Unnatural Cycles: Anthropogenic Disruption to Health and Planetary Functions
Abstract
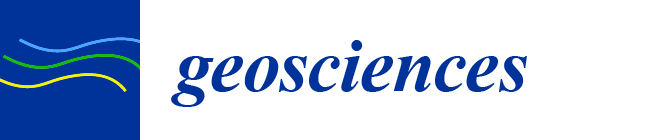
:1. Introduction
2. The Impact of Asthma and COPD
| Year | Country | Currency | Total Cost | Prescription Medicines | GP Visits | In-Patient | OPD | A&E | Non-Medical | Indirect | Number of Cases | Ref. |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2008–2013 | USA | USD | 3100/patient/year; 81.9 billion total (2013) | 1830 per patient pa (4) | 529 mean/patient stay (4) | 176/patient/visit (4) | 105/patient/visit | 3 billion total | 29 billion total | 40 million pa (13% population) | [14,15] | |
| 2010 | Iran | USD | 3100 total; 368/patient pa | 253/patient pa | 6.49/patient/visit | [16] | ||||||
| 2011 | South Korea | USD | Total, 831 Million: 336/person average | 144.9 million pa | 61 million dollars pa | 310 million pa | 831.1 million pa | 103.1 million pa | [17] | |||
| 2017 | Europe | Euro | 1900/patient pa; total 4.3 billion pa | 315 mean/per patient pa; total 17.2 billion pa | 97 mean/patient | 1783/patient | 12.2 million pa | [14] | ||||
| 2017 | Greece | Euro | 2281.8/patient pa | [18] | ||||||||
| 2017 | Abu Dhabi | USD | 150/patient | [19] | ||||||||
| 2021 | United Kingdom | British pounds (GBP) | 3 billion asthma; 1.9 billion COPD, pa | 64 million visits pa [uncosted] | 270/day/patient | [13] |
“The annual economic cost of premature deaths from air pollution across the countries of the WHO European region stood at US $1.431 trillion, and the overall annual economic cost of health impacts and mortality from air pollution, including estimates for morbidity costs, stood at US $1.575 trillion”.[20] (p. 26)
3. The Environmental Burden of Inhalers
4. What Happens Next?
5. New Products
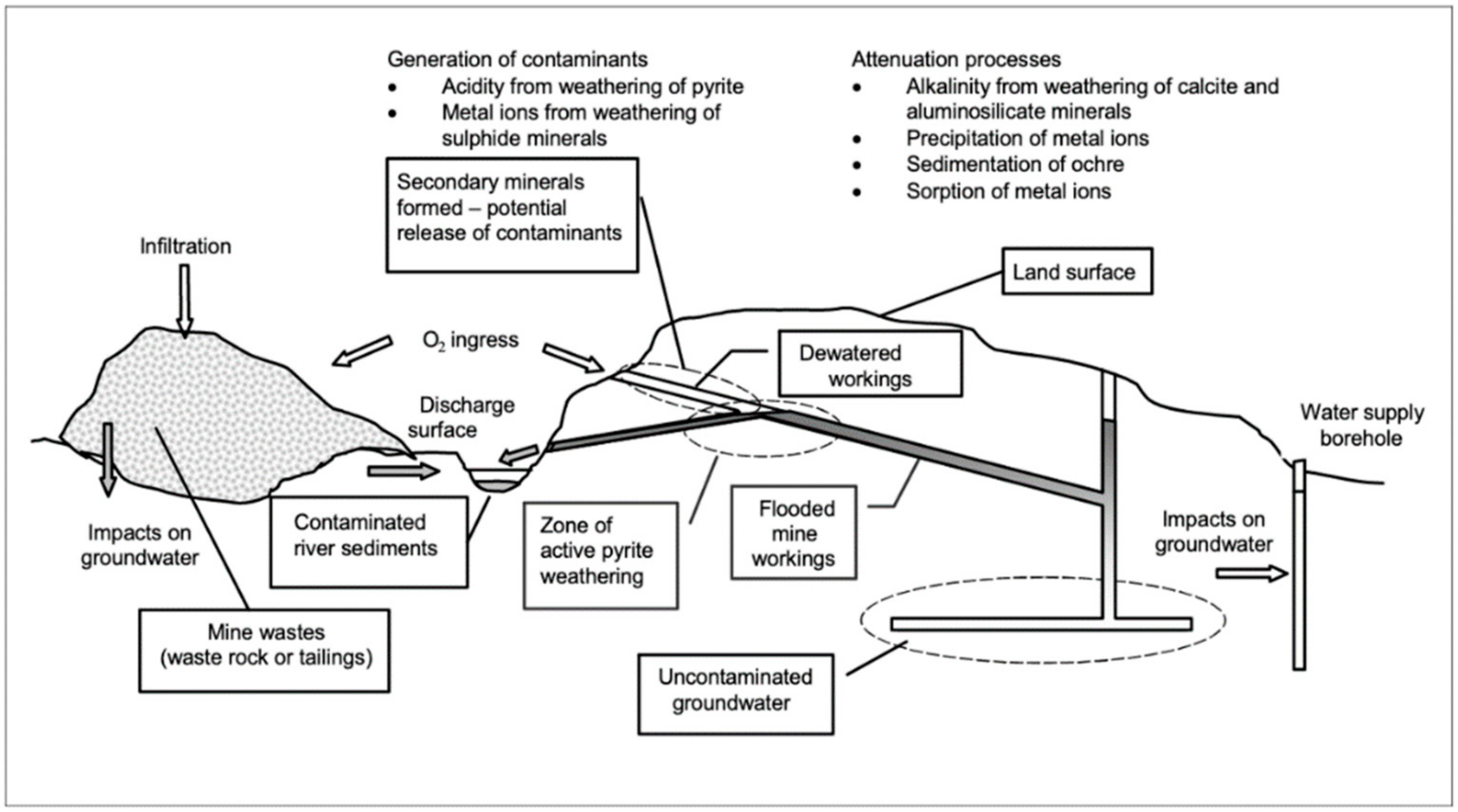
6. Mining Problems Migrate
7. Unintended Consequences
8. Daily Actions
9. Who Pays? and Who Benefits?
- what is the problem? Increasing cases of asthma and COPD
- what caused the problem? Poor air quality
- what did we do about it? Prescribed inhalers to treat the symptoms
- what did this achieve? Possible improvement of patient condition; definite consumption of raw materials; definite creation of a difficult-to-manage waste stream
- has the problem been resolved? No, it has been exacerbated
- why did this not work? Because political will and money need to be invested in the right place
10. Bigger Problems
11. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Rodell, M.; Beaudoing, H.K.; L’Ecuyer, T.S.; Olson, W.S.; Famiglietti, J.S.; Houser, P.R. The observed state of the water cycle in the early twenty-first century. J. Clim. 2015, 28, 8289–8318. [Google Scholar] [CrossRef]
- Gruber, N.; Galloway, J.N. An Earth-system perspective of the global nitrogen cycle. Nature 2008, 451, 293–296. [Google Scholar] [CrossRef] [PubMed]
- Friedlingstein, P.; O’Sullivan, M.; Jones, M.W.; Andrew, R.M.; Hauck, J.; Olsen, A.; Peters, G.P.; Peters, W.; Pongratz, J.; Sitch, S.; et al. Global Carbon Budget 2020. Earth Syst. Sci. Data 2020, 12, 3269–3340. [Google Scholar] [CrossRef]
- Vos, T.; Lim, S.S.; Abbafati, C.; Abbas, K.M.; Abbasi, M.; Abbasifard, M.; Abbasi-Kangevari, M.; Abbastabar, H.; Abd-Allah, F.; Abdelalim, A.; et al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020, 396, 1204–1222. [Google Scholar] [CrossRef]
- To, T.; Stanojevic, S.; Moores, G.; Gershon, A.S.; Bateman, E.D.; Cruz, A.A.; Boulet, L.-P. Global asthma prevalence in adults: Findings from the cross-sectional World Health Survey. BMC Public Health 2012, 12, 204. [Google Scholar] [CrossRef] [Green Version]
- Fisher, S.; Bellinger, D.C.; Cropper, M.L.; Kumar, P.; Binagwaho, A.; Koudenoukpo, J.B.; Park, Y.; Taghian, G.; Landrigan, P.J. Air pollution and development in Africa: Impacts on health, the economy, and human capital. Lancet Planet. Health 2021, 5, e681–e688. [Google Scholar] [CrossRef]
- GBD 2015 Chronic Respiratory Disease Collaborators. Global, regional, and national deaths, prevalence, disability-adjusted life years, and years lived with disability for chronic obstructive pulmonary disease and asthma, 1990–2015: A systematic analysis for the Global Burden of Disease Study 2015. Lancet Respir. Med. 2017, 5, 691–706. [Google Scholar] [CrossRef] [Green Version]
- Hunt, A.; Abraham, J.L.; Judson, B.; Berry, C.L. Toxicologic and Epidemiologic clues from the characterization of the 1952 London smog fine particulate matter in archival autopsy lung tissues. Environ. Health Perspect. 2003, 111, 1209–1214. [Google Scholar] [CrossRef] [Green Version]
- Bell, M.L.; Davis, D.L.; Fletcher, T. A Retrospective Assessment of Mortality from the London Smog Episode of 1952: The Role of Influenza and Pollution. Environ. Health Perspect. 2004, 112, 6–8. [Google Scholar] [CrossRef] [Green Version]
- Bharadwaj, P.; Zivin, J.G.; Mullins, J.T.; Neidell, M. Early-Life exposure to the Great Smog of 1952 and the development of asthma. Am. J. Respir. Crit. Care Med. 2016, 194, 1475–1482. [Google Scholar] [CrossRef] [Green Version]
- Mukherjee, M.; Stoddart, A.; Gupta, R.P.; Nwaru, B.I.; Farr, A.; Heaven, M.; Fitzsimmons, D.; Bandyopadhyay, A.; Aftab, C.; Simpson, C.R.; et al. The epidemiology, healthcare and societal burden and costs of asthma in the UK and its member nations: Analyses of standalone and linked national databases. BMC Med. 2016, 14, 113. [Google Scholar] [CrossRef] [Green Version]
- Cumella, A.; Haque, A. On the edge. In How Inequality Affects People with Asthma; Asthma: London, UK, 2018. [Google Scholar]
- NHS England. Respiratory Disease. Available online: https://www.england.nhs.uk/ourwork/clinical-policy/respiratory-disease/ (accessed on 14 October 2021).
- Nunes, C.; Pereira, A.M.; Morais-Almeida, M. Asthma costs and social impact. Asthma Res. Pract. 2017, 3, 1. [Google Scholar] [CrossRef] [Green Version]
- Nurmagambetov, T.; Kuwahara, R.; Garbe, P. The economic burden of asthma in the United States, 2008–2013. Ann. Am. Thorac. Soc. 2018, 15, 348–356. [Google Scholar] [CrossRef]
- Sharifi, L.; Dashti, R.; Pourpak, Z.; Fazlolahhi, M.R.; Movahedi, M.; Chavoshzadeh, Z.; Soheili, H.; Bokair, S.; Kazemnejad, A.; Moin, M. Economic burden of pediatric asthma: Annual cost of disease in Iran. Iran. J. Public Health 2018, 47, 256–263. [Google Scholar]
- Lee, Y.-H.; Yoon, S.-J.; Kim, E.-J.; Kim, Y.-A.; Seo, H.-Y.; Oh, I.-H. Economic burden of asthma in Korea. Allergy Asthma Proc. 2011, 32, e35–e40. [Google Scholar] [CrossRef]
- Souliotis, K.; Kousoulakou, H.; Hillas, G.; Bakakos, P.; Toumbis, M.; Loukides, S.; Vassilakopoulos, T. Direct and indirect costs of asthma management in Greece: An expert panel approach. Front. Public Health 2017, 5, 67. [Google Scholar] [CrossRef] [Green Version]
- Alzaabi, A.; Alseiari, M.; Mahboub, B. Economic burden of asthma in Abu Dhabi: A retrospective study. Clin. Outcomes Res. CEOR 2014, 6, 445–450. [Google Scholar] [CrossRef] [Green Version]
- World Health Organization. Economic Cost of the Health Impact of Air Pollution in Europe: Clean Air, Health and Wealth; World Health Organization: Geneva, Switzerland, 2015. [Google Scholar]
- Simons, E.; Dell, S.D.; Moineddin, R.; To, T. Neighborhood material deprivation is associated with childhood asthma development: Analysis of prospective administrative data. Can. Respir. J. 2019, 2019, e6808206. [Google Scholar] [CrossRef]
- Alsallakh, M.A.; Rodgers, S.E.; Lyons, R.A.; Sheikh, A.; Davies, G.A. Association of socioeconomic deprivation with asthma care, outcomes, and deaths in Wales: A 5-year national linked primary and secondary care cohort study. PLoS Med. 2021, 18, e1003497. [Google Scholar] [CrossRef]
- Collins, P.F.; Stratton, R.J.; Kurukulaaratchy, R.J.; Elia, M. Influence of deprivation on health care use, health care costs, and mortality in COPD. Int. J. Chron. Obstruct. Pulm. Dis. 2018, 13, 1289–1296. [Google Scholar] [CrossRef] [Green Version]
- Bambra, C.; Riordan, R.; Ford, J.; Matthews, F. The COVID-19 pandemic and health inequalities. J. Epidemiol. Community Health 2020, 74, 964–968. [Google Scholar] [CrossRef] [PubMed]
- Environmental Audit Committee. UK Progress on Reducing F-Gas Emissions, Fifth Report of Session 2017-19; House of Commons: London, UK, 2018.
- Hillman, T.; Mortimer, F.; Hopkinson, N.S. Inhaled drugs and global warming: Time to shift to dry powder inhalers. BMJ 2013, 346, f3359. [Google Scholar] [CrossRef] [PubMed]
- Sellers, W.F.S. Asthma pressurised metered dose inhaler performance: Propellant effect studies in delivery systems. Allergy Asthma Clin. Immunol. 2017, 13, 30. [Google Scholar] [CrossRef] [PubMed]
- Jeswani, H.K.; Azapagic, A. Life cycle environmental impacts of inhalers. J. Clean. Prod. 2019, 237, 117733. [Google Scholar] [CrossRef]
- Janson, C.; Henderson, R.; Löfdahl, M.; Hedberg, M.; Sharma, R.; Wilkinson, A.J.K. Carbon footprint impact of the choice of inhalers for asthma and COPD. Thorax 2020, 75, 82–84. [Google Scholar] [CrossRef] [Green Version]
- Lavorini, F.; Corrigan, C.J.; Barnes, P.J.; Dekhuijzen, P.R.N.; Levy, M.L.; Pedersen, S.; Roche, N.; Vincken, W.; Crompton, G.K. Retail sales of inhalation devices in European countries: So much for a global policy. Respir. Med. 2011, 105, 1099–1103. [Google Scholar] [CrossRef] [Green Version]
- Atherton, M. Environmental Impact of Inhalers; Low Carbon Hub: Oxford, UK, 2017. [Google Scholar]
- Trueman, P.; Taylor, D.G.; Lowson, K.; Bligh, A.; Meszaros, A.; Wright, D.; Glanville, J.; Newbould, J.; Bury, M.; Barber, N.; et al. Evaluation of the Scale, Causes and Costs of Waste Medicines; Final Report; University of London School of Pharmacy: London, UK, 2010; ISBN 978-0-902936-20-1. [Google Scholar]
- UK Government. Circular Economy Package Policy Statement. Available online: https://www.gov.uk/government/publications/circular-economy-package-policy-statement/circular-economy-package-policy-statement (accessed on 1 September 2021).
- European Commission. Circular Economy Action Plan. Available online: https://ec.europa.eu/environment/strategy/circular-economy-action-plan_en (accessed on 1 September 2021).
- Circular Change. The State of the Circular Economy in America—The First Report. Available online: https://www.circularchange.com/news/the-state-of-the-circular-economy-in-america-the-first-report (accessed on 1 September 2021).
- Alshabani, K.; Attaway, A.A.; Smith, M.J.; Majumdar, U.; Rice, R.; Han, X.; Wang, X.; Hatipoğlu, U. Electronic inhaler monitoring and healthcare utilization in chronic obstructive pulmonary disease. J. Telemed. Telecare 2020, 26, 495–503. [Google Scholar] [CrossRef]
- Attaway, A.H.; Alshabani, K.; Bender, B.; Hatipoğlu, U.S. The utility of electronic inhaler monitoring in COPD management: Promises and challenges. Chest 2020, 157, 1466–1477. [Google Scholar] [CrossRef]
- European Commission. Waste from Electrical and Electronic Equipment (WEEE). Available online: https://ec.europa.eu/environment/topics/waste-and-recycling/waste-electrical-and-electronic-equipment-weee_en (accessed on 1 September 2021).
- US Energy Information Administration (EIA). The Basic Metals Industry is One of the World’s Largest Industrial Energy Users. Available online: https://www.eia.gov/todayinenergy/detail.php?id=38392 (accessed on 6 November 2021).
- Paulikas, D.; Katona, S.; Ilves, E.; Stone, G.; O’Sullivan, A. Where Should Metals for the Green Transition Come from? Comparing Environmental, Social, and Economic Impacts of Supplying Base Metals from Land Ores and Seafloor Polymetallic Nodules; LCA White Paper, Technical Report; 2020. [Google Scholar] [CrossRef]
- Entwistle, J.A.; Hursthouse, A.S.; Marinho Reis, P.A.; Stewart, A.G. Metalliferous mine dust: Human health impacts and the potential determinants of disease in mining communities. Curr. Pollut. Rep. 2019, 5, 67–83. [Google Scholar] [CrossRef] [Green Version]
- Stewart, A.G. Mining is bad for health: A voyage of discovery. Environ. Geochem. Health 2020, 42, 1153–1165. [Google Scholar] [CrossRef] [Green Version]
- Tian, S.; Liang, T.; Li, K.; Wang, L. Source and path identification of metals pollution in a mining area by PMF and rare earth element patterns in road dust. Sci. Total Environ. 2018, 633, 958–966. [Google Scholar] [CrossRef]
- Vaughan, J.; Tungpalan, K.; Parbhakar-Fox, A.; Fu, W.; Gagen, E.J.; Nkrumah, P.N.; Southam, G.; van der Ent, A.; Erskine, P.D.; Gow, P.; et al. Toward closing a loophole: Recovering rare earth elements from uranium metallurgical process tailings. JOM 2021, 73, 39–53. [Google Scholar] [CrossRef]
- Jiang, X.; Lu, W.X.; Zhao, H.Q.; Yang, Q.C.; Yang, Z.P. Potential ecological risk assessment and prediction of soil heavy-metal pollution around coal gangue dump. Nat. Hazards Earth Syst. Sci. 2014, 14, 1599–1610. [Google Scholar] [CrossRef] [Green Version]
- Johnson, D.; Potter, H.; Jones, C.; Rolley, S.; Watson, I.; Pritchard, J. Abandoned Mines and the Water Environment; Environment Agency: Bristol, UK, 2008.
- Younger, P.L.; Banwart, S.A.; Hedin, R.S. Mine Water: Hydrology, Pollution, Remediation; Environmental Pollution; Kluwer Academic Publishers: Dordrecht, The Netherlands; Boston, MA, USA, 2002; ISBN 978-1-4020-0137-6. [Google Scholar]
- Mazzotta, M. Sustainable Development Management Plan for NHS England 2018–2020; NHS England: Leeds, UK, 2018. Available online: https://www.england.nhs.uk/wp-content/uploads/2018/05/nhse-sustainable-development-management-plan-2018-2020.pdf (accessed on 23 January 2022).
- Gupta, S.K.; Nikhil, K. Ground water contamination in coal mining areas: A critical review. Int. J. Eng. Appl. Sci. 2016, 3, 69–74. [Google Scholar]
- Fayiga, A.O.; Ipinmoroti, M.; Chirene, T. Environmental pollution in Africa. Environ. Dev. Sustain. 2017, 20, 41–73. [Google Scholar] [CrossRef]
- Gál, J.; Hursthouse, A.; Tatner, P.; Stewart, F.; Welton, R. Cobalt and secondary poisoning in the terrestrial food chain: Data review and research gaps to support risk assessment. Environ. Int. 2008, 34, 821–838. [Google Scholar] [CrossRef]
- Sharifuzzaman, S.M.; Rahman, H.; Ashekuzzaman, S.M.; Islam, M.M.; Chowdhury, S.R.; Hossain, M.S. Heavy Metals Accumulation in Coastal Sediments. In Environmental Remediation Technologies for Metal-Contaminated Soils; Hasegawa, H., Rahman, I.M.d.M., Rahman, M.A., Eds.; Springer: Tokyo, Japan, 2016; pp. 21–42. ISBN 978-4-431-55758-6. [Google Scholar]
- Zbyszewski, M.; Corcoran, P.L. Distribution and degradation of fresh water plastic particles along the beaches of Lake Huron, Canada. Water Air Soil Pollut. 2011, 220, 365–372. [Google Scholar] [CrossRef]
- Vidal-Durà, A.; Burke, I.T.; Stewart, D.I.; Mortimer, R.J.G. Reoxidation of estuarine sediments during simulated resuspension events: Effects on nutrient and trace metal mobilisation. Estuar. Coast. Shelf Sci. 2018, 207, 40–55. [Google Scholar] [CrossRef]
- Yokota, K.; Waterfield, H.; Hastings, C.; Davidson, E.; Kwietniewski, E.; Wells, B. Finding the missing piece of the aquatic plastic pollution puzzle: Interaction between primary producers and microplastics. Limnol. Oceanogr. Lett. 2017, 2, 91–104. [Google Scholar] [CrossRef] [Green Version]
- Valipour, R.; Boegman, L.; Bouffard, D.; Rao, Y.R. Sediment resuspension mechanisms and their contributions to high-turbidity events in a large lake. Limnol. Oceanogr. 2017, 62, 1045–1065. [Google Scholar] [CrossRef] [Green Version]
- Kerfoot, W.C.; Urban, N.; Jeong, J.; MacLennan, C.; Ford, S. Copper-Rich “halo” off Lake Superior’s Keweenaw Peninsula and how mass mill tailings dispersed onto tribal lands. J. Gt. Lakes Res. 2020, 46, 1423–1443. [Google Scholar] [CrossRef]
- Kalnejais, L.H.; Martin, W.R.; Signell, R.P.; Bothner, M.H. Role of sediment resuspension in the remobilization of particulate-phase metals from coastal sediments. Environ. Sci. Technol. 2007, 41, 2282–2288. [Google Scholar] [CrossRef]
- He, T.; Jin, L.; Li, X. On the Triad of air particulate pollution, pathogenic bioaerosols, and lower respiratory infection. Environ. Geochem. Health 2021, 1–11. [Google Scholar] [CrossRef]
- Lelieveld, J.; Evans, J.S.; Fnais, M.; Giannadaki, D.; Pozzer, A. The contribution of outdoor air pollution sources to premature mortality on a global scale. Nature 2015, 525, 367–371. [Google Scholar] [CrossRef]
- Johansson, J.H.; Salter, M.E.; Navarro, J.C.A.; Leck, C.; Nilsson, E.D.; Cousins, I.T. Global transport of perfluoroalkyl acids via sea spray aerosol. Environ. Sci. Process. Impacts 2019, 21, 635–649. [Google Scholar] [CrossRef] [Green Version]
- Allen, S.; Allen, D.; Phoenix, V.R.; Le Roux, G.; Durántez Jiménez, P.; Simonneau, A.; Binet, S.; Galop, D. Atmospheric transport and deposition of microplastics in a remote mountain catchment. Nat. Geosci. 2019, 12, 339–344. [Google Scholar] [CrossRef]
- Potgieter-Vermaak, S.; Rotondo, G.; Novakovic, V.; Rollins, S.; Van Grieken, R. Component-specific toxic concerns of the inhalable fraction of urban road dust. Environ. Geochem. Health 2012, 34, 689–696. [Google Scholar] [CrossRef]
- Patinha, C.; Durães, N.; Sousa, P.; Dias, A.C.; Reis, A.P.; Noack, Y.; Ferreira da Silva, E. Assessment of the influence of traffic-related particles in urban dust using sequential selective extraction and oral bioaccessibility tests. Environ. Geochem. Health 2015, 37, 707–724. [Google Scholar] [CrossRef]
- Amato-Lourenço, L.F.; dos Santos Galvão, L.; de Weger, L.A.; Hiemstra, P.S.; Vijver, M.G.; Mauad, T. An emerging class of air pollutants: Potential effects of microplastics to respiratory human health? Sci. Total Environ. 2020, 749, 141676. [Google Scholar] [CrossRef]
- UNSCEAR. Sources, Effects and Risks of Ionizing Radiation; United Nations Scientific Committee on the Effects of Atomic Radiation 1988 Report to the General Assembly, with Annexes; United Nations: New York, NY, USA, 1988. [Google Scholar]
- Masson, O.; Baeza, A.; Bieringer, J.; Brudecki, K.; Bucci, S.; Cappai, M.; Carvalho, F.P.; Connan, O.; Cosma, C.; Dalheimer, A.; et al. Tracking of airborne radionuclides from the damaged Fukushima Dai-Ichi nuclear reactors by European networks. Environ. Sci. Technol. 2011, 45, 7670–7677. [Google Scholar] [CrossRef]
- Eurocontrol. Ash-Cloud of April and May 2010: Impact on Air Traffic; European Organisation for the Safety of Air Navigation: Brussels, Belgium, 2010. [Google Scholar]
- Harrison, R.G.; Nicoll, K.A.; Marlton, G.J.; Ryder, C.L.; Bennett, A.J. Saharan dust plume charging observed over the UK. Environ. Res. Lett. 2018, 13, 054018, Erratum in Environ. Res. Lett. 2018, 13, 109502. [Google Scholar] [CrossRef] [Green Version]
- Gauderman, W.J.; Vora, H.; McConnell, R.; Berhane, K.; Gilliland, F.; Thomas, D.; Lurmann, F.; Avol, E.; Kunzli, N.; Jerrett, M.; et al. Effect of exposure to traffic on lung development from 10 to 18 years of age: A cohort study. Lancet 2007, 369, 571–577. [Google Scholar] [CrossRef]
- National Research Council. Science for Environmental Protection: The Road Ahead; The National Academies Press: Washington, DC, USA, 2012; ISBN 978-0-309-26489-1. [Google Scholar]
- World Bank. The Global Health Cost of PM2.5 Air Pollution: A Case for Action beyond 2021; World Bank: Washington, DC, USA, 2021; ISBN 978-1-4648-1816-5. [Google Scholar]
- Arrow, K.J.; Cropper, M.L.; Eads, G.C.; Hahn, R.W.; Lave, L.B.; Noll, R.G.; Portney, P.R.; Russell, M.; Schmalensee, R.; Smith, V.K.; et al. Is there a role for benefit-cost analysis in environmental, health and safety regulation? Science 1996, 272, 221–222. [Google Scholar] [CrossRef] [PubMed]
- Beggs, P.J.; Bambrick, H.J. Is the global rise of asthma an early impact of anthropogenic climate change? Environ. Health Perspect. 2005, 113, 915–919. [Google Scholar] [CrossRef]
- Levin, K.; Cashore, B.; Bernstein, S.; Auld, G. Overcoming the tragedy of super wicked problems: Constraining our future selves to ameliorate global climate change. Policy Sci. 2012, 45, 123–152. [Google Scholar] [CrossRef]
- Costello, A.; Montgomery, H.; Watts, N. Climate change: The challenge for healthcare professionals. BMJ 2013, 347, f6060. [Google Scholar] [CrossRef]
- Finch, C. The Role of Global Air Pollution in Aging and Disease, 1st ed.; Academic Press: London, UK, 2018; ISBN 978-0-12-813102-2. [Google Scholar]
- Muir, J. My First Summer in the Sierra; Houghton Mifflin: Boston, MA, USA, 1911; ISBN 978 0217618649. [Google Scholar]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gibson, G.; Stewart, A.G. Unnatural Cycles: Anthropogenic Disruption to Health and Planetary Functions. Geosciences 2022, 12, 137. https://doi.org/10.3390/geosciences12030137
Gibson G, Stewart AG. Unnatural Cycles: Anthropogenic Disruption to Health and Planetary Functions. Geosciences. 2022; 12(3):137. https://doi.org/10.3390/geosciences12030137
Chicago/Turabian StyleGibson, Gillian, and Alex G. Stewart. 2022. "Unnatural Cycles: Anthropogenic Disruption to Health and Planetary Functions" Geosciences 12, no. 3: 137. https://doi.org/10.3390/geosciences12030137
APA StyleGibson, G., & Stewart, A. G. (2022). Unnatural Cycles: Anthropogenic Disruption to Health and Planetary Functions. Geosciences, 12(3), 137. https://doi.org/10.3390/geosciences12030137