Short-Term Effects of Air Pollution on Coronary Events in Strasbourg, France—Importance of Seasonal Variations
Abstract
1. Introduction
2. Materials and Methods
2.1. Population Studied
2.2. Cases
2.3. Assessment of Exposure to Air Pollution
2.4. Seasonality
2.5. Lags
2.6. Statistical Analysis
3. Results
3.1. Number and Categories of Coronary Events
3.2. Pollutants
3.3. Impact of the NO2 Concentration on Coronary Events
3.4. Impact of the PM2.5 Concentration on Coronary Events
3.5. Impact of the PM10 Concentration on Coronary Events
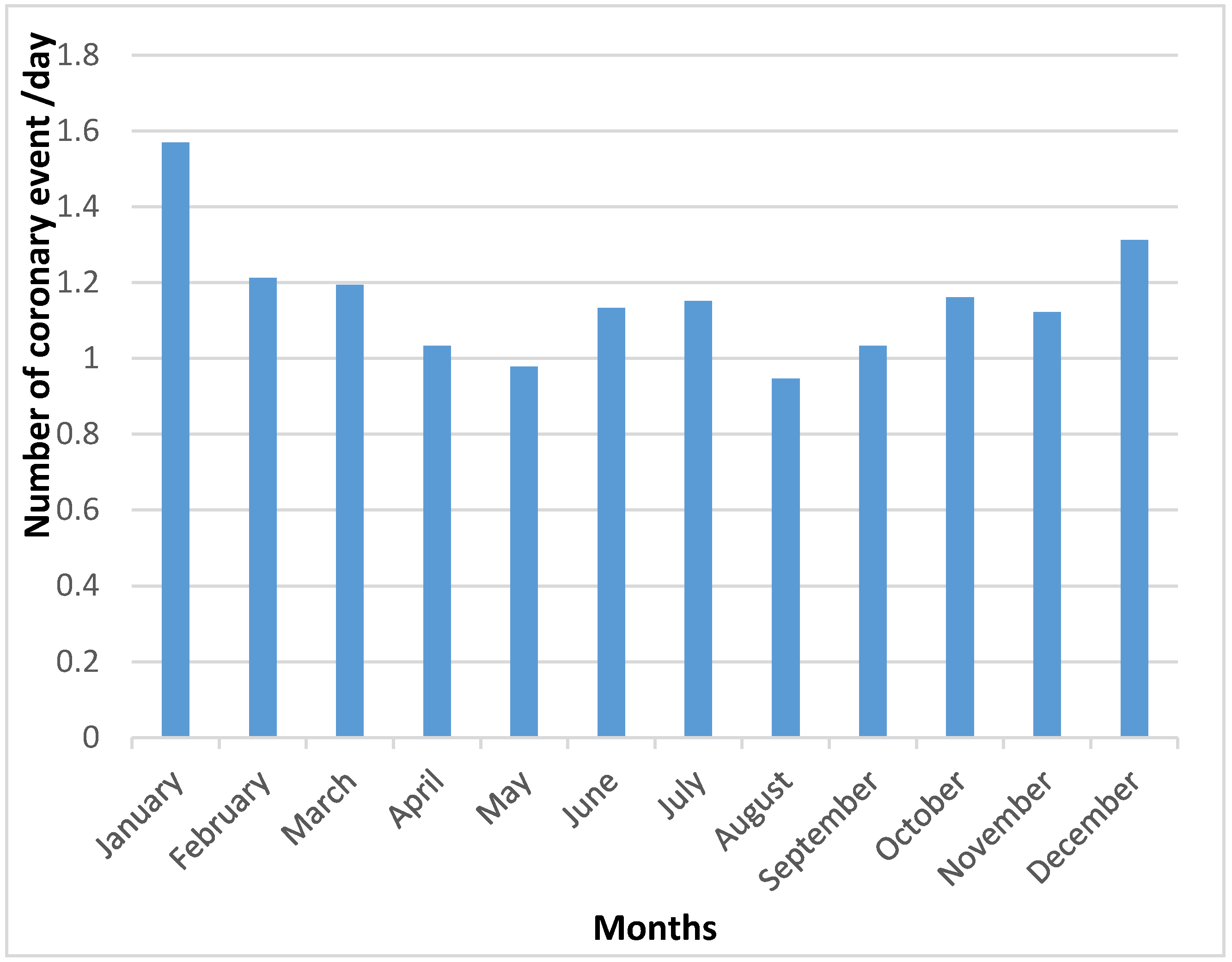
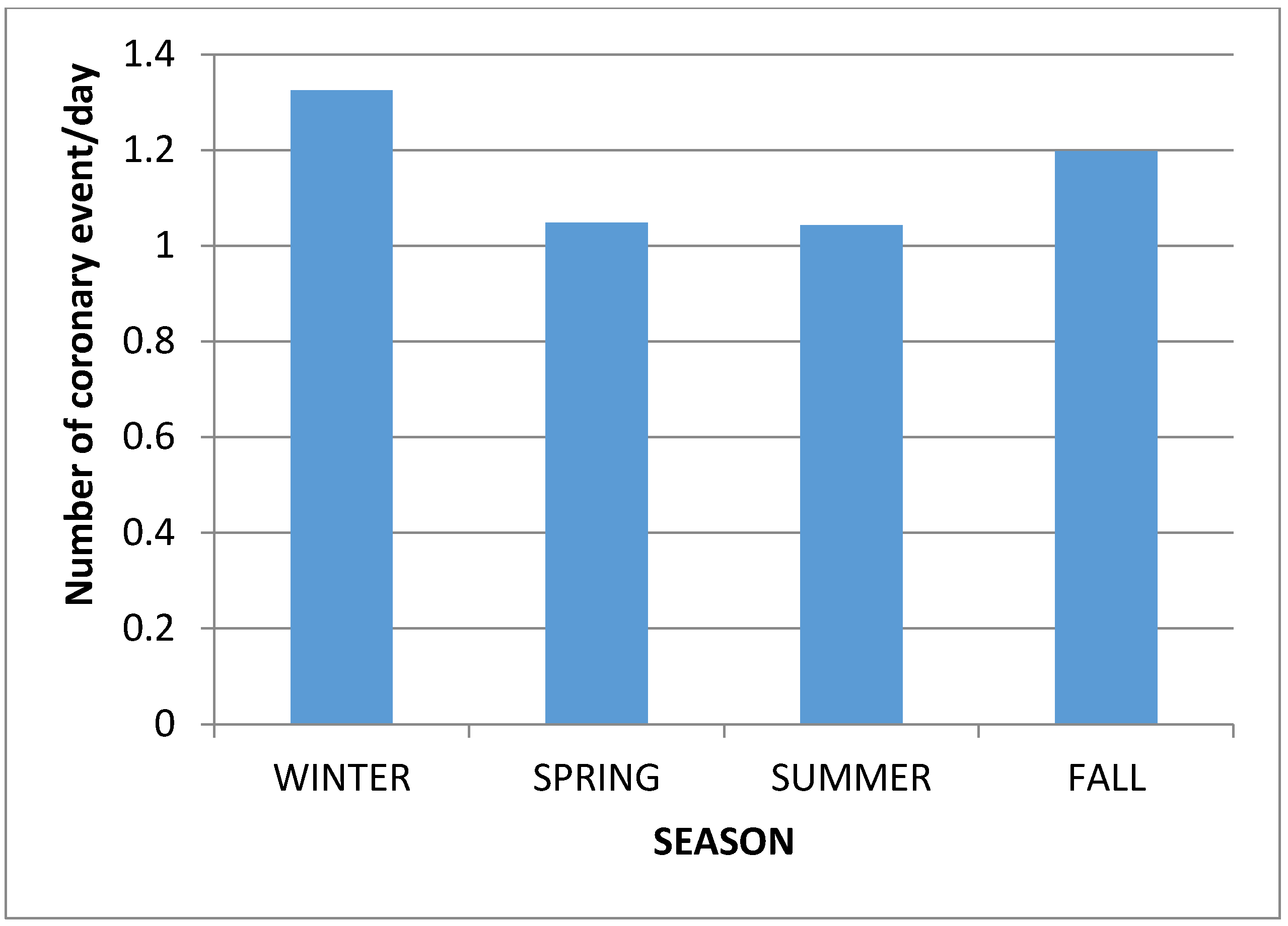
3.6. The Seasonality of Coronary Events
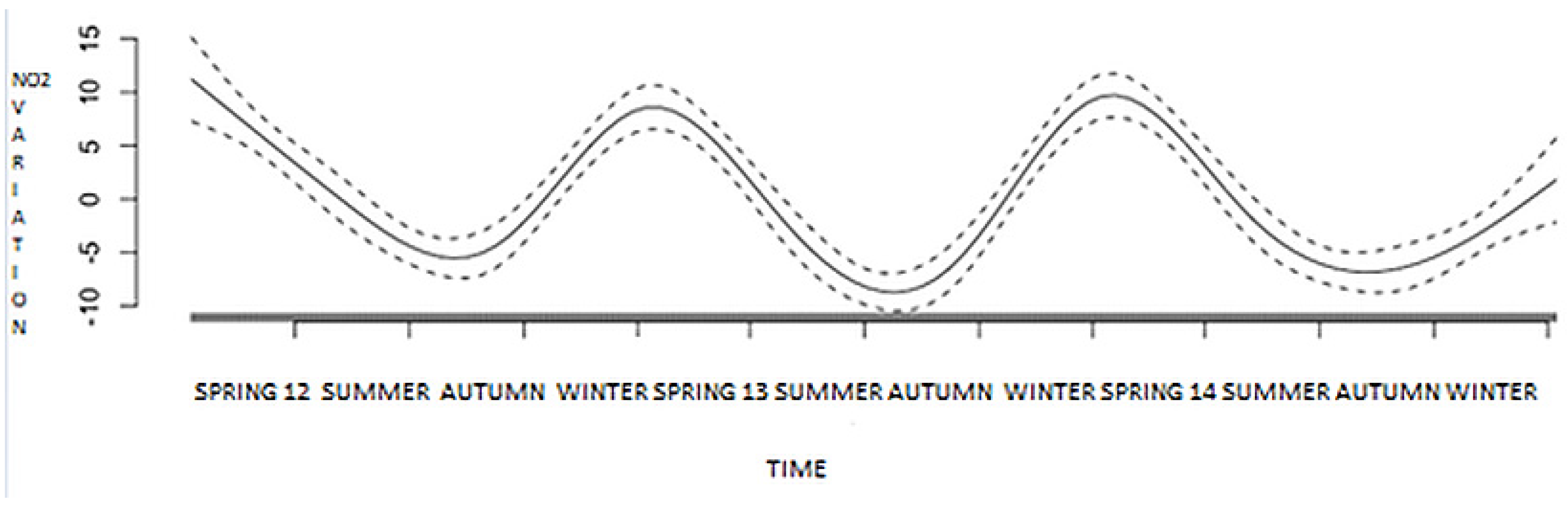
3.7. Inferential Analysis: Generalized Additive Model (GAM)—Pollutant and Time Effect
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Liu, H.; Tian, Y.H.; Xiang, X.; Sun, K.; Juan, J.; Song, J.; Cao, Y.Y.; Xu, B.B.; Hu, Y.H. Air Pollution and Hospitalization for Acute Myocardial Infarction in China. Am. J. Cardiol. 2017, 120, 753–758. [Google Scholar] [CrossRef] [PubMed]
- Lee, M.W.; Choi, B.G.; Kim, S.W.; Rha, S.-W.; Shim, M.S.; Kim, D.J.; Seo, S.H.; Oh, D.J.; Jeonh, M.H. Air Pollution and Short-Term Clinical Outcomes of Patients with Acute Myocardial Infar on. Clin. Exp. Pharmacol. Physiol. 2017, 44, 631–638. [Google Scholar] [CrossRef] [PubMed]
- Garelnabi, M.; Uzoigwe, J.C.; Prum, T.; Bresnahan, E. The Emerging Role of Outdoor and Indoor Air Pollution in Cardiovascular Disease. N. Am. J. Med Sci. 2013, 5, 445–453. [Google Scholar] [CrossRef] [PubMed]
- Lelieveld, J.; Evans, J.S.; Fnais, M.; Giannadaki, D.; Pozzer, A. The Contribution of Outdoor Air Pollution Sources to Premature Mortality on a Global Scale. Nature 2015, 525, 367–371. [Google Scholar] [CrossRef] [PubMed]
- Xu, M.; Guo, Y.; Zhang, Y.; Westerdahl, D.; Mo, Y.; Liang, F.; Pan, X. Spatiotemporal Analysis of Particulate Air Pollution and Ischemic Heart Disease Mortality in Beijing, China. Environ. Health 2014, 13, 109. [Google Scholar] [CrossRef] [PubMed]
- Bourdrel, T.; Bind, M.-A.; Béjot, Y.; Morel, O.; Argacha, J.-F. Cardiovascular Effects of Air Pollution. Arch. Cardiovasc. Dis. 2017, 110, 634–642. [Google Scholar] [CrossRef]
- Bhaskaran, K.; Hajat, S.; Haines, A.; Herrett, E.; Wilkinson, P.; Smeeth, L. Effects of Air Pollution on the Incidence of Myocardial Infarction. Heart 2009, 95, 1746–1759. [Google Scholar] [CrossRef]
- Rasche, M.; Walther, M.; Schiffner, R.; Kroegel, N.; Rupprecht, S.; Schlattmann, P.; Schulze, P.C.; Franzke, P.; Witte, O.W.; Schwab, M.; et al. Rapid Increases in Nitrogen Oxides Are Associated with Acute Myocardial Infarction: A Case-Crossover Study. Eur. J. Prev. Cardiol. 2018, 25, 1707–1716. [Google Scholar] [CrossRef]
- Collart, P.; Dubourg, D.; Leveque, A.; Sierra, N.B.; Coppieters, Y. Short-Term Effects of Nitrogen Dioxide on Hospital Admissions for Cardiovascular Disease in Wallonia, Belgium. Int. J. Cardiol. 2018, 255, 231–236. [Google Scholar] [CrossRef]
- Vidale, S.; Arnaboldi, M.; Bosio, V.; Corrado, G.; Guidotti, M.; Sterzi, R.; Campana, C. Short-Term Air Pollution Exposure and Cardiovascular Events: A 10-Year Study in the Urban Area of Como, Italy. Int. J. Cardiol. 2017, 248, 389–393. [Google Scholar] [CrossRef]
- Barbara, K.B.; Atkinson, R.W.; Milojevic, A.; Heal, M.R.; Doherty, R.M.; Armstrong, B.G.; Mackenzie, L.A.; Vieno, M.; Lin, C.; Wilkinson, P. Myocardial Infarction, ST-Elevation and Non-ST-Elevation Myocardial Infarction and Modelled Daily Pollution Concentrations: A Case-Crossover Analysis of MINAP Data. Open Heart 2016, 3, e000429. [Google Scholar] [CrossRef]
- Comparateur de Territoire—Commune de Strasbourg (67482). Available online: https://www.insee.fr/fr/statistiques/1405599?geo=COM-67482 (accessed on 6 March 2018).
- MONICA Manual. Available online: https://thl.fi/publications/monica/manual/ (accessed on 8 April 2018).
- Bard, D.; Kihal, W.; Schillinger, C.; Fermanian, C.; Segala, C.; Glorion, S.; Arveiler, D.; Weber, C. Traffic-Related Air Pollution and the Onset of Myocardial Infarction: Disclosing Benzene as a Trigger? A Small-Area Case-Crossover Study. PLoS ONE 2014, 9, e100307. [Google Scholar] [CrossRef] [PubMed]
- Bilan_de_la_Qualite_de_2.pdf. Available online: http://www.atmo-alsace.net/medias/produits/Bilan_de_la_qualite_de_2.pdf (accessed on 5 April 2018).
- Milojevic, A.; Wilkinsoon, P.; Armstrong, B.; Bhaskaran, K.; Smeeth, L.; Hajat, S. Short-Term Effects of Air Pollution on a Range of Cardiovascular Events in England and Wales: Case-Crossover Analysis of the MINAP Database, Hospital Admissions and Mortality. Heart 2014, 100, 1093–1098. [Google Scholar] [CrossRef] [PubMed]
- Roswall, N.; Raaschou-Nielsen, O.; Ketzel, M.; Gammelmark, A.; Overvad, K.; Olaen, A.; Sorensen, M. Long-Term Residential Road Traffic Noise and NO2exposure in Relation to Risk of Incident Myocardial Infarction—A Danish Cohort Study. Environ. Res. 2017, 156, 80–86. [Google Scholar] [CrossRef]
- Short Term Exposure to Air Pollution and Stroke: Systematic Review and Meta-Analysis. Available online: https://www-ncbi-nlm-nih-gov.scd-rproxy.u-strasbg.fr/pmc/articles/PMC4373601/ (accessed on 9 April 2018).
- Nicholas, L.M.; Törnqvist, H.; Robinson, S.D.; Gonzalez, M.; Darnley, K.; MacNee, W.; Boon, N.A.; Donaldson, K.; Blomberg, A.; Sandstrom, T.; et al. Diesel Exhaust Inhalation Causes Vascular Dysfunction and Impaired Endogenous Fibrinolysis. Circulation 2005, 112, 3930–3936. [Google Scholar] [CrossRef]
- Rückerl, R.; Greven, S.; Ljungman, P.; Aalto, P.; Antoniades, C.; Bellander, T.; Berglind, N.; Chrysohoou, C.; Forastiere, F.; Jacquemin, B.; et al. Air Pollution and Inflammation (Interleukin-6, C-Reactive Protein, Fibrinogen) in Myocardial Infarction Survivors. Environ. Health Perspect. 2007, 115, 1072–1080. [Google Scholar] [CrossRef]
- Andrew, J.L.; Lundbäck, M.; Mills, N.L.; Faratian, D. Diesel Exhaust Inhalation Increases Thrombus Formation in Man. Eur. Heart J. 2008, 29, 3043–3051. [Google Scholar] [CrossRef]
- Gibelin, P. Météo et saisons influencent-elles notre cœur? La Presse Médicale 2015, 44, 821–827. [Google Scholar] [CrossRef]
- Trends of Myocardial Infarction Morbidity and Its Associations with Weather Conditions-ScienceDirect. Available online: https://www-sciencedirect-com.scd-rproxy.u-strasbg.fr/science/article/pii/S1010660×14000524 (accessed on 4 April 2018).
- Nagarajan, V.; Fonarow, G.C.; Ju, C.; Pencina, M.; Laskey, W.K.; Maddox, T.M.; Hernandez, A.; Bhatt, D.L. Seasonal and Circadian Variations of Acute Myocardial Infarction: Findings from the Get with the Guidelines–Coronary Artery Disease (GWTG-CAD) Program. Am. Heart J. 2017, 189, 85–93. [Google Scholar] [CrossRef]
- Swampillai, J.; Wijesinghe, N.; Sebastian, C.; Devlin, G.P. Seasonal Variations in Hospital Admissions for ST-Elevation Myocardial Infarction in New Zealand. Cardiol. Res. 2012, 3, 205–208. [Google Scholar] [CrossRef][Green Version]
- Smeeth, L.; Thomas, S.L.; Hall, A.J.; Hubbard, R.; Farrington, P.; Vallance, P. Risk of Myocardial Infarction and Stroke after Acute Infection or Vaccination. N. Engl. J. Med. 2004, 351, 2611–2618. [Google Scholar] [CrossRef] [PubMed]
| Diagnostic Categories | Number of Coronary Events (% of Total Events) |
|---|---|
| 1 Myocardial infarction characterized | 243 (19.2%) |
| 2 Probable coronary death | 74 (5.8%) |
| 3 Sudden death in less than 24 h | 172 (13.6%) |
| 4 Acute Coronary Syndrome | 443 (35%) |
| 5 Unstable angina | 159 (12.6%) |
| 6 Other acute form of ischemic heart disease | 174 (13.9%) |
| Daily Coronary Events | Days (%) |
|---|---|
| 0 | 353 (32.2%) |
| 1 | 372 (33.9%) |
| 2 | 261 (23.8%) |
| 3 | 83 (7.6%) |
| 4 | 18 (1.6%) |
| 5 | 6 (0.5%) |
| 6 | 2 (0.2%) |
| 7 | 0 |
| 8 | 1 (0.1%) |
| Pollutant | Mean | SD | Min | Q1 | Med | Q3 | Max | IQR |
|---|---|---|---|---|---|---|---|---|
| NO2 | 34.68 | 12.53 | 9.67 | 25.33 | 33.33 | 41.67 | 92.67 | 16.33 |
| PM2.5 | 17.49 | 10.60 | 2 | 10 | 15 | 22 | 66 | 12 |
| PM10 | 23.82 | 13.30 | 5,5 | 14 | 21.5 | 30.5 | 87.5 | 16.5 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vaudrey, B.; Mielcarek, M.; Sauleau, E.; Meyer, N.; Marchandot, B.; Moitry, M.; Robellet, P.; Reeb, T.; Jesel, L.; Ohlmann, P.; et al. Short-Term Effects of Air Pollution on Coronary Events in Strasbourg, France—Importance of Seasonal Variations. Med. Sci. 2020, 8, 31. https://doi.org/10.3390/medsci8030031
Vaudrey B, Mielcarek M, Sauleau E, Meyer N, Marchandot B, Moitry M, Robellet P, Reeb T, Jesel L, Ohlmann P, et al. Short-Term Effects of Air Pollution on Coronary Events in Strasbourg, France—Importance of Seasonal Variations. Medical Sciences. 2020; 8(3):31. https://doi.org/10.3390/medsci8030031
Chicago/Turabian StyleVaudrey, Baptiste, Marie Mielcarek, Erik Sauleau, Nicolas Meyer, Benjamin Marchandot, Marie Moitry, Pierre Robellet, Thierry Reeb, Laurence Jesel, Patrick Ohlmann, and et al. 2020. "Short-Term Effects of Air Pollution on Coronary Events in Strasbourg, France—Importance of Seasonal Variations" Medical Sciences 8, no. 3: 31. https://doi.org/10.3390/medsci8030031
APA StyleVaudrey, B., Mielcarek, M., Sauleau, E., Meyer, N., Marchandot, B., Moitry, M., Robellet, P., Reeb, T., Jesel, L., Ohlmann, P., Bourdrel, T., & Morel, O. (2020). Short-Term Effects of Air Pollution on Coronary Events in Strasbourg, France—Importance of Seasonal Variations. Medical Sciences, 8(3), 31. https://doi.org/10.3390/medsci8030031





