Selenium Content in the Gonads of Healthy Cats (Felis catus) and Cats with Impaired Homeostasis from the Warsaw Area (Poland)
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Animals
2.2. Chemical Analyses
2.3. Statistical Analysis
3. Results and Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Fairweather-Tait, S.J.; Collings, R.; Hurst, R. Selenium bioavailability: Current knowledge and future research requirements. Am. J. Clin. Nutr. 2010, 91, 1484S–1491S. [Google Scholar] [CrossRef]
- Zhang, Y.; Roh, Y.J.; Han, S.J.; Park, I.; Lee, H.M.; Ok, Y.S.; Lee, B.C.; Lee, S.R. Role of selenoproteins in redox regulation of signaling and the antioxidant system: A Review. Antioxidants 2020, 9, 383. [Google Scholar] [CrossRef]
- Levander, O.A.; Ager, A.L.; Beck, M.A. Vitamin E and selenium: Contrasting and interacting nutritional determinants of host resistance to parasites and viral infections. Proc. Nutr. Soc. 1995, 54, 475–487. [Google Scholar] [CrossRef] [PubMed]
- Flohe, L. Selenium in mammalian spermiogenesis. Biol. Chem. 2007, 388, 987–995. [Google Scholar] [CrossRef] [PubMed]
- Kieliszek, M. Selenium. In Advances in Food and Nutrition Research; Academic Press Inc.: Cambridge, MA, USA, 2021; Volume 96, pp. 417–429. ISBN 9780128206485. [Google Scholar]
- Mistry, H.D.; Pipkin, F.B.; Redman, C.W.; Poston, L. Selenium in reproductive health. Am. J. Obstet. Gynecol. 2012, 206, 21–30. [Google Scholar] [CrossRef] [PubMed]
- Kielczykowska, M.; Kocot, J.; Pazdzior, M.; Musik, I. Selenium—A fascinating antioxidant of protective properties. Adv. Clin. Exp. Med. 2018, 27, 245–255. [Google Scholar] [CrossRef] [PubMed]
- Behne, D.; Weiler, H.; Kyriakopoulos, A. Effects of selenium deficiency on testicular morphology and function in rats. J. Reprod. Fertil. 1996, 106, 291–297. [Google Scholar] [CrossRef] [PubMed]
- Ceko, M.J.; O’Leary, S.; Harris, H.H.; Hummitzsch, K.; Rodgers, R.J. Trace elements in ovaries: Measurement and physiology. Biol. Reprod. 2016, 94, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Irvine, D.S. Glutathione as a treatment for male infertility. Rev. Reprod. 1996, 1, 6–12. [Google Scholar] [CrossRef] [PubMed]
- Marin-Guzman, J.; Mahan, D.C.; Chung, Y.K.; Pate, J.L.; Pope, W.F. Effects of dietary selenium and vitamin E on boar performance and tissue responses, semen quality, and subsequent fertilization rates in mature gilts. J. Anim. Sci. 1997, 75, 2994–3003. [Google Scholar] [CrossRef]
- Qazi, I.H.; Angel, C.; Yang, H.; Zoidis, E.; Pan, B.; Wu, Z.; Ming, Z.; Zeng, C.J.; Meng, Q.; Han, H.; et al. Role of Selenium and Selenoproteins in Male Reproductive Function: A Review of Past and Present Evidences. Antioxidants 2019, 8, 268. [Google Scholar] [CrossRef]
- Cerolini, S.; Maldjian, A.; Surai, P.; Noble, R. Viability, susceptibility to peroxidation and fatty acid composition of boar semen during liquid storage. Anim. Reprod. Sci. 2000, 58, 99–111. [Google Scholar] [CrossRef]
- Mehdi, Y.; Hornick, J.L.; Istasse, L.; Dufrasne, I. Selenium in the environment, metabolism and involvement in body functions. Molecules 2013, 18, 3292–3331. [Google Scholar] [CrossRef]
- Skibniewska, E.M.; Skibniewski, M.; Kośla, T.; Urbańska-Słomka, G. Hair zinc levels in pet and feral cats (Felis catus). J. Elem. 2011, 16, 481–488. [Google Scholar] [CrossRef]
- Skibniewski, M.; Kośla, T.; Skibniewska, E.M. Manganese status in free ranging European bisons from Białowieża primeval forest. Bull. Vet. Inst. Pulawy 2010, 54, 429–432. [Google Scholar]
- Nguyen, D.X.; Massagué, J. Genetic determinants of cancer metastasis. Nat. Rev. Genet. 2007, 8, 341–352. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Li, W.; Guo, M.; Li, C.; Qiu, C. Protective role of selenium compounds on the proliferation, apoptosis, and angiogenesis of a canine breast cancer Cell Line. Biol. Trace Elem. Res. 2016, 169, 86–93. [Google Scholar] [CrossRef] [PubMed]
- Günay Uçmak, Z.; Koenhemsi, L.; Ateş, F.; Tarhan, D.; Öztürk Gürgen, H.; Yildirim, F.; Uçmak, M.; Kirşan, İ.; Ercan, A.M.; Or, M.E. Amounts of tissue magnesium and some trace elements in cats with mammary tumors related to various clinicopathological parameters. J. Trace Elem. Med. Biol. 2023, 79, 127246. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.J.; Choi, M.C.; Park, J.M.; Chung, A.S. Antitumor effects of selenium. Int. J. Mol. Sci. 2021, 22, 11844. [Google Scholar] [CrossRef]
- Combs, G.F., Jr. Current evidence and research needs to support a health claim for selenium and cancer prevention. J. Nutr. 2005, 135, 343–347. [Google Scholar]
- Zeng, H.; Combs, G.F. Selenium as an anticancer nutrient: Roles in cell proliferation and tumor cell invasion. J. Nutr. Biochem. 2008, 19, 1–7. [Google Scholar] [CrossRef]
- Abdulah, R.; Miyazaki, K.; Nakazawa, M.; Koyama, H. Chemical forms of selenium for cancer prevention. J. Trace Elem. Med. Biol. 2005, 19, 141–150. [Google Scholar] [CrossRef]
- Selenius, M.; Rundlöf, A.K.; Olm, E.; Fernandes, A.P.; Björnstedt, M. Selenium and the selenoprotein thioredoxin reductase in the prevention, treatment and diagnostics of cancer. Antioxid. Redox. Sign. 2010, 12, 867–880. [Google Scholar] [CrossRef]
- Kahya, M.C.; Nazıroğlu, M.; Çiğ, B. Selenium reduces mobile phone (900 MHz)—Induced oxidative stress, mitochondrial function, and apoptosis in breast cancer cells. Biol. Trace Elem. Res. 2014, 160, 285–293. [Google Scholar] [CrossRef]
- Thomas, R. Cytogenomics of feline cancers: Advances and opportunities. Vet. Sci. 2015, 2, 246–258. [Google Scholar] [CrossRef] [PubMed]
- Goldschmidt, M.H.; Pena, L.; Zappulli, V. Tumors of the mammary gland. In Tumors in Domestic Animals; Meuten, D.J., Ed.; Wiley-Blackwell: Hoboken, NJ, USA, 2017; pp. 723–765. [Google Scholar]
- Zappulli, V.; Rasotto, R.; Caliari, D.; Mainenti, M.; Peña, L.; Goldschmidt, M.H.; Kiupel, M. Prognostic evaluation of feline mammary carcinomas: A review of the literature. Vet. Pathol. 2015, 52, 46–60. [Google Scholar] [CrossRef]
- German, A.J. The growing problem of obesity in dogs and cats. J. Nutr. 2006, 136, 1940S–1946S. [Google Scholar] [CrossRef] [PubMed]
- Lusby, A.L.; Kirk, C.A.; Bartges, J.W. The role of key adipokines in obesity and insulin resistance in cats. J. Am. Vet. Med. Assoc. 2009, 235, 518–522. [Google Scholar] [CrossRef] [PubMed]
- Suzuki, K.; Simpson, K.A.; Minnion, J.S.; Shillito, J.C.; Bloom, S.R. The role of gut hormones and the hypothalamus in appetite regulation. Endocr. J. 2010, 57, 359–372. [Google Scholar] [CrossRef] [PubMed]
- Loftus, J.P.; Wakshlag, J.J. Canine and feline obesity: A review of pathophysiology, epidemiology, and clinical management. Vet. Med. 2015, 30, 49–60. [Google Scholar] [CrossRef]
- Slingerland, L.I.; Fazilova, V.V.; Plantinga, E.A.; Kooistra, H.S.; Beynen, A.C. Indoor confinement and physical inactivity rather than the proportion of dry food are risk factors in the development of feline type 2 diabetes mellitus. Vet. J. 2009, 179, 247–253. [Google Scholar] [CrossRef]
- Kienzle, E.; Bergler, R.; Mandernach, A. A comparison of the feeding behavior and the human-animal relationship in owners of normal and obese dogs. J. Nutr. 1998, 128, 2779S–2782S. [Google Scholar] [CrossRef]
- Kienzle, E.; Bergler, R. Human–animal relationship of owners of normal and overweight cats. J. Nutr. 2006, 136, 1947S–1950S. [Google Scholar] [CrossRef]
- Skibniewska, E.M.; Skibniewski, M.; Kołnierzak, M. Muscle selenium content in red deer (Cervus elaphus), roe deer (Capreolus capreolus) and cattle (Bos taurus) from north-eastern Poland. J. Elem. 2020, 25, 621–631. [Google Scholar] [CrossRef]
- Schomburg, L.D.L. Variations in selenium metabolism in males and females. In Selenium: Its Molecular Biology and Role in Human Health; Hatfield, D.L., Berry, M.J., Gladyshev, V.N., Eds.; Springer Science Business Media, LLC.: Philadelphia, PA, USA, 2012. [Google Scholar] [CrossRef]
- Roveri, A.; Orsini, F.; Flohe, L.; Miorino, M. PHGPx and spermatogenesis. Biofactors 2001, 12, 213–222. [Google Scholar] [CrossRef] [PubMed]
- Romagnoli, S.; Bensaia, C.; Ferré-Dolcet, L.; Sontas, H.B.; Stelletta, C. Fertility parameters and reproductive management of Norwegian Forest Cats, Maine Coon, Persian and Bengal cats raised in Italy: A questionnaire-based study. J. Feline Med. Surg. 2019, 21, 1188–1197. [Google Scholar] [CrossRef] [PubMed]
- Ng, T.T.; Fascetti, A.J.; Larsen, J.A. Reproduction of domestic cats in laboratories, catteries, and feral colonies: A Review. Top Companion Anim. Med. 2023, 55, 100780. [Google Scholar] [CrossRef] [PubMed]
- Forrer, R.; Gautschi, K.; Lutz, H. Comparative determination of selenium in the serum of various animal species and humans by means of electrothermal atomic absorption spectrometry. J. Trace Elem. Electrolytes Health Dis. 1991, 5, 101–113. [Google Scholar] [PubMed]
- Foster, D.J.; Thoday, K.L.; Arthur, J.R.; Nicol, F.; Beatty, J.A.; Svendsen, C.K.; Labuc, R.; McConnell, M.; Sharp, M.; Thomas, J.B.; et al. Selenium status of cats in four regions of the world and comparison with reported incidence of hyperthyroidism in cats in those regions. Am. J. Vet. Res. 2001, 62, 934–937. [Google Scholar] [CrossRef] [PubMed]
- Todd, S.E.; Thomas, D.G.; Hendriks, W.H. Selenium balance in the adult cat in relation to intake of dietary sodium selenite and organically bound selenium. J. Anim. Physiol. Anim. Nutr. 2011, 96, 148–158. [Google Scholar] [CrossRef] [PubMed]
- Allen, M.E.; Ullrey, D.E. Relationships among nutrition and reproduction and relevance for wild animals. Zoo. Biol. 2004, 23, 475–487. [Google Scholar] [CrossRef]
- Bogden, J.D.; Kemp, F.W.; Chen, X.; Stagnaro-Green, A.; Stein, T.P.; Scholl, T.O. Low-normal serum selenium early in human pregnancy predicts lower birth weight. Nutr. Res. 2006, 26, 497–502. [Google Scholar] [CrossRef]
- Kumar, N.; Garg, A.K.; Dass, R.S.; Chaturvedi, V.K.; Mudgal, V.; Varshney, V.P. Selenium supplementation influences growth performance, antioxidant status and immune response in lambs. Anim. Feed Sci. Technol. 2009, 153, 77–87. [Google Scholar] [CrossRef]
- Ren, Y.; Wang, Q.; Shi, L.; Yue, W.; Zhang, C.; Lei, F. Effects of maternal and dietary selenium (Se-enriched yeast) on the expression of p34cdc2 and CyclinB1 of germ cells of their offspring in goats. Anim. Reprod. Sci. 2011, 123, 187–191. [Google Scholar] [CrossRef]
- Pfeifer, H.; Conrad, M.; Roethlein, D.; Kyriakopoulos, A.; Brielmeier, M.; Bornkamm, G.W.; Behne, D. Identification of a specific sperm nuclei selenoenzyme necessary for protamine thiol crosslinking during sperm maturation. FASEB J. 2001, 15, 1236–1238. [Google Scholar] [CrossRef]
- Rederstorff, M.; Krol, A.; Lescure, A. Understanding the importance of selenium and selenoproteins in muscle function. Cell. Mol. Life Sci. 2006, 63, 52–59. [Google Scholar] [CrossRef] [PubMed]
- Neville, T.L.; Caton, J.S.; Hammer, C.J.; Reed, J.J.; Luther, J.S.; Taylor, J.B.; Redmer, D.A.; Reynolds, L.P.; Vonnahme, K.A. Ovine offspring growth and diet digestibility are influenced by maternal selenium supplementation and nutritional intake during pregnancy despite a common postnatal diet. J. Anim. Sci. 2010, 88, 3645–3656. [Google Scholar] [CrossRef][Green Version]
- Adeniyi, M.J.; Agoreyo, F.O.; Olorunnisola, O.L.; Olaniyan, O.T.; Seriki, S.A.; Ozolua, O.P.; Odetola, A.A. Photo-pollution disrupts reproductive homeostasis in female rats: The duration-dependent role of selenium administrations. Chin. J. Physiol. 2020, 63, 235–243. [Google Scholar] [CrossRef]
- Carr, S.; Jia, Y.; Crites, B.; Hamilton, C.; Burris, W.; Edwards, J.L.; Matthews, J.; Bridges, P.J. Form of supplemental selenium in vitamin-mineral premixes differentially affects early luteal and gestational concentrations of progesterone, and postpartum concentrations of prolactin in beef cows. Animals 2020, 10, 967. [Google Scholar] [CrossRef]
- Moreno-Reyes, R.; Suetens, C.; Mathieu, F.; Begaux, F.; Zhu, D.; Rivera, M.T.; Boelaert, M.; Neve, J.; Perlmutter, N.; Vanderpas, L. Kashin– Beck osteoarthropathy in rural Tibet in relation to selenium and iodine status. N. Engl. J. Med. 1998, 339, 1112–1120. [Google Scholar] [CrossRef]
- Köhrle, J.; Jakob, F.; Contempre, B.; Dumont, J.E. Selenium, the thyroid, and the endocrine system. Endocr. Rev. 2005, 26, 944–984. [Google Scholar] [CrossRef]
- Ebert, R.; Jakob, F. Selenium deficiency as a putative risk factor for osteoporosis. Int. Congr. Series. 2007, 1297, 158–164. [Google Scholar] [CrossRef]
- Ren, F.L.; Guo, X.; Zhang, R.J.; Wang, S.J.; Zuo, H.; Zhang, Z.T.; Geng, D.; Yu, Y.; Su, M. Effects of selenium and iodine deficiency on bone, cartilage growth plate and chondrocyte differentiation in two generations of rats. Osteoarthr. Cartil. 2007, 15, 1171–1177. [Google Scholar] [CrossRef]
- Taylor, E.W.; Nadimpalli, R.G.; Ramanathan, C.S. Genomic structures of viral agents in relation to the biosynthesis of selenoproteins. Biol. Trace Elem. Res. 1997, 56, 63–91. [Google Scholar] [CrossRef]
- Kasaikina, M.V.; Kravtsova, M.A.; Lee, B.C.; Seravalli, J.; Peterson, D.A.; Walter, J.; Legge, R.; Benson, A.K.; Hatfield, D.L.; Gladyshev, V.N. Dietary selenium affects host selenoproteome expression by influencing the gut microbiota. FASEB J. 2011, 25, 2492–2499. [Google Scholar] [CrossRef] [PubMed]
- Huang, Z.; Rose, A.H.; Hoffmann, P.R. The role of selenium in inflammation and immunity: From molecular mechanisms to therapeutic opportunities. Antioxid. Redox. Signal. 2012, 16, 705–743. [Google Scholar] [CrossRef]
- Arthur, J.R.; Beckett, G.J.; Mitchell, J.H. The interactions between selenium and iodine deficiencies in man and animals. Nutr. Res. Rev. 1999, 12, 55–73. [Google Scholar] [CrossRef] [PubMed]
- Hatfield, D.L.; Gladyshev, V.N. How selenium has altered our understanding of the genetic code. Mol. Cell. Biol. 2002, 22, 3565–3576. [Google Scholar] [CrossRef]
- Rucker, R.B.; Fascetti, A.J.; Keen, C.L. Trace minerals. In Clinical Biochemistry of Domestic Animals, 6th ed.; Kaneko, J.J., Harvey, J.W., Eds.; Academic: Burlington, VT, USA, 2008; pp. 663–694. [Google Scholar]
- McCann, J.C.; Ames, B.N. Adaptive dysfunction of selenoproteins from the perspective of the triage theory: Why modest selenium deficiency may increase risk of diseases of aging. FASEB J. 2011, 25, 1793–1814. [Google Scholar] [CrossRef] [PubMed]
- Mirone, M.; Giannetta, E.; Isidori, A.M. Selenium and reproductive function. A systematic review. J. Endocrinol. Investig. 2013, 36, 28–36. [Google Scholar]
- Singh, A.K.; Chattopadhyay, R.; Chakravarty, B.; Chaudhury, K. Markers of oxidative stress in follicular fluid of women with endometriosis and tubal infertility undergoing IVF. Reprod. Toxicol. 2013, 42C, 116–124. [Google Scholar] [CrossRef]
- Fairweather-Tait, S.J.; Bao, Y.; Broadley, M.R.; Collings, R.; Ford, D.; Hesketh, J.E.; Hurst, R. Selenium in human health and disease. Antioxid. Redox. Sign. 2011, 14, 1337–1382. [Google Scholar] [CrossRef] [PubMed]
- Van Zelst, M.; Hesta, M.; Gray, K.; Staunton, R.; Du Laing, G.; Janssens, G.P. Biomarkers of selenium status in dogs. BMC Vet. Res. 2016, 12, 15. [Google Scholar] [CrossRef]
- Alfthan, G.; Aro, A.; Arvilommi, H.; Huttunen, J.K. Selenium metabolism and platelet glutathione peroxidase activity in healthy Finnish men: Effects of selenium yeast, selenite, and selenate. Am. J. Clin. Nutr. 1991, 53, 120–125. [Google Scholar] [CrossRef]
- Wedekind, K.J.; Cowell, C.; Combs, G.F., Jr. Bioavailability of selenium in petfood ingredients. FASEB J. 1997, 11, A360. [Google Scholar]
- Todd, S.E.; Thomas, D.G.; Bosch, G.; Hendriks, W.H. Selenium status in adult cats and dogs fed high levels of dietary inorganic and organic selenium. J. Anim. Sci. 2012, 90, 2549–2555. [Google Scholar] [CrossRef]
- Enginler, S.O.; Toydemir, T.S.F.; Ates, A.; Oztürk, B.; Erdogan, O.; Ozdemir, S.; Kýrsan, I.; Or, M.E.; Arun, S.S.; Barutcu, U.B. Examination of oxidative/antioxidative status and trace element levels in dogs with mammary tumors. Bulg. J. Agric. Sci. 2015, 21, 1086–1091. [Google Scholar]
- Pilarczyk, B.; Tomza-Marciniak, A.; Pilarczyk, R.; Bąkowska, M.; Gaik, M.; Wilk, M.; Kuba, J. Relationship between serum Se concentration in dogs and incidence of some disease conditions. Cent. Eur. J. Biol. 2013, 8, 527–533. [Google Scholar] [CrossRef]
- Overley, B.; Shofer, F.S.; Goldschmidt, M.H.; Sherer, D.; Sorenmo, K.U. Association between ovarihysterectomy and feline mammary carcinoma. J. Vet. Intern. Med. 2005, 19, 560–563. [Google Scholar] [CrossRef]
- Forte, G.; Ariu, F.; Bocca, B.; Solinas, G.; Leoni, G.G.; Podda, A.; Madeddu, R.; Bogliolo, L. Heavy Metal(loid) accumulation in the ovarian tissue of free-ranging queens and bitches Inhabiting highly polluted urban environments. Animals 2023, 13, 650. [Google Scholar] [CrossRef]
- Eisen, J.L.; Sibrava, N.J.; Boisseau, C.L.; Mancebo, M.C.; Stout, R.L.; Pinto, A.; Rasmussen, S.A. Five-year course of obsessive-compulsive disorder: Predictors of remission and relapse. J. Clin. Psychiatry 2013, 74, 233–239. [Google Scholar] [CrossRef]
- Costa, D.; da Conceição, L.; de Campos, A.P.; de Bragança Pereira, C.A.; Torres, A.R.; dos Santos, A.C.; Requena, G.; Ferrão, Y.A.; do Rosário, M.C.; Miguel, E.C.; et al. Latency to treatment seeking in patients with obsessive-compulsive disorder: Results from a large multicenter clinical sample. Psychiatry Res. 2022, 312, 114567. [Google Scholar] [CrossRef] [PubMed]
- Fontenelle, L.F.; Nicolini, H.; Brakoulias, V. Early intervention in obsessive-compulsive disorder: From theory to practice. Compr. Psychiatry 2022, 119, 152353. [Google Scholar] [CrossRef] [PubMed]
- Funahashi, T.; Shimomura, I.; Matsuzawa, Y. Adipocytokines. In Encyclopedia of Endocrine Diseases; Martini, L., Ed.; Elsevier: Amsterdam, The Netherlands, 2004; pp. 41–44. [Google Scholar]
- Skoog, G.; Skoog, I. A 40-year follow-up of patients with obsessive-compulsive disorder. Arch. Gen. Psychiatry 1999, 56, 121–127. [Google Scholar] [CrossRef] [PubMed]
- Thompson, E.M.; Torres, A.R.; Albertella, L.; Ferrão, Y.A.; Tiego, J.; Shavitt, R.G.; Conceição do Rosario, M.; Miguel, E.C.; Fontenelle, L.F. The speed of progression towards obsessive-compulsive disorder. J. Affec. Disord. 2020, 264, 181–186. [Google Scholar] [CrossRef] [PubMed]
- Niendam, T.A.; Berzak, J.; Cannon, T.D.; Bearden, C.E. Obsessive compulsive symptoms in the psychosis prodrome: Correlates of clinical and functional outcome. Schizophr. Res. 2009, 108, 170–175. [Google Scholar] [CrossRef] [PubMed]
- Hur, J.-W.; Shin, N.Y.; Jang, J.H.; Shim, G.; Park, H.Y.; Hwang, J.Y.; Kim, S.N.; Yoo, J.H.; Hong, K.S.; Kwon, J.S. Clinical and neurocognitive profiles of subjects at high risk for psychosis with and without obsessive–compulsive symptoms. Aust. N. Z. J. Psychiatry. 2012, 46, 161–169. [Google Scholar] [CrossRef]

 young females,
young females,  adult females,
adult females,  obese females,
obese females,  mammary carcinomas.
mammary carcinomas.
 young females,
young females,  adult females,
adult females,  obese females,
obese females,  mammary carcinomas.
mammary carcinomas.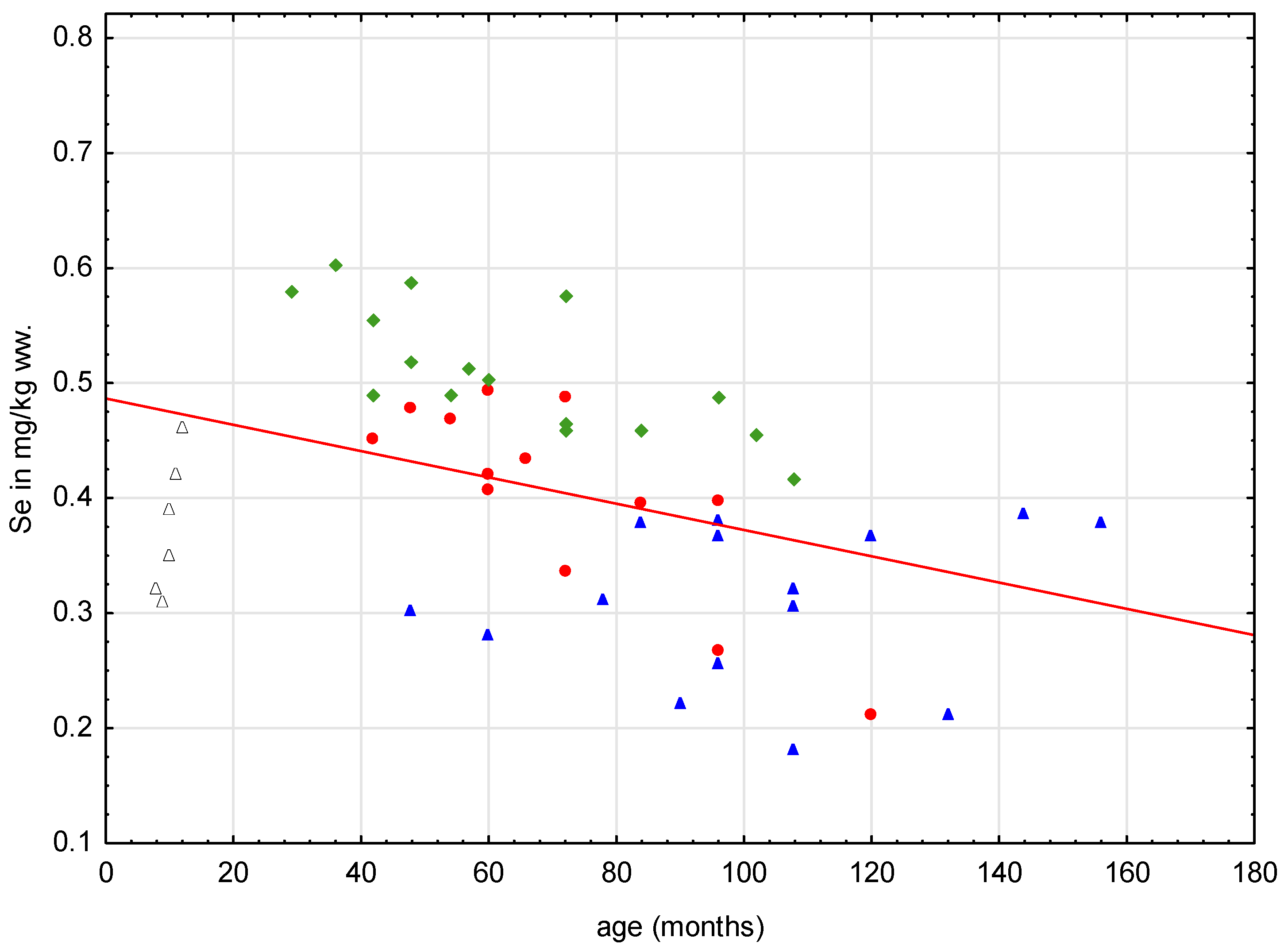

| Group | N | Mean | SD | Median | Min. | Max. | Q25 | Q75 | |
|---|---|---|---|---|---|---|---|---|---|
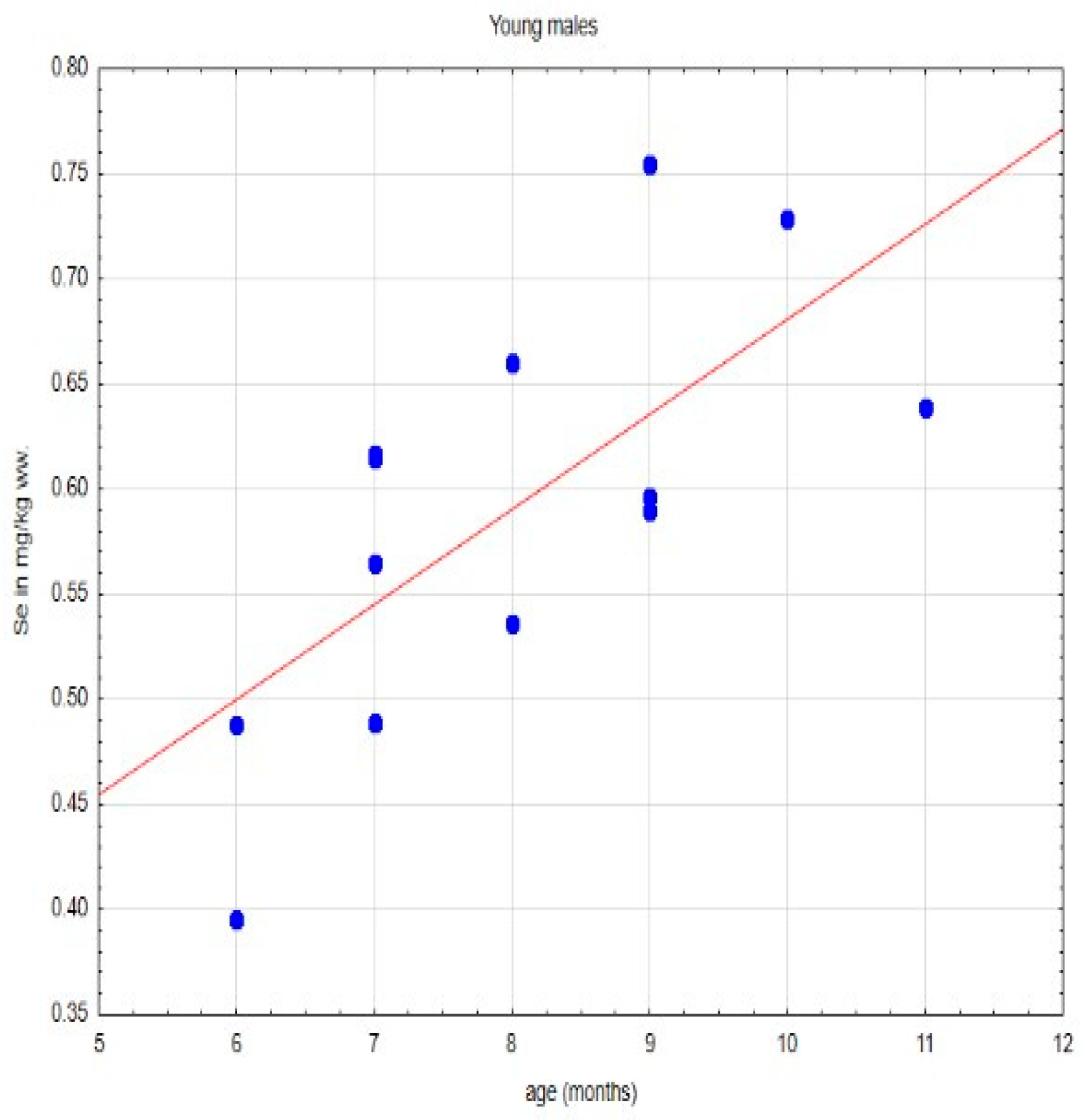
| Young males | Body mass | 13 | 2.98 | 0.41 | 3.0 | 2.1 | 3.6 | 2.8 | 3.2 |
| Age | 8.0 | 1.53 | 8.0 | 6.0 | 11 | 7 | 9 | ||
| Young females | Body mass | 6 | 1.83 | 0.26 | 1.8 | 1.5 | 2.2 | 1.6 | 2.0 |
| Age | 10 | 1.41 | 10 | 8.0 | 12.0 | 9.0 | 11.0 | ||
| Healthy females | Body mass | 16 | 4.1 | 1.22 | 4.0 | 2.9 | 6.0 | 3.3 | 4.45 |
| Age | 63.87 | 24.01 | 58.5 | 29.0 | 108.0 | 45.0 | 78.0 | ||
| Obese females | Body mass | 13 | 7.0 | 1.3 | 7.0 | 4.6 | 9.0 | 6.5 | 7.7 |
| Age | 71.5 | 22.1 | 66.0 | 42.0 | 120.0 | 60.0 | 84 | ||
| Females with mammary carcinomas | Body mass | 15 | 3.91 | 0.68 | 4.0 | 2.8 | 5.0 | 3.4 | 4.5 |
| Age | 101.6 | 29.08 | 96.0 | 48.0 | 156.0 | 84.0 | 120.0 |
| Group | N | Median | Min. | Max. | Q25 | Q75 |
|---|---|---|---|---|---|---|
| Healthy young males | 13 | 0.5960 | 0.3950 | 0.7550 | 0.5360 | 0.6390 |
| Group | N | Median | Min. | Max. | Q25 | Q75 |
|---|---|---|---|---|---|---|
| All females studied | 50 | 0.4120 | 0.1810 | 0.6020 | 0.3200 | 0.4870 |
| Healthy young females | 6 | 0.3700 A | 0.3100 | 0.460 | 0.3200 | 0.4200 |
| Healthy adult females | 16 | 0.4915 B | 0.4170 | 0.6020 | 0.4615 | 0.5650 |
| Obese females | 13 | 0.4200 C | 0.2120 | 0.5030 | 0.3950 | 0.4680 |
| Females with mammary gland carcinomas | 15 | 0.3120 A | 0.1810 | 0.3850 | 0.2560 | 0.3780 |
| Age group | N | Median | Min. | Max. | Q25 | Q75 |
|---|---|---|---|---|---|---|
| 20–60 months | 10 | 0.4725 A | 0.2800 | 0.6020 | 0.4200 | 0.5030 |
| ≥60–100 months | 21 | 0.4330 AB | 0.2200 | 0.5880 | 0.3670 | 0.4890 |
| ≥100 months | 13 | 0.3660 B | 0.1810 | 0.4640 | 0.3050 | 0.4170 |
| Se | Body Mass | Age (Months) | |
|---|---|---|---|
| Se | ------ | −0.0668 | −0.6753 ** |
| Body mass | −0.0668 | ------ | 0.1427 |
| Age (months) | −0.6753 ** | 0.1427 | ------- |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Skibniewska, E.M.; Skibniewski, M. Selenium Content in the Gonads of Healthy Cats (Felis catus) and Cats with Impaired Homeostasis from the Warsaw Area (Poland). Animals 2024, 14, 440. https://doi.org/10.3390/ani14030440
Skibniewska EM, Skibniewski M. Selenium Content in the Gonads of Healthy Cats (Felis catus) and Cats with Impaired Homeostasis from the Warsaw Area (Poland). Animals. 2024; 14(3):440. https://doi.org/10.3390/ani14030440
Chicago/Turabian StyleSkibniewska, Ewa M., and Michał Skibniewski. 2024. "Selenium Content in the Gonads of Healthy Cats (Felis catus) and Cats with Impaired Homeostasis from the Warsaw Area (Poland)" Animals 14, no. 3: 440. https://doi.org/10.3390/ani14030440
APA StyleSkibniewska, E. M., & Skibniewski, M. (2024). Selenium Content in the Gonads of Healthy Cats (Felis catus) and Cats with Impaired Homeostasis from the Warsaw Area (Poland). Animals, 14(3), 440. https://doi.org/10.3390/ani14030440





