4. Discussion
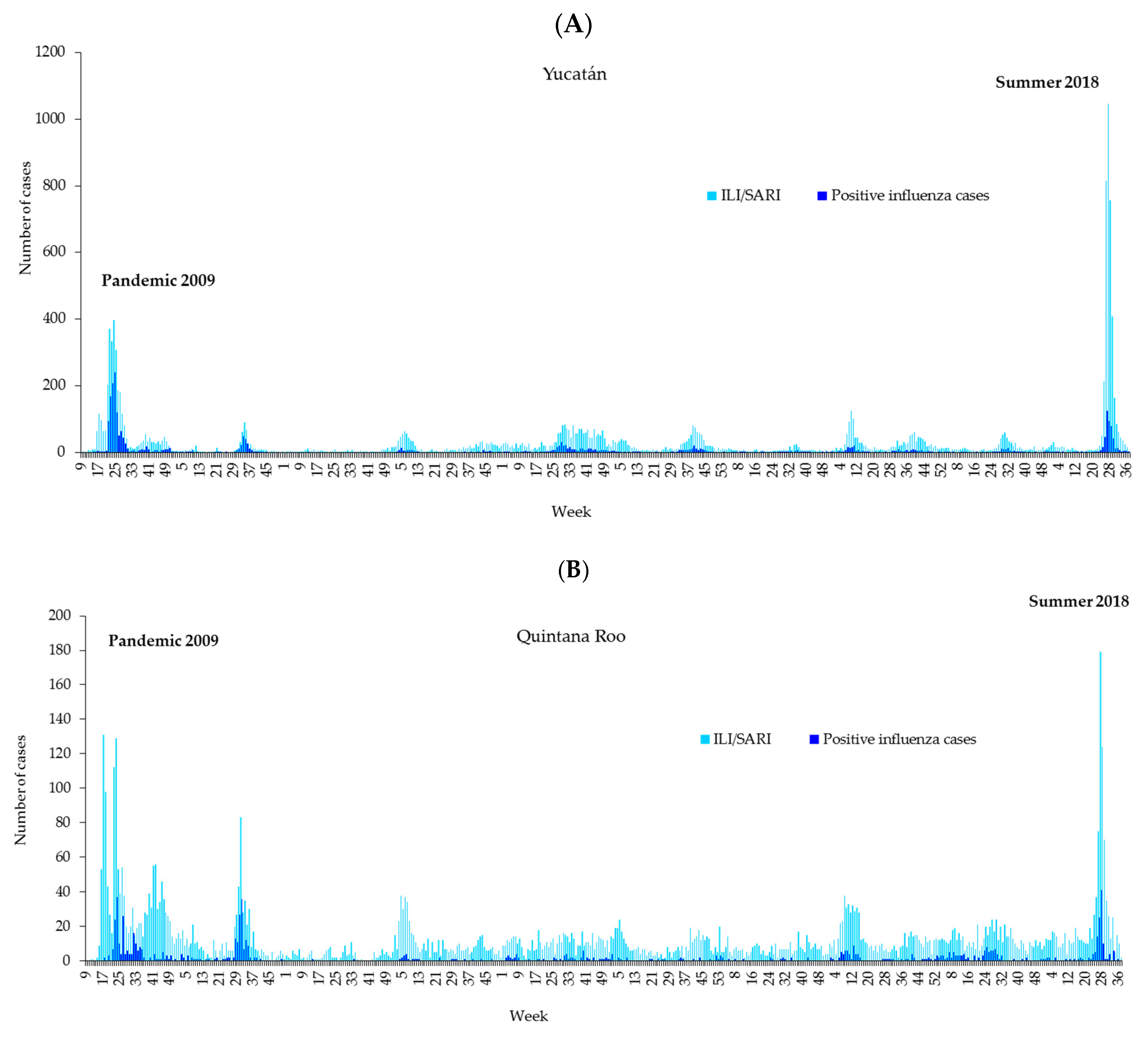
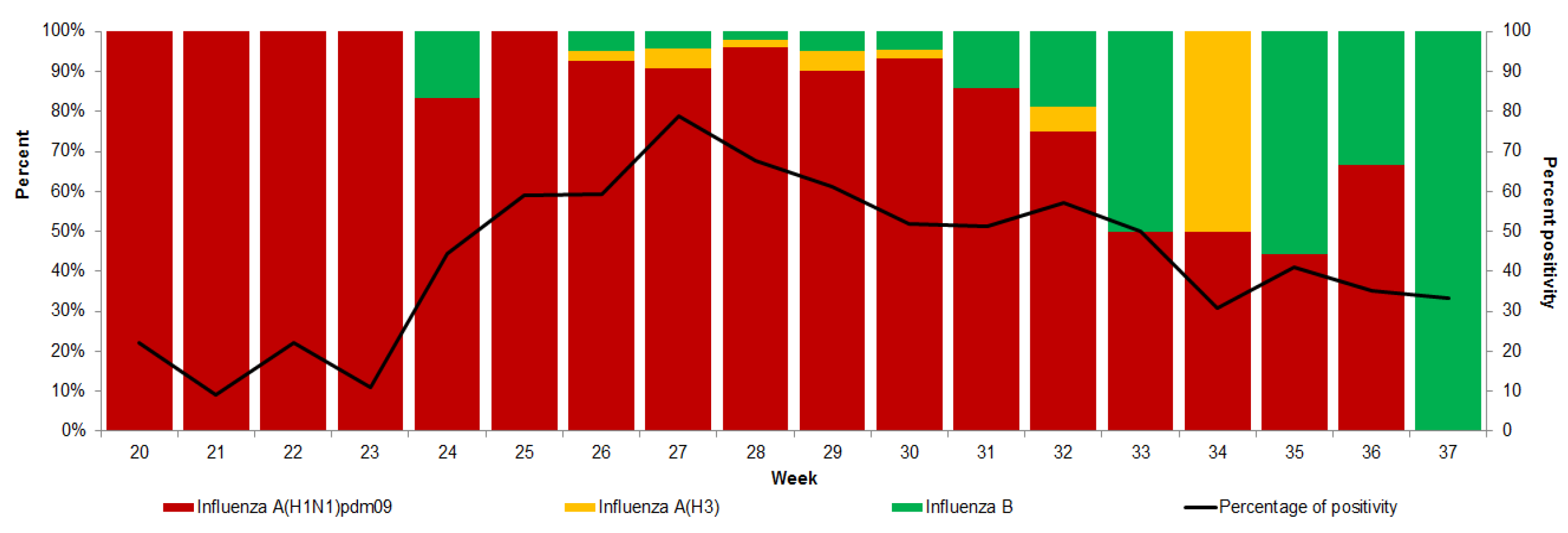
We characterized the epidemiology of a recurrent wave of influenza A(H1N1)pdm09 transmission on the Yucatan Peninsula spanning weeks 21 to 37 of 2018, on the basis of the ILI/SARI and laboratory-confirmed infections. We compared the impact, severity and age patterns. We used individual-level patient information collected through a prospective influenza surveillance system put into place especially for the 2009 pandemic by the largest Mexican Social Security medical system. We also documented a significant increase in the proportion of influenza A/H1N1 and ILI/SARI cases relative to the 2009 pandemic.
Previously, Australia experienced unusually high levels of influenza activity in 2017 because of several factors potentially contributing to the lower vaccine effectiveness, including the genetic diversity of the dominant influenza A(H3N2) strains currently circulating, the greater proportion of elderly affected individuals, who are known to have reduced responses to vaccines, and ongoing problems with identifying suitable influenza A(H3N2) vaccine candidates [
8]. Intense interseasonal influenza outbreaks (in the Northern Hemisphere summer) have been documented in other countries and years [
9,
10,
11] providing a clearer understanding of the epidemiology and burden of interseasonal influenza and trends over time. In this sense, Li et al. showed that the influenza virus had clear seasonal epidemics in winter months in most temperate sites, but the timing of epidemics was more variable and less seasonal with decreasing distance from the equator. The influenza virus had clear seasonal epidemics in both temperate and tropical regions but sometimes started in the late summer months in the tropics of each hemisphere; these patterns became less pronounced closer to the equator, with the emergence of summer epidemics in some sites [
12].
Specifically, in this study, an increase was observed in ILI/SARI cases in the Yucatan Peninsula; it was due to influenza A(H1N1)pdm09 in both periods. Additionally, through sentinel epidemiological surveillance, the Ministry of Health of Mexico revealed an increase in cases of influenza in the Yucatan Peninsula, with a predominance of influenza A(H1N1)pdm09 circulation in 80% of the cases, where 59.9% of the cases were concentrated in Yucatan and Quintana Roo [
2]. The Institute of Epidemiological Diagnosis and Reference (InDRE) has not identified mutations related to antigenic changes or changes in the virulence or pathogenicity of the influenza virus. No viral resistance to oseltamivir was identified in Mexico in this summer [
2]. Similarly, in the IMSS, a substantial increase in the number of SARI hospitalizations during the period December 2011 to March 2012 and an older age distribution of laboratory-confirmed A(H1N1)pdm09 influenza hospitalizations and deaths relative to 2009 A(H1N1)pdm09 pandemic patterns were documented [
13]. Additionally, the number of influenza A(H1N1)pdm09-related hospitalizations and deaths during the period of October 2013–January 2014 and the proportionate shift of severe disease to middle-aged adults relative to the preceding A(H1N1)pdm09 2011–2012 epidemic in the IMSS were reported [
14]. Notably, in 2018, 66.5% of confirmed cases occurred in patients between 25 and 64 years of age, whereas in 2009, 61.8% were in patients between 5 and 24 years of age. At the end of 2010, 28.5 million doses were administered free of charge in Mexico [
15]. After the 2009 influenza pandemic, programmatic groups (based on targets) were established in Mexico for influenza vaccination (so vaccination is not universal). Influenza vaccination in Mexico is based on the assumption that influenza peaks in winter. The target group included older adults and people from 19 to 59 years of age with risk factors; therefore, one hypothesis for the change in age observed in 2018 is that this target population received the vaccination. People who had received a seasonal influenza vaccine in the previous year had a reduced risk of influenza A(H1N1)pdm09 infection. Between October 2018 and March 2019, 10,902,605 doses of influenza vaccine were scheduled for the population insured by the IMSS; 160,090 doses were for Quintana Roo and 217,931 for Yucatan. The increase in cases during 2018 occurred prior to this vaccination event, so the hypotheses of this lag can be seen in the risk estimators for vaccination and the fatality rate in older adults. The discrepancies in the estimated risk of vaccination between the two periods are hypothesized to be that in 2009, vaccination was universal and in the intensive phase due to the pandemic year. In 2018, however, it was in target groups, and contradictorily, the point estimate was a modest risk; this can be explained by the vaccination history of the 2017–2018 season. Finally, in Mexico, the circulation of influenza A(H1N1)pdm09 coincided with a higher incidence of severe pneumonia, predominantly in young adults, in March and April 2009 [
1]. The circulation of influenza viruses in Mexico after 2009 was biennial, in the winter [
16]. What was observed in the interseasonal period of 2018 in the Yucatan Peninsula highlights that it was due to a sudden activity by influenza A(H1N1)pdm09, which has been characterized by abrupt increases each winter. Additionally, the interim influenza vaccine effectiveness (VE) estimates from Australia documented that the adjusted VE was low overall at 33% (95CI% 17 to 46) and 50% (95% CI: 8 to 74) for influenza A(H1N1)pdm09 [
17]. In 2009, the protective factor of mass vaccination against influenza was observed throughout the year. However, this was not the case in 2018, when vaccination was targeted to certain programmatic groups.
Previously, it was documented that elderly participants also had a higher risk of hospital admission, and children aged less than 5 years were at a lower risk of death, probably because the children aged less than 5 years were at a higher risk of developing pneumonia [
18].
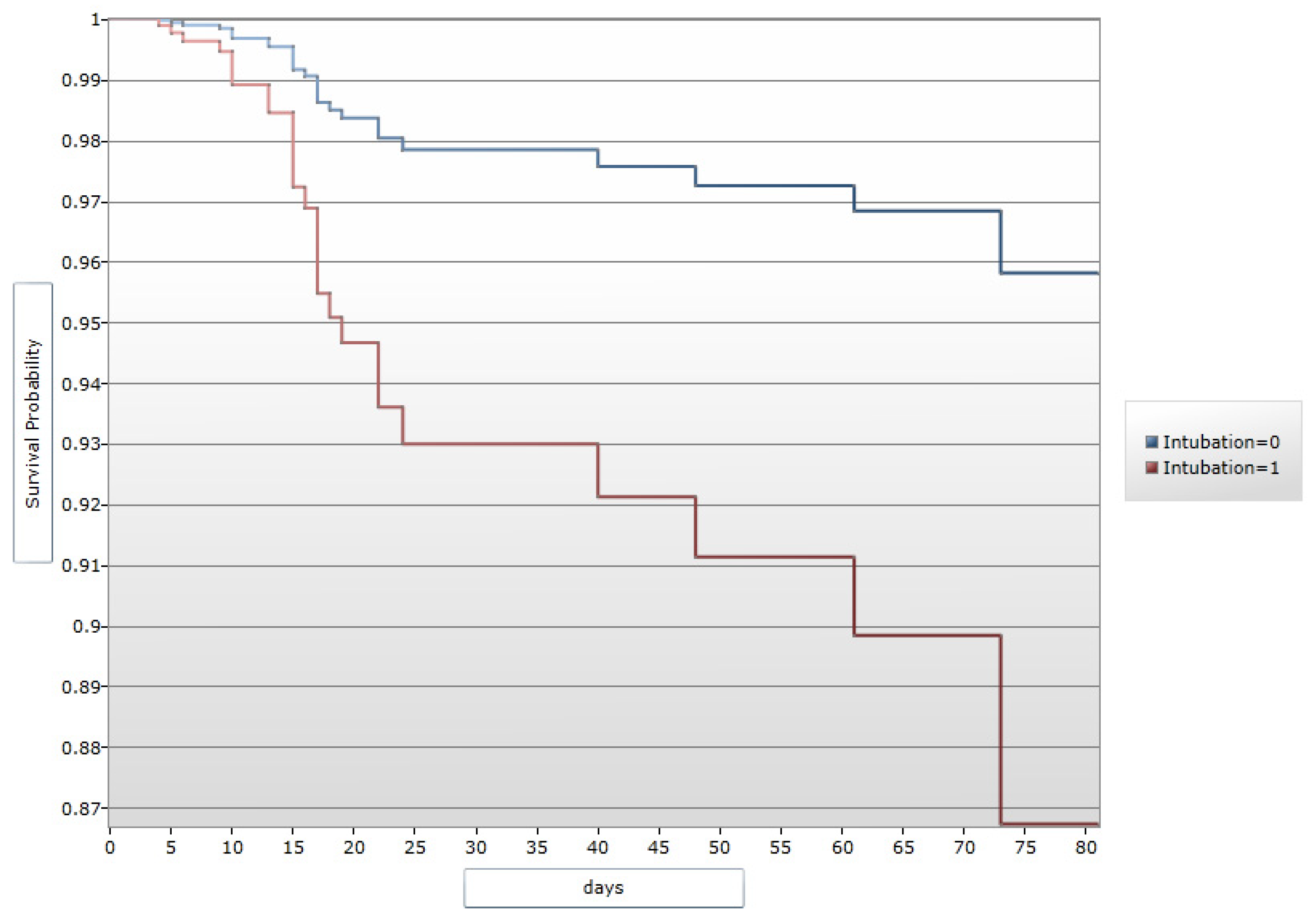
In terms of clinical manifestations, dyspnea, tachypnea, cyanosis and being confined to bed were prognostic factors for hospital admission and death during influenza A(H1N1)pdm09 virus infection in Mexico in 2009 [
19]; this was consistent with the findings of this study in 2009 and 2018 in a specific area of Mexico because the source of information is the same, although adjustments in the epidemiological surveillance system (diagnostic algorithms) have been made.
Asthma and obesity were identified as risk factors associated with the presentation of influenza in this study. Coleman BL et al. [
20] also identified asthma as a risk factor for hospitalization, as well as obesity, especially in severe situations [
21]. However, a meta-analysis of 59 studies revealed that obesity was a risk factor for death [
18]. In the present study, obesity presented a minimal risk of death in both periods. It remains unclear whether obesity in itself is a risk factor or whether it reflects the presence of other comorbidities such as cardiovascular diseases and diabetes mellitus; in our risk model, obesity alone resulted in an HR of 1.55, with the limitation of analyzing more comorbidities simultaneously. This highlights the need to strengthen preventive measures in these groups, as well as adherence to asthma treatment. One risk worth highlighting was travel history in 2009, a year marked by the influenza pandemic, where travel history was given priority; this situation was not reflected in the estimated risks for 2018.
Although the phenomenon that occurred has been reported previously, this behavior is unique given that it is the first time that an abrupt increase of this magnitude has been observed in the months prior to the winter season since 2009 in Mexico. The influenza cases presented seasonality, with a single peak between the months of November and March of each year [
3]. However, the Yucatan Peninsula (states of Campeche, Quintana Roo, and Yucatan) is one of the primary entry points for influenza variants in Mexico because of its large influx of tourists and commercial activities in the areas surrounding Merida and Cancun; population movement for recreational purposes in the summer or the behavior of the Southern Hemisphere influenza season could affect individuals traveling to the Peninsula. One hypothesis to consider is the climate in the region, with cold fronts generating a “typical temperate winter” [
22], and the effects of the geographical location of the Yucatan Peninsula are determined mainly by the Caribbean Sea, resulting in a dry and warm winter and a summer with bimodal precipitation [
23]. In this sense, although lower temperature was associated with higher activity of both the influenza virus and respiratory syncytial virus, higher relative humidity was associated with higher influenza virus activity when the temperature was above the annual average [
12], and the geographical location of the Yucatan Peninsula is in the tropics, with high humidity; 85.5% of the state of Yucatan has a warm subhumid climate, while 99% of the state of Quintana Roo has a warm subhumid climate [
24]. Another hypothesis to consider corresponds to previous studies on the historical behavior of the influenza virus in the southeastern region of the country, so modifying influenza vaccination schemes according to the different patterns observed in the southeastern region and the Yucatan Peninsula has been recommended [
22], and one study reported that the seasonality of the virus is associated with the rainy season [
25]. These findings are particularly important for the inhabitants of the Yucatan Peninsula, but they should also be considered for high-risk groups traveling to the region. Similarly, vaccination should be considered for use in confined populations, such as daycare and nursing homes and hospitalized persons who do not have a contraindication to the vaccine, where some susceptible groups will be found (for example, people with diabetes, cancer, immunosuppression and renal failure). In general, influenza dynamics in the tropical Yucatan Peninsula differs from the rest of the country [
22]. Ayora has consistently insisted that assuming there is a single seasonal pattern for influenza in Mexico is a mistake, and therefore, determining whether there are different geographic patterns of virus and disease circulation is essential for developing and implementing control and prevention strategies [
26].
The IMSS is a tripartite Mexican health system covering approximately 40% of the Mexican population and comprises workers in the private sector and their families, relying on a network of 1099 primary healthcare units and 259 hospitals nationwide [
27].
In summary, our findings indicate a changing distribution of ILI/SARI and laboratory-confirmed A(H1N1)pdm09 influenza in the summer of 2018 relative to 2009 A/H1N1 pandemic patterns: the behavior of the epidemic curve, changes in age groups and the case fatality rate. This surprising behavior was documented in Australia during the summer of 2017. These authors reported that ILI activity was moderate during the interseasonal period from January to March of 2017; for example, on the Yucatan Peninsula, it presented a high percentage of positivity for several weeks.
The strengths of this study include the following: (1) it was a population-based study, (2) it had a regional focus, (3) it included confirmed cases, (4) it included a description of the percentage of positivity and (5) it included the time distribution of ILI/SARI cases during the different epidemic waves. Nevertheless, our findings need to be contextualized, considering several limitations. The analyzed data were derived from passive database systems, which collect information from patients who seek and receive medical care at IMSS healthcare facilities. Additionally, specific information about the administration of specific therapeutics before or during hospitalization was unavailable, and another limitation was not having the rates of vaccination by age group in 2017 and 2018 and comparing them with the information from the epidemiological surveillance system.