Implications of Pleural Fluid Composition in Persistent Pleural Effusion following Orthotopic Liver Transplant
Abstract
1. Introduction
2. Materials and Methods
2.1. Design, Setting, and Population
2.2. Data Collection
2.3. Data Analysis
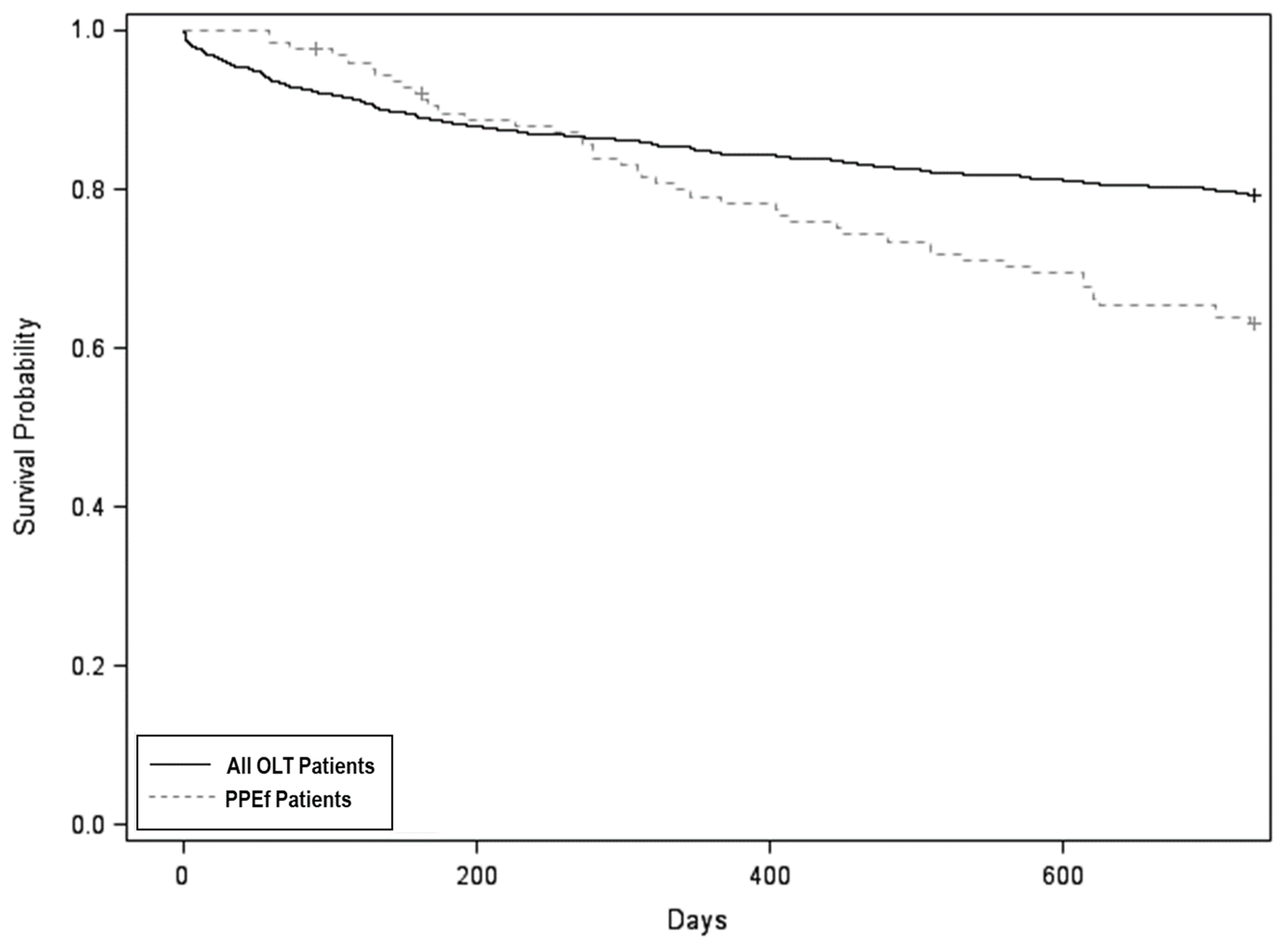
3. Results
3.1. Clinical Characteristics of OLT Recipients with PPEf
3.2. Predictors of 1-Year Mortality in PPEf Patients
3.3. Clinical Significance of Exudates Defined by Light’s Criteria
3.4. Clinical Significance of Protein—vs. LDH-Based Definition of Exudates
3.5. Significance of PF Cellular Content
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| All OLT (n = 1602) | PPEf (n = 124) | p-Value | |
|---|---|---|---|
| Age (years) a | 54.7 ± 11.2 | 55.0 ± 9.3 | 0.76 |
| Female b | 584 (36.5%) | 52 (41.9%) | 0.22 |
| MELD Score a | 26.4 ± 12.2 | 28.2 ± 12.7 | 0.12 |
Appendix B
| All PPEf (n = 124) | PPEf with PF Protein and LDH Data (n = 91) | p-Value | |
|---|---|---|---|
| Age (years) a | 55.0 ± 9.3 | 55.3 ± 8.8 | 0.82 |
| Female b | 52 (41.9%) | 37 (40.7%) | 0.89 |
| MELD Score a | 28.2 ± 12.7 | 28.2 ± 12.4 | 0.98 |
| Charlson Comorbidity Index a | 5.9 ± 1.8 | 5.9 ± 1.7 | 0.96 |
References
- Bozbas, S.S.; Eyuboglu, F.O.; Sevmis, S.; Karakayali, H.; Haberal, M. Pulmonary complications and mortality after liver transplant. Exp. Clin. Transplant. 2008, 6, 264–270. [Google Scholar] [PubMed]
- Pirat, A.; Özgur, S.; Torgay, A.; Candan, S.; Zeyneloğlu, P.; Arslan, G. Risk factors for postoperative respiratory complications in adult liver transplant recipients. Transplant. Proc. 2004, 36, 218–220. [Google Scholar] [CrossRef] [PubMed]
- Lin, Y.; Cai, Z.; Jiang, Y.; Lü, L.; Zhang, X.; Cai, Q. Perioperative Risk Factors for Pulmonary Complications after Liver Transplantation. J. Int. Med. Res. 2010, 38, 1845–1855. [Google Scholar] [CrossRef] [PubMed]
- Glanemann, M.; Langrehr, J.; Kaisers, U.; Schenk, R.; Müller, A.; Stange, B.; Neumann, U.; Bechstein, W.-O.; Falke, K.; Neuhaus, P. Postoperative tracheal extubation after orthotopic liver transplantation. Acta Anaesthesiol. Scand. 2001, 45, 333–339. [Google Scholar] [CrossRef] [PubMed]
- Lui, J.K.; Spaho, L.; Hakimian, S.; Devine, M.; Bui, R.; Touray, S.; Holzwanger, E.; Patel, B.; Ellis, D.; Fridlyand, S.; et al. Pleural Effusions Following Liver Transplantation: A Single-Center Experience. J. Intensiv. Care Med. 2021, 36, 862–872. [Google Scholar] [CrossRef]
- Durán, F.G.; Piqueras, B.; Romero, M.; Carneros, J.A.; de Diego, A.; Salcedo, M.; Santos, L.; Ferreiroa, J.; Cos, E.; Clemente, G. Pulmonary complications following orthotopic liver transplant. Transpl. Int. 1998, 11, S255–S259. [Google Scholar] [CrossRef]
- Cohen, J.; Singer, P.; Keslin, J.; Shapira, Z.; Grunberg, G.; Grozovski, E.; Shmueli, D. Immediate postoperative course and complications of orthotopic liver transplantation: The first 31 adult patients. Transplant. Proc. 1997, 29, 2882. [Google Scholar] [CrossRef]
- Hong, S.; Hwang, S.; Lee, S.; Lee, L.; Ahn, C.; Kim, K.; Moon, D.; Ha, T. Pulmonary Complications Following Adult Liver Transplantation. Transplant. Proc. 2006, 38, 2979–2981. [Google Scholar] [CrossRef]
- Judson, M.A.; Sahn, S.A. The pleural space and organ transplantation. Am. J. Respir. Crit. Care Med. 1996, 153, 1153–1165. [Google Scholar] [CrossRef]
- Chen, A.; Ho, Y.-S.; Tu, Y.-C.; Tang, H.-S.; Cheng, T.-C. Diaphragmatic Defect as a Cause of Massive Hydrothorax in Cirrhosis of Liver. J. Clin. Gastroenterol. 1988, 10, 663–666. [Google Scholar] [CrossRef]
- Feltracco, P.; Carollo, C.; Barbieri, S.; Pettenuzzo, T.; Ori, C. Early respiratory complications after liver transplantation. World J. Gastroenterol. 2013, 19, 9271–9281. [Google Scholar] [CrossRef] [PubMed]
- Olutola, P.S.; Hutton, L.; Wall, W.J. Pleural effusion following liver transplantation. Radiology 1985, 157, 594. [Google Scholar] [CrossRef] [PubMed]
- Golfieri, R.; Giampalma, E.; Morselli/labate, A.M.; D’Arienzo, P.; Jovine, E.; Grazi, G.L.; Mazziotti, A.; Maffei, M.; Muzzi, C.; Tancioni, S.; et al. Pulmonary complications of liver transplantation: Radiological appearance and statistical evaluation of risk factors in 300 cases. Eur. Radiol. 2000, 10, 1169–1183. [Google Scholar] [CrossRef] [PubMed]
- Light, R.W.; Macgregor, M.I.; Luchsinger, P.C.; Ball, W.C. Pleural Effusions: The Diagnostic Separation of Transudates and Exudates. Ann. Intern. Med. 1972, 77, 507–513. [Google Scholar] [CrossRef] [PubMed]
- Heidecker, J.T.; Huggins, J.T.; Doelken, P.; Sahn, S.A. Is it a transudate or an exudate? Dysynchrony between pleural fluid protein and LDH in 211 initial thoracenteses. Chest 2005, 128, 156S. [Google Scholar] [CrossRef]
- Chen, C.-H.; Shih, C.-M.; Chou, J.-W.; Liu, Y.-H.; Hang, L.-W.; Hsia, T.-C.; Hsu, W.-H.; Tu, C.-Y. Outcome predictors of cirrhotic patients with spontaneous bacterial empyema. Liver Int. 2011, 31, 417–424. [Google Scholar] [CrossRef] [PubMed]
- Jiménez-Gutiérrez, J.M.; García-Juárez, I.; Olivas-Martinez, A.; Ruiz, I. One-year outcome of patients with cirrhosis who developed spontaneous bacterial empyema: A cohort study. J. Dig. Dis. 2021, 22, 714–720. [Google Scholar] [CrossRef]
- Sauer, P.; Gotthardt, D.N.; Weiss, K.H.; Rathenberg, V.; Schemmer, P.; Stremmel, W. Persistent ascites after liver transplantation: Etiology, treatment and impact on survival. Ann. Transplant. 2013, 18, 378–383. [Google Scholar] [CrossRef]
- Arroyo, V.; Ginès, P.; Gerbes, A.L.; Dudley, F.J.; Gentilini, P.; Laffi, G.; Reynolds, T.B.; Ring-Larsen, H.; Schölmerich, J. Definition and diagnostic criteria of refractory ascites and hepatorenal syndrome in cirrhosis. Hepatology 1996, 23, 164–176. [Google Scholar] [CrossRef]
- Light, R.W.; Rogers, J.T.; Moyers, J.P.; Lee, Y.C.G.; Rodriguez, R.M.; Alford, W.C.; Ball, S.K.; Burrus, G.R.; Coltharp, W.H.; Glassford, D.M.; et al. Prevalence and Clinical Course of Pleural Effusions at 30 Days after Coronary Artery and Cardiac Surgery. Am. J. Respir. Crit. Care Med. 2002, 166, 1567–1571. [Google Scholar] [CrossRef] [PubMed]
- Sadikot, R.T.; Rogers, J.T.; Cheng, N.-S.; Moyers, P.; Rodriguez, M.; Light, R.W. Pleural fluid characteristics of patients with symptomatic pleural effusion after coronary artery bypass graft surgery. Arch. Intern. Med. 2000, 160, 2665–2668. [Google Scholar] [CrossRef]
- Ahn, J.; Bhuket, T.; Mosadeghi, S.; Frenette, C.; Liu, B.; Wong, R.J. End-stage liver disease patients with MELD >40 have higher waitlist mortality compared to Status 1A patients. Hepatol. Int. 2016, 10, 838–846. [Google Scholar] [CrossRef] [PubMed]
- Charlson, M.E.; Pompei, P.; Ales, K.L.; MacKenzie, C.R. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J. Chronic Dis. 1987, 40, 373–383. [Google Scholar] [CrossRef] [PubMed]
- Perego, C.; Sbolli, M.; Specchia, C.; Fiuzat, M.; McCaw, Z.R.; Metra, M.; Oriecuia, C.; Peveri, G.; Wei, L.-J.; O’Connor, C.M.; et al. Utility of Restricted Mean Survival Time Analysis for Heart Failure Clinical Trial Evaluation and Interpretation. JACC Heart Fail. 2020, 8, 973–983. [Google Scholar] [CrossRef] [PubMed]
- Uno, H.; Claggett, B.; Tian, L.; Fu, H.; Huang, B.; Kim, D.; Wei, L. Adding a new analytical procedure with clinical interpretation in the tool box of survival analysis. Ann. Oncol. 2018, 29, 1092–1094. [Google Scholar] [CrossRef] [PubMed]
- Lui, J.K.; Spaho, L.; Holzwanger, E.; Bui, R.; Daly, J.S.; Bozorgzadeh, A.; Kopec, S.E. Intensive Care of Pulmonary Complications Following Liver Transplantation. J. Intensiv. Care Med. 2018, 33, 595–608. [Google Scholar] [CrossRef]
- Shirali, A.S.; Grotts, J.; Elashoff, D.; Barjaktarevic, I.; Melamed, K.H.; Van Hassel, J.; Cameron, R.B.; Lee, J.M.; Yanagawa, J. Predictors of Outcomes After Thoracic Surgery in Orthotopic Liver Transplant Recipients With Pleural Disease. Semin. Thorac. Cardiovasc. Surg. 2019, 31, 604–611. [Google Scholar] [CrossRef]
- Amiri, M.; Toosi, M.N.; Moazzami, B.; Jafarian, A.; Shahsavari, H.; Javaherian, M.; Dashti, H.; Fakhar, N.; Karimi, M.; Khani, F. Factors Associated With Length of Hospital Stay Following Liver Transplant Surgery. Exp. Clin. Transplant. 2020, 18, 313–319. [Google Scholar] [CrossRef]
- Mercer, R.M.; Corcoran, J.P.; Porcel, J.M.; Rahman, N.M.; Psallidas, I. Interpreting pleural fluid results. Clin. Med. J. R. Coll. Physicians Lond. 2019, 19, 213–217. [Google Scholar] [CrossRef]
- Drent, M.; Cobben, N.; Henderson, R.; Wouters, E.; van Dieijen-Visser, M. Usefulness of lactate dehydrogenase and its isoenzymes as indicators of lung damage or inflammation. Eur. Respir. J. 1996, 9, 1736–1742. [Google Scholar] [CrossRef]
- Porcel, J.M.; Light, R.W. Pleural Fluid Analysis: Are Light’s Criteria Still Relevant After Half a Century? Clin. Chest Med. 2021, 42, 599–609. [Google Scholar] [CrossRef] [PubMed]
- Ferreiro, L.; Sánchez-Sánchez, R.; Valdés, L.; Kummerfeldt, C.E.; Huggins, J.T. Concordant and Discordant Exudates and Their Effect on the Accuracy of Light’s Criteria to Diagnose Exudative Pleural Effusions. Am. J. Med. Sci. 2016, 352, 549–556. [Google Scholar] [CrossRef] [PubMed]
- Melamed, K.H.; Dai, D.; Cuk, N.; Markovic, D.; Follett, R.; Wang, T.; Lopez, R.C.; Shirali, A.S.; Yanagawa, J.; Busuttil, R.; et al. Preoperative Trapped Lung Is Associated With Increased Mortality After Orthotopic Liver Transplantation. Prog. Transplant. 2021, 31, 47–54. [Google Scholar] [CrossRef] [PubMed]
- Porcel, J.M. Pearls and myths in pleural fluid analysis. Respirology 2010, 16, 44–52. [Google Scholar] [CrossRef] [PubMed]
- Light, R.W.; Erozan, Y.S.; Ball, W.C. Cells in Pleural Fluid: Their Value in Differential Diagnosis. Arch. Intern. Med. 1973, 132, 854–860. [Google Scholar] [CrossRef]
| Total PPEf Patients (n = 124) | Alive at One Year (n = 97) | Deceased at One Year (n = 27) | p-Value | |
|---|---|---|---|---|
| Demographics | ||||
| Age (years) a | 55.0 ± 9.3 | 54.1 ± 10.0 | 58.3 ± 5.5 | 0.04 |
| Female b | 52 (41.9%) | 43 (44.3%) | 9 (33.3%) | 0.38 |
| MELD Score a | 28.2 ± 12.7 | 28.1 ± 12.8 | 28.4 ± 12.4 | 0.92 |
| Charlson Comorbidity Index a | 5.9 ± 1.8 | 5.6 ± 1.7 | 6.8 ± 1.7 | 0.002 |
| Etiology of Liver Disease | ||||
| Alcoholic Cirrhosis b | 38 (30.7%) | 28 (28.9%) | 10 (37.0%) | 0.48 |
| HBV Cirrhosis b | 13 (10.5%) | 10 (10.3%) | 3 (11.1%) | >0.99 |
| HCV Cirrhosis b | 64 (51.6%) | 49 (50.5%) | 15 (55.6%) | 0.67 |
| NASH b | 61 (49.2%) | 49 (50.5%) | 12 (44.4%) | 0.66 |
| HCC b | 46 (37.1%) | 34 (35.1%) | 12 (44.4%) | 0.38 |
| Pre-OLT Morbidity | ||||
| Prior MI b | 6 (4.8%) | 5 (5.2%) | 1 (3.7%) | >0.99 |
| COPD b | 5 (4.0%) | 2 (2.1%) | 3 (11.1%) | 0.07 |
| Asthma b | 7 (5.6%) | 5 (5.2%) | 2 (7.4%) | 0.65 |
| Portopulmonary Hypertension b | 7 (5.6%) | 5 (5.2%) | 2 (7.4%) | 0.65 |
| Hepatopulmonary Syndrome b | 29 (23.4%) | 22 (22.7%) | 7 (25.9%) | 0.80 |
| Hepatorenal Syndrome b | 71 (57.3%) | 54 (55.7%) | 17 (63.0%) | 0.52 |
| CKD b | 15 (12.1%) | 8 (8.2%) | 7 (25.9%) | 0.02 |
| Hemodialysis b,c | 56 (45.2%) | 41 (42.3%) | 15 (55.6%) | 0.28 |
| Ventilator dependence b,c | 39 (31.5%) | 30 (30.9%) | 9 (33.3%) | 0.82 |
| Vasopressor requirement b,c | 30 (24.2%) | 24 (24.7%) | 6 (22.2%) | >0.99 |
| Admitted from home b | 45 (36.3%) | 36 (37.1%) | 9 (33.3%) | 0.82 |
| Thoracentesis b | 20 (16.1%) | 17 (17.5%) | 3 (11.1%) | 0.56 |
| Surgical Pleural intervention b | 4 (3.2%) | 2 (2.1%) | 2 (7.4%) | 0.21 |
| Post-OLT Liver Function | ||||
| Alanine transaminase a,d | 361 ± 493 | 354 ± 502 | 386 ± 468 | 0.77 |
| Aspartate transaminase a,d | 497 ± 1067 | 409 ± 777.9 | 812 ± 1737 | 0.08 |
| Total bilirubin a,d | 9.8 ± 9.7 | 8.2 ± 8.0 | 15.5 ± 13.0 | <0.001 |
| Post-OLT Morbidity | ||||
| Hemodialysis b,e | 53 (42.7%) | 41 (42.3%) | 12 (44.4%) | >0.99 |
| Ventilator dependence b,e | 25 (20.2%) | 20 (20.6%) | 5 (18.5%) | >0.99 |
| Vasopressor requirement b,e | 11 (8.9%) | 8 (8.2%) | 3 (11.1%) | 0.70 |
| LOS for index OLT hospitalization (days) f | 33 (19–75.5) | 35 (20–77) | 29 (16–60) | 0.68 |
| Total LOS in first year after OLT (days) f | 75.5 (50–129) | 72 (47–117) | 81 (64.5–156) | 0.049 |
| Readmissions in first year after OLT a | 3.1 ± 2.0 | 3.0 ± 1.9 | 3.4 ± 2.5 | 0.52 |
| Total number of pleural interventions a | 2.27 ± 1.61 | 2.16 ± 1.49 | 2.66 ± 1.98 | 0.16 |
| Surgical pleural intervention b,g | 53 (42.7%) | 38 (39.2%) | 15 (55.6%) | 0.19 |
| Positive PF Culture b | 14 (11.3%) | 10 (10.3%) | 4 (14.8%) | 0.74 |
| ExudLight (n = 111) | Transudate (n = 12) | Effect Size (95% CI) | p-Value | |
|---|---|---|---|---|
| Age (years) a | 54.9 ± 9.4 | 56.4 ± 10.0 | 0.59 | |
| MELD Score a | 27.1 ± 12.7 | 34.6 ± 8.7 | 0.049 | |
| Charlson Comorbidity Index a | 5.9 ± 1.8 | 5.5 ± 1.3 | 0.46 | |
| Outcomes | ||||
| One-Year Survival b | 85 (78.0%) | 10 (83.3%) | 1.57 (0.36, 6.86) c | 0.55 |
| Hemodialysis b,d | 44 (39.6%) | 7 (58.3%) | 0.83 (0.21, 3.27) e | 0.79 |
| Ventilator dependence b,d | 22 (19.8%) | 1 (8.3%) | 3.13 (0.37, 26.14) e | 0.29 |
| Vasopressor requirement b,d | 10 (9.0%) | 0 (0.0%) | 5.16 (0.24, 110.71) e,f | 0.29 |
| LOS Post-Op (days) g | 33 (19–76) | 29.5 (17.25–41) | 0.4 (−0.09, 0.88) h | 0.11 |
| Surgical Pleural Intervention b,i | 50 (45.0%) | 3 (25.0%) | 2.73 (0.68, 10.93) e | 0.16 |
| Positive PF Culture b | 14 (12.6%) | 0 (0%) | 4.14 (0.21, 80.67) e,f | 0.35 |
| ExudProt (N = 75) | Non-ExudProt (N = 16) | Effect Size (95% CI) | p-Value | ExudLDH (N = 63) | Non-ExudLDH (N = 28) | Effect Size (95% CI) | p-Value | |
|---|---|---|---|---|---|---|---|---|
| Age (years) a | 55.5 ± 8.5 | 54.6 ± 10.4 | 0.73 | 55.0 ± 8.6 | 56.0 ± 9.4 | 0.65 | ||
| MELD Score a | 27.4 ± 12.8 | 31.9 ± 9.3 | 0.19 | 28.3 ± 11.7 | 27.8 ± 13.9 | 0.86 | ||
| Charlson Comorbidity Index a | 6.0 ± 1.7 | 5.6 ± 1.9 | 0.40 | 5.9 ± 1.7 | 5.9 ± 1.6 | 0.99 | ||
| Outcomes One-Year Survival b | 58 (79.5%) | 13 (81.3%) | 1.11 (0.32, 3.88) c | 0.87 | 51 (83.6%) | 20 (71.4%) | 0.56 (0.22, 1.42) c | 0.22 |
| Hemodialysis b,d | 32 (42.7%) | 7 (43.8%) | 1.57 (0.43, 5.66) e | 0.49 | 28 (44.4%) | 11 (39.3%) | 1.44 (0.44, 4.66) e | 0.54 |
| Ventilator Dependence b,d | 20 (26.7%) | 1 (6.3%) | 5.89 (0.72, 47.99) e | 0.10 | 19 (30.2%) | 2 (7.1%) | 5.59 (1.20, 26.04) e | 0.03 |
| Vasopressor Requirement b,d | 10 (13.3%) | 0 (0%) | 7.55 (0.38, 148.44) e,f | 0.18 | 7 (11.1%) | 3 (10.7%) | 1.18 (0.26, 5.41) e | 0.83 |
| LOS Post-Op (days) g | 36 (20–69) | 30 (19–80) | 0.17 (−0.26, 0.60) h | 0.42 | 48 (20.5–85) | 29 (15–49) | 0.38 (0.04, 0.73) h | 0.03 |
| Surgical Pleural Intervention b,i | 30 (40.0%) | 8 (50.0%) | 0.69 (0.23, 2.07) e | 0.51 | 30 (47.6%) | 8 (28.6%) | 2.26 (0.87, 5.91) e | 0.10 |
| Positive PF Culture b | 8 (10.7%) | 2 (12.5%) | 0.86 (0.16, 4.72) e | 0.87 | 9 (14.3%) | 1 (3.6%) | 4.48 (0.53, 37.72) e | 0.17 |
| Ne-Predominance (N = 26) | No Ne- Predominance (N = 86) | Effect Size (95% CI) | p-Value | Lym- Predominance (N = 33) | No Lym- Predominance (N = 79) | Effect Size (95% CI) | p-Value | |
|---|---|---|---|---|---|---|---|---|
| Age (years) a | 55.7 ± 6.6 | 54.3 ± 10.3 | 0.52 | 53.8 ± 10.5 | 54.9 ± 9.2 | 0.55 | ||
| MELD Score a | 26.5 ± 12.0 | 27.5 ± 13.0 | 0.74 | 26.2 ± 12.9 | 27.7 ± 12.7 | 0.59 | ||
| Charlson Comorbidity Index a | 6.2 ± 1.5 | 5.8 ± 1.9 | 0.40 | 5.9 ± 1.9 | 5.9 ± 1.8 | 0.96 | ||
| Outcomes One-Year Survival b | 17 (65.4%) | 70 (81.4%) | 2.16 (0.9, 5.16) c | 0.08 | 26 (78.8%) | 61 (77.2%) | 1.14 (0.46, 2.81) c | 0.77 |
| Hemodialysis b,d | 10 (38.5%) | 35 (40.7%) | 1.03 (0.33, 3.18) e | 0.96 | 11 (33.3%) | 34 (43.0%) | 0.72 (0.24, 2.19) e | 0.57 |
| Ventilator Dependence b,d | 9 (34.6%) | 13 (15.1%) | 3.10 (1.12, 8.55) e | 0.03 | 2 (6.1%) | 20 (25.3%) | 0.19 (0.04, 0.88) e | 0.03 |
| Vasopressor Requirement b,d | 4 (15.4%) | 4 (4.7%) | 10.96 (1.46, 82.15) e | 0.02 | 0 (0%) | 8 (10%) | 0.10 (0.01, 1.81) e,f | 0.12 |
| LOS Post-Op (days) g | 35.5 (17–56.5) | 30.5 (19–74) | −0.04 (−0.4, 0.32) h | 0.82 | 25 (19–48) | 36 (18.5–78.5) | −0.28 (−0.6, 0.05) h | 0.09 |
| Surgical Pleural Intervention b,i | 15 (57.7%) | 28 (32.6%) | 2.88 (1.17, 7.10) e | 0.02 | 11 (33.3%) | 32 (40.5%) | 0.72 (0.31, 1.70) e | 0.45 |
| Positive PF Culture b | 5 (19.2%) | 8 (9.3%) | 2.56 (0.74, 8.91) e | 0.14 | 0 (0%) | 13 (16.5%) | 0.07 (0.01, 1.17) e | 0.06 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Patel, B.H.; Melamed, K.H.; Wilhalme, H.; Day, G.L.; Wang, T.; DiNorcia, J.; Farmer, D.; Agopian, V.; Kaldas, F.; Barjaktarevic, I. Implications of Pleural Fluid Composition in Persistent Pleural Effusion following Orthotopic Liver Transplant. Med. Sci. 2023, 11, 24. https://doi.org/10.3390/medsci11010024
Patel BH, Melamed KH, Wilhalme H, Day GL, Wang T, DiNorcia J, Farmer D, Agopian V, Kaldas F, Barjaktarevic I. Implications of Pleural Fluid Composition in Persistent Pleural Effusion following Orthotopic Liver Transplant. Medical Sciences. 2023; 11(1):24. https://doi.org/10.3390/medsci11010024
Chicago/Turabian StylePatel, Bhavesh H., Kathryn H. Melamed, Holly Wilhalme, Gwenyth L. Day, Tisha Wang, Joseph DiNorcia, Douglas Farmer, Vatche Agopian, Fady Kaldas, and Igor Barjaktarevic. 2023. "Implications of Pleural Fluid Composition in Persistent Pleural Effusion following Orthotopic Liver Transplant" Medical Sciences 11, no. 1: 24. https://doi.org/10.3390/medsci11010024
APA StylePatel, B. H., Melamed, K. H., Wilhalme, H., Day, G. L., Wang, T., DiNorcia, J., Farmer, D., Agopian, V., Kaldas, F., & Barjaktarevic, I. (2023). Implications of Pleural Fluid Composition in Persistent Pleural Effusion following Orthotopic Liver Transplant. Medical Sciences, 11(1), 24. https://doi.org/10.3390/medsci11010024






