Evaluating Self-Directed Rehabilitation for Knee and Hip Arthroplasty During the COVID-19 Pandemic: A Multicenter Study
Abstract
1. Introduction
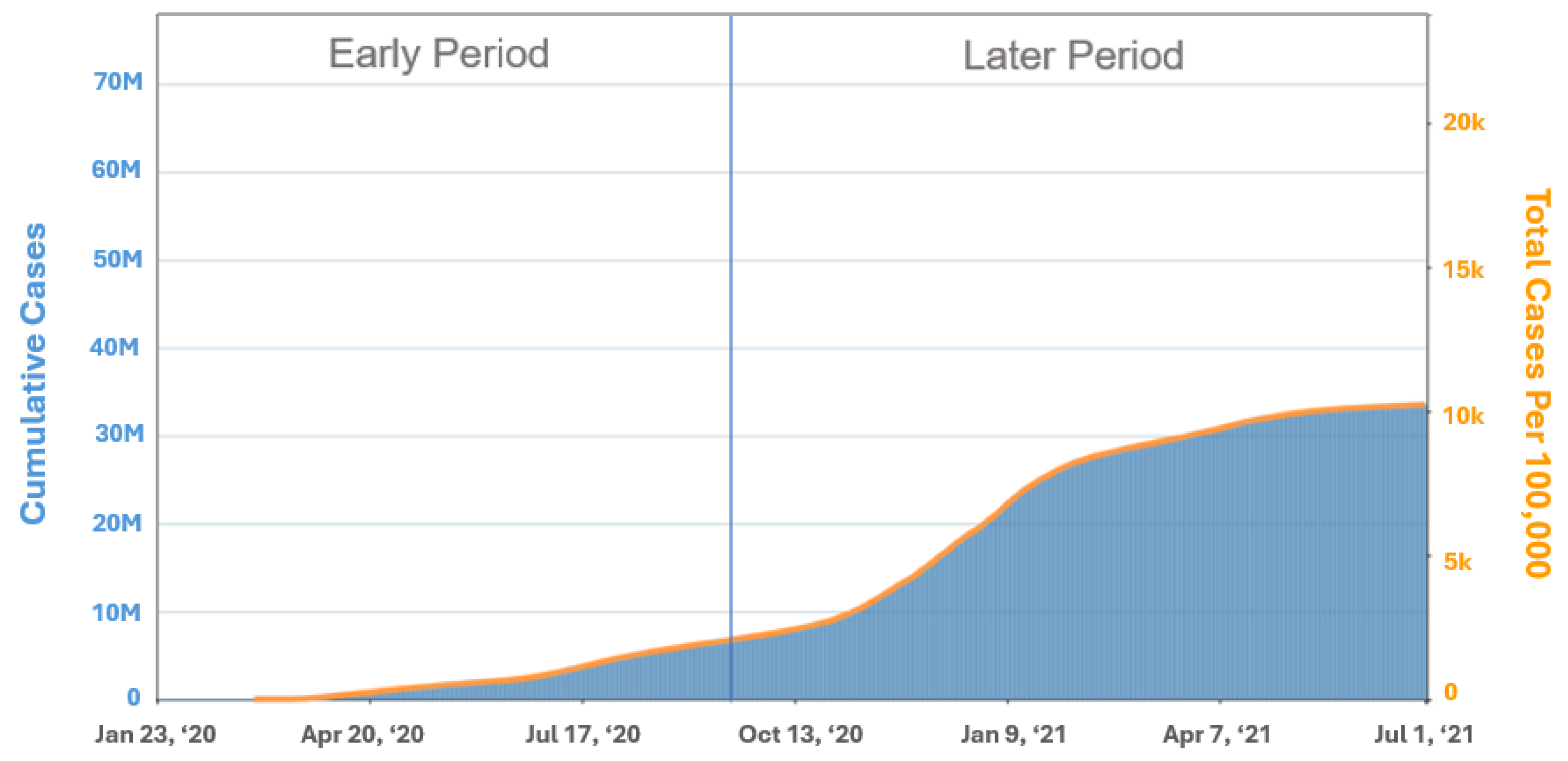
2. Methods
Statistical Analysis
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Moreland, A.; Herlihy, C.; Tynan, M.A.; Sunshine, G.; McCord, R.F.; Hilton, C. Timing of state and territorial COVID-19 stay-at-home orders and changes in population movement—united states, March 1–May 31, 2020. MMWR Morb. Mortal. Wkly. Rep. 2020, 69, 1198–1203. [Google Scholar] [CrossRef] [PubMed]
- Alpalhao, V.; Alpalhao, M. Impact of COVID-19 on physical therapist practice in portugal. Phys. Ther. 2020, 100, 1052–1053. [Google Scholar] [CrossRef]
- Battista, S.; Dell’Isola, A.; Manoni, M.; Englund, M.; Palese, A.; Testa, M. Experience of the COVID-19 pandemic as lived by patients with hip and knee osteoarthritis: An italian qualitative study. BMJ Open 2021, 11, e053194. [Google Scholar] [CrossRef]
- Miller, M.J.; Pak, S.S.; Keller, D.R.; Barnes, D.E. Evaluation of pragmatic telehealth physical therapy implementation during the COVID-19 pandemic. Phys. Ther. 2021, 101, pzaa193. [Google Scholar] [CrossRef] [PubMed]
- Bosworth, A.; Ruhter, J.; Samson, L.W.; Sheingold, S.; Taplin, C.; Tarazi, W.; Zuckerman, R. Medicare Beneficiary Use of Telehealth Visit: Early Data from the Start of the COVID-19 Pandemic; Office of the Assistant Secretary for Planning and Evaluation USDoHaHS: Washington, DC, USA, 2020. [Google Scholar]
- Tenforde, A.S.; Borgstrom, H.; Polich, G.; Steere, H.; Davis, I.S.; Cotton, K.; O’donnell, M.M.; Silver, J.K. Outpatient physical, occupational, and speech therapy synchronous telemedicine: A survey study of patient satisfaction with virtual visits during the COVID-19 pandemic. Am. J. Phys. Med. Rehabil. 2020, 99, 977–981. [Google Scholar] [CrossRef] [PubMed]
- Barton, C.; Ezzat, A.; Merolli, M.; Williams, C.; Haines, T.; Mehta, N.; Malliaras, P. “It’s second best”: A mixed-methods evaluation of the experiences and attitudes of people with musculoskeletal pain towards physiotherapist delivered telehealth during the COVID-19 pandemic. Musculoskelet. Sci. Pract. 2022, 58, 102500. [Google Scholar] [CrossRef]
- Bennell, K.L.; Lawford, B.J.; Metcalf, B.; Mackenzie, D.; Russell, T.; Berg, M.v.D.; Finnin, K.; Crowther, S.; Aiken, J.; Fleming, J.; et al. Physiotherapists and patients report positive experiences overall with telehealth during the COVID-19 pandemic: A mixed-methods study. J. Physiother. 2021, 67, 201–209. [Google Scholar] [CrossRef]
- Cliffe, S.; Stevenson, K. Patient experiences of virtual consultation during COVID-19: A musculoskeletal service evaluation. Musculoskelet. Care 2021, 19, 380–383. [Google Scholar] [CrossRef]
- La Rosa, G.; Frizziero, A.; Roi, G.S. Musculoskeletal telerehabilitation experience during the 70 days of COVID-19 lockdown in italy. Eur. J. Phys. Rehabil. Med. 2022, 58, 151–153. [Google Scholar] [CrossRef]
- Ku, B.P.S.; Tse, A.W.S.; Pang, B.C.H.; Cheung, N.T.; Pang, J.Y.W.; Chan, J.K.Y.; Hui, H.L.; Chu, D.; Choi, K.H.W. Tele-rehabilitation to combat rehabilitation service disruption during COVID-19 in hong kong: Observational study. JMIR Rehabil. Assist. Technol. 2021, 8, e19946. [Google Scholar] [CrossRef]
- Bearne, L.M.; Gregory, W.J.; Hurley, M.V. Remotely delivered physiotherapy: Can we capture the benefits beyond COVID-19? Rheumatology 2021, 60, 1582–1584. [Google Scholar] [CrossRef] [PubMed]
- Landry, M.D.; Geddes, L.; Moseman, A.P.; Lefler, J.P.; Raman, S.R.; van Wijchen, J. Early reflection on the global impact of COVID-19, and implications for physiotherapy. Physiotherapy 2020, 107, A1–A3. [Google Scholar] [CrossRef] [PubMed]
- Sloan, M.; Premkumar, A.; Sheth, N.P. Projected volume of primary total joint arthroplasty in the U.S., 2014 to 2030. J. Bone Jt. Surg. Am. 2018, 100, 1455–1460. [Google Scholar] [CrossRef]
- McKeon, J.F.; McKeon, J.F.; Alvarez, P.M.; Alvarez, P.M.; Vajapey, A.S.; Vajapey, A.S.; Sarac, N.; Sarac, N.; Spitzer, A.I.; Spitzer, A.I.; et al. Expanding role of technology in rehabilitation after lower-extremity joint replacement: A systematic review. JBJS Rev. 2021, 9, e21. [Google Scholar] [CrossRef]
- Austin, M.S.; Urbani, B.T.; Fleischman, A.N.; Fernando, N.D.; Purtill, J.J.; Hozack, W.J.; Parvizi, J.; Rothman, R.H. Formal physical therapy after total hip arthroplasty is not required: A randomized controlled trial. J. Bone Jt. Surg. Am. 2017, 99, 648–655. [Google Scholar] [CrossRef]
- Cottrell, M.A.; Galea, O.A.; O’Leary, S.P.; Hill, A.J.; Russell, T.G. Real-time telerehabilitation for the treatment of musculoskeletal conditions is effective and comparable to standard practice: A systematic review and meta-analysis. Clin. Rehabil. 2017, 31, 625–638. [Google Scholar] [CrossRef] [PubMed]
- Suso-Martí, L.; La Touche, R.; Herranz-Gómez, A.; Angulo-Díaz-Parreño, S.; Paris-Alemany, A.; Cuenca-Martínez, F. Effectiveness of telerehabilitation in physical therapist practice: An umbrella and mapping review with meta-meta-analysis. Phys. Ther. 2021, 101, pzab075. [Google Scholar] [CrossRef]
- Crawford, D.A.; Duwelius, P.J.; Sneller, M.A.; Morris, M.J.; Hurst, J.M.; Berend, K.R.; Lombardi, A.V. 2021 mark coventry award: Use of a smartphone-based care platform after primary partial and total knee arthroplasty: A prospective randomized controlled trial. Bone Jt. J. 2021, 103-B (Suppl. A), 3–12. [Google Scholar] [CrossRef]
- Crawford, D.A.; Lombardi, A.V.; Berend, K.R.; Huddleston, J.I.; Peters, C.L.; DeHaan, A.; Zimmerman, E.K.; Duwelius, P.J. Early outcomes of primary total hip arthroplasty with use of a smartphone-based care platform: A prospective randomized controlled trial. Bone Jt. J. 2021, 103-B (Suppl. B), 91–97. [Google Scholar] [CrossRef]
- Tripuraneni, K.R.; Foran, J.R.; Munson, N.R.; Racca, N.E.; Carothers, J.T. A smartwatch paired with a mobile application provides postoperative self-directed rehabilitation without compromising total knee arthroplasty outcomes: A randomized controlled trial. J. Arthroplast. 2021, 36, 3888–3893. [Google Scholar] [CrossRef]
- Bäcker, H.C.; Wu, C.H.; Schulz, M.R.G.; Weber-Spickschen, T.S.; Perka, C.; Hardt, S. App-based rehabilitation program after total knee arthroplasty: A randomized controlled trial. Arch. Orthop. Trauma Surg. 2021, 141, 1575–1582. [Google Scholar] [CrossRef] [PubMed]
- Cdc Museum COVID-19 Timeline: Centers for Disease Control and Prevention. 2022. Available online: https://www.cdc.gov/museum/timeline/covid19.html#Early-2020 (accessed on 4 September 2021).
- Dierick, F.; Pierre, A.; Profeta, L.; Telliez, F.; Buisseret, F. Perceived usefulness of telerehabilitation of musculoskeletal disorders: A belgium-france pilot study during second wave of COVID-19 pandemic. Healthcare 2021, 9, 1605. [Google Scholar] [CrossRef] [PubMed]
- Flanagan, E.W.; Beyl, R.A.; Fearnbach, S.N.; Altazan, A.D.; Martin, C.K.; Redman, L.M. The impact of COVID-19 stay-at-home orders on health behaviors in adults. Obesity 2021, 29, 438–445. [Google Scholar] [CrossRef] [PubMed]
- Watson, K.B.; Whitfield, G.P.; Huntzicker, G.; Omura, J.D.; Ussery, E.; Chen, T.J.; Fanfair, R.N. Cross-sectional study of changes in physical activity behavior during the COVID-19 pandemic among us adults. Int. J. Behav. Nutr. Phys. Act. 2021, 18, 91. [Google Scholar] [CrossRef] [PubMed]
- Agostini, M.; Moja, L.; Banzi, R.; Pistotti, V.; Tonin, P.; Venneri, A.; Turolla, A. Telerehabilitation and recovery of motor function: A systematic review and meta-analysis. J. Telemed. Telecare 2015, 21, 202–213. [Google Scholar] [CrossRef]
- Latif-Zade, T.; Tucci, B.; Verbovetskaya, D.; Bialkin, E.; Ng, B.; Heddon, S.; Berteau, J.-P. Systematic review shows tele-rehabilitation might achieve comparable results to office-based rehabilitation for decreasing pain in patients with knee osteoarthritis. Medicina 2021, 57, 764. [Google Scholar] [CrossRef]
- Alsobayel, H.; Alodaibi, F.; Albarrati, A.; Alsalamah, N.; Alhawas, F.; Alhowimel, A. Does telerehabilitation help in reducing disability among people with musculoskeletal conditions? A preliminary study. Int. J. Environ. Res. Public Health 2021, 19, 72. [Google Scholar] [CrossRef]
- Roberts, A.; Johnston, G.H.; Landells, C. COVID-19: Pivoting from in-person to virtual orthopedic surgical evaluation. Can. J. Surg. 2021, 64, E101–E102. [Google Scholar] [CrossRef]
- Lee, E.C.; Grigorescu, V.; Enogieru, I.; Smith, S.R.; Samson, L.W.; Conmy, A.B.; De Lew, N. Updated National Survey Trends in Telehealth Utilization and Modality: 2021–2022 (Issue Brief No. HP-2023-09); Office of the Assistant Secretary for Planning and Evaluation, U.S. Department of Health and Human Services: Washington, DC, USA, 2023. [Google Scholar]
- Ferguson, S.L. Is the end of the pandemic the end of telerehabilitation? Phys. Ther. 2022, 102, pzac004. [Google Scholar] [CrossRef]
- Pylypchuk, Y.; Barker, W. Use of Telemedicine Among Office-Based Physicians, 2021; ONC Data Brief, no. 65; Office of the National Coordinator for Health Information Technology: Washington, DC, USA, 2021. [Google Scholar]
- Predmore, Z.S.; Roth, E.; Breslau, J.; Fischer, S.H.; Uscher-Pines, L. Assessment of patient preferences for telehealth in post-COVID-19 pandemic health care. JAMA Netw. Open 2021, 4, e2136405. [Google Scholar] [CrossRef]

| COVID-19 Pandemic Period | |||
|---|---|---|---|
| Early (n = 551) | Late (n = 1114) | p Value | |
| TKA | |||
| Age (years) | 65.1 ± 8.6 | 64.2 ± 9.0 | 0.177 |
| BMI (kg/m2) | 30.9 ± 6.3 | 31.6 ± 6.4 | 0.157 |
| Sex (% female) | 60.2% | 59.0% | 0.816 |
| PKA | |||
| Age (years) | 61.7 ± 8.7 | 61.8 ± 9.4 | 0.921 |
| BMI (kg/m2) | 30.5 ± 5.6 | 30.4 ± 6.3 | 0.982 |
| Sex (% female) | 53.6% | 64.4% | 0.192 |
| THA | |||
| Age (years) | 61.8 ± 10.2 | 62.1 ± 10.1 | 0.649 |
| BMI (kg/m2) | 29.5 ± 6.2 | 29.0 ± 6.2 | 0.379 |
| Sex (% female) | 56.3% | 47.0% | 0.024 |
| COVID-19 Pandemic Period | |||
|---|---|---|---|
| Early (n = 551) | Late (n = 1114) | p Value | |
| TKA | |||
| Pre | 4818.6 ± 3214.1 | 4655.7 ± 2965.8 | 0.494 |
| Post | 5352.1 ± 3003.1 | 5164.8 ± 2713.7 | 0.402 |
| PKA | |||
| Pre | 5869.1 ± 4370.3 | 4631.3 ± 3214.4 | 0.066 |
| Post | 6513.6 ± 3533.9 | 6215.0 ± 3228.7 | 0.588 |
| THA | |||
| Pre | 4789.9 ± 3315.8 | 4826.5 ± 3230.6 | 0.886 |
| Post | 6023.9 ± 3446.6 | 6093.1 ± 3366.6 | 0.808 |
| Pandemic Period | |||
|---|---|---|---|
| Early | Late | p Value | |
| TKA—KOOS JR | 17.70 | 18.36 | 0.544 |
| PKA—KOOS JR | 15.97 | 16.53 | 0.801 |
| THA—HOOS JR | 28.58 | 29.00 | 0.750 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Miner, T.M.; Anderson, M.B.; Van Andel, D.C.; Neher, R.E.; Redfern, R.E.; Duwelius, P.J. Evaluating Self-Directed Rehabilitation for Knee and Hip Arthroplasty During the COVID-19 Pandemic: A Multicenter Study. Med. Sci. 2024, 12, 69. https://doi.org/10.3390/medsci12040069
Miner TM, Anderson MB, Van Andel DC, Neher RE, Redfern RE, Duwelius PJ. Evaluating Self-Directed Rehabilitation for Knee and Hip Arthroplasty During the COVID-19 Pandemic: A Multicenter Study. Medical Sciences. 2024; 12(4):69. https://doi.org/10.3390/medsci12040069
Chicago/Turabian StyleMiner, Todd M., Mike B. Anderson, David C. Van Andel, Robert E. Neher, Roberta E. Redfern, and Paul J. Duwelius. 2024. "Evaluating Self-Directed Rehabilitation for Knee and Hip Arthroplasty During the COVID-19 Pandemic: A Multicenter Study" Medical Sciences 12, no. 4: 69. https://doi.org/10.3390/medsci12040069
APA StyleMiner, T. M., Anderson, M. B., Van Andel, D. C., Neher, R. E., Redfern, R. E., & Duwelius, P. J. (2024). Evaluating Self-Directed Rehabilitation for Knee and Hip Arthroplasty During the COVID-19 Pandemic: A Multicenter Study. Medical Sciences, 12(4), 69. https://doi.org/10.3390/medsci12040069






