Impacts from Wildfires on Livestock Health and Production: Producer Perspectives
Abstract
:Simple Summary
Abstract
1. Introduction
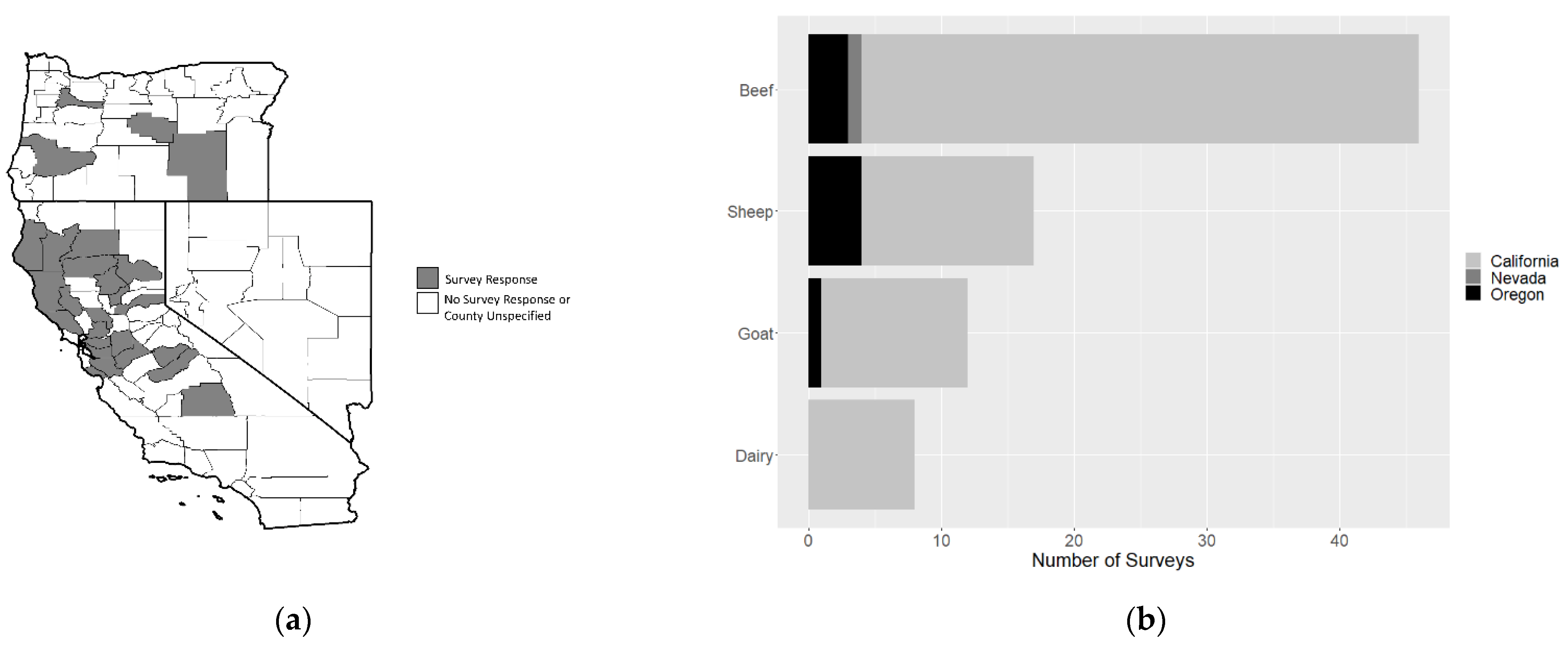
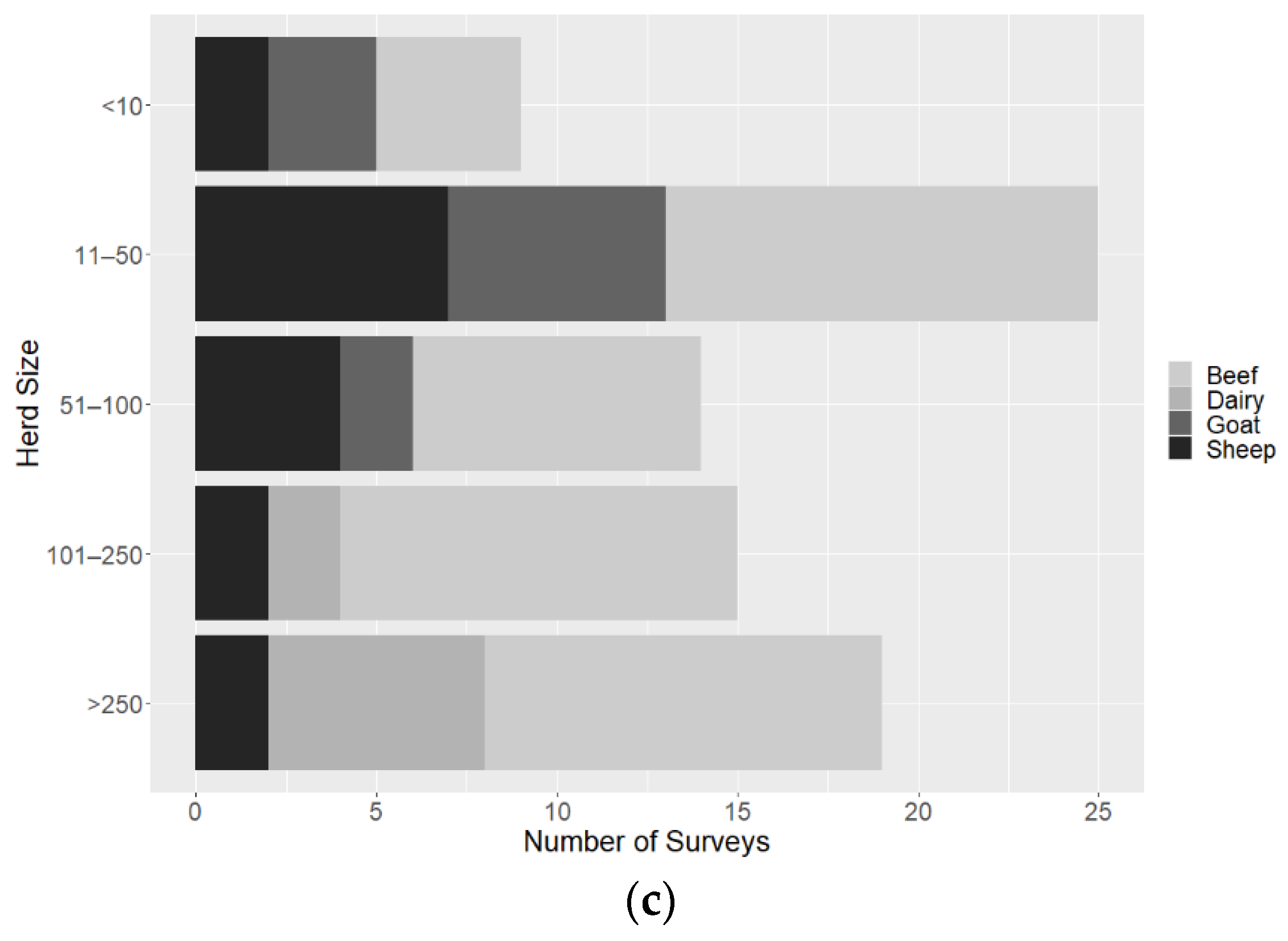
2. Materials and Methods
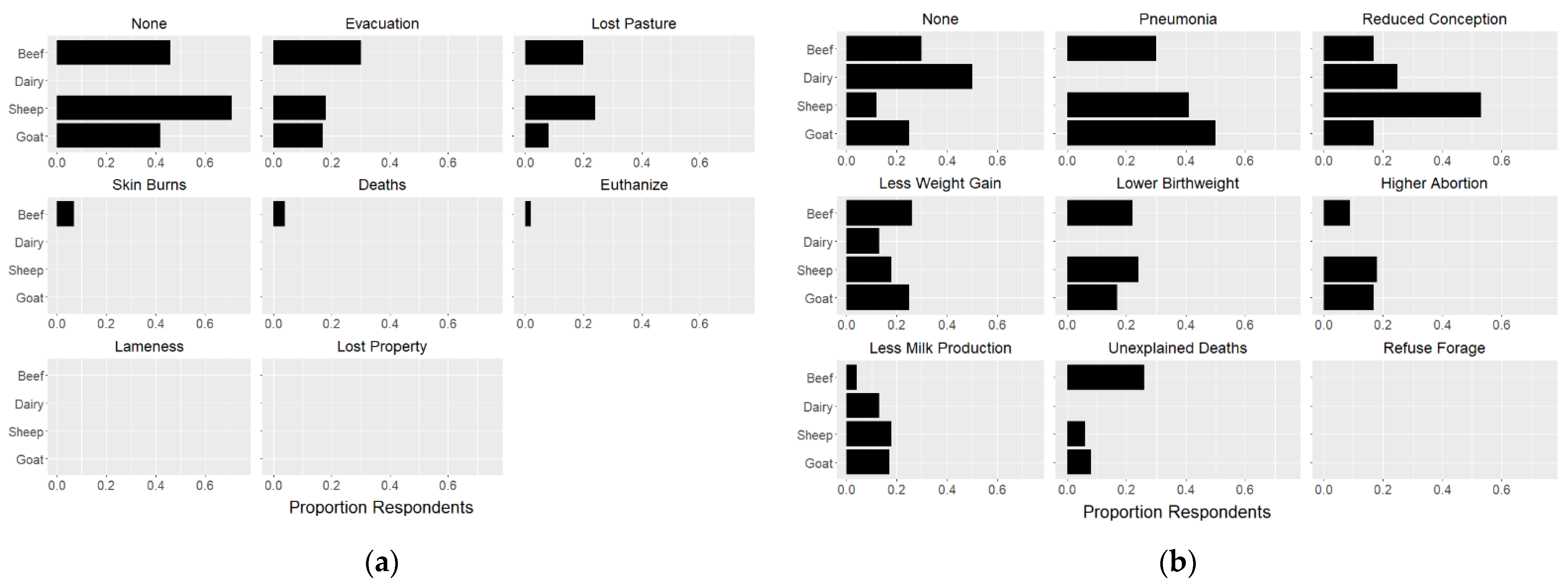
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Xu, R.; Yu, P.; Abramson, M.J.; Johnston, F.H.; Samet, J.M.; Bell, M.L.; Haines, A.; Ebi, K.L.; Li, S.; Guo, Y. Wildfires, Global Climate Change, and Human Health. N. Engl. J. Med. 2020, 383, 2173–2181. [Google Scholar] [CrossRef]
- Congressional Research Service. Wildfire Statistics. 2021. Available online: https://sgp.fas.org/crs/misc/IF10244.pdf (accessed on 5 September 2021).
- Dennison, P.E.; Brewer, S.C.; Arnold, J.D.; Moritz, M.A. Large wildfire trends in the western United States, 1984–2011. Geophysc Res. Lett. 2014, 41, 2928–2933. [Google Scholar] [CrossRef]
- Li, S.; Banerjee, T. Spatial and temporal pattern of wildfires in California from 2000 to 2019. Sci. Rep. 2021, 11, 8779. [Google Scholar] [CrossRef] [PubMed]
- National Interagency Fire Center. National Report of Wildland Fires and Acres Burned by State. 2020. Available online: https://www.predictiveservices.nifc.gov/intelligence/2020_statssumm/fires_acres20.pdf (accessed on 5 September 2021).
- CAL FIRE. Top 20 Largest California Wildfires. 2021. Available online: https://www.fire.ca.gov/media/4jandlhh/top20_acres.pdf (accessed on 5 September 2021).
- CAL FIRE. Top 20 Most Destructive California Wildfires. 2021. Available online: https://www.fire.ca.gov/media/t1rdhizr/top20_destruction.pdf (accessed on 5 September 2021).
- National Interagency Coordination Center; N.I.F.C.Predictive Services. National Significant Wildland Fire Potential Outlook. 2021. Available online: https://www.predictiveservices.nifc.gov/outlooks/monthly_seasonal_outlook.pdf (accessed on 5 September 2021).
- Huang, Y.; Jin, Y.; Schwartz, M.W.; Thorne, J.H. Intensified burn severity in California’s northern coastal mountains by drier climatic condition. Environ. Res. Lett. 2020, 15, 104033. [Google Scholar] [CrossRef]
- Rossiello, M.R.; Szema, A. Health Effects of Climate Change-induced Wildfires and Heatwaves. Cureus 2019, 11, e4771. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Balmes, J.R. The Changing Nature of Wildfires: Impacts on the Health of the Public. Clin. Chest Med. 2020, 41, 771–776. [Google Scholar] [CrossRef]
- Reid, C.E.; Maestas, M.M. Wildfire smoke exposure under climate change: Impact on respiratory health of affected communities. Curr. Opin. Pulm. Med. 2019, 25, 179–187. [Google Scholar] [CrossRef] [PubMed]
- Black, C.; Tesfaigzi, Y.; Bassein, J.A.; Miller, L.A. Wildfire smoke exposure and human health: Significant gaps in research for a growing public health issue. Environ. Toxicol. Pharmacol. 2017, 55, 186–195. [Google Scholar] [CrossRef] [PubMed]
- Walter, C.M.; Schnieder-Futschik, E.K.; Knibbs, L.D.; Irving, L.B. Health impacts of bushfire smoke exposure in Australia. Respirology 2020, 25, 495–501. [Google Scholar] [CrossRef]
- Chen, H.; Samet, J.M.; Bromberg, P.A.; Tong, H. Cardiovascular health impacts of wildfire smoke exposure. Part. Fibre Toxicol. 2021, 18, 2. [Google Scholar] [CrossRef]
- Amjad, S.; Chojecki, D.; Osornio-Vargas, A.; Ospina, M.B. Wildfire exposure during pregnancy and the risk of adverse birth outcomes: A systematic review. Environ. Int. 2021, 156, 106644. [Google Scholar] [CrossRef]
- Reid, C.E.; Brauer, M.; Johnston, F.H.; Jerrett, M.; Balmes, J.R.; Elliott, C.T. Critical Review of Health Impacts of Wildfire Smoke Exposure. Environ. Health Perspect. 2016, 124, 1334–1343. [Google Scholar] [CrossRef] [Green Version]
- Maxmen, A. California biologists are using wildfires to assess health risks of smoke. Nature 2019, 575, 15–16. [Google Scholar] [CrossRef] [PubMed]
- Burke, M.; Driscoll, A.; Heft-Neal, S.; Xue, J.; Burney, J.; Wara, M. The changing risk and burden of wildfire in the United States. Proc. Natl. Acad. Sci. USA 2021, 118, e2011048118. [Google Scholar] [CrossRef] [PubMed]
- Cascio, W.E. Wildland fire smoke and human health. Sci. Total Environ. 2018, 624, 586–595. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.C.; Pereira, G.; Uhl, S.A.; Bravo, M.A.; Bell, M.L. A systematic review of the physical health impacts from non-occupational exposure to wildfire smoke. Environ. Res. 2015, 136, 120–132. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Adetona, O.; Reinhardt, T.E.; Domitrovich, J.; Broyles, G.; Adetona, A.M.; Kleinman, M.T.; Ottmar, R.; Naeher, L.P. Review of the health effects of wildland fire smoke on wildland firefighters and the public. Inhal Toxicol. 2016, 28, 95–139. [Google Scholar] [CrossRef] [PubMed]
- Holm, S.M.; Miller, M.D.; Balmes, J.R. Health effects of wildfire smoke in children and public health tools: A narrative review. J. Expo. Sci. Environ. Epidemiol. 2021, 31, 1–20. [Google Scholar] [CrossRef] [PubMed]
- Navarro, K. Working in Smoke: Wildfire Impacts on the Health of Firefighters and Outdoor Workers and Mitigation Strategies. Clin. Chest Med. 2020, 41, 763–769. [Google Scholar] [CrossRef] [PubMed]
- Herndon, D.N.; Traber, D.L.; Niehaus, G.D.; Linares, H.A.; Traber, L.D. The pathophysiology of smoke inhalation injury in sheep model. J. Trauma 1984, 24, 1044–1051. [Google Scholar] [CrossRef]
- Cox, R.A.; Burke, A.S.; Soejima, K.; Murakami, J.; Katahira, L.D.; Traber, D.N.; Herndon, F.C.; Schmalstieg, D.L.T.; Hawkins, H.K. Airway obstruction in sheep with burn and smoke inhalation injuries. Am. J. Respir. Cell Mol. Biol. 2003, 29, 295–302. [Google Scholar] [CrossRef]
- Herndon, D.N.; Traber, L.D.; Linares, H.; Flynn, J.D.; Niehaus, G.; Kramer, G.; Traber, D.L. Etiology of the pulmonary pathophysiology associated with inhalation injury. Resuscitation 1986, 14, 43–59. [Google Scholar] [CrossRef]
- Hubbard, G.B.; Langlinais, P.C.; Shimanzu, T.; Okerberg, C.V.; Mason, A.D.; Pruitt, B.A. The morphology of smoke inhalation injury in sheep. J. Trauma 1991, 31, 1477–1486. [Google Scholar] [CrossRef] [Green Version]
- Soejima, K.; McGuire, R.; Snyder, N.; Uchida, T.; Szabó, C.; Salzman, A.; Traber, L.D.; Trader, D.L. The effect of inducible nitric oxide synthase (iNOS) inhibition on smoke inhalation injury in sheep. Shock 2000, 13, 261–266. [Google Scholar] [CrossRef]
- Lalonde, C.; Demling, R.; Brain, J.; Blanchard, J. Smoke inhalation injury in sheep is caused by the particle phase, not the gas phase. J. Apply Physiol. 1985, 77, 15–22. [Google Scholar] [CrossRef] [PubMed]
- Abdi, S.; Evans, M.J.; Cox, R.A.; Lubbesmeyer, H.; Herndon, D.N.; Traber, D.L. Inhalation injury to tracheal epithelium in an ovine model of cotton smoke exposure: Early phase (30 minutes). Am. Rev. Respir. Dis. 1990, 142, 1436–1439. [Google Scholar] [CrossRef]
- Jacob, S.; Kraft, R.; Zhu, Y.; Jacob, R.K.; Herndon, D.N.; Traber, D.L.; Hawkins, H.K.; Cox, R.A. Acute secretory cell toxicity and epithelial exfoliation after smoke inhalation injury in sheep: An electron and light microscopic study. Toxicol. Mech. Methods 2010, 20, 504–509. [Google Scholar] [CrossRef]
- Shimoda, K.; Nakazawa, H.; Traber, M.G.; Traber, D.L.; Nozaki, M. Plasma and tissue vitamin E depletion in sheep with burn and smoke inhalation injury. Burns 2008, 34, 1137–1141. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Maybauer, D.M.; Maybauer, M.O.; Traber, L.D.; Westphal, M.; Nakano, Y.Y.; Enkhbaatar, P.; Morita, N.; Herndon, D.N.; Traber, D.L. Effects of severe smoke inhalation injury and septic shock on global hemodynamics and microvascular blood flow in sheep. Shock 2006, 26, 489–495. [Google Scholar] [CrossRef] [PubMed]
- Barrow, R.E.; Wang, C.Z.; Cox, R.A.; Evans, M.J. Cellular sequence of tracheal repair in sheep after smoke inhalation injury. Lung 1992, 170, 331–338. [Google Scholar] [CrossRef]
- Yamamato, Y.; Enkhbaatar, P.; Sakurai, H.; Rehbuerg, S.; Asmussen, S.; Ito, H.; Sousse, L.E.; Cox, R.A.; Deyo, D.J.; Traber, L.D.; et al. Development of a long-term ovine model of cutaneous burn and smoke inhalation injury and the effects of early excision and skin autografting. Burns 2012, 38, 908–916. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Enkhbaatar, P.; Esechie, A.; Wang, J.; Cox, R.A.; Nakano, Y.; Hamahata, A.; Lange, M.; Traber, L.D.; Prough, D.S.; Herndon, D.N.; et al. Combined anticoagulants ameliorate acute lung injury in sheep after burn and smoke inhalation. Clin. Sci. 2008, 114, 321–329. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Enkhbaatar, P.; Cox, R.A.; Traber, L.D.; Westphal, M.; Aimalohi, E.; Morita, N.; Prough, D.S.; Herndon, D.N.; Traber, D.L. Aerosolized anticoagulants ameliorate acute lung injury in sheep after exposure to burn and smoke inhalation. Crit. Care Med. 2007, 2007, 12. [Google Scholar] [CrossRef]
- Enkhbaatar, P.; Connelly, R.; Wang, J.; Nakano, Y.; Lange, M.; Hamahata, A.; Horvath, E.; Szabo, C.; Jarch, S.; Hölscher, P.; et al. Inhibition of neuronal nitric oxide synthase in ovine model of acute lung injury. Crit. Care Med. 2009, 37, 208–214. [Google Scholar] [CrossRef]
- Westphal, M.; Enkhbaatar, P.; Schmalstieg, F.C.; Kulp, G.A.; Traber, L.D.; Morita, N.; Cox, R.A.; Hawkins, H.K.; Westphal-Varghese, B.B.; Rubloff, H.E.; et al. Neuronal nitric oxide synthase inhibition attenuates cardiopulmonary dysfunctions after combined burn and smoke inhalation injury in sheep. Crit. Care Med. 2008, 36, 1196–1204. [Google Scholar] [CrossRef] [PubMed]
- Morita, N.; Traber, M.G.; Enkhbaatar, P.; Westphal, M.; Murakami, K.; Leonard, S.W.; Cox, R.A.; Hawkins, H.A.; Herndon, D.; Traber, L.D.; et al. Aerosolized alpha-tocopherol ameliorates acute lung injury following combined burn and smoke inhalation injury in sheep. Shock 2006, 25, 277–282. [Google Scholar] [CrossRef] [Green Version]
- Morita, N.; Shimoda, K.; Traber, M.G.; Westphal, M.; Enkhbaater, P.; Murakami, K.; Leonard, S.W.; Traber, L.D.; Traber, D.L. Vitamin E attenuates acute lung injury in sheep with burn and smoke inhalation injury. Redox Rep. 2006, 11, 61–70. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Palmieri, T.L.; Enkhbaatar, P.; Bayliss, R.; Traber, L.D.; Cox, R.A.; Hawkins, H.K.; Herndon, D.N.; Greenhalgh, D.G.; Traber, D.L. Continuous nebulized albuterol attenuates acute lung injury in an ovine model of combined burn and smoke inhalation. Crit. Care Med. 2006, 34, 1719–1724. [Google Scholar] [CrossRef]
- Maybauer, M.O.; Maybauer, D.M.; Fraser, J.F.; Traber, L.D.; Westphal, M.; Enkhbaatar, P.; Cox, R.A.; Huda, R.; Hawkinds, H.K.; Morita, N.; et al. Recombinant human activated protein C improves pulmonary function in ovine acute lung injury resulting from smoke inhalation and sepsis. Crit. Care Med. 2006, 34, 2432–2438. [Google Scholar] [CrossRef] [PubMed]
- Murakami, K.; McGuire, R.; Cox, R.A.; Jodoin, J.M.; Schmalstieg, F.C.; Traber, L.D.; Hawkins, H.K.; Herndon, D.N.; Traber, D.L. Recombinant antithrombin attenuates pulmonary inflammation following smoke inhalation and pneumonia in sheep. Crit. Care Med. 2003, 31, 577–583. [Google Scholar] [CrossRef]
- Murakami, K.; Enkhbaatar, P.; Shimoda, K.; Mizutani, A.; Cox, R.A.; Schmalstieg, F.C.; Jodoin, J.M.; Hawkins, H.K.; Traber, L.D.; Traber, D.L. High-dose heparin fails to improve acute lung injury following smoke inhalation in sheep. Clin. Sci. 2003, 104, 349–356. [Google Scholar] [CrossRef]
- Jacob, S.; Deyo, D.J.; Cox, R.A.; Traber, D.L.; Herndon, D.N.; Hawkins, H.K. Mechanisms of toxic smoke inhalation and burn injury: Role of neutral endopeptidase and vascular leakage in mice. Toxicol. Mech. Methods 2009, 19, 191–196. [Google Scholar] [CrossRef] [PubMed]
- Jacob, S.; Deyo, D.J.; Cox, R.A.; Jacob, R.K.; Herndon, D.N.; Traber, D.L.; Hawkins, H.K. Substance P antagonist CP-96345 blocks lung vascular leakage and inflammation more effectively than its stereoisomer CP-96344 in a mouse model of smoke inhalation and burn injury. Toxicol. Mech. Methods 2010, 20, 197–203. [Google Scholar] [CrossRef] [Green Version]
- Li, T.; Cai, S.; Zeng, Z.; Zhang, J.; Gao, Y.; Wang, X.; Chen, Z. Protective effect of polydatin against burn-induced lung injury in rats. Respir. Care 2014, 59, 1412–1421. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jacob, S.; Deyo, D.J.; Cox, R.A.; Traber, D.L.; Hawkins, H.K. Assessment of lung inflammation in a mouse model of smoke inhalation and burn injury: Strain-specific differences. Toxicol. Mech. Methods 2008, 18, 551–559. [Google Scholar] [CrossRef] [PubMed]
- Mizutani, A.; Enkhbaatar, P.; Esechie, A.; Trabder, L.D.; Cox, R.A.; Hawkins, H.K.; Deyo, D.J.; Murakami, K.; Noguchi, T.; Traber, D.L. Pulmonary changes in a mouse model of combined burn and smoke inhalation-induced injury. J. Appl. Physiol. 2008, 105, 678–684. [Google Scholar] [CrossRef] [PubMed]
- Eid, B.; Beggs, D.; Mansell, P. The Impact of Bushfire Smoke on Cattle—A Review. Animals 2021, 11, 848. [Google Scholar] [CrossRef]
- Sharpe, A.N.; Gunther-Harrington, C.T.; Epstein, S.E.; Li, R.H.L.; Stern, J.A. Cats with thermal burn injuries from California wildfires show echocardiographic evidence of myocardial thickening and intracardiac thrombi. Sci. Rep. 2020, 10, 2648. [Google Scholar] [CrossRef] [PubMed]
- Willson, B.E.; Gee, N.A.; Willits, N.H.; Li, L.; Zhang, Q.; Pinkerton, K.E.; Lasley, B.L. Effects of the 2018 Camp Fire on birth outcomes in non-human primates: Case-control study. Repro. Toxicol. 2021, 206, 128–135. [Google Scholar] [CrossRef]
- Ledbetter, K. Wildfire damage to cattle may be more than the eye can see. In AgriLife Today; Texas A&M University: Amarillo, TX, USA, 2011. [Google Scholar]
- Ranches, J. Animal Exposure to Wildfire Smoke. 2020. Available online: https://extension.oregonstate.edu/animals-livestock/beef/animal-exposure-wildfire-smoke (accessed on 5 September 2021).
- Texas A&M AgriLife Extension, D.E.N. Managing and Caring for Horses Affected by Fires. 2007. Available online: https://texashelp.tamu.edu/wp-content/uploads/2016/02/managing-caring-for-horses-burns.pdf (accessed on 5 September 2021).
- Smith, D.W. Protecting Farms & Ranches from Wildfires. 2016. Available online: https://texashelp.tamu.edu/wp-content/uploads/2016/02/ProtectingFarmsRanchesfromWildfires.pdf (accessed on 5 September 2021).
- Texas A&M AgriLife Extension. Protection of Rangeland and Pastures from Wildfire. 2017. Available online: https://texashelp.tamu.edu/wp-content/uploads/2017/03/protection-rangeland-and-pastures-from-wildfire.pdf (accessed on 5 September 2021).
- Madigan, J.; Wilson, D.; Stull, C. Wildfire, Smoke and Livestock. 2008. Available online: http://cecentralsierra.ucanr.edu/files/220420.pdf (accessed on 5 September 2021).
- University of California Davis. Guidelines for Horses Exposed to Wildfire Smoke. 2017. Available online: https://www.vetmed.ucdavis.edu/news/guidelines-horses-exposed-wildfire-smoke (accessed on 5 September 2021).
- Oregon State University Extension Service. Fire. 2021. Available online: https://extension.oregonstate.edu/forests/fire (accessed on 5 September 2021).
- Environmental Protection Agency (EPA). Wildfire Smoke Factsheet: Protect Your Large Animals and Livestock from Wildfire Smoke. 2021. Available online: https://www.airnow.gov/sites/default/files/2021-06/protect-your-large-animals-and-livestock-from-wildfire-smoke.pdf (accessed on 5 September 2021).
- American Veterinary Medical Association (AVMA). Wildfire Smoke and Animals. 2021. Available online: https://www.avma.org/resources/pet-owners/emergencycare/wildfire-smoke-and-animals (accessed on 5 September 2021).
- Fitzgerald, K.T.; Flood, A.A. Smoke Inhalation. Clin. Tech. Small Anim. Pract. 2006, 21, 205–214. [Google Scholar] [CrossRef]
- Saxon, W.D.; Kirby, R. Treatment of acute burn injury and smoke inhalation. In Kirk's Veterinary Therapy; Saunders: Philadelphia, PA, USA, 1992. [Google Scholar]
- Vaughn, L.; Beckel, N. Severe burn injury, burn shock, and smokeinhalation injury in small animals. Part 1: Burnclassification and pathophysiology. J. Vet. Emerg. Crit. Care 2012, 22, 179–186. [Google Scholar] [CrossRef]
- Vaughn, L.; Beckel, N.; Walters, P. Severe burn injury, burn shock, and smoke inhalation injury in small animals. Part 2: Diagnosis, therapy, complications, and prognosis. J. Vet. Emerg. Crit. Care 2012, 22, 187–200. [Google Scholar] [CrossRef]
- Rethorst, D.N.; Spare, R.K.; Kellenberger, J.L. Wildfire Response in Range Cattle. Vet. Clin. Food Anim. 2018, 34, 281–288. [Google Scholar] [CrossRef]
- Texas A&M Agrilife Extension. Wildfires Leave behind Hungry Cattle and Downed Fences. 2011. Available online: https://texashelp.tamu.edu/wp-content/uploads/2016/02/Wildfires-leave-behind-hungry-cattle-and-downed-fences.pdf (accessed on 5 September 2021).
- Texas A&M Agrilife Extension. Wildfires Leave More than Ashes Behind. 2011. Available online: https://texashelp.tamu.edu/wp-content/uploads/2016/02/Wildfires-leave-more-than-ashes-behind.pdf (accessed on 5 September 2021).
- United States Department of Agriculture (USDA); F.S.A. USDA California Farm Service Agency Offers Wildfire Recovery Assistance. 2021. Available online: https://www.fsa.usda.gov/state-offices/California/news-releases/2020/usda-california-farm-service-agency-offers-wildfire-recovery-assistance (accessed on 5 September 2021).
- Qualtrics; Version May 2021, Copyright 2021; Qualtrics: Provo, UT, USA, 2005.
- Boslaugh, S. Encyclopedia of Epidemiology; SAGE Publications, Inc.: Thousand Oaks, CA, USA, 2008. [Google Scholar]
- RStudio Team. RStudio: Integrated Development for R; RStudio, Inc.: Boston, MA, USA, 2015. [Google Scholar]
- Hanzlicek, G.A.; Renter, D.R.; White, B.J.; Wagner, B.A.; Dargatz, D.A.; Sanderson, M.W.; Scott, H.M.; Larson, R.E. Management practices associated with the rate of respiratory tract disease among preweaned beef calves in cow-calf operations in the United States. Sci. Rep. 2013, 242, 1271–1278. [Google Scholar] [CrossRef] [PubMed]
- Smith, D.R. Risk factors for bovine respiratory disease in beef cattle. Anim. Health Res. Rev. 2020, 21, 149–152. [Google Scholar] [CrossRef] [PubMed]
- Williams, K.M.; Franzi, L.M.; Last, J.A. Cell-specific oxidative stress and cytotoxicity after wildfire coarse particulate matter instillation into mouse lung. Toxicol. Appl. Pharmacol. 2013, 266, 48–55. [Google Scholar] [CrossRef] [Green Version]
- Malley, C.S.; Kuylenstierna, J.C.I.; Vallack, H.W.; Henze, D.K.; Blencowe, H.; Ashmore, M.R. Preterm birth associated with material fine particulate matter exposure: A global, regional and national assessment. Envion. Int. 2017, 101, 173–182. [Google Scholar] [CrossRef] [PubMed]
- Field, T.; Diego, M.; Hernandez-Reif, M. Prenatal depression effects of the fetus and newborn: A review. Infant Behav. Dev. 2006, 29, 445–455. [Google Scholar] [CrossRef]
- United States Department of Agriculture (USDA); National Agricultural Statistics Service (NASS). Census of Agriculture. 2017. Available online: www.nass.usda.gov/AgCensus (accessed on 5 September 2021).
- Register, F. Supplemental Agricultural Disaster Assistance Programs, Payment Limitations, and Payment Eligibility. Final Rule; 2014. Available online: https://www.federalregister.gov/documents/2018/10/02/2018-21257/supplemental-agricultural-disaster-assistance-programs-payment-limitation-and-payment-eligibility (accessed on 5 September 2021).
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
O’Hara, K.C.; Ranches, J.; Roche, L.M.; Schohr, T.K.; Busch, R.C.; Maier, G.U. Impacts from Wildfires on Livestock Health and Production: Producer Perspectives. Animals 2021, 11, 3230. https://doi.org/10.3390/ani11113230
O’Hara KC, Ranches J, Roche LM, Schohr TK, Busch RC, Maier GU. Impacts from Wildfires on Livestock Health and Production: Producer Perspectives. Animals. 2021; 11(11):3230. https://doi.org/10.3390/ani11113230
Chicago/Turabian StyleO’Hara, Kathleen C., Juliana Ranches, Leslie M. Roche, Tracy Kay Schohr, Roselle C. Busch, and Gabriele U. Maier. 2021. "Impacts from Wildfires on Livestock Health and Production: Producer Perspectives" Animals 11, no. 11: 3230. https://doi.org/10.3390/ani11113230
APA StyleO’Hara, K. C., Ranches, J., Roche, L. M., Schohr, T. K., Busch, R. C., & Maier, G. U. (2021). Impacts from Wildfires on Livestock Health and Production: Producer Perspectives. Animals, 11(11), 3230. https://doi.org/10.3390/ani11113230






