Modified Proximal Interphalangeal Joint Arthrodesis in a Yearling Filly with an Osseous Cyst-Like Lesion in the Proximal Phalanx
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Case Selection and History
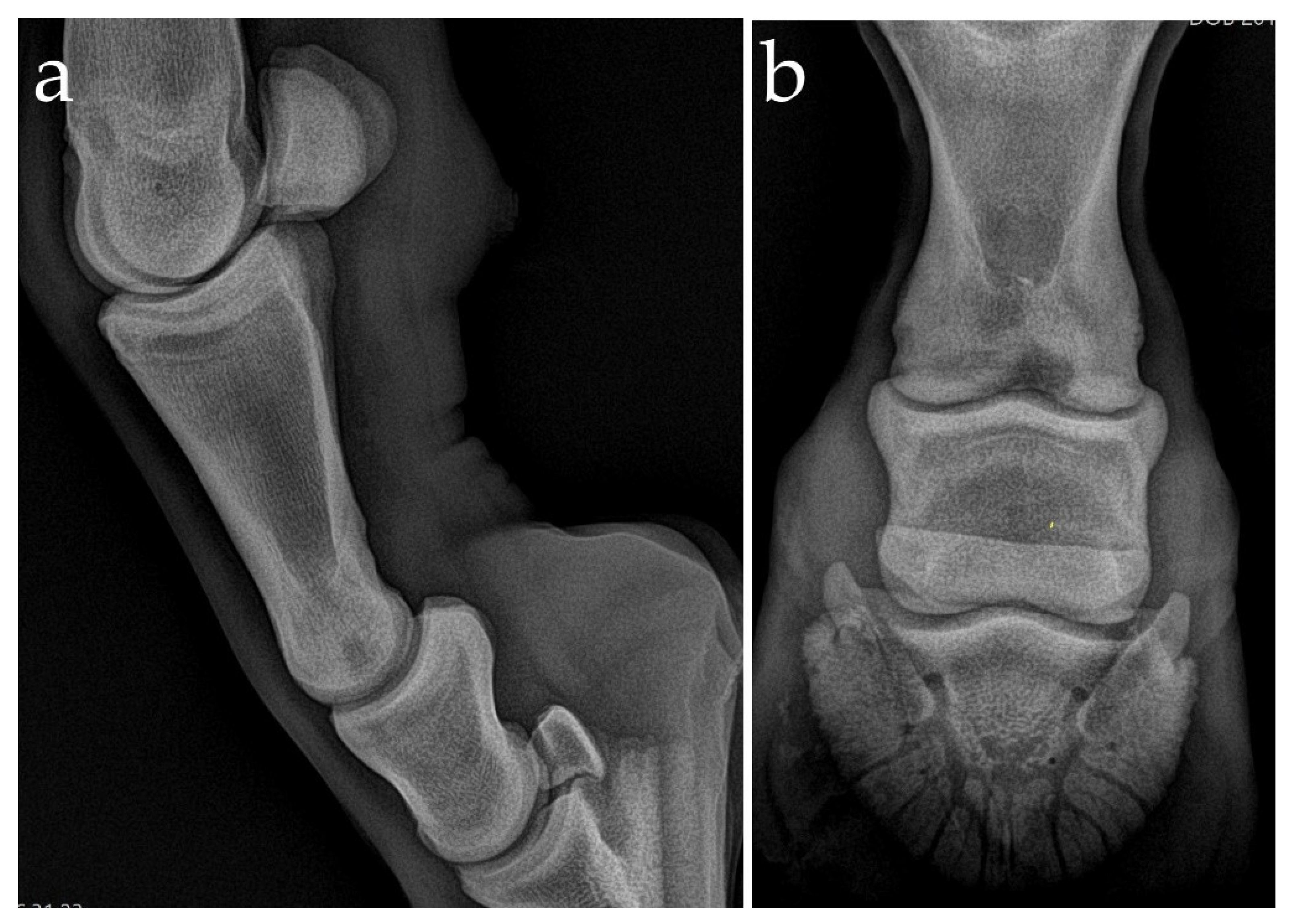
2.2. Clinical and Radiographic Examination
2.3. Preoperative Management
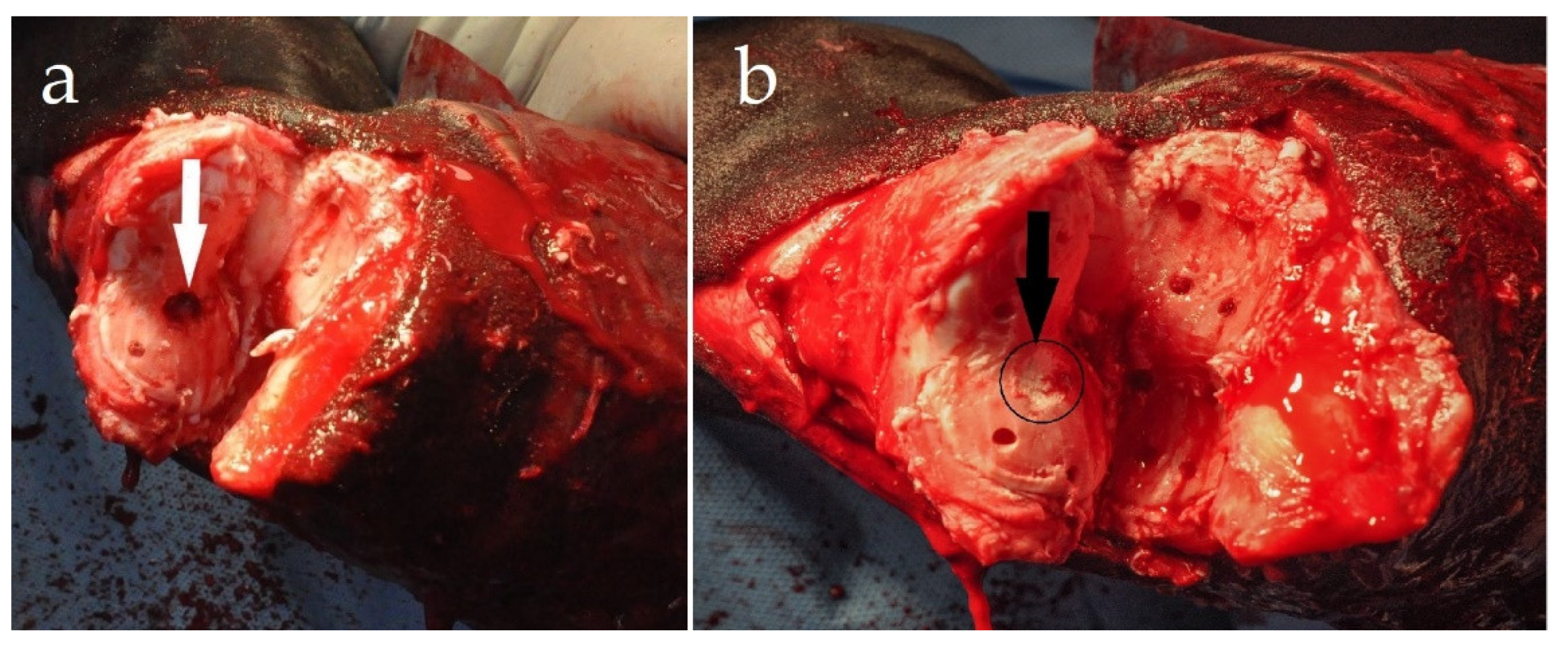
2.4. Surgical Procedure
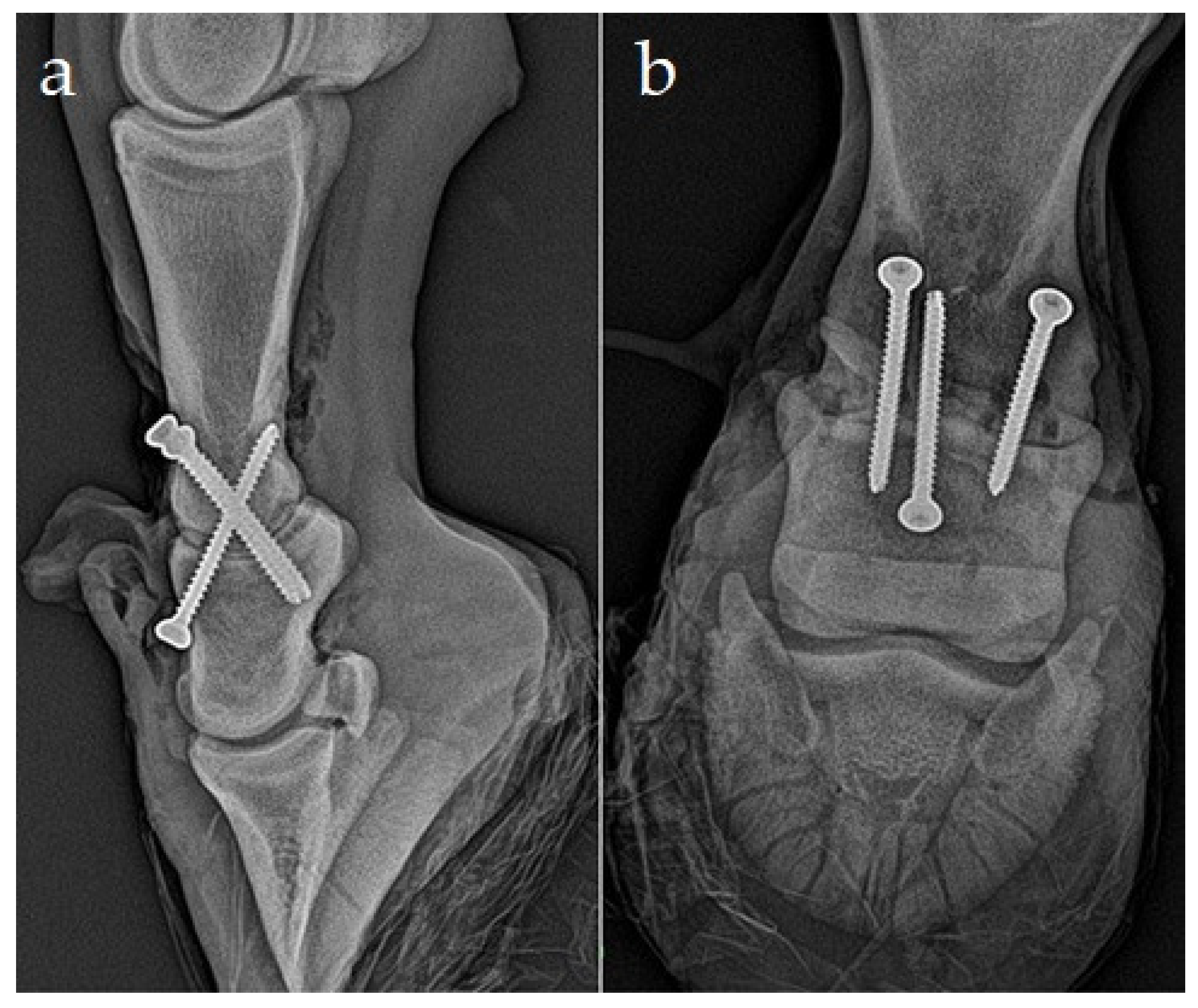
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Auer, J.A.; Lischer, C.J. Arthrodesis technique. In Equine Surgery, 5th ed.; Auer, J.A., Stick, J.A., Kümmerle, J.M., Prange, T., Eds.; Elsevier: St. Louis, MO, USA, 2019; p. 1377. [Google Scholar]
- Steenhaut, M.; Verschooten, F.; De Moor, A. Arthrodesis of the pastern joint in the horse. Equine Vet. J. 1985, 17, 35–40. [Google Scholar] [CrossRef]
- Schneider, J.E.; Guffy, M.M.; Leipold, H.W. Arthrodesis to correct deviation of the phalanges in the horse. J. Equine Vet. Sci. 1987, 7, 24–28. [Google Scholar] [CrossRef]
- Caron, J.P.; Fretz, P.B.; Bailey, J.V.; Barber, S.M. Proximal interphalangeal arthrodesis in the horse, a retrospective study and a modified screw technique. Vet. Surg. 1990, 19, 196–202. [Google Scholar] [CrossRef]
- Watts, A.E.; Fortier, L.A.; Caldwell, F.J. Proximal interphalangeal joint arthrodesis in a one-month-old foal for superficial digital flexor tendon and straight sesamoidean ligament disruption. Equine Vet. Educ. 2007, 19, 407–412. [Google Scholar] [CrossRef]
- Zert, Z.; Krisova, S.; Zuffova, K. Pastern joint arthrodesis using two paraaxial and one axial crossed lag screws: A case report. Vet. Med. 2013, 58, 322–326. [Google Scholar] [CrossRef]
- Taylor, E.; Anderson, D.; Patwell, J.; Plaut, K.; McCullough, K. Dorland’s Illustrated Medical Dictionary, 27th ed.; WB Saunders: Philadelphia, PA, USA, 1988. [Google Scholar]
- Redding, W. Pathologic conditions involving the internal structures of the foot. In Equine Podiatry; Floyd, A., Mansmann, R., Eds.; Saunders: St. Louis, MO, USA, 2007; pp. 253–293. [Google Scholar]
- Von Rechenberg, B.; McIlwraith, C.; Auer, J.A. Cystic bone lesions in horses and humans: A comparative review. Vet. Comp. Orthop. Traumatol. 1988, 11, 8–18. [Google Scholar]
- Trotter, G.; Dyson, S. Osseous cyst like lesions in the distal phalanx. In Diagnosis and Management of Lameness in the Horse; Ross, M., Dyson, S., Eds.; Saunders: St. Louis, MO, USA, 2003. [Google Scholar]
- Sherlock, C.; Mair, T. Osseous cyst-like lesions/subchondral bone cysts of the phalanges. Equine Vet. Educ. 2011, 23, 191–204. [Google Scholar] [CrossRef]
- Wagner, P.; Modransky, P.; Gavin, P.; Grant, B. Surgical management of subchondral bone cysts in the third phalanx in the horse. Equine Pract. 1982, 4, 9–15. [Google Scholar]
- White, N.; McIlwraith, C. Retrospective study of femoral bone cyst curettage in the horse. Vet. Surg. 1985, 14, 70. [Google Scholar]
- White, N.; McIlwraith, C.; Allen, D. Curettage of subchondral bone cysts in medial femoral condyles of the horse. Equine Vet. J. Suppl. 1988, 6, 120–124. [Google Scholar] [CrossRef]
- Sandler, E.B.; Bramlage, L.R.; Embertson, R.; Ruggles, A.; Frisbie, D. Correlation of radiographic appearance, lesion size and racing performance, after arthroscopic surgical treatment of subchondral cystic lesions of the medial femoral condyle in thoroughbreds: 150 cases. Vet. Surg. 2002, 31, 495. [Google Scholar]
- Hendrix, S.; Baxter, G.; Trumble, T.; McIlwraith, C. Association between medial mensical and medial femoral condyle subchondral lesions in horses. Vet. Surg. 2005, 34, E12. [Google Scholar]
- Smith, M.; Walmsley, J.; Phillips, T.; Pinchbeck, G.; Booth, T.; Greet, T.; Richardson, D.; Ross, M.; Schramme, M.; Singer, E.; et al. Effect of age at presentation on outcome following arthroscopic debridement of subchondral cystic lesions of the medial femoral condyle: 85 horses (1993–2003). Equine Vet. J. 2005, 37, 175–180. [Google Scholar] [CrossRef] [PubMed]
- Medvecky, L.; Giretova, M.; Stulajterova, R.; Kasiarova, M. Effect of microstructure characteristics on tetracalcium phosphate–nanomonetite cement in vitro cytotoxic city. Biomed. Mater. 2015, 10, 025006. [Google Scholar] [CrossRef] [PubMed]
- McIlwraith, C.W. Subchondral bone cysts in the horse: Aetiology, diagnosis and treatment options. Equine Vet. Educ. 1998, 10, 313–317. [Google Scholar] [CrossRef]
- Frisbie, D.D.; Werpy, N.M.; Kawcak, C.E.; Barrett, M.F. Distal Limb. In Joint Disease in the Horse, 2nd ed.; McIlwraith, C.W., Frisbie, D.D., Kawcak, C.E., Van Weeren, R.P., Eds.; WB Saunders: St. Louis, MO, USA, 2016; pp. 85–299. [Google Scholar]
- Jacquet, S.; Robert, C.; Valette, J.P.; Denoix, J.M. Evolution of radiological findings detected in the limbs of 321 young horses between the ages of 6 and 18 months. Vet. J. 2013, 197, 58–64. [Google Scholar] [CrossRef]
- Denoix, J.M.; Jeffcott, L.B.; McIlwraith, C.W.; van Weeren, P.R. A review of terminology for equine juvenile osteochondral conditions (JOCC) based on anatomical and functional considerations. Vet. J. 2013, 197, 29–35. [Google Scholar] [CrossRef]
- McIlwraith, C.W. Subchondral Cystic Lesions. In Joint Disease in the Horse, 2nd ed.; McIlwraith, C.W., Frisbie, D.D., Kawcak, C.E., Van Weeren, R.P., Eds.; WB Saunders: St. Louis, MO, USA, 2016; pp. 85–90. [Google Scholar]
- Kold, S.E.; Killingbeck, M. The use of autogenous cancellous bone graft for treatment of subchondral bone cysts in the distal phalanges: 3 cases. Equine Vet. Educ. 1998, 10, 307–312. [Google Scholar] [CrossRef]
- McIlwraith, C.W. Subchondral cystic lesions. Vet. Clinics North Am. Large Anim. Pract. 1983, 5, 350–355. [Google Scholar]
- Jackson, W.A.; Stick, J.A.; Arnoczky, S.P.; Nickels, F.A. The effect of compacted cancellous bone grafting on the healing of subchondral bone defects of the medial femoral condyle in horses. Vet. Surg. 2000, 29, 8–16. [Google Scholar] [CrossRef]
- Ortved, K.F.; Nixon, A.J.; Mohammed, H.O.; Fortier, L.A. Treatment of subchondral cystic lesions of the medial femoral condyle of mature horses with growth factor enhanced chondrocyte grafts: A retrospective study of 49 cases. Equine Vet. J. 2012, 44, 606–613. [Google Scholar] [CrossRef] [PubMed]
- Fürst, A.; Kaegi, B.; von Rechenberg, B.; Auer, J.A. Die Behandlung von 5 Pferdenmit subchondralen zystoiden Defekten im Fesselbein. Pferdeheilkunde 1997, 13, 147–161. (In German) [Google Scholar] [CrossRef]
- Bodo, G.; Hangody, L.; Modis, L.; Hurtig, M. Autologous osteochondral grafting (mosaic arthroplasty) for treatment of subchondral cystic lesions in the equine stifle and fetlock joints. Vet. Surg. 2004, 33, 588–596. [Google Scholar] [CrossRef] [PubMed]
- Jackson, M.A.; Ohlerth, S.; Kummer, M.; Bettschart, R.; Watson, J.; Manera, C.L.; von Rechenberg, B.; Auer, J.; Fürst, A. Use of a parathyroid hormone peptide (PTH 1-34)-enriched fibrin hydrogel for the treatment of subchondral cystic lesions in 15 horses. Pferdeheilkunde 2012, 28, 642–649. [Google Scholar] [CrossRef]
- Wallis, T.W.; Goodrich, L.R.; McIlwraith, C.W.; Frisbie, D.D.; Hendrickson, D.A.; Trotter, G.W.; Baxter, G.M.; Kawcak, C.E. Arthroscopic injection of corticosteroids into the fibrous tissue of subchondral cystic lesions of the medial femoral condyle in horses: A retrospective study of 52 cases (2001–2006). Equine Vet. J. 2008, 40, 461–467. [Google Scholar] [CrossRef] [PubMed]
- Santschi, E.M.; Williams, J.M.; Morgan, J.W.; Johnson, C.R.; Bertone, A.L.; Juzwiak, J.S. Preliminary investigation of the treatment of equine medial femoral condylar subchondral cystic lesions with a transcondylar screw. Vet. Surg. 2015, 44, 281–288. [Google Scholar] [CrossRef]
- Roquet, I.; Lane Easter, J.; Coomer, R.P.C.; Ezquerra, L.J.; Marsh, C.A.; Trostle, S.S.; Santschi, E.M. Treatment of subchondral lucencies in the medial proximal radius with a bone screw in 8 horses. Vet. Surg. 2017, 46, 478–485. [Google Scholar] [CrossRef] [PubMed]
- Tothova, C.; Novotny, J.; Nagy, O.; Hornakova, P.; Zert, Z.; Varga, M.; Medvecky, L.; Vdoviakova, K.; Danko, J.; Petrovova, E. Changes in the Acute-Phase Protein Con centrations and Activities of Some Enzymes in Pigs Following the Repair of Experimentally Induced Articular Cartilage Defects Using Two Types of Biocement Powder. Animals 2019, 9, 931. [Google Scholar] [CrossRef] [PubMed]
- Stashak, T.S. The foot: Luxation and subluxation of the proximal interphalangeal (pastern) joint. In Adams’ Lameness in Horses, 5th ed.; Stashak, T.S., Ed.; Lippincott, Williams, and Wilkins: Philadelphia, PA, USA, 2002; pp. 741–744. [Google Scholar]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kol’vek, F.; Krešáková, L.; Vdoviaková, K.; Medvecký, Ľ.; Žert, Z. Modified Proximal Interphalangeal Joint Arthrodesis in a Yearling Filly with an Osseous Cyst-Like Lesion in the Proximal Phalanx. Animals 2021, 11, 948. https://doi.org/10.3390/ani11040948
Kol’vek F, Krešáková L, Vdoviaková K, Medvecký Ľ, Žert Z. Modified Proximal Interphalangeal Joint Arthrodesis in a Yearling Filly with an Osseous Cyst-Like Lesion in the Proximal Phalanx. Animals. 2021; 11(4):948. https://doi.org/10.3390/ani11040948
Chicago/Turabian StyleKol’vek, Filip, Lenka Krešáková, Katarína Vdoviaková, Ľubomír Medvecký, and Zdeněk Žert. 2021. "Modified Proximal Interphalangeal Joint Arthrodesis in a Yearling Filly with an Osseous Cyst-Like Lesion in the Proximal Phalanx" Animals 11, no. 4: 948. https://doi.org/10.3390/ani11040948
APA StyleKol’vek, F., Krešáková, L., Vdoviaková, K., Medvecký, Ľ., & Žert, Z. (2021). Modified Proximal Interphalangeal Joint Arthrodesis in a Yearling Filly with an Osseous Cyst-Like Lesion in the Proximal Phalanx. Animals, 11(4), 948. https://doi.org/10.3390/ani11040948






