1. Introduction
A significant increase in the number of computed tomography (CT) scanners has highlighted the need to reduce the amount of radiation used in them [
1]. While the evolution of the CT technique has resulted in the enhanced diagnosis of disease, its disadvantage has been the corresponding radiation dosage [
2]. Numerous analysts have suggested rational scan protocols for regular CT investigations and expressed a desire for the various manufacturers to guarantee high image quality using less radiation [
3,
4]. Consequently, radiation doses can now be lowered without sacrificing diagnostic details in the image [
3]. One solution for improving image quality at low-radiation levels has relied on progress being made in the rebuilding methods [
5,
6,
7,
8], among which iterative reconstruction (IR) algorithms are commonly used. In addition, several studies have recommended that low-contrast detail (LCD) detection capability might be the most suitable method for standardising images [
9,
10,
11]. LCD refers to the capability of a CT scan to differentiate between various objects that have similar X-ray attenuation coefficients. The most serious and noteworthy challenge in this aspect is that techniques utilising low dose decline the detectible performance of LCD, uniquely in abdomen examinations. For example, carcinogenic disease of the liver is customarily demonstrated as low-attenuation lesions inside a background of slightly higher attenuation normal tissue. Detectible capacity of LCD must be preserved with any dose-reduction strategy. Contrast-to-noise ratio (CNR) is an important tool used to determine image quality. It is a measure of image quality established on a contrast. Prior studies have shown that images obtained using hybrid-type IR (HIR) algorithms, which comprise the majority of various accessible IR procedures, are able to maintain image standards using a decrease in radiation of 20–25% to 65–67%, although some image noise and artefacts remain [
12,
13]. Recently, iterative-type model reproduction (IMR), an information-based IR calculation, has enabled an additional decrease in radiation dosage with enhanced image representation, although this has resulted in a notable decrease in contrast and a suppression of artefacts that are differentiated into filtered back projection in the period.
Filtered back projection (FBP) and HIR calculations in LCD scans [
14,
15,
16,
17,
18]. The two foremost methods—subjective and objective—are accessible for computing the LCD of various CT images [
19]. The subjective technique depends on human perception, and the objective one is based on quantitative measurements of contrast-to-noise ratio (CNR) [
9]. Because of the subjectivity of human observers, the objective way is considered to be more suitable for dealing with estimating LCD execution. In this study, we aimed to assess the impacts of the settings—essentially, milliampere-second (mAs) and Kilovoltage peak (kVp)—on the LCD of CT scanners. The strategy used was based on the CNR estimations of scanned objects. We also examined the differences between different CT scanners, in terms of the CNR estimations of those scanned objects. Our overarching aim was thus to evaluate the methodology used in CNR measurements in order to assess image quality in terms of the detectability of LCD in CT images.
3. Results
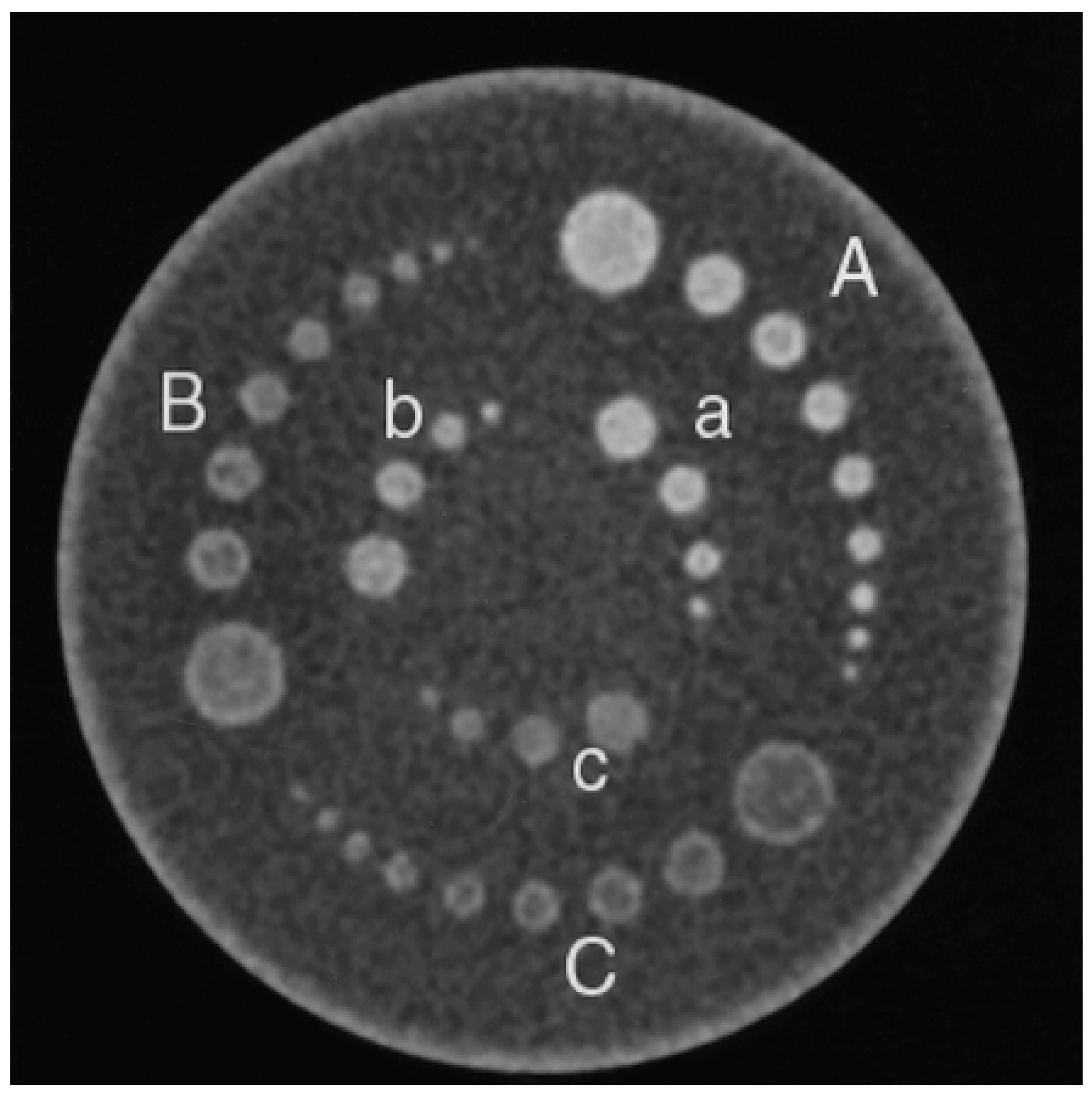
The effects of the size of the objects, with 1% contrast level, on CNR values were evaluated for different MDCT scanners, reconstruction algorithms, object contrast levels and mAs selections (
Figure 2 and
Table 3 and
Table 4). Changes in the CNR values for 16-MDCT with 8-mm object size and for 80-MDCT with 5-mm object size can be seen in
Figure 2. Data from the soft-tissue and reproducing-algorithm images and objects at 1% contrast are recorded in
Table 3 and
Table 4.
The effects of object size on the CNR values were examined at first. Object size in relation to different scanners, reconstruction calculations, levels of object contrast and mAs was also scrutinised. The effect of the reconstruction calculations, mAs, kVp and section thickness on the CNR data were then assessed. The output of the various scanners was then compared, based on the CNR values.
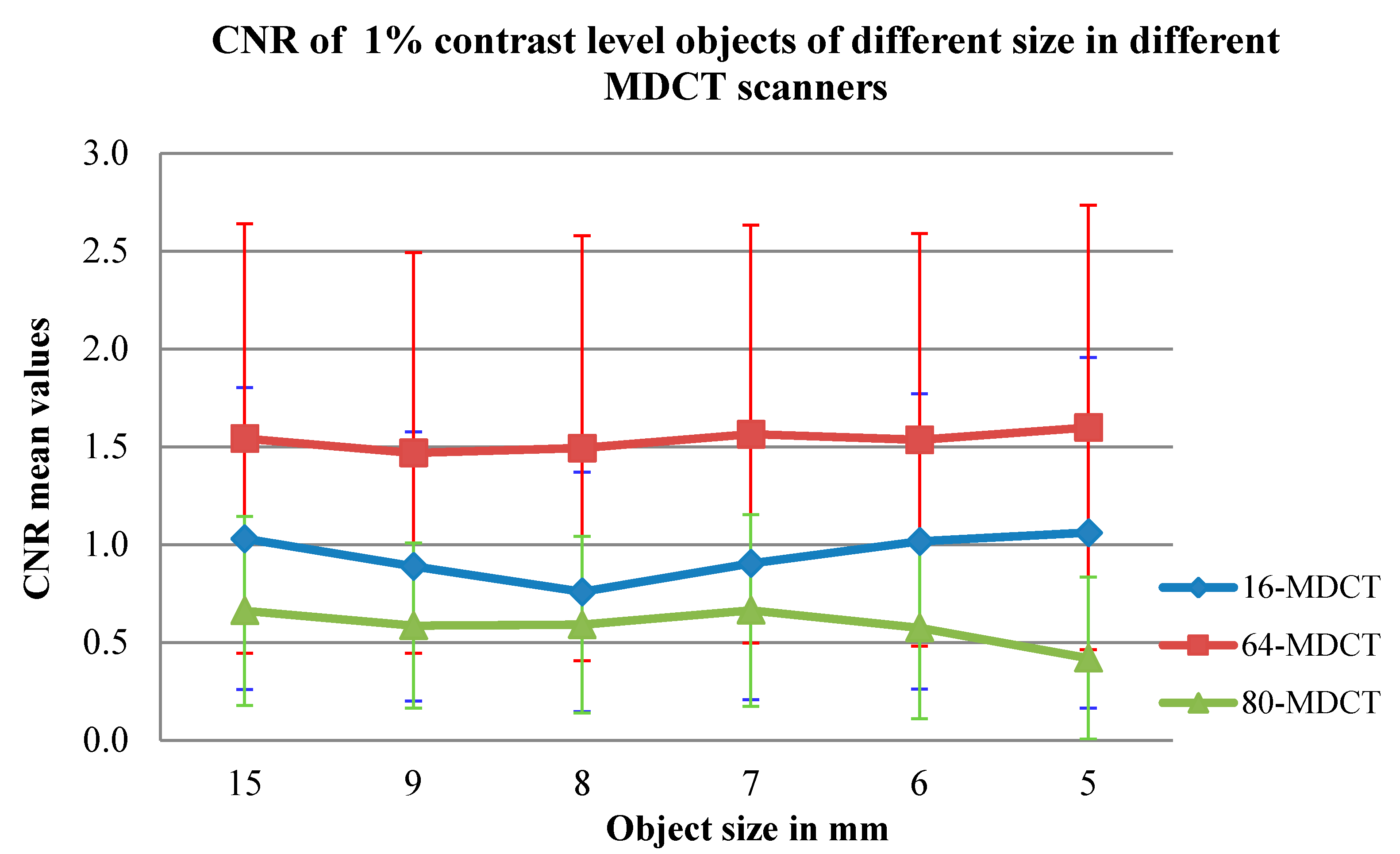
3.1. Effect of Object Size on CNR Values
The effect of object size on the CNR values, at a 1% contrast level, was assessed for each MDCT scanner, for the various reconstruction calculations, contrast levels on the objects and mAs values. It was found that negligible variations in the mean CNR values occurred for the objects of various sizes across all scanners (
p value > 0.1) (see
Table 5), but there were considerable variations (
p value = 0.021) between the 5- and 8-mm objects at 1% contrast in the 16-MDCT. In the 64-MDCT, there was always a negligible difference in CNR values among the objects of different dimensions. In the 80-MDCT, there were significant contrasts in the CNR values between a 5-mm object and the 8- and 15-mm objects.
3.2. Impact of Image Reconstruction Calculations on CNR Values
In the 64-MDCT and corresponding 16-MDCT, the CNR values for the reconstructed soft-tissue images were substantially higher than those for the corresponding lung images (p value < 0.001). The soft-tissue images had impressively higher CNR values than the standard images in the 16-MDCT and 64-MDCT (p values = 0.011 and <0.001, respectively). In the 80-MDCT, however, the standard images had much higher CNR estimates than the other types of images (p value < 0.001).
3.3. Impact of kVp on CNR Values
Using a higher kVp gave higher CNR values in all CT scanners. There were critical increases in the CNR values when the kVp was increased from 80 to 120 (
Table 6). On the other hand, there was little separation between the CNR values at levels of 80 and 120 kVp at 10 mAs and corresponding 0.625-mm section thickness (
p value = 1) within the 16-MDCT. Considering 100 mAs and corresponding 0.625 mm, there were, however, inconsequential distinctions in the CNR values when the kVp was increased to 120 (
p value = 0.894). Considering the 64-MDCT, wide variations in the CNR values were seen when the kVp was elevated from 80 to 120 kVp, as well as one significant occurrence at 20 mAs and 0.625-mm thickness (
p value < 0.639). In the 80-MDCT, there were insignificant increases in the CNR values at 10 and 20 mAs for each section during kVp increment from 80 to 120 kVp. Considering 50 mAs and 0.5- and 1-mm section thicknesses, there were inconsequential elevations occurring to the CNR values (
p values = 0.51 and 0.77, respectively) for elevations from 80 to 120 kVp. In addition, further increments in the CNR values at 80 and 120 kVp were seen at 100 mAs and 0.5-mm section thickness (the
p value = 0.81).
3.4. Impact of mAs on CNR Values
Increased mAs levels increased the CNR values, especially at higher section thicknesses, in all CT scanners. Several significant increases in CNR values occurred when the mAs was increased from 10 to 20 mAs, initially, and then to 50, 100 or 200 mAs (
Table 7). Ultimately, there was inconsequential variations in the values of CNR between 10 and 20 mAs, especially at the lowest kVp and with progressively more thinner thicknesses (the
p value > 0.1) in all corresponding CT scanners. Considering the 16-MDCT, there were inconsequential variations at 10 and 50 mAs as well as at 80 kVp, when using 0.625- and 1.25-mm thicknesses of the sections (
p values = 0.914 and 0.244). Considering 120 kVp, there were inconsequential changes in the values of CNR at 10 and 20 mAs as well as with 0.625, 1.25 and 2.5 mm thicknesses (the
p values = 0.76, 1 and 0.6, respectively). In the 64-MDCT, insignificant variations were present between images at 10 and 20 mAs and 120 kVp, with a 0.625-mm section thickness (
p value = 0.781). In the 80-MDCT, there were insignificant variations between images at 10 and 50 mAs and 120 kVp, with a 1.25-mm thickness (
p value = 0.643).
3.5. Impact of Section Thickness on CNR Values
Thicker sections produced increased CNR values in almost all the CT scanners. Several significant increases in CNR values occurred when the section thickness was increased from 0.625 to 1.25, 2.5 or 5 mm (
Table 8). In the 16-MDCT, there was insignificant differentiation between the CNR values for the 0.625- and 1.25-mm section thicknesses at 20, 50 and 100 mAs and 80 kVp, as well as at 10, 20, 50 and 200 mAs and 120 kVp. There were also inconsequential differences when comparing the images with 0.625- and 1.25-mm section thicknesses at 20, 50, 100 and 200 mAs and 80 kVp, as well as at 10, 20, 50 and 200 mAs and 120 kVp. Inconsequential peaks were seen between the images utilising 0.625- and 2.5-mm section thicknesses at 10 and 50 mAs and 80 kVp, as well as at 10, 20 and 50 mAs and 120 kVp. In addition, there were inconsequential peaks between the images using 0.625- and 5-mm section thicknesses at 10 mAs and 80 and 120 kVp (
Table 8). In the 64-MDCT, there were inconsequential variations in the CNR values in some places for the 0.625- and 1.25-mm thicknesses and for the 0.625- and 2.5-mm thicknesses at 10 and 20 mAs and 80 kVp. There were similarly inconsequential distinctions between images for the 0.625- and 1.25-mm thicknesses at 100 mAs and 80 kVp (
p value = 0.138). There were also insignificant distinctions between the images of the 0.625- and 1.25-mm section thicknesses at 10 mAs and 120 kVp (
Table 8).
Considering the 80-MDCT, inconsequential distinctions were present between the images of the 0.5- and 1-mm thicknesses at 20, 50 and 200 mAs and kVp of 80. In addition, there were inconsequential peaks between images of the 0.5- and 2-mm thicknesses when considered at 50 mAs and 80 kVp, as well as insignificant distinctions between images of the 0.5- and 1-mm section thicknesses at 20, 50, 100 and 200 mAs and 120 kVp. Inconsequential peaks were also seen between images of the 0.5- and 2-mm thicknesses at 120 kVp and 10 mAs (
Table 8).
3.6. Correlation between Scanners Based on CNR Values
With respect to the CNR values, the 64-MDCT worked as well as the other CT scanners, although the 16-MDCT produced higher CNR values than the 64-MDCT at 80 kVp and 10 mAs with a 1.25-mm section thickness. The 16-MDCT generally worked better than the 80-MDCT, although the 80-MDCT (
Figure 2) produced better CNR values than the 16-MDCT at 80 kVp and 10 mAs with a 2.5-mm section thickness, at 80 kVp and 20 mAs with various cut thicknesses and at 80 kVp and 50 mAs with a 2.5-mm section thickness. Large variations were found between the 16-MDCT and 64-MDCT scanners, having certain exceptions: at 10 mAs and 80 kVp with 0.625- or 1.25-mm section thicknesses and at 50 mAs and 120 kVp with a 0.625-mm section thickness (
Table 9). Basic differences were also seen in the CNR values between the 16-MDCT and the 80-MDCT scanners at low introduction factors: at 10 mAs and 80 kVp with 2.5- or 5-mm section thicknesses, at 20 mAs and 80 kVp with various section thickness; and at 50 mAs and 80 kVp with 0.625-mm/0.5-mm and 1.25-mm/1-mm section thicknesses. Change in CNR values at 10 mAs among 1-, 2- and 5-mm slice thickness images can be seen in
Figure 3. The distinction in CNR values between the 64-MDCT and 80-MDCT scanners were continually basic. The 64-MDCT not only produced higher CNR values than the other scanners, it furthermore provided superior linearity in the CNR values, which increased with elevated mAs, kVp and section thickness.
4. Discussion
The effect of object size on CNR values was examined from various angles, in terms of scanner type, reconstruction calculation, contrast level of the object and mAs. The outcomes of the modifying factors—mAs, kVp and section thickness—on the values of CNR were also investigated, and the operation of the various scanners, based on the CNR values, were compared and correlated.
It was seen that the CNR values were considerably affected by adjusting the image reconstruction calculations. Although it was seen that the CNR values were high in the upper level in the soft-tissue reconstruction images in the 16-MDCT and 64-MDCT scanners, some CNR values were found to be higher in the standard reconstruction images than in the other types of algorithmic reconstruction images in the 80-MDCT scanner. This accords with the findings of several different studies [
22,
23]. As found by Kalender and Khadivi [
1], changing the algorithmic reconstruction produces different trademark pixel sound estimates, which are characterised by the reconstruction. For example, a normal pixel sound for soft tissue is 62.1 HU, while, for standard and high-goal parts, they are 31.5 and 57.5 HU, respectively, for a 1- and 32-mm section thickness. The sound level of CT images is a significant factor, compared to the location of LCD objects [
1,
24]. The outcomes do not show any noteworthy changes in the CNR values among other object estimates, down to the smallest measurable object (5 mm). It was observed that the ability to identify objects depends on the differentiation standard of the object, as well as its size [
19,
20,
21,
22,
23,
24,
25,
26]. Step-by-step instructions to control undefined, minor lesions (e.g., nodules in CT lung screening) have become a significant concern. Although most very small nodules are benign, a few will end up being cancer-causing [
27]. Some minor lesions, (e.g., small-cell carcinomas) grow in rapid increments, with a mean volume multiplying time of around 149 days [
28]. Consequently, early intervention is vital to implement treatment [
27]. The exact measurement and precise identification of the size of pulmonary nodules and various injuries are necessary in various clinical cases. This allows monitoring of the impacts of chemotherapy and injury development at follow-up, which may reveal risk [
29]. An appraisal method based on estimated CNR values is not good enough to determine the consequences of object size on the capacity of the LCD.
Overall, a higher kVp produced superior CNR values in all the CT scanners. Specifically, there were critical elevations in CNR values when the voltage was elevated from 80 to 120 kVp. The impacts of kVp on the quality of image relative to the CNR values were as anticipated, with elevating kVp increasing photon entrance and the radiation portion when the other factors were notably fixed, even though the radiation portion is not straight with kVp. Subsequently, the noise is diminished and the CNR is increased [
9,
30].
Higher mAs levels mainly produced better CNR values, especially for thicker sections. As expected, the CNR is improved with increasing mAs because this decreases the image noise. The radiation portion is directly related to the mAs [
31,
32]. With thicker sections, the CNR values mostly got elevated. The impact of section thickness on the imaging ability of the CT scanners was anticipated because thicker sections decrease image noise so the image quality improves [
33]. As indicated above, there were inconsequential differences in the CNR values for the 0.625-mm/0.5-mm and 1.25-mm/1-mm section thicknesses at all mAs levels, as well as between the 0.625-mm/0.5-mm and 2.5-mm/2-mm section thicknesses, especially at lower introduction factors. The noise elevates with thinner slices if the radiation dose is not allowed to escalate [
9,
30,
33]. In any case, thinner sections give high-goal, isotropic image informational indices, and subsequently the through-plane, incomplete-volume averaging impacts are limited and the image is upgraded [
1,
34,
35].
With respect to the CNR value estimations, the 64-MDCT scanner worked the best, whilst the 16-MDCT scanner worked better than the 80-MDCT scanner, for the most part. There were important and consequential differences between the 16-MDCT and 64-MDCT scanners. The specific properties and framework specifications of each scanner determined their imaging capabilities. The CT scanner manufacturer, model, geometry, tube details and locator configuration all determine the noise and image clarity, which all influence the imaging and image quality [
9,
26,
36]. This study was restricted by using only one scanner arrangement, from one manufacturer, and by the smallest quantifiable object being 5 mm in diameter.
5. Conclusions
The LCD assessment technique, based on the CNR values, was sensitive to the quantification of the impacts of kVp, mAs and section thickness on image quality. This technique was also successful in assessing the impacts on image quality of various reconstruction calculations and objects at different levels, based on the CNR values. However, it should be noted that the smallest object size that could be estimated, using this technique with the Catphan® 600, was 5 mm. Smaller objects could not be distinguished with any precision without estimating the outside of the object in order to determine the object’s mean CT value. In that respect, no notable CNR changes were found between various object sizes. Thus, LCD perceptibility is not only dictated by object differentiation, but also by object size. Therefore, this method is not an appropriate method to measure LCD detectability performance. It is also not possible for this phantom design to appraise an object of the same size and contrast at different position levels inside the phantom. It is a time consuming, inconvenient and vexatious as it necessitates scrutiny of an immensely vast quantity of data. Furthermore, authenticity of this technique is comparatively low as human eyewitnesses were not incorporated in the procedure. Thus, utilisation of Catphan® 600 should not be considered as an appurtenant apparatus for image optimisation intentions and regularly based appraisals. In addition, volume CT dose index (CTDIvol), which is a systematised calculation of the radiation output coming out of a CT system, that permits users to find out the quantity of radiation emitted and equates the radiation output between various scanners, can be considered in future research. Another point to be mentioned is that the dose–length product (DLP), which is directly connected to the patient (stochastic) dangers, can also be utilised for future similar research.