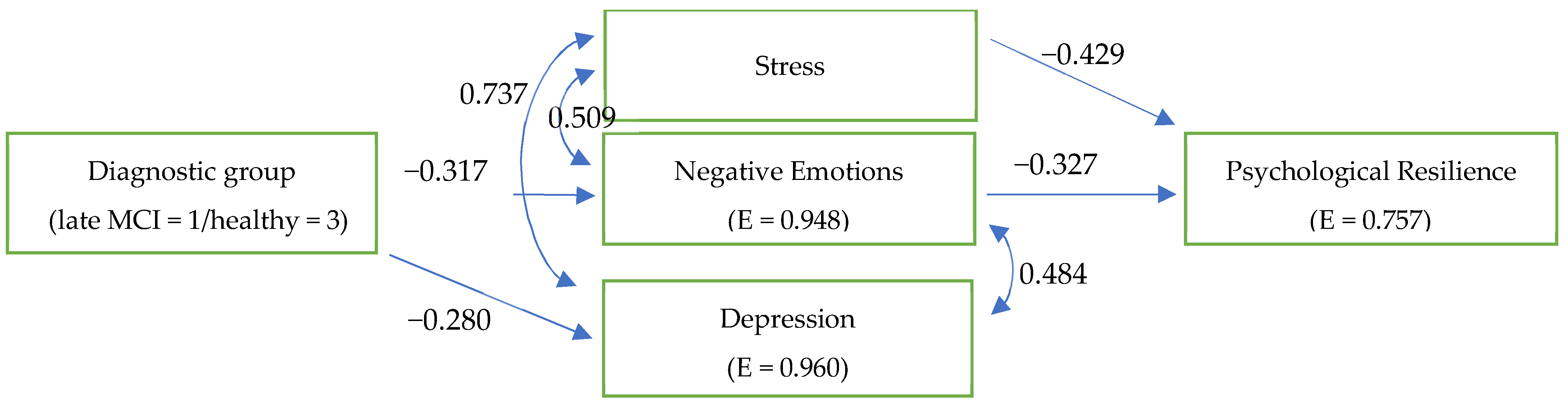
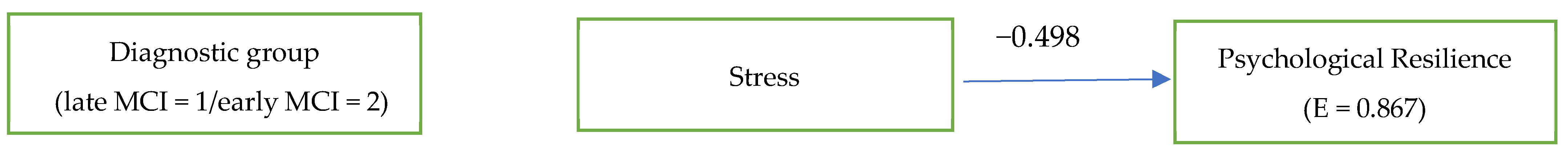
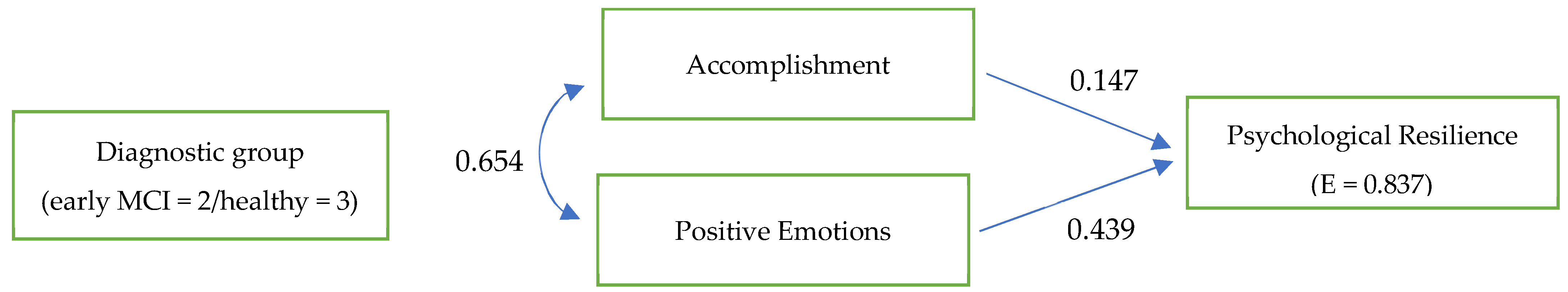
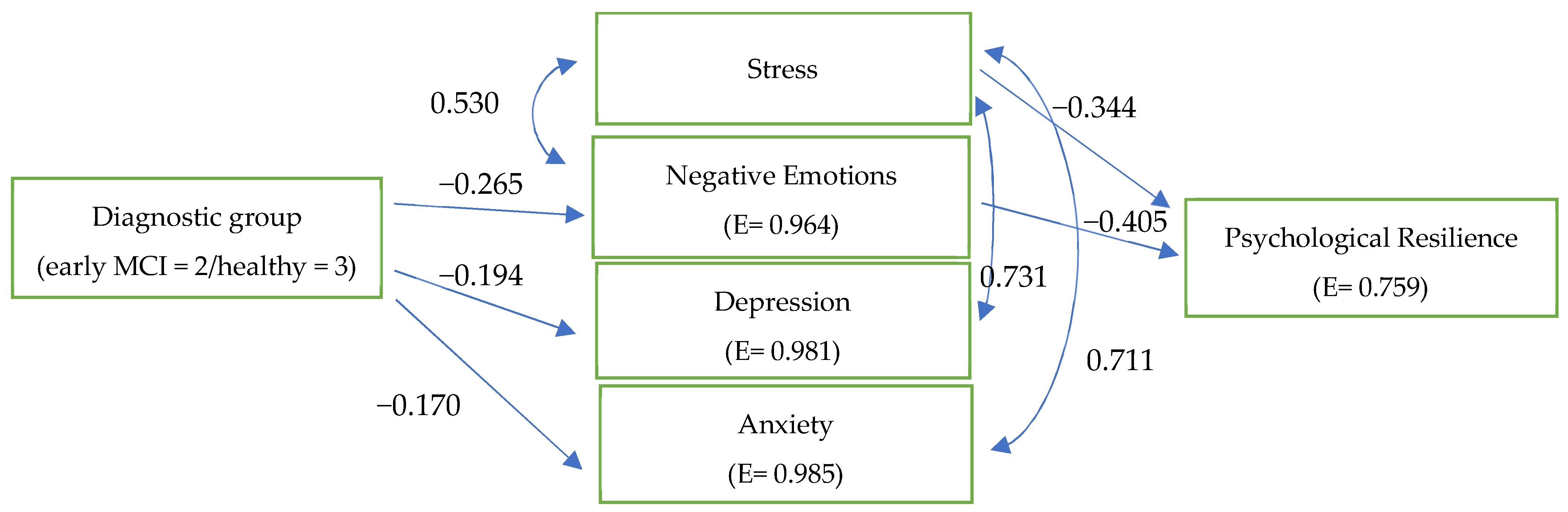
3. Results
4. Discussion
5. Implications
6. Limitations
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Gauthier, S.; Reisberg, B.; Zaudig, M.; Petersen, R.C.; Ritchie, K.; Broich, K.; Belleville, S.; Brodaty, H.; Bennett, D.A.; Chertkow, H.; et al. Mild Cognitive Impairment. Lancet 2006, 367, 1262–1270. [Google Scholar] [CrossRef] [PubMed]
- Libon, D.J.; Drabick, D.A.G.; Giovannetti, T.; Price, C.C.; Bondi, M.W.; Eppig, J.S.; Devlin, K.N.; Nieves, C.; Lamar, M.; Delano-Wood, L.; et al. Neuropsychological Syndromes Associated with Alzheimer’s/Vascular Dementia: A Latent Class Analysis. J. Alzheimer’s Dis. 2014, 42, 999–1014. [Google Scholar] [CrossRef] [PubMed]
- American Psychiatric Association; Washington American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Association: Washington, DC, USA, 2013. [Google Scholar]
- Rapp, S.R.; Legault, C.; Henderson, V.W.; Brunner, R.L.; Masaki, K.; Jones, B.N.; Absher, J.R.; Thal, L.J. Subtypes of Mild Cognitive Impairment in Older Postmenopausal Women. Alzheimer Dis. Assoc. Disord. 2010, 24, 248–255. [Google Scholar] [CrossRef]
- Petersen, R.C.; Smith, G.E.; Waring, S.C.; Ivnik, R.J.; Tangalos, E.G.; Kokmen, E. Mild Cognitive Impairment. Arch. Neurol. 1999, 56, 303. [Google Scholar] [CrossRef] [PubMed]
- What is Resilience? Available online: http://psychcentral.com/lib/what-is-resilience/0001145 (accessed on 20 February 2023).
- Vella, S.-L.; Pai, N.B. A Theoretical Review of Psychological Resilience: Defining Resilience and Resilience Research over the Decades. Arch. Med. Health Sci. 2019, 7, 233. [Google Scholar] [CrossRef]
- Garmezy, N.; Masten, A.S.; Tellegen, A. The study of stress and competence in children: A building block for developmental psychopathology. Child Dev. 1984, 55, 97–111. [Google Scholar] [CrossRef]
- Garmezy, N. Resiliency and vulnerability to adverse developmental outcomes associated with poverty. Am. Behav. Sci. 1991, 34, 416–430. [Google Scholar] [CrossRef]
- Rutter, M. Resilience in the Face of Adversity. Br. J. Psychiatry 1985, 147, 598–611. [Google Scholar] [CrossRef]
- Luthar, S.S.; Cicchetti, D.; Becker, B.E. The Construct of Resilience: A Critical Evaluation and Guidelines for Future Work. Child Dev. 2000, 71, 543–562. [Google Scholar] [CrossRef]
- Garmezy, N.; Streitman, S. Children at risk: The search for the antecedents of schizophrenia: I. Conceptual models and research methods. Schizophr. Bull. 1974, 1, 14–90. [Google Scholar] [CrossRef][Green Version]
- Rutter, M. Psychosocial resilience and protective mechanisms. Am. J. Orthopsychiatry 1987, 57, 316–331. [Google Scholar] [CrossRef]
- Luthar, S.S.; Zelazo, L.B. Research on Resilience: An Integrative Review. In Resilience and Vulnerability: Adaptation in the Context of Childhood Adversities; Luthar, S.S., Ed.; Cambridge University Press: Cambridge, UK, 2003; pp. 510–550. [Google Scholar] [CrossRef]
- Masten, A.S.; Powell, J.L. A Resilience Framework for Research, Policy, and Practice. In Resilience and Vulnerability: Adaptation in the Context of Childhood Adversities; Luthar, S.S., Ed.; Cambridge University Press: Cambridge, UK, 2003; pp. 1–26. [Google Scholar] [CrossRef]
- McLaughlin, K.A.; Sheridan, M.A.; Lambert, H.K. Childhood Adversity and Neural Development: Deprivation and Threat as Distinct Dimensions of Early Experience. Neurosci. Biobehav. Rev. 2014, 47, 578–591. [Google Scholar] [CrossRef]
- McLaughlin, K.A.; Colich, N.L.; Rodman, A.M.; Weissman, D.G. Mechanisms Linking Childhood Trauma Exposure and Psychopathology: A Transdiagnostic Model of Risk and Resilience. BMC Med. 2020, 18, 96. [Google Scholar] [CrossRef] [PubMed]
- Gee, D.G. Early Adversity and Development: Parsing Heterogeneity and Identifying Pathways of Risk and Resilience. Am. J. Psychiatry 2021, 178, 998–1013. [Google Scholar] [CrossRef]
- Kalisch, R.; Cramer, A.O.J.; Binder, H.; Fritz, J.; Leertouwer, I.; Lunansky, G.; Meyer, B.; Timmer, J.; Veer, I.M.; Van Harmelen, A.-L. Deconstructing and Reconstructing Resilience: A Dynamic Network Approach. Perspect. Psychol. Sci. 2019, 14, 765–777. [Google Scholar] [CrossRef] [PubMed]
- United Nations Department of Economic and Social Affairs. World Population Ageing 2020. Highlights; United Nations Department of Economic and Social Affairs: New York, NY, USA, 2021. [Google Scholar] [CrossRef]
- Seligman, M.E.P. Flourish: A Visionary New Understanding of Happiness and Well-Being. Choice Rev. Online 2011, 48, 48–7217. [Google Scholar] [CrossRef]
- Bergman, M.E. The Relationship between Affective and Normative Commitment: Review and Research Agenda. J. Organ. Behav. 2006, 27, 645–663. [Google Scholar] [CrossRef]
- Knight, M.; Seymour, T.L.; Gaunt, J.T.; Baker, C.M.; Nesmith, K.; Mather, M. Aging and Goal-Directed Emotional Attention: Distraction Reverses Emotional Biases. Emotion 2007, 7, 705–714. [Google Scholar] [CrossRef]
- Sims, T.; Carstensen, L.L. The Elusiveness of a Life-Span Model of Emotion Regulation. ISSBD Bull. 2014, 38, 30–32. [Google Scholar]
- Wilson, D.; Watanabe, S.; Milner, H.V.; Ainge, J.A. Lateral Entorhinal Cortex Is Necessary for Associative but Not Non-associative Recognition Memory. Hippocampus 2013, 23, 1280–1290. [Google Scholar] [CrossRef]
- Butler, J.M.; Kern, M.L. The PERMA-Profiler: A Brief Multidimensional Measure of Flourishing. Int. J. Wellbeing 2016, 6, 1–48. [Google Scholar] [CrossRef]
- Waterworth, S.; Raphael, D.; Gott, M.; Arroll, B.; Jarden, A. Uncovering Strengths within Community Dwelling Older Adults: What Does It Mean for Health Care Practice? Health Soc. Care Community 2020, 28, 932–940. [Google Scholar] [CrossRef] [PubMed]
- Ionescu, T. The Variability-Stability-Flexibility Pattern: A Possible Key to Understanding the Flexibility of the Human Mind. Rev. Gen. Psychol. 2017, 21, 123–131. [Google Scholar] [CrossRef]
- Camitan, D.S.; Bajin, L.N. The Importance of Well-Being on Resiliency of Filipino Adults During the COVID-19 Enhanced Community Quarantine: A Necessary Condition Analysis. Front. Psychol. 2021, 12, 908. [Google Scholar] [CrossRef]
- Csikszentmihalyi, M. Flow. In The Encyclopedia of Positive Psychology; Lopez, S., Ed.; Chichester Blackwell Publishing Ltd.: Hoboken, NJ, USA, 2009; pp. 394–400. Available online: https://www.scirp.org/(S(i43dyn45teexjx455qlt3d2q))/reference/ReferencesPapers.aspx?ReferenceID=2335789 (accessed on 3 March 2023).
- McFadden, S.H.; Basting, A. Healthy Aging Persons and Their Brains: Promoting Resilience Through Creative Engagement. Clin. Geriatr. Med. 2010, 26, 149–161. [Google Scholar] [CrossRef]
- Hardy, J.; Selkoe, D.J. The Amyloid Hypothesis of Alzheimer’s Disease: Progress and Problems on the Road to Therapeutics. Science 2002, 297, 353–356. [Google Scholar] [CrossRef] [PubMed]
- Waugh, C.E.; Koster, E.H.W. A Resilience Framework for Promoting Stable Remission from Depression. Clin. Psychol. Rev. 2015, 41, 49–60. [Google Scholar] [CrossRef]
- Chmitorz, A.; Kunzler, A.; Helmreich, I.; Tüscher, O.; Kalisch, R.; Kubiak, T.; Wessa, M.; Lieb, K.P. Intervention Studies to Foster Resilience—A Systematic Review and Proposal for a Resilience Framework in Future Intervention Studies. Clin. Psychol. Rev. 2018, 59, 78–100. [Google Scholar] [CrossRef] [PubMed]
- Singh, K.; Yu, X. Psychometric Evaluation of the Connor-Davidson Resilience Scale (CD-RISC) in a Sample of Indian Students. J. Psychol. 2010, 1, 23–30. [Google Scholar] [CrossRef]
- Raue, P.J.; McGovern, A.; Kiosses, D.N.; Sirey, J.A. Advances in Psychotherapy for Depressed Older Adults. Curr. Psychiatry Rep. 2017, 19. [Google Scholar] [CrossRef]
- Ma, L. Depression, Anxiety, and Apathy in Mild Cognitive Impairment: Current Perspectives. Front. Aging Neurosci. 2020, 12, 9. [Google Scholar] [CrossRef] [PubMed]
- Palmer, K.T.; Berger, A.; Monastero, R.; Winblad, B.; Bäckman, L.; Fratiglioni, L. Predictors of Progression from Mild Cognitive Impairment to Alzheimer Disease. Neurology 2007, 68, 1596–1602. [Google Scholar] [CrossRef] [PubMed]
- Potvin, O.; Hudon, C.; Dion, M.; Grenier, S.; Préville, M. Anxiety Disorders, Depressive Episodes and Cognitive Impairment No Dementia in Community-Dwelling Older Men and Women. Int. J. Geriatr. Psychiatry 2010, 26, 1080–1088. [Google Scholar] [CrossRef]
- Rozzini, L.; Chilovi, B.V.; Conti, M.; Delrio, I.; Borroni, B.; Trabucchi, M.; Padovani, A. Neuropsychiatric Symptoms in Amnestic and Nonamnestic Mild Cognitive Impairment. Dement. Geriatr. Cogn. Disord. 2007, 25, 32–36. [Google Scholar] [CrossRef] [PubMed]
- Allen, A.E.; Kennedy, P.J.; Cryan, J.F.; Dinan, T.G.; Clarke, G. Biological and Psychological Markers of Stress in Humans: Focus on the Trier Social Stress Test. Neurosci. Biobehav. Rev. 2014, 38, 94–124. [Google Scholar] [CrossRef]
- McEwen, B.S. Central Effects of Stress Hormones in Health and Disease: Understanding the Protective and Damaging Effects of Stress and Stress Mediators. Eur. J. Pharmacol. 2008, 583, 174–185. [Google Scholar] [CrossRef] [PubMed]
- Jain, N.; Wang, Y.; Zhang, Y.; Jacobsen, E.; Andreescu, C.; Snitz, B.E.; Chang, C.-C.H.; Ganguli, M. It Goes Both Ways: The Relationship between Anxiety and Mild Cognitive Impairment. Int. J. Geriatr. Psychiatry 2023, 38, e5899. [Google Scholar] [CrossRef]
- Zapater-Fajarí, M.; Crespo-Sanmiguel, I.; Hidalgo, V.; Salvador, A. Resilience and Psychobiological Response to Stress in Older People: The Mediating Role of Coping Strategies. Front. Aging Neurosci. 2021, 13, 632141. [Google Scholar] [CrossRef]
- Keyes, C.L.M. The Mental Health Continuum: From Languishing to Flourishing in Life. J. Health Soc. Behav. 2002, 43, 207. [Google Scholar] [CrossRef]
- Nasreddine, Z.S.; Phillips, N.A.; Bédirian, V.; Charbonneau, S.; Whitehead, V.; Collin, I.; Cummings, J.L.; Chertkow, H. The Montreal Cognitive Assessment, MoCA: A Brief Screening Tool for Mild Cognitive Impairment. J. Am. Geriatr. Soc. 2005, 53, 695–699. [Google Scholar] [CrossRef]
- Poptsi, E.; Moraitou, D.; Eleftheriou, M.; Kounti-Zafeiropoulou, F.; Papasozomenou, C.; Agogiatou, C.; Bakoglidou, E.; Batsila, G.; Liapi, D.; Markou, N.; et al. Normative Data for the Montreal Cognitive Assessment in Greek Older Adults with Subjective Cognitive Decline, Mild Cognitive Impairment and Dementia. J. Geriatr. Psychiatry Neurol. 2019, 32, 265–274. [Google Scholar] [CrossRef] [PubMed]
- Kounti, F.; Tsolaki, M.; Kiosseoglou, G. Functional Cognitive Assessment Scale (FUCAS): A New Scale to Assess Executive Cognitive Function in Daily Life Activities in Patients with Dementia and Mild Cognitive Impairment. Hum. Psychopharmacol. -Clin. Exp. 2006, 21, 305–311. [Google Scholar] [CrossRef] [PubMed]
- Folstein, M.F.; Folstein, S.E.; McHugh, P.R. Mini-Mental State. J. Psychiatr. Res. 1975, 12, 189–198. [Google Scholar] [CrossRef] [PubMed]
- Fountoulakis, K.N.; Tsolaki, M.; Chantzi, H.; Kazis, A. Mini Mental State Examination (MMSE): A Validation Study in Greece. Am. J. Alzheimers Dis. Other Dement. 2000, 15, 342–345. [Google Scholar] [CrossRef]
- Reisberg, B.; Ferris, S.H.; de Leon, M.J.; Crook, T. The Global Deterioration Scale for assessment of primary degenerative dementia. Am. J. Psychiatry 1982, 139, 1136–1139. [Google Scholar] [CrossRef]
- Cummings, J.L.; Mega, M.S.; Gray, K.E.; Rosenberg-Thompson, S.; Carusi, D.; Gornbein, J. The Neuropsychiatric Inventory: Comprehensive Assessment of Psychopathology in Dementia. Neurology 1994, 44, 2308. [Google Scholar] [CrossRef]
- Politis, A.; Mayer, L.D.; Passa, M.; Maillis, A.; Lyketsos, C.G. Validity and Reliability of the Newly Translated Hellenic Neuropsychiatric Inventory(H-NPI) Applied to Greek Outpatients with Alzheimer’s Disease: A Study of Disturbing Behaviors among Referrals to a Memory Clinic. Int. J. Geriatr. Psychiatry 2004, 19, 203–208. [Google Scholar] [CrossRef]
- Yesavage, J.A.; Brink, T.L.; Rose, T.L.; Lum, O.; Huang, V.; Adey, M.; Leirer, V.O. Development and Validation of a Geriatric Depression Screening Scale: A Preliminary Report. J. Psychiatr. Res. 1982, 17, 37–49. [Google Scholar] [CrossRef]
- Fountoulakis, K.N.; Tsolaki, M.; Iacovides, A.; Yesavage, J.A.; O’Hara, R.; Kazis, A.; Ierodiakonou, C. The Validation of the Short Form of the Geriatric Depression Scale (GDS) in Greece. Aging Clin. Exp. Res. 1999, 11, 367–372. [Google Scholar] [CrossRef]
- Beck, A.T. An Inventory for Measuring Depression. Arch. Gen. Psychiatry 1961, 4, 561. [Google Scholar] [CrossRef]
- Sinoff, G.; Ore, L.; Zlotogorsky, D.; Tamir, A. Short Anxiety Screening Test—A brief instrument for detecting anxiety in the elderly. Int. J. Geriatr. Psychiatry 1999, 14, 1062–1071. [Google Scholar] [CrossRef]
- Grammatikopoulos, I.A.; Sinoff, G.; Alegakis, A.; Kounalakis, D.K.; Antonopoulou, M.; Lionis, C. The Short Anxiety Screening Test in Greek: Translation and Validation. Ann. Gen. Psychiatry 2010, 9, 1. [Google Scholar] [CrossRef] [PubMed]
- Beck, A.T.; Epstein, N.B.; Brown, G.C.; Steer, R.A. An Inventory for Measuring Clinical Anxiety: Psychometric Properties. J. Consult. Clin. Psychol. 1988, 56, 893–897. [Google Scholar] [CrossRef] [PubMed]
- Baddeley, A.D.; Hitch, G.J. Developments in the Concept of Working Memory. Neuropsychology 1994, 8, 485–493. [Google Scholar] [CrossRef]
- Chatzikostopoulos, A.; Moraitou, D.; Tsolaki, M.; Masoura, E.; Papantoniou, G.; Sofologi, M.; Papaliagkas, V.; Kougioumtzis, G.A.; Papatzikis, E. Episodic Memory in Amnestic Mild Cognitive Impairment (AMCI) and Alzheimer’s Disease Dementia (ADD): Using the “Doors and People” Tool to Differentiate between Early AMCI—Late AMCI—Mild ADD Diagnostic Groups. Diagnostics 2022, 12, 1768. [Google Scholar] [CrossRef]
- Kounti, F.; Tsolaki, M.; Eleftheriou, M.; Agogiatou, C.; Karagiozi, K.; Bakoglidou, E.; Nikolaides, E.; Nakou, S.; Poptsi, E.; Zafiropoulou, M.; et al. Administration of Montreal Cognitive Assessment (MoCA) test in Greek healthy elderly, patients with Mild Cognitive Impairment and patients with Dementia. In Proceedings of the European Conference on Psychological Assessment and 2th International Conference of the Psychological Society of Northern Greece, Thessaloniki, Greece, 5–7 May 2007. [Google Scholar]
- Bernstein, I.H.; Lacritz, L.H.; Barlow, C.E.; Weiner, M.F.; DeFina, L.F. Psychometric Evaluation of the Montreal Cognitive Assessment (MoCA) in Three Diverse Samples. Clin. Neuropsychol. 2010, 25, 119–126. [Google Scholar] [CrossRef]
- Zheng, L.; Teng, E.L.; Varma, R.; Mack, W.J.; Mungas, D.M.; Lu, P.H.; Chui, H.C. Chinese-Language Montreal Cognitive Assessment for Cantonese or Mandarin Speakers: Age, Education, and Gender Effects. Int. J. Alzheimer’s Dis. 2012, 2012, 204623. [Google Scholar] [CrossRef]
- De Freitas, S.M.S.F.; Simões, M.R.; Alves, L.; Vicente, M.; Santana, I. Montreal Cognitive Assessment (MoCA): Validation Study for Vascular Dementia. J. Int. Neuropsychol. Soc. 2012, 18, 1031–1040. [Google Scholar] [CrossRef]
- Hess, R.S.; D’Amato, R.C. Book Review: Doors and People: A Test of Visual and Verbal Recall and Recognition. J. Psychoeduc. Assess. 1999, 17, 175–180. [Google Scholar] [CrossRef]
- Arabatzi, X.; Masoura, E. Episodic Memory and Norms’ Development for the Battery “Doors and People” in the Greek Population; No. GRI-2021-9114; Aristotle University of Thessaloniki: Thessaloniki, Greece, 2012; Unpublished Dissertation. [Google Scholar]
- Smith, B.W.; Dalen, J.; Wiggins, K.J.; Tooley, E.M.; Christopher, P.J.; Bernard, J.F. The Brief Resilience Scale: Assessing the Ability to Bounce Back. Int. J. Behav. Med. 2008, 15, 194–200. [Google Scholar] [CrossRef]
- Amat, S.; Subhan, M.; Jaafar, W.M.W.; Mahmud, Z.; Johari, K.S.K. Evaluation and Psychometric Status of the Brief Resilience Scale in a Sample of Malaysian International Students. Asian Soc. Sci. 2014, 10, 240–245. [Google Scholar] [CrossRef]
- De Holanda Coelho, G.L.; Hanel, P.H.P.; Leal, T.C.; Rezende, A.T.; Gouveia, V.V. Brief Resilience Scale: Testing Its Factorial Structure and Invariance in Brazil. Univ. Psychol. 2016, 15, 397. [Google Scholar] [CrossRef]
- Rodríguez-Rey, R.; Alonso-Tapia, J.; Garrido-Hernansaiz, H. Reliability and Validity of the Brief Resilience Scale (BRS) Spanish Version. Psychol. Assess. 2016, 28, e101–e110. [Google Scholar] [CrossRef] [PubMed]
- Consten, C. Measuring Resilience with the Brief Resilience Scale: Factor Structure, Reliability and Validity of the Dutch Version of the BRS (BRSnl). Bachelor’s Thesis, University of Twente, Enschede, The Netherlands, 2016. Available online: http://essay.utwente.nl/70095/ (accessed on 13 March 2023).
- Stalikas, A.; Kyriazos, T.A. The Scale of Positive and Negative Experience (SPANE), Greek Version; Athens Hellenic Association of Positive Psychology: Athens, Greece, 2017; Available online: https://scirp.org/reference/referencespapers.aspx?referenceid=2326119 (accessed on 16 March 2023).
- Kyriazos, T.A.; Stalikas, A.; Prassa, K.; Galanakis, M.; Yotsidi, V.; Lakioti, A. Psychometric Evidence of the Brief Resilience Scale (BRS) and Modeling Distinctiveness of Resilience from Depression and Stress. Psychology 2018, 9, 1828–1857. [Google Scholar] [CrossRef]
- Pezirkianidis, C.; Stalikas, A.; Lakioti, A.; Yotsidi, V. Validating a Multidimensional Measure of Wellbeing in Greece: Translation, Factor Structure, and Measurement Invariance of the PERMA Profiler. Current Psychology 2019, 40, 3030–3047. [Google Scholar] [CrossRef]
- Lovibond, P.F.; Lovibond, S.H. The Structure of Negative Emotional States: Comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behav. Res. Ther. 1995, 33, 335–343. [Google Scholar] [CrossRef]
- Gloster, A.T.; Rhoades, H.M.; Novy, D.M.; Klotsche, J.; Senior, A.; Kunik, M.E.; Wilson, N.; Stanley, M.A. Psychometric Properties of the Depression Anxiety and Stress Scale-21 in Older Primary Care Patients. J. Affect. Disord. 2008, 110, 248–259. [Google Scholar] [CrossRef]
- Bottesi, G.; Ghisi, M.; Altoè, G.; Conforti, E.; Melli, G.; Sica, C. The Italian Version of the Depression Anxiety Stress Scales-21: Factor Structure and Psychometric Properties on Community and Clinical Samples. Compr. Psychiatry 2015, 60, 170–181. [Google Scholar] [CrossRef]
- Sinclair, S.J.; Siefert, C.J.; Slavin-Mulford, J.; Stein, M.B.; Renna, M.E.; Blais, M.A. Psychometric Evaluation and Normative Data for the Depression, Anxiety, and Stress Scales-21 (DASS-21) in a Nonclinical Sample of U.S. Adults. Eval. Health Prof. 2011, 35, 259–279. [Google Scholar] [CrossRef]
- Lyrakos, G.; Arvaniti, C.; Smyrnioti, M.-E.; Kostopanagiotou, G. Translation and Validation Study of the Depression Anxiety Stress Scale in the Greek General Population and in a Psychiatric Patient’s Sample. Eur. Psychiatry 2011, 26, 1731. [Google Scholar] [CrossRef]
- Pezirkianidis, C.; Karakasidou, E.; Lakioti, A.; Stalikas, A.; Galanakis, M. Psychometric Properties of the Depression, Anxiety, Stress Scales-21 (DASS-21) in a Greek Sample. Psychology 2018, 09, 2933–2950. [Google Scholar] [CrossRef]
- Bentler, P.M. EQS 6, Structural Equations Program Manual; Multivariate Software Inc.: Encino, CA, USA, 2006. [Google Scholar]
- Hu, L.-T.; Bentler, P.M. Cutoff Criteria for Fit Indexes in Covariance Structure Analysis: Conventional Criteria versus New Alternatives. Struct. Equ. Model. 1999, 6, 1–55. [Google Scholar] [CrossRef]
- Bollen, K.A. Overall Fit in Covariance Structure Models: Two Types of Sample Size Effects. Psychol. Bull. 1990, 107, 256–259. [Google Scholar] [CrossRef]
- Fredrickson, B.L. The role of Positive emotions in Positive Psychology: The Broaden-and-Build Theory of Positive Emotions. Am. Psychol. 2001, 56, 218–226. [Google Scholar] [CrossRef] [PubMed]
- Seligman, M.E.P.; Ernst, R.M.; Gillham, J.E.; Reivich, K.; Linkins, M. Positive Education: Positive Psychology and Classroom Interventions. Oxf. Rev. Educ. 2009, 35, 293–311. [Google Scholar] [CrossRef]
- Boyle, P.A.; Buchman, A.S.; Barnes, L.L.; Bennett, D.A. Effect of a Purpose in Life on Risk of Incident Alzheimer Disease and Mild Cognitive Impairment in Community-Dwelling Older Persons. Arch. Gen. Psychiatry 2010, 67, 304. [Google Scholar] [CrossRef]
- Boyle, P.A.; Buchman, A.S.; Wilson, R.; Yu, L.; Schneider, J.A.; Bennett, D.A. Effect of Purpose in Life on the Relation Between Alzheimer Disease Pathologic Changes on Cognitive Function in Advanced Age. Arch. Gen. Psychiatry 2012, 69, 499. [Google Scholar] [CrossRef]
- Dubicka, B.; Marwedel, S.; Banares, S.; McCulloch, A.; Tahoun, T.; Hearn, J.H.; Kroll, L. Feasibility Study of a New Behavioural Activation Programme for Young People with Depressed Mood. Child Adolesc. Ment. Health 2021, 27, 131–137. [Google Scholar] [CrossRef]
- Damayanti, N.; Ali, N.M. EMOGAME: Digital Games Therapy for Older Adults. Int. J. Adv. Comput. Sci. Appl. 2022, 13. [Google Scholar] [CrossRef]
- Palestra, G.; Pino, O. Detecting Emotions during a Memory Training Assisted by a Social Robot for Individuals with Mild Cognitive Impairment (MCI). Multimed. Tools Appl. 2020, 79, 35829–35844. [Google Scholar] [CrossRef]
- Van Son, D.; De Rover, M.; De Blasio, F.M.; Van Der Does, W.; Barry, R.J.; Putman, P. Electroencephalography Theta/Beta Ratio Covaries with Mind Wandering and Functional Connectivity in the Executive Control Network. Ann. N. Y. Acad. Sci. 2019, 1452, 52–64. [Google Scholar] [CrossRef] [PubMed]
- Franks, K.H.; Bransby, L.; Saling, M.M.; Pase, M.P. Association of Stress with Risk of Dementia and Mild Cognitive Impairment: A Systematic Review and Meta-Analysis. J. Alzheimer’s Dis. 2021, 82, 1573–1590. [Google Scholar] [CrossRef] [PubMed]
- Matsumoto, N.; Sugimoto, T.; Kuroda, Y.; Uchida, K.; Kishino, Y.; Arai, H.; Sakurai, T. Psychological Resilience Among Older Japanese Adults with Mild Cognitive Impairment During the COVID-19 Pandemic. Front. Psychiatry 2022, 13, 898990. [Google Scholar] [CrossRef] [PubMed]
- Innes, K.E.; Selfe, T.K.; Brown, C.M.; Rose, K.; Thompson-Heisterman, A.A. The Effects of Meditation on Perceived Stress and Related Indices of Psychological Status and Sympathetic Activation in Persons with Alzheimer’s Disease and Their Caregivers: A Pilot Study. Evid. -Based Complement. Altern. Med. 2012, 2012, 927509. [Google Scholar] [CrossRef] [PubMed]
- Leonard, B.E. HPA and Immune Axes in Stress: Involvement of the Serotonergic System. Neuroimmunomodulation 2006, 13, 268–276. [Google Scholar] [CrossRef] [PubMed]
- Serejo, F.; Emerit, I.; Filipe, P.; Fernandes, A.; Costa, M.; Freitas, J.; De Moura, M.C. Oxidative Stress in Chronic Hepatitis C: The Effect of Interferon Therapy and Correlation with Pathological Features. Can. J. Gastroenterol. 2003, 17, 644–650. [Google Scholar] [CrossRef]
- Andersen, J.K. Oxidative Stress in Neurodegeneration: Cause or Consequence? Nat. Med. 2004, 10, S18–S25. [Google Scholar] [CrossRef]
- Mecocci, P. Oxidative Stress in Mild Cognitive Impairment and Alzheimer Disease: A Continuum. J. Alzheimer’s Dis. 2004, 6, 159–163. [Google Scholar] [CrossRef]
- Vannini, P.; Gagliardi, G.; Kuppe, M.; Dossett, M.L.; Donovan, N.J.; Gatchel, J.R.; Quiroz, Y.T.; Premnath, P.Y.; Amariglio, R.E.; Sperling, R.A.; et al. Stress, Resilience, and Coping Strategies in a Sample of Community-Dwelling Older Adults during COVID-19. J. Psychiatr. Res. 2021, 138, 176–185. [Google Scholar] [CrossRef]
- Taherkhani, Z.; Kaveh, M.H.; Mani, A.; Ghahremani, L.; Khademi, K. The Effect of Positive Thinking on Resilience and Life Satisfaction of Older Adults: A Randomized Controlled Trial. Sci. Rep. 2023, 13, 3478. [Google Scholar] [CrossRef]
- Mirza, S.S.; Wolters, F.J.; Swanson, S.A.; Koudstaal, P.J.; Hofman, A.; Tiemeier, H.; Ikram, M.A. 10-Year Trajectories of Depressive Symptoms and Risk of Dementia: A Population-Based Study. Lancet Psychiatry 2016, 3, 628–635. [Google Scholar] [CrossRef] [PubMed]
- Smith, K.M.; Greene, M.F.; Babu, J.R.; Frugé, A.D. Psychobiotics as Treatment for Anxiety, Depression, and Related Symptoms: A Systematic Review. Nutr. Neurosci. 2019, 24, 963–977. [Google Scholar] [CrossRef] [PubMed]
- Santabárbara, J.; Bueno-Notivol, J.; Lipnicki, D.M.; De La Cámara, C.; López-Antón, R.; Lobo, A.; Gracia-García, P. A Novel Score for Predicting Alzheimer’s Disease Risk from Late Life Psychopathological and Health Risk Factors. Int. J. Environ. Res. Public Health 2021, 18, 1802. [Google Scholar] [CrossRef]
- Pink, A.; Lopez-Jimenez, F.; Syrjanen, J.; Vassilaki, M.; Lowe, V.J.; Vemuri, P.; Stokin, G.B.; Christianson, T.J.H.; Kremers, W.K.; Jack, C.R.; et al. A Longitudinal Investigation of Aβ, Anxiety, Depression, and Mild Cognitive Impairment. Alzheimers Dement. 2021, 18, 1824–1831. [Google Scholar] [CrossRef] [PubMed]
- Weisenbach, S.L.; Kim, J.; Hammers, D.B.; Koppelmans, V. Linking Late Life Depression and Alzheimer’s Disease: Mechanisms and Resilience. Curr. Behav. Neurosci. Rep. 2019, 6, 103–112. [Google Scholar] [CrossRef]
- Ovaska-Stafford, N.; Maltby, J.; Dale, M. Literature Review: Psychological Resilience Factors in People with Neurodegenerative Diseases. Arch. Clin. Neuropsychol. 2019, 36, 283–306. [Google Scholar] [CrossRef]
- Vadikolias, K.; Tsiakiri-Vatamidis, A.; Tripsianis, G.; Tsivgoulis, G.; Ioannidis, P.; Serdari, A.; Heliopoulos, J.; Livaditis, M.; Piperidou, C. Mild Cognitive Impairment: Effect of Education on the Verbal and Nonverbal Tasks Performance Decline. Brain Behav. 2012, 2, 620–627. [Google Scholar] [CrossRef]
- Allegri, R.F.; Taragano, F.E.; Krupitzki, H.; Serrano, C.; Dillon, C.; Sarasola, D.; Feldman, M.; Tufró, G.; Martelli, M.P.; Sanchez, V. Role of Cognitive Reserve in Progression from Mild Cognitive Impairment to Dementia. Dement. Neuropsychol. 2010, 4, 28–34. [Google Scholar] [CrossRef]
- Mendez, M.F. The Relationship Between Anxiety and Alzheimer’s Disease1. J. Alzheimer’s Dis. Rep. 2021, 5, 171–177. [Google Scholar] [CrossRef]
| Demographic Variables | Late MCI (n = 28) | Early MCI (n = 31) | Healthy (n = 30) |
|---|---|---|---|
| Male (n) | 9 | 5 | 9 |
| Female (n) | 19 | 26 | 21 |
| Age (years) M (S.D.) | 75.68 (5.07) | 73.39 (7.65) | 69.60 (5.30) |
| Education | |||
| Low (%) | 19 (67.9%) | 6 (19.4%) | 3 (10%) |
| High (%) | 9 (32.1%) | 25 (80.6%) | 27 (90%) |
| Assessment Tools | Late MCI | Early MCI | Healthy | Cronbach’s Alpha |
|---|---|---|---|---|
| Brief Resilience Scale | 3.07 (±0.99) | 3.18 (±0.67) | 3.45 (±0.68) | 0.807 |
| PERMA Profiler | 6.75 (±0.87) | 6.68 (±0.92) | 6.63 (±0.95) | 0.847 |
| Positive Emotions | 7.15 (±1.39) | 6.80 (±1.71) | 7.06 (±1.55) | 0.844 |
| Engagement | 6.48 (±1.64) | 6.76 (±1.67) | 7.11 (±1.70) | 0.565 |
| Accomplishment | 6.40 (±1.62) | 6.80 (±1.57) | 7.22 (±1.66) | 0.759 |
| Negative Emotions | 5.50 (±2.89) | 5.17 (±1.67) | 4.19 (±1.63) | 0.559 |
| Dass-21 | 0.61 (±0.55) | 0.66 (±0.59) | 0.47 (±0.45) | 0.935 |
| Depression | 0.73 (±0.67) | 0.71 (±0.73) | 0.43 (±0.49) | 0.865 |
| Anxiety | 0.40 (±0.54) | 0.46 (±0.63) | 0.25 (±0.40) | 0.866 |
| Stress | 0.69 (±0.62) | 0.80 (±0.55) | 0.74 (±0.58) | 0.855 |
| RES | POSEM | ENG | REL | MEAN | ACC | NEG | LON | PHY | HAP | DEP | ANX | STRESS | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| RES | Late MCI | 1 | 0.495 ** | 0.450 * | Non sig. | 0.445 * | 0.510 ** | −0.394 * | −0.431 * | Non sig. | 0.580 ** | −0.540 ** | −0.524 ** | −0.526 ** |
| Early MCI | 1 | 0.456 * | Non sig. | Non sig. | 0.420 * | Non sig. | −0.453 * | −0.381 * | 0.366 * | Non sig. | −0.376 * | −0.147 | −0.421 * | |
| Healthy | 1 | 0.621 ** | Non sig. | 0.554 ** | 0.387 * | 0.507 ** | -0.638 ** | −0.598 ** | 0.421 * | 0.607 ** | −0.721 ** | −0.508 ** | −0.672 ** |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tsormpatzoudi, S.O.; Moraitou, D.; Papaliagkas, V.; Pezirkianidis, C.; Tsolaki, M. Resilience in Mild Cognitive Impairment (MCI): Examining the Level and the Associations of Resilience with Subjective Wellbeing and Negative Affect in Early and Late-Stage MCI. Behav. Sci. 2023, 13, 792. https://doi.org/10.3390/bs13100792
Tsormpatzoudi SO, Moraitou D, Papaliagkas V, Pezirkianidis C, Tsolaki M. Resilience in Mild Cognitive Impairment (MCI): Examining the Level and the Associations of Resilience with Subjective Wellbeing and Negative Affect in Early and Late-Stage MCI. Behavioral Sciences. 2023; 13(10):792. https://doi.org/10.3390/bs13100792
Chicago/Turabian StyleTsormpatzoudi, Styliani Olympia, Despina Moraitou, Vasileios Papaliagkas, Christos Pezirkianidis, and Magda Tsolaki. 2023. "Resilience in Mild Cognitive Impairment (MCI): Examining the Level and the Associations of Resilience with Subjective Wellbeing and Negative Affect in Early and Late-Stage MCI" Behavioral Sciences 13, no. 10: 792. https://doi.org/10.3390/bs13100792
APA StyleTsormpatzoudi, S. O., Moraitou, D., Papaliagkas, V., Pezirkianidis, C., & Tsolaki, M. (2023). Resilience in Mild Cognitive Impairment (MCI): Examining the Level and the Associations of Resilience with Subjective Wellbeing and Negative Affect in Early and Late-Stage MCI. Behavioral Sciences, 13(10), 792. https://doi.org/10.3390/bs13100792










