Levels and Factors Associated with Resilience in Italian Healthcare Professionals during the COVID-19 Pandemic: A Web-Based Survey
Abstract
1. Introduction
2. Materials and Methods
2.1. Social and Health Context and Design of the Study
2.2. Survey Development
2.3. Survey Structure
2.4. Target Population and Survey Administration
2.5. Ethical Considerations
2.6. Statistical Analysis
3. Results
3.1. General Characteristics of the Study Sample
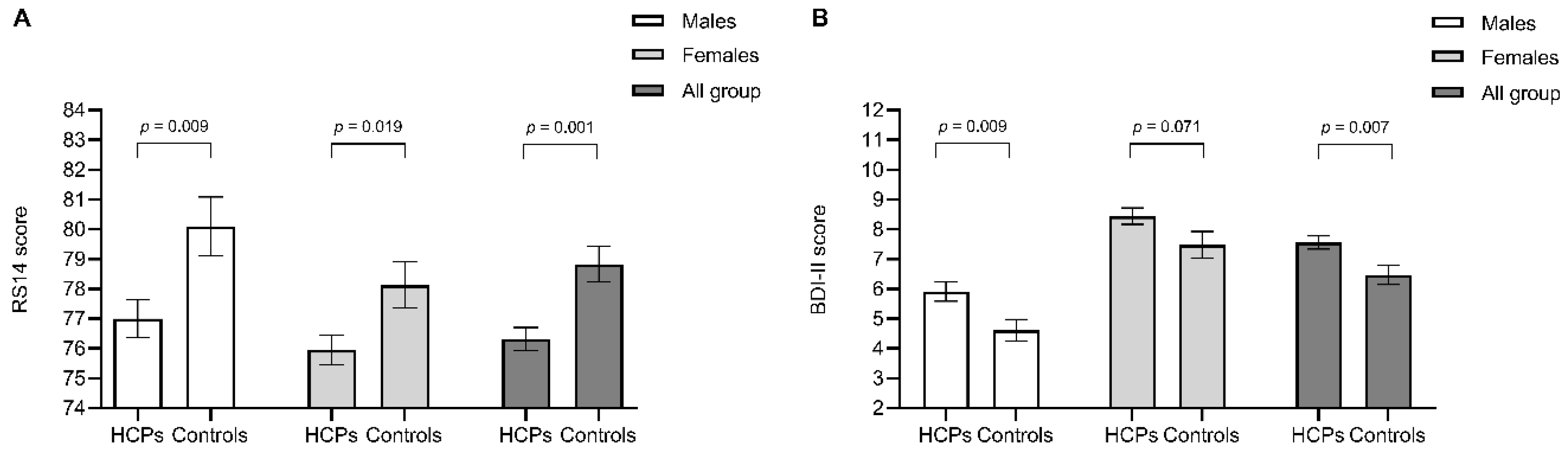
3.2. Levels of Resilience in HCPs during the COVID-19 Pandemic
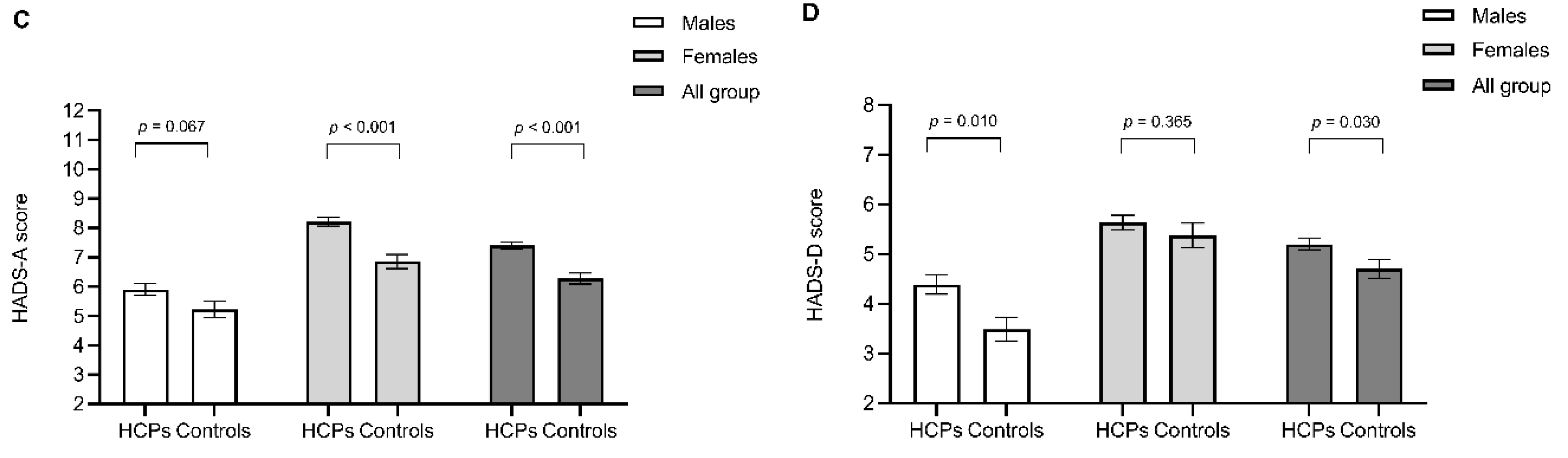
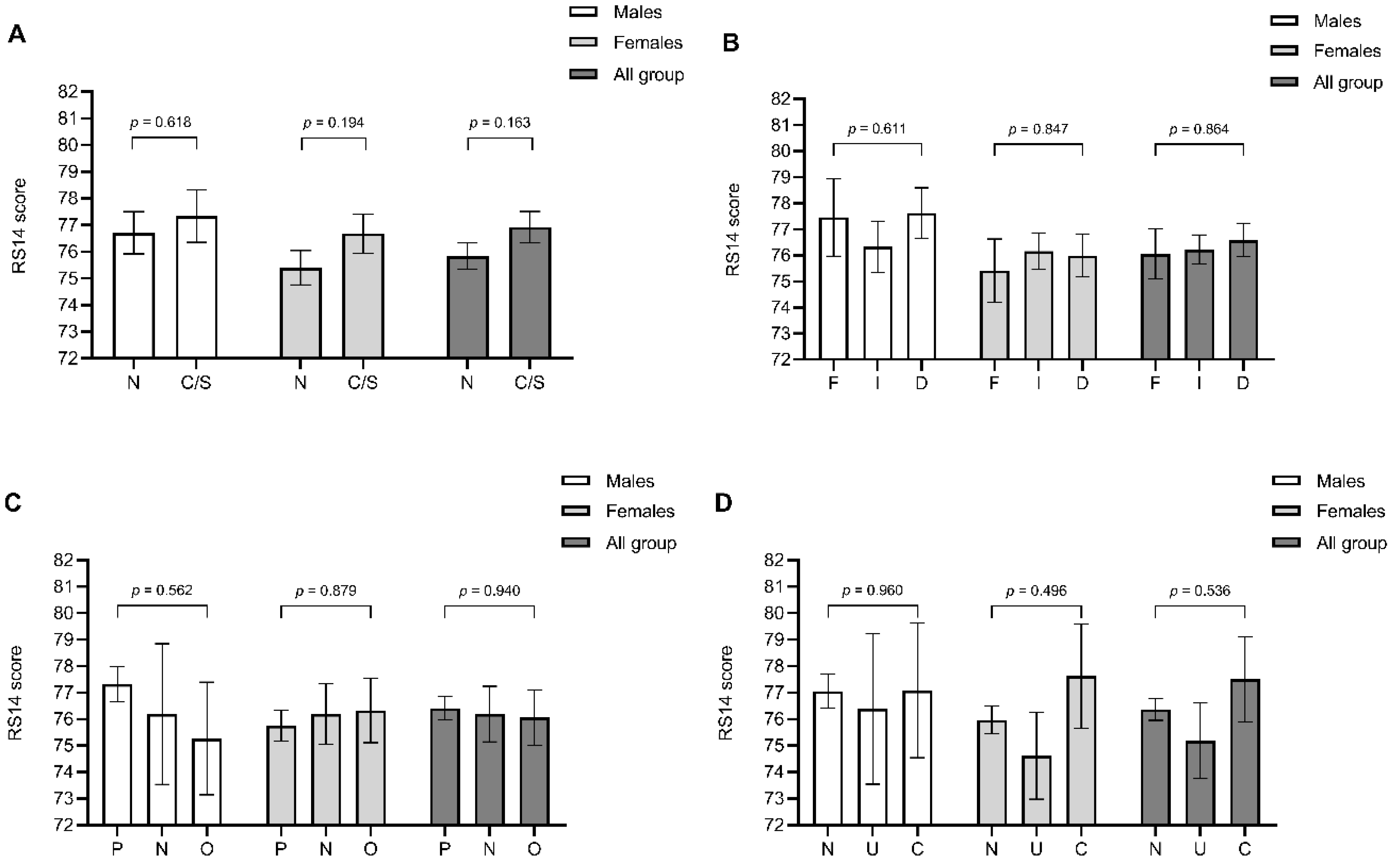
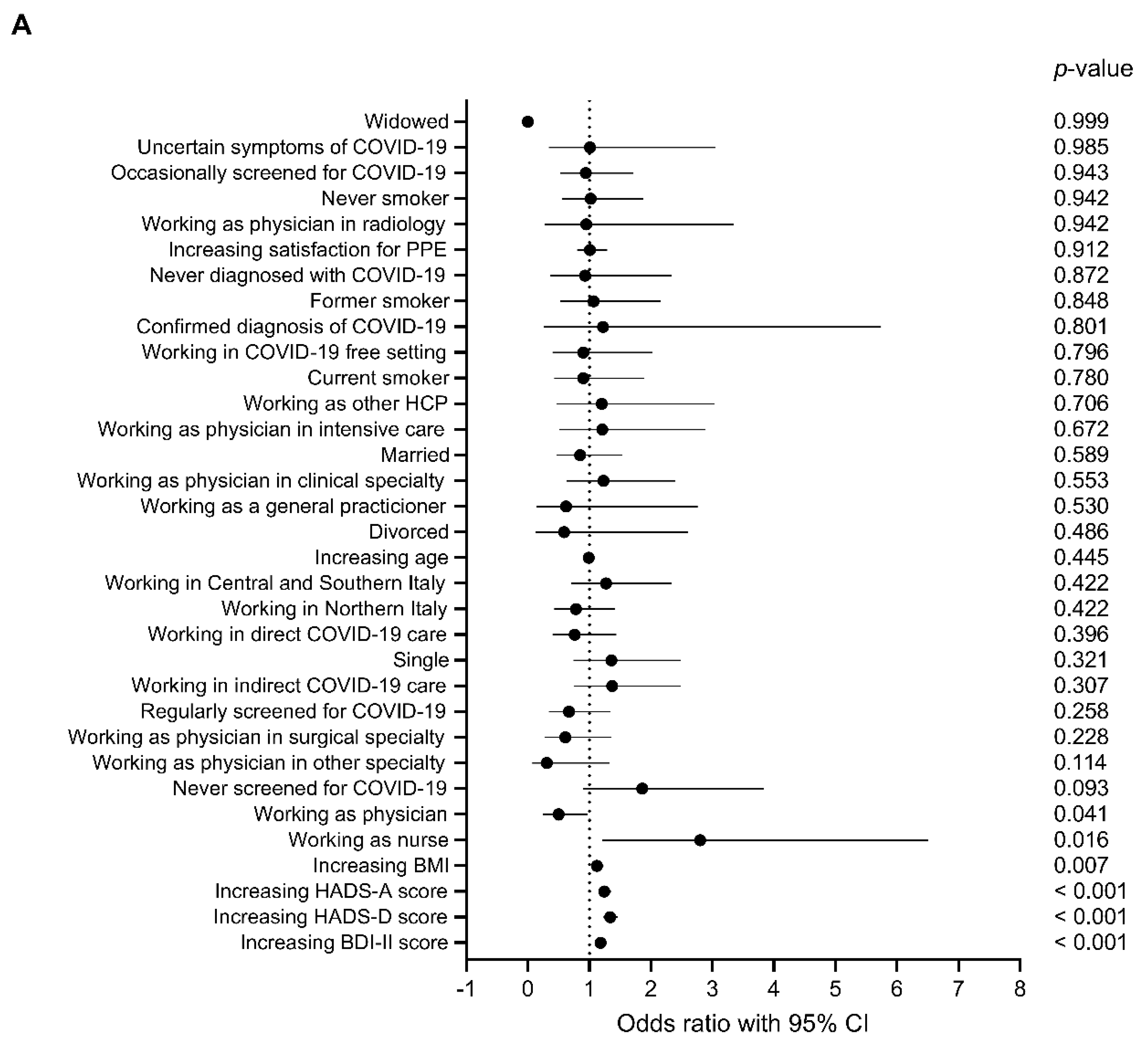
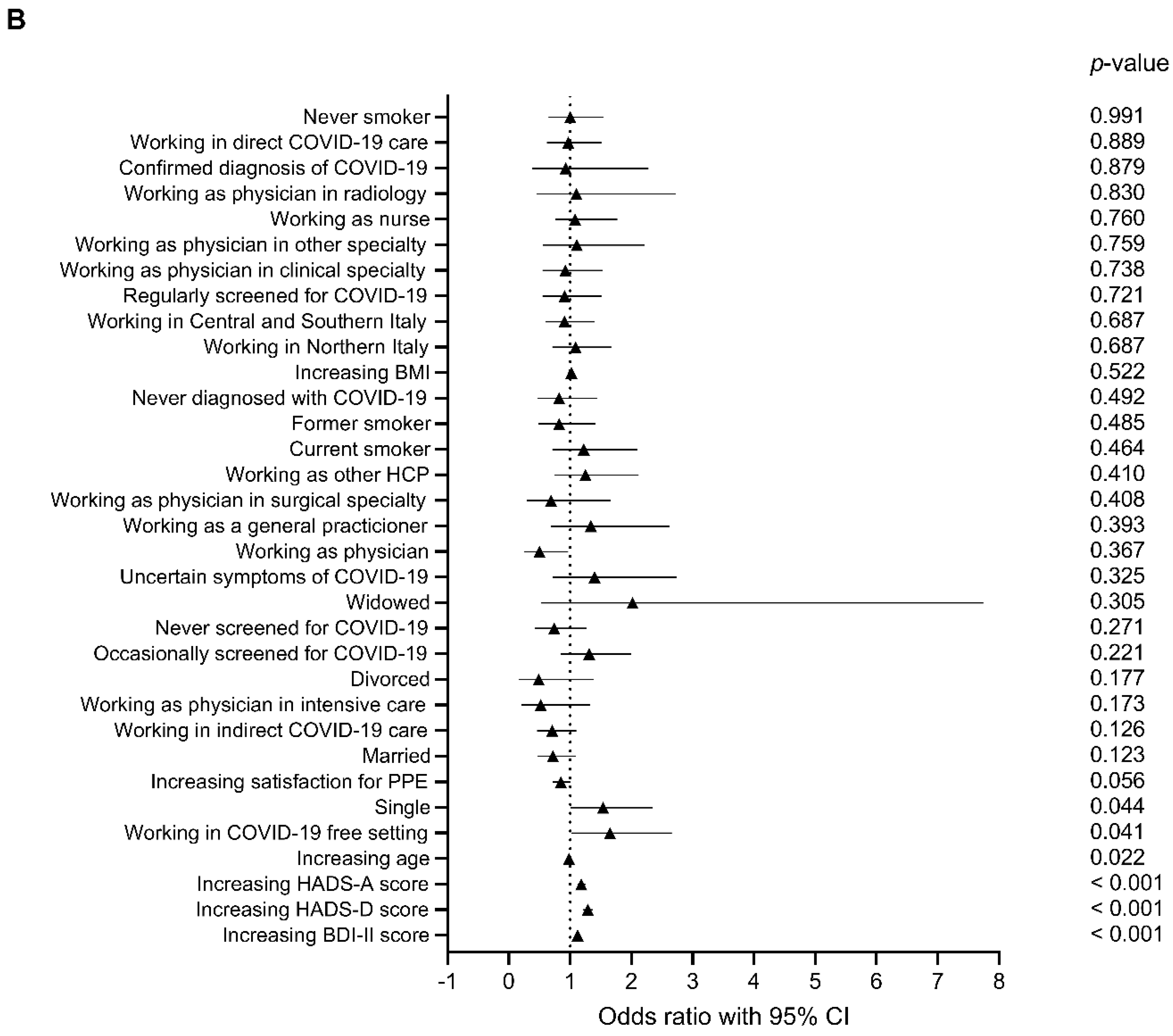
3.3. Factors Affecting Resilience in HCPs during the COVID-19 Pandemic
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Johnston, M.C.; Porteous, T.; Crilly, M.A.; Burton, C.D.; Elliott, A.; Iversen, L.; McArdle, K.; Murray, A.; Phillips, L.H.; Black, C. Physical disease and resilient outcomes: A systematic review of resilience definitions and study methods. J. Psychosom. Res. 2015, 56, 168–180. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.; Cranford, J.A. Does resilience moderate the associations between parental problem drinking and adolescents’ internalizing and externalizing behaviors? Drug Alcohol Depend. 2008, 96, 213–221. [Google Scholar] [CrossRef] [PubMed]
- Jackson, D.; Firtko, A.; Edenborough, M. Personal resilience as a strategy for surviving and thriving in the face of workplace adversity: A literature review. J. Adv. Nurs. 2007, 60, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Edmonstone, J. Personal Resilience for Healthcare Staff, when the Going Gets Tough; Radcliffe Publishing: London, UK, 2013. [Google Scholar]
- Zhou, P.; Yang, X.-L.; Wang, X.-G.; Hu, B.; Zhang, L.; Zhang, W.; Si, H.-R.; Zhu, Y.; Li, B.; Huang, C.-L.; et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature 2020, 579, 270–273. [Google Scholar] [CrossRef]
- WHO. Director-General’s Opening Remarks at the Media Briefing on COVID-19–11 March 2020. Available online: https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 (accessed on 17 May 2020).
- WHO. WHO Coronavirus Disease (COVID-19) Dashboard. Available online: https://covid19.who.int/?gclid=Cj0KCQjwn7j2BRDrARIsAHJkxmzAoKqHqHfKLNTzlSN9vL6NKpoZWXUmP_wXL03mphsjLlPPvpJndVAaAliwEALw_wcB (accessed on 18 November 2020).
- International Monetary Fund. The Great Lockdown: Worst Economic Downturn since the Great Depression. Available online: https://blogs.imf.org/2020/04/14/the-great-lockdown-worst-economic-downturn-since-the-great-depression/ (accessed on 4 October 2020).
- González-Sanguino, C.; Ausín, B.; Castellanos, M.Á.; Saiz, J.; López-Gómez, A.; Ugidos, C.; Muñoz, M. Mental health consequences during the initial stage of the 2020 Coronavirus pandemic (COVID-19) in Spain. Brain Behav. Immun. 2020, 87, 172–176. [Google Scholar] [CrossRef]
- Wang, C.; Pan, R.; Wan, X.; Tan, Y.; Xu, L.; McIntyre, R.S.; Choo, F.N.; Tran, B.; Ho, R.; Sharma, V.K.; et al. A longitudinal study on the mental health of general population during the COVID-19 epidemic in China. Brain Behav. Immun. 2020. [Google Scholar] [CrossRef]
- Pfefferbaum, B.; North, C.S. Mental health and the Covid-19 pandemic. N. Engl. J. Med. 2020, 383, 510–512. [Google Scholar] [CrossRef]
- FNOMCEO. Elenco dei Medici Caduti nel Corso dell’epidemia di Covid-19. Available online: https://portale.fnomceo.it/elenco-dei-medici-caduti-nel-corso-dellepidemia-di-covid-19/ (accessed on 30 October 2020).
- Greenberg, N.; Docherty, M.; Gnanapragasam, S.; Wessely, S. Managing mental health challenges faced by healthcare workers during covid-19 pandemic. BMJ 2020, 368, m1211. [Google Scholar] [CrossRef]
- Santarone, K.; McKenney, M.; Elkbuli, A. Preserving mental health and resilience in frontline healthcare workers during COVID-19. Am. J. Emerg. Med. 2020, 38, 1530–1531. [Google Scholar] [CrossRef]
- Preti, E.; Di Mattei, V.; Perego, G.; Ferrari, F.; Mazzetti, M.; Taranto, P.; Di Pierro, R.; Madeddu, F.; Calati, R. The psychological impact of epidemic and pandemic outbreaks on healthcare workers: Rapid review of the evidence. Curr. Psychiatry Rep. 2020, 22, 1–22. [Google Scholar] [CrossRef]
- Liang, Y.; Wu, K.; Zhou, Y.; Huang, X.; Zhou, Y.; Liu, Z. Mental health in frontline medical workers during the 2019 novel Coronavirus disease epidemic in China: A comparison with the general population. Int. J. Environ. Res. Public Health 2020, 17, 6550. [Google Scholar] [CrossRef] [PubMed]
- McCann, C.M.; Beddoe, E.; McCormick, K.; Huggard, P.; Kedge, S.; Adamson, C.; Huggard, J. Resilience in the health professions: A review of recent literature. Int. J. Wellbeing 2013, 3, 60–81. [Google Scholar] [CrossRef]
- Luo, M.; Guo, L.; Yu, M.; Jiang, W.; Wang, H. The psychological and mental impact of coronavirus disease 2019 (COVID-19) on medical staff and general public-A systematic review and meta-analysis. Psychiatry Res. 2020, 291, 113190. [Google Scholar] [CrossRef] [PubMed]
- Southwick, S.M.; Charney, D.S.; Chang, J.C.; Lockner, D.A.; Reches, Z. The science of resilience: Implications for the prevention and treatment of depression. Science 2012, 338, 79–82. [Google Scholar] [CrossRef]
- Pappa, S.; Ntella, V.; Giannakas, T.; Giannakoulis, V.G.; Papoutsi, E.; Katsaounou, P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: A systematic review and meta-analysis. Brain Behav. Immun. 2020. [Google Scholar] [CrossRef]
- Barnett, J.E.; Baker, E.K.; Elman, N.S.; Schoener, G.R. In pursuit of wellness: The self-care imperative. Prof. Psychol. Res. Pract. 2007, 38, 603–612. [Google Scholar] [CrossRef]
- Robertson, H.D.; Elliott, A.M.; Burton, C.; Iversen, L.; Murchie, P.; Porteous, T.; Matheson, C. Resilience of primary healthcare professionals: A systematic review. Br. J. Gen. Pract. 2016, 66, e423–e433. [Google Scholar] [CrossRef]
- Iflaifel, M.; Lim, R.; Ryan, K.; Crowley, C. Resilient Health Care: A systematic review of conceptualisations, study methods and factors that develop resilience. BMC Health Serv. Res. 2020, 20, 324. [Google Scholar] [CrossRef]
- Eley, D.S.; Cloninger, C.R.; Walters, L.; Laurence, C.; Synnott, R.; Wilkinson, D. The relationship between resilience and personality traits in doctors: Implications for enhancing well being. PeerJ 2013, 1, e216. [Google Scholar] [CrossRef]
- Knox, B.S.; Duffy, M.E.; Bunting, B.P.; Parr, H.; De Almeida, M.D.V.; Gibney, M. Associations between obesity (BMI and waist circumference) and socio-demographic factors, physical activity, dietary habits, life events, resilience, mood, perceived stress and hopelessness in healthy older Europeans. BMC Public Health 2012, 12, 424. [Google Scholar] [CrossRef]
- Wu, Z.; Liu, Y.; Li, X.; Li, X. Resilience and associated factors among mainland Chinese women newly diagnosed with breast cancer. PLoS ONE 2016, 11, e0167976. [Google Scholar] [CrossRef] [PubMed]
- Nishimi, K.; Choi, K.W.; Cerutti, J.; Powers, A.; Bradley, B.; Dunn, E.C. Measures of adult psychological resilience following early-life adversity: How congruent are different measures? Psychol Med. 2020, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Hirani, S.; Lasiuk, G.; Hegadoren, K. The intersection of gender and resilience. J. Psychiatr. Ment. Heal. Nurs. 2016, 23, 455–467. [Google Scholar] [CrossRef] [PubMed]
- Morano, C. Resilience and coping with trauma: Does gender make a difference? J. Hum. Behav. Soc. Environ. 2010, 20, 553–568. [Google Scholar] [CrossRef]
- Novel Coronavirus. Available online: http://www.salute.gov.it/portale/nuovocoronavirus/homeNuovoCoronavirus.jsp (accessed on 28 July 2020).
- Istituto Superiore di Sanità (ISS). COVID-19 Pandemic-National Update April 28, 2020. Available online: https://www.epicentro.iss.it/coronavirus/bollettino/Bollettino-sorveglianza-integrata-COVID-19_28-aprile-2020.pdf (accessed on 12 August 2020).
- Walters, C.; Harter, Z.J.; Wayant, C.C.; Vo, N.; Warren, M.; Chronister, J.; Tritz, D.; Vassar, M. Do oncology researchers adhere to reproducible and transparent principles? A cross-sectional survey of published oncology literature. BMJ Open 2019, 9, e033962. [Google Scholar] [CrossRef] [PubMed]
- Capraş, R.-D.; Bulboacă, A.E.; Bolboac, S.D. Evidence-based medicine self-assessment, knowledge, and integration into daily practice: A survey among Romanian physicians and comparison between trainees and specialists. BMC Med. Educ. 2020, 20, 1–10. [Google Scholar] [CrossRef]
- Iqbal, M.R.; Chaudhuri, A. COVID-19: Results of a national survey of United Kingdom healthcare professionals’ perceptions of current management strategy-A cross-sectional questionnaire study. Int. J. Surg. 2020, 79, 156–161. [Google Scholar] [CrossRef]
- Eysenbach, G. Improving the quality of web surveys: The checklist for reporting results of internet E-surveys (CHERRIES). J. Med. Internet Res. 2004, 6, e34. [Google Scholar] [CrossRef]
- Wagnild, G. The Resilience Scale User’s Guide for the US English Version of the Resilience Scale and the 14-Item Resilience Scale (RS–14); Resilience Center: Billings, MT, USA, 2016. [Google Scholar]
- Callegari, C.; Bertù, L.; Lucano, M.; Ielmini, M.; Braggio, E.; Vender, S. Reliability and validity of the Italian version of the 14-item Resilience Scale. Psychol. Res. Behav. Manag. 2016, 9, 277–284. [Google Scholar] [CrossRef]
- Sacco, R.; Santangelo, G.; Stamenova, S.; Bisecco, A.; Bonavita, S.; Lavorgna, L.; Trojano, L.; D’Ambrosio, A.; Tedeschi, G.; Gallo, A. Psychometric properties and validity of Beck Depression Inventory II in multiple sclerosis. Eur. J. Neurol. 2016, 23, 744–750. [Google Scholar] [CrossRef]
- Beck, A.T.; Steer, R.A.; Brown, G.K. BDI-II: Beck Depression Inventory Manual, 2nd ed.; Psychological Corporation: San Antonio, TX, USA, 1996. [Google Scholar]
- Kendall, P.C.; Hollon, S.D.; Beck, A.T.; Hammen, C.L.; Ingram, R.E. Issues and recommendations regarding use of the Beck Depression Inventory. Cogn. Ther. Res. 1987, 11, 289–299. [Google Scholar] [CrossRef]
- Annunziata, M.A.; Muzzatti, B.; Altoè, G. Defining Hospital Anxiety and Depression Scale (HADS) structure by confirmatory factor analysis: A contribution to validation for oncological settings. Ann. Oncol. 2011, 22, 2330–2333. [Google Scholar] [CrossRef] [PubMed]
- Snaith, R.P.; Zigmond, A.S. The Hospital Anxiety and Depression Scale Manual; Nfer-Nelson: Windsor, UK, 1994. [Google Scholar]
- Crawford, J.R.; Henry, J.D.; Crombie, C.; Taylor, E.P. Normative data for the HADS from a large non-clinical sample. Br. J. Clin. Psychol. 2001, 40, 429–434. [Google Scholar] [CrossRef] [PubMed]
- World Medical Association. World medical association declaration of Helsinki: Ethical principles for medical research involving human subjects. JAMA 2013, 310, 2191–2194. [Google Scholar] [CrossRef]
- Cronbach, L.J. Coefficient alpha and the internal structure of tests. Psychometrika 1951, 16, 297–334. [Google Scholar] [CrossRef]
- Lewsey, J. Medical statistics: A guide to data analysis and critical appraisal. Ann. R. Coll. Surg. Engl. 2006, 88, 603. [Google Scholar] [CrossRef]
- Hornor, G. Resilience. J. Pediatr. Health Care 2017, 31, 384–390. [Google Scholar] [CrossRef]
- Steptoe, A.; Dockray, S.; Wardle, J. Positive affect and psychobiological processes relevant to health. J. Personal. 2009, 77, 1747–1776. [Google Scholar] [CrossRef]
- Davydov, D.M.; Stewart, R.C.; Ritchie, K.; Chaudieu, I. Resilience and mental health. Clin. Psychol. Rev. 2010, 30, 479–495. [Google Scholar] [CrossRef]
- Kain, J.; Jex, S. Karasek’s (1979) job demands-control model: A summary of current issues and recommendations for future research. New Dev. Theor. Concept. Approach. Job Stress 2010, 8, 237–268. [Google Scholar] [CrossRef]
- Goldzweig, G.; Merims, S.; Ganon, R.; Peretz, T.; Altman, A.; Baider, L. Informal caregiving to older cancer patients: Preliminary research outcomes and implications. Ann. Oncol. 2013, 24, 2635–2640. [Google Scholar] [CrossRef] [PubMed]
- Bavafa, A.; Khazaie, H.; Khaledi-Paveh, B.; Rezaie, L. The relationship of severity of symptoms of depression, anxiety, and stress with sleep quality in earthquake survivors in Kermanshah. J. Inj. Violence Res. 2019, 11, 225–232. [Google Scholar] [CrossRef] [PubMed]
- Cleary, M.; Kornhaber, R.; Thapa, D.K.; West, S.; Visentin, D. The effectiveness of interventions to improve resilience among health professionals: A systematic review. Nurse Educ. Today 2018, 71, 247–263. [Google Scholar] [CrossRef] [PubMed]
| COVID-19-Free Setting (n = 195) A | Indirect COVID-19 Care (n = 451) B | Direct COVID-19 Care (n = 363) C | Controls (n = 375) D | p-Value | ||
|---|---|---|---|---|---|---|
| Age, years | 43.78 ± 13.12 | 43.37 ± 12.05 | 40.88 ± 11.23 | 48.39 ± 13.66 A,B,C | <0.001 | |
| Gender, n (%) | Male | 61 (31.3) | 160 (35.5) | 132 (36.4) | 133 (35.5) | 0.670 |
| Female | 134 (68.7) | 291 (64.5) | 231 (63.6) | 242 (64.5) | ||
| Body mass index, kg/m2 | 24.12 ± 3.85 | 24.05 ± 3.85 | 23.82 ± 3.90 | 24.41 ± 3.79 | 0.218 | |
| Marital status, n (%) | Single | 67 (34.4) | 180 (39.9) | 143 (39.4) | 123 (32.8) | <0.001 |
| Married | 109 (55.9) | 241 (53.4) | 188 (51.8) | 212 (56.5) | ||
| Divorced | 10 (5.1) | 26 (5.8) | 32 (8.8) | 33 (8.8) | ||
| Widowed | 9 (4.6) | 4 (0.9) | 0 (0) | 7 (1.9) | ||
| Smoking habits, n (%) | Never smoker | 120 (61.5) | 270 (59.9) | 222 (61.2) | 184 (49.1) A,B,C | 0.001 |
| Former smoker | 50 (25.6) | 96 (21.3) | 65 (17.9) | 104 (27.7) C | ||
| Current smoker | 25 (12.8) | 85 (18.8) | 76 (20.9) | 87 (23.2) A | ||
| Geographic area, n (%) | Northern Italy | 55 (28.2) | 256 (56.8) | 250 (68.9) | 228 (60.8) A | <0.001 |
| Southern and Central Italy | 140 (71.8) | 195 (43.2) | 113 (31.1) | 147 (39.2) A | ||
| Chronic comorbidities, n (%) | 76 (39.0) | 151 (33.5) | 93 (25.6) | 134 (35.7) C | 0.004 | |
| HCP role, n (%) | Physician | 100 (51.3) #,B,C | 323 (71.6) | 254 (70.0) | - | <0.001 |
| Nurse | 34 (17.4) # | 71 (15.7) | 76 (20.9) | - | ||
| Other HCP | 61 (31.3) #,B,C | 57 (12.6) | 33 (9.1) | - | ||
| Medical specialty area, n (%) | Clinical | 24 (12.3) #,B,C | 105 (23.3) | 105 (28.9) | - | <0.001 |
| Surgical | 9 (4.6) #,B,C | 78 (17.3) | 44 (12.1) | - | ||
| Intensive Care | 0 (0) #,B,C | 22 (4.9) | 75 (20.7) | - | ||
| Radiology | 1 (0.5) #,B | 46 (10.2) | 10 (2.8) | - | ||
| Other medical specialties | 46 (23.6) #,B,C | 48 (10.6) | 8 (2.2) | - | ||
| General practice | 28 (14.4) #,C | 37 (8.2) | 17 (4.7) | - | ||
| COVID-19 screening, n (%) | Never | 99 (50.8) #,B,C | 86 (19.1) | 18 (5.0) | 375 (100.0) A,B,C | <0.001 |
| Occasionally | 82 (42.1) #,B,C | 240 (53.2) | 221 (60.9) | 0 (0) A,B,C | ||
| Regularly | 14 (7.2) #,B,C | 125 (27.7) | 124 (34.2) | 0 (0) A,B,C | ||
| Symptomatic COVID-19, n (%) | No | 179 (91.8) #,C | 384 (85.1) | 307 (84.6) | 375 (100.0) A,B,C | <0.001 |
| Uncertain | 14 (7.2) | 42 (9.3) | 31 (8.5) | 0 (0) A,B,C | ||
| Yes | 2 (1.0) #,B,C | 25 (5.5) | 25 (6.9) | 0 (0) B,C | ||
| COVID-19 duration, days | 1.13 ± 5.70 | 2.81 ± 9.53 | 2.11 ± 7.00 | - | 0.049 | |
| PPE satisfaction, 5-point Likert-type scale | 2.58 ± 1.39 #,B,C | 2.81 ± 1.18 | 3.41 ± 1.16 | - | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lisi, L.; Ciaffi, J.; Bruni, A.; Mancarella, L.; Brusi, V.; Gramegna, P.; Ripamonti, C.; Quaranta, E.; Borlandelli, E.; Gallo, G.; et al. Levels and Factors Associated with Resilience in Italian Healthcare Professionals during the COVID-19 Pandemic: A Web-Based Survey. Behav. Sci. 2020, 10, 183. https://doi.org/10.3390/bs10120183
Lisi L, Ciaffi J, Bruni A, Mancarella L, Brusi V, Gramegna P, Ripamonti C, Quaranta E, Borlandelli E, Gallo G, et al. Levels and Factors Associated with Resilience in Italian Healthcare Professionals during the COVID-19 Pandemic: A Web-Based Survey. Behavioral Sciences. 2020; 10(12):183. https://doi.org/10.3390/bs10120183
Chicago/Turabian StyleLisi, Lucia, Jacopo Ciaffi, Antonella Bruni, Luana Mancarella, Veronica Brusi, Pasquale Gramegna, Claudio Ripamonti, Elisabetta Quaranta, Elena Borlandelli, Gaetano Gallo, and et al. 2020. "Levels and Factors Associated with Resilience in Italian Healthcare Professionals during the COVID-19 Pandemic: A Web-Based Survey" Behavioral Sciences 10, no. 12: 183. https://doi.org/10.3390/bs10120183
APA StyleLisi, L., Ciaffi, J., Bruni, A., Mancarella, L., Brusi, V., Gramegna, P., Ripamonti, C., Quaranta, E., Borlandelli, E., Gallo, G., Garofalo, E., Chiaravalloti, A., Viola, P., Ruscitti, P., Caio, G., D’Onghia, M., D’Amuri, A., Cimellaro, A., Facchini, G., ... Ursini, F. (2020). Levels and Factors Associated with Resilience in Italian Healthcare Professionals during the COVID-19 Pandemic: A Web-Based Survey. Behavioral Sciences, 10(12), 183. https://doi.org/10.3390/bs10120183









