Training-Induced Muscle Fatigue with a Powered Lower-Limb Exoskeleton: A Preliminary Study on Healthy Subjects
Abstract
1. Introduction
2. Materials and Methods
2.1. Subjects
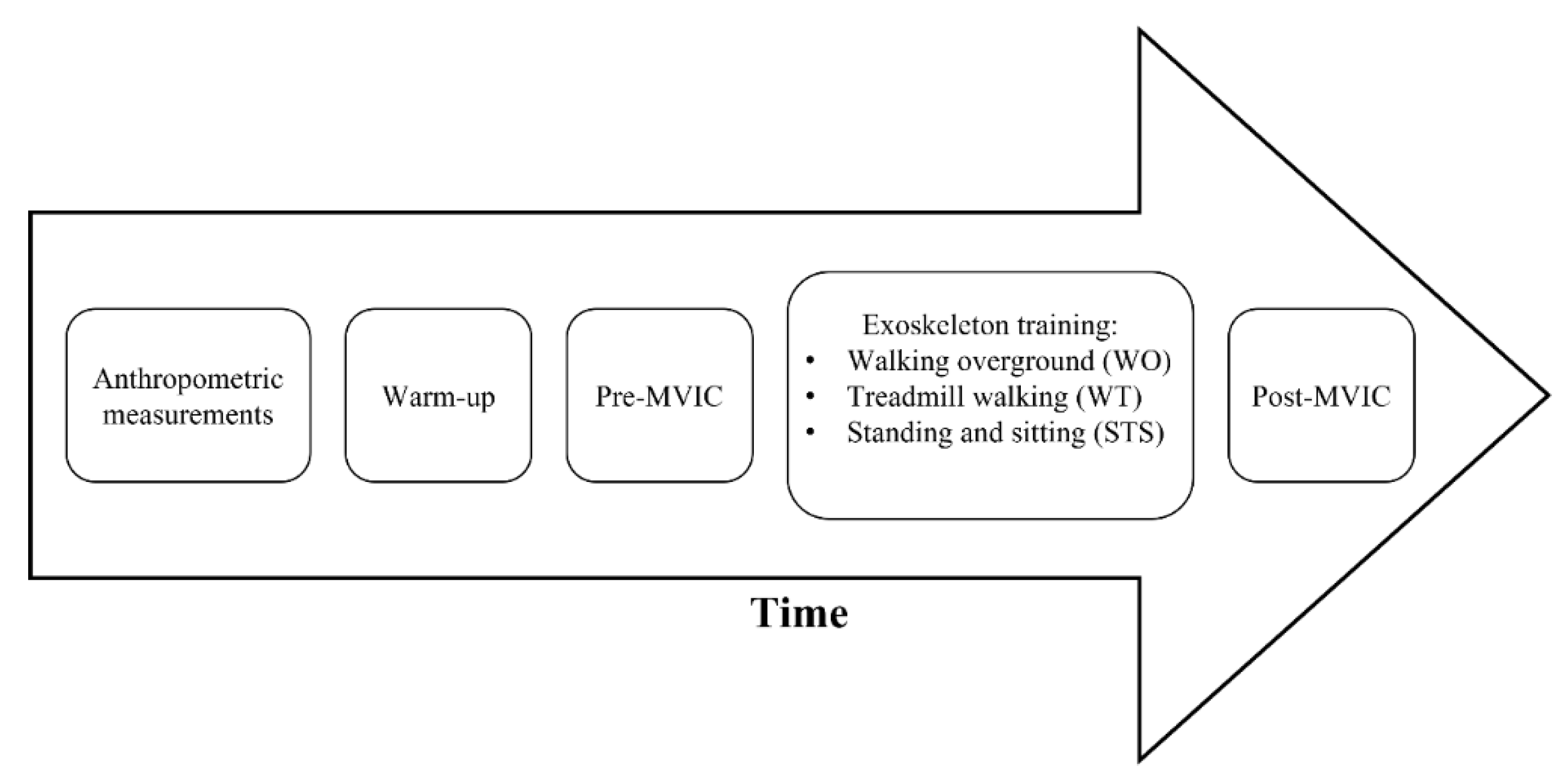
2.2. Study Design
ExoAtlet II
2.3. Statistical Analysis
3. Results
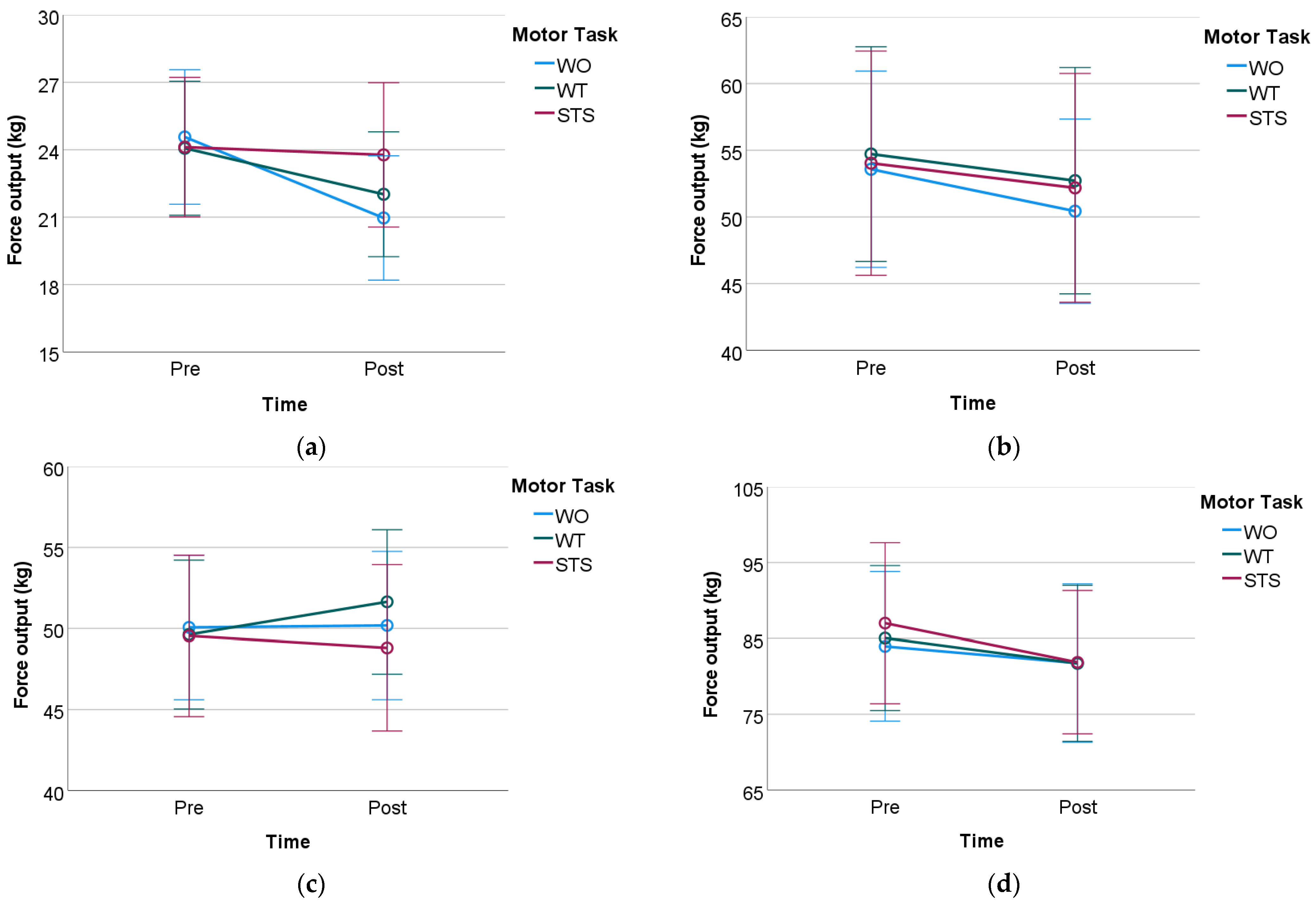
3.1. Knee Flexion MVIC Test
3.2. Knee Extension MVIC Test
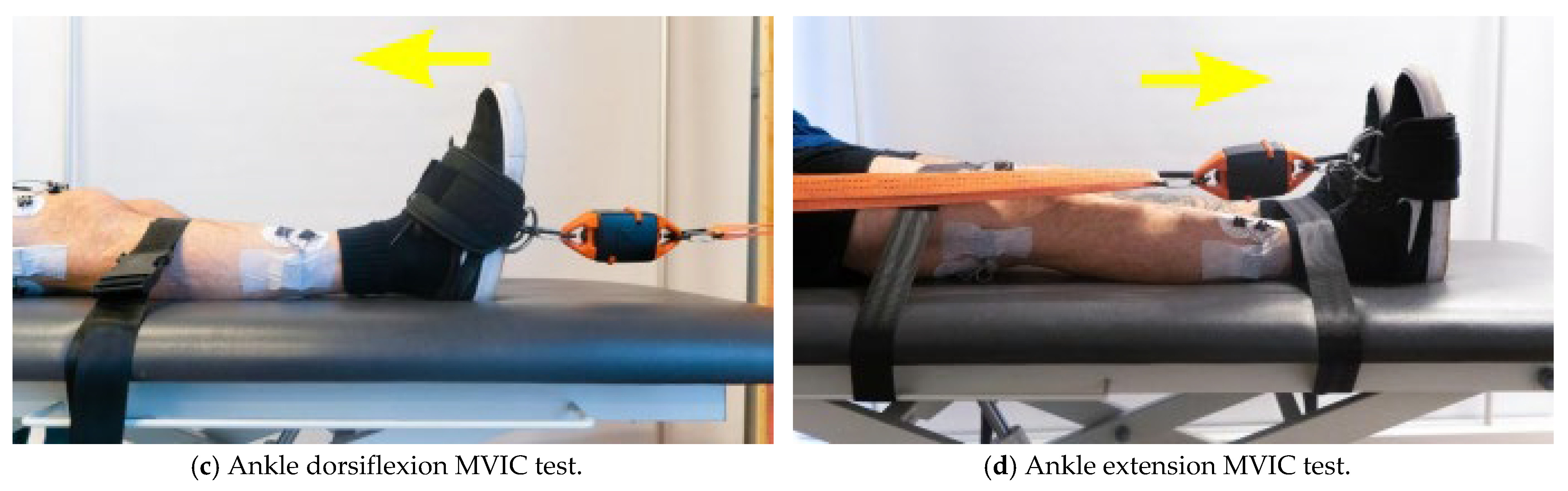
3.3. Ankle Dorsiflexion MVIC Test
3.4. Ankle Extension MVIC Test
4. Discussion
Statistical Considerations for Further Studies
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Qiu, J.; Liu, H. Gait Recognition for Human-Exoskeleton System in Locomotion Based on Ensemble Empirical Mode Decomposition. Math. Probl. Eng. 2021, 2021, 285. [Google Scholar] [CrossRef]
- Chen, G.; Chan, C.K.; Guo, Z.; Yu, H. A Review of Lower Extremity Assistive Robotic Exoskeletons in Rehabilitation Therapy. Crit. Rev. Biomed. Eng. 2013, 41, 343–363. [Google Scholar] [CrossRef]
- Vaughan-Graham, J.; Brooks, D.; Rose, L.; Nejat, G.; Pons, J.; Patterson, K. Exoskeleton use in post-stroke gait rehabilitation: A qualitative study of the perspectives of persons post-stroke and physiotherapists. J. Neuroeng. Rehabil. 2020, 17, 1–15. [Google Scholar] [CrossRef]
- Miller, L.E.; Zimmermann, A.K.; Herbert, W.G. Clinical effectiveness and safety of powered exoskeleton-assisted walking in patients with spinal cord injury: Systematic review with meta-analysis. Med. Dev. Auckland NZ 2016, 2016, 455–466. [Google Scholar] [CrossRef]
- Ditunno, P.L.; Patrick, M.; Stineman, M.; Ditunno, J.F. Who wants to walk? Preferences for recovery after SCI: A longitudinal and cross-sectional study. Spinal Cord 2008, 46, 500–506. [Google Scholar] [CrossRef]
- Lajeunesse, V.; Vincent, C.; Routhier, F.; Careau, E.; Michaud, F. Exoskeletons’ design and usefulness evidence according to a systematic review of lower limb exoskeletons used for functional mobility by people with spinal cord injury. Disabil. Rehabil. Assist. Technol. 2016, 11, 535–547. [Google Scholar] [CrossRef]
- Lau, J.C.L.; Mombaur, K. Preliminary Study on a Novel Protocol for Improving Familiarity with a Lower-Limb Robotic Exoskeleton in Able-Bodied, First-Time Users. Front. Robot. AI 2022, 8, 785251. [Google Scholar] [CrossRef]
- Ahuja, C.S.; Wilson, J.R.; Nori, S.; Kotter, M.; Druschel, C.; Curt, A.; Fehlings, M.G. Traumatic spinal cord injury. Nat. Rev. Dis. Prim. 2017, 3, 1–21. [Google Scholar] [CrossRef]
- Physiopedia. World Report on Disability. Physiopedia. 2022. Available online: https://www.physio-pedia.com/Wheelchair_Users (accessed on 25 August 2022).
- Moore, C.D.; Craven, B.C.; Thabane, L.; Laing, A.C.; Frank-Wilson, A.W.; Kontulainen, S.A.; Papaioannou, A.; Adachi, J.D.; Giangregorio, L.M. Lower-extremity muscle atrophy and fat infiltration after chronic spinal cord injury. J. Musculoskelet. Neuronal Interact. 2015, 15, 32. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5092153/ (accessed on 2 May 2022).
- La Fountaine, M.F.; Cirnigliaro, C.M.; Emmons, R.R.; Kirshblum, S.C.; Galea, M.; Spungen, A.M.; Bauman, W.A. Lipoprotein heterogeneity in persons with Spinal Cord Injury: A model of prolonged sitting and restricted physical activity. Lipids Health Dis. 2015, 14, 1–10. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Contreras-Vidal, J.L.; Bhagat, N.A.; Brantley, J.; Cruz-Garza, J.G.; He, Y.; Manley, Q.; Nakagome, S.; Nathan, K.; Tan, S.H.; Zhu, F.; et al. Powered exoskeletons for bipedal locomotion after spinal cord injury. J. Neural Eng. 2016, 13, 031001. [Google Scholar] [CrossRef]
- Adams, M.M.; Hicks, A.L. Spasticity after spinal cord injury. Spinal Cord 2005, 43, 577–586. [Google Scholar] [CrossRef] [PubMed]
- Twomey, R.; Aboodarda, S.J.; Kruger, R.; Culos-Reed, S.N.; Temesi, J.; Millet, G.Y. Neuromuscular fatigue during exercise: Methodological considerations, etiology and potential role in chronic fatigue. Neurophysiol. Clin. 2017, 47, 95–110. [Google Scholar] [CrossRef] [PubMed]
- Enoka, R.M.; Duchateau, J. Translating Fatigue to Human Performance. Med. Sci. Sports Exerc. 2016, 48, 2228–2238. [Google Scholar] [CrossRef]
- Enoka, R.M.; Stuart, D.G. Neurobiology of muscle fatigue. J. Appl. Physiol. 1992, 72, 1631–1648. [Google Scholar] [CrossRef] [PubMed]
- Barsotti, A.; Khalaf, K.; Gan, D. Muscle fatigue evaluation with EMG and Acceleration data: A case study. Proc. Annu. Int. Conf. IEEE Eng. Med. Biol. Soc. EMBS 2020, 2020, 3138–3141. [Google Scholar] [CrossRef]
- Magal, M.; Riebe, D. New preparticipation health screening recommendations: What exercise professionals need to know. ACSM’s Heal. Fit. J. 2016, 20, 22–27. [Google Scholar] [CrossRef]
- Craig, C.L.; Marshall, A.L.; Sjöström, M.; Bauman, A.E.; Booth, M.L.; Ainsworth, B.E.; Pratt, M.; Ekelund, U.L.F.; Yngve, A.; Sallis, J.F.; et al. International physical activity questionnaire: 12-Country reliability and validity. Med. Sci. Sports Exerc. 2003, 35, 1381–1395. [Google Scholar] [CrossRef]
- Gallagher, D.; Heymsfield, S.B. Muscle distribution: Variations with body weight, gender, and age. Appl. Radiat. Isot. 1998, 49, 733–734. [Google Scholar] [CrossRef]
- Abdelmohsen, A.M. Leg Dominance Effect on Isokinetic Muscle Strength of Hip Joint. J. Chiropr. Med. 2019, 18, 27. [Google Scholar] [CrossRef]
- Van Geel, F.; Hvid, L.G.; van Noten, P.; Eijnde, B.O.; Dalgas, U.; Feys, P. Is maximal muscle strength and fatigability of three lower limb muscle groups associated with walking capacity and fatigability in multiple sclerosis? An exploratory study. Mult. Scler. Relat. Disord. 2021, 50, 02841. [Google Scholar] [CrossRef] [PubMed]
- ExoAtlet, ExoAtlet Global SA, Luxembourg. 2022. Available online: https://exoatlet.lu/ (accessed on 23 August 2022).
- Pais-Vieira, C.; Allahdad, M.; Neves-Amado, J.; Perrotta, A.; Morya, E.; Moioli, R.; Shapkova, E.; Pais-Vieira, M. Method for positioning and rehabilitation training with the ExoAtlet® powered exoskeleton. MethodsX 2020, 7, 100849. [Google Scholar] [CrossRef] [PubMed]
- Drużbicki, M.; Guzik, A.; Przysada, G.; Brzozowska-Magoń, A.; Cygoń, K.; Boczula, G.; Bartosik-Psujek, H. Effects of Robotic Exoskeleton-Aided Gait Training in the Strength, Body Balance, and Walking Speed in Individuals With Multiple Sclerosis: A Single-Group Preliminary Study. Arch. Phys. Med. Rehabil. 2021, 102, 175–184. [Google Scholar] [CrossRef] [PubMed]
- Polkowski, G.G.; Clohisy, J.C. Hip biomechanics. Sports Med. Arthrosc. 2010, 18, 56–62. [Google Scholar] [CrossRef]
- Thomas, A.C.; McLean, S.G.; Palmieri-Smith, R.M. Quadriceps and hamstrings fatigue alters hip and knee mechanics. J. Appl. Biomech. 2010, 26, 159–170. [Google Scholar] [CrossRef]
- Chow, J.W.; Stokic, D.S. Relations between knee and ankle muscle coactivation and temporospatial gait measures in patients without hypertonia early after stroke. Exp. Brain Res. 2020, 238, 2909–2919. [Google Scholar] [CrossRef]
- Garland, S.J.; Willems, D.A.; Ivanova, T.D.; Miller, K.J. Recovery of standing balance and functional mobility after stroke. Arch. Phys. Med. Rehabil. 2003, 84, 1753–1759. [Google Scholar] [CrossRef]
- Swank, C.; Almutairi, S.; Wang-Price, S.; Gao, F. Immediate kinematic and muscle activity changes after a single robotic exoskeleton walking session post-stroke. Top. Stroke Rehabil. 2020, 27, 503–515. [Google Scholar] [CrossRef]


| Inclusion Criteria | Exclusion Criteria |
|---|---|
| |
|
|
|
|
|
|
|
|
| Male | Female | Overall | p-Value (Mann-Whitney U Test) | |
|---|---|---|---|---|
| Number | 15 | 15 | 30 | |
| Age (mean ± SD) | 24 ± 3.2 | 22.3 ± 1.7 | 23.2 ± 2.7 | 0.164 |
| Height (mean ± SD, cm) | 180.7 ± 5 | 164.6 ± 5.5 | 172.7 ± 9.7 | <0.001 |
| Weight (mean ± SD, kg) | 78.7 ± 9.8 | 58.3 ± 8.4 | 68.5 ± 13.7 | <0.001 |
| IPAQ (median (IQR), MET-minutes/week) | 6960 (5152) | 3342 (6604) | 5055 (6880) | 0.237 |
| IPAQ Category | ||||
|---|---|---|---|---|
| Gender | Inactive | Minimally Active | HEPA Active | Total |
| Male | 0 | 3 | 12 | 15 |
| Female | 0 | 6 | 9 | 15 |
| Total | 0 | 9 | 21 | 30 |
| Task | Setup Parameters | Value |
|---|---|---|
| Walking overground | Pause between steps (s) | 0 |
| & | Step length (cm) | 40 |
| Treadmill walking | Step height (cm) | 15 |
| Step duration (s) | 1.2 | |
| Stand-up sit-down | Standing up duration (s) | 3 |
| Sitting down duration (s) | 2 |
| Motor Task | Time | Knee Flexion ± SD (kg) | Knee Extension ± SD (kg) | Ankle Dorsi Flexion ± SD (kg) | Ankle Extension ± SD (kg) |
|---|---|---|---|---|---|
| WO | Pre | 24.57 ± 8.01 | 53.58 ± 19.71 | 50.06 ± 11.94 | 83.96 ± 26.4 |
| Post | 20.97 ± 7.41 | 50.43 ± 18.51 | 50.18 ± 12.25 | 81.76 ± 27.95 | |
| WT | Pre | 24.07 ± 7.98 | 54.72 ± 21.56 | 49.63 ± 12.29 | 85.05 ± 25.6 |
| Post | 22.02 ± 7.44 | 52.72 ± 22.73 | 51.64 ± 11.93 | 81.71 ± 27.56 | |
| STS | Pre | 24.12 ± 8.31 | 54.03 ± 22.52 | 49.55 ± 13.33 | 87.01 ± 28.43 |
| Post | 23.77 ± 8.6 | 52.18 ± 22.99 | 48.81 ± 13.74 | 81.87 ± 25.3 |
| Repeated Measures Two-Way ANOVA—Within-Subjects Effects | |||||
|---|---|---|---|---|---|
| Cases | df | Mean Square | |||
| Motor task | 2 | 22.8 | 1.78 | 0.178 | 0.058 |
| Time | 1 | 179.74 | 17.68 | <0.001 † | 0.379 |
| Motor task x Time | 2 | 39.83 | 5.937 | 0.005 † | 0.17 |
| Pairwise Comparisons Motor Task × Time | |||||||
|---|---|---|---|---|---|---|---|
| Motor Task | Time (I) | Time (J) | Mean Diff. (I-J) | Std. Error | 95% Confidence Interval for Difference a | ||
| Lower Bound | Upper Bound | ||||||
| WO | Pre | Post | 3.603 | 0.749 | <0.001 † | 2.072 | 5.135 |
| WT | Pre | Post | 2.047 | 0.723 | 0.008 † | 0.568 | 3.526 |
| STS | Pre | Post | 0.345 | 0.699 | 0.625 | −1.084 | 1.775 |
| Repeated Measures Two-Way ANOVA—Within-Subjects Effects | |||||
|---|---|---|---|---|---|
| Cases | df | Mean Square | |||
| Motor task | 2 | 45.25 | 0.482 | 0.62 | 0.016 |
| Time | 1 | 244.43 | 10.461 | 0.003 † | 0.265 |
| Motor task x Time | 2 | 7.528 | 0.38 | 0.686 | 0.013 |
| Repeated Measures Two-Way ANOVA—Within-Subjects Effects | |||||
|---|---|---|---|---|---|
| Cases | df | Mean Square | |||
| Motor task | 2 | 32.83 | 0.629 | 0.537 | 0.021 |
| Time | 1 | 9.73 | 0.349 | 0.559 | 0.012 |
| Motor task x Time | 2 | 29.72 | 1.825 | 0.17 | 0.059 |
| Repeated Measures Two-Way ANOVA—Within-Subjects Effects | |||||
|---|---|---|---|---|---|
| Cases | df | Mean Square | |||
| Motor task | 2 | 38.75 | 0.339 | 0.714 | 0.012 |
| Time | 1 | 569.23 | 8.817 | 0.006 † | 0.233 |
| Motor task x Time | 2 | 32.99 | 0.853 | 0.431 | 0.029 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Baptista, R.; Salvaggio, F.; Cavallo, C.; Pizzocaro, S.; Galasso, S.; Schmid, M.; De Nunzio, A.M. Training-Induced Muscle Fatigue with a Powered Lower-Limb Exoskeleton: A Preliminary Study on Healthy Subjects. Med. Sci. 2022, 10, 55. https://doi.org/10.3390/medsci10040055
Baptista R, Salvaggio F, Cavallo C, Pizzocaro S, Galasso S, Schmid M, De Nunzio AM. Training-Induced Muscle Fatigue with a Powered Lower-Limb Exoskeleton: A Preliminary Study on Healthy Subjects. Medical Sciences. 2022; 10(4):55. https://doi.org/10.3390/medsci10040055
Chicago/Turabian StyleBaptista, Renato, Francesco Salvaggio, Caterina Cavallo, Serena Pizzocaro, Svonko Galasso, Micaela Schmid, and Alessandro Marco De Nunzio. 2022. "Training-Induced Muscle Fatigue with a Powered Lower-Limb Exoskeleton: A Preliminary Study on Healthy Subjects" Medical Sciences 10, no. 4: 55. https://doi.org/10.3390/medsci10040055
APA StyleBaptista, R., Salvaggio, F., Cavallo, C., Pizzocaro, S., Galasso, S., Schmid, M., & De Nunzio, A. M. (2022). Training-Induced Muscle Fatigue with a Powered Lower-Limb Exoskeleton: A Preliminary Study on Healthy Subjects. Medical Sciences, 10(4), 55. https://doi.org/10.3390/medsci10040055







