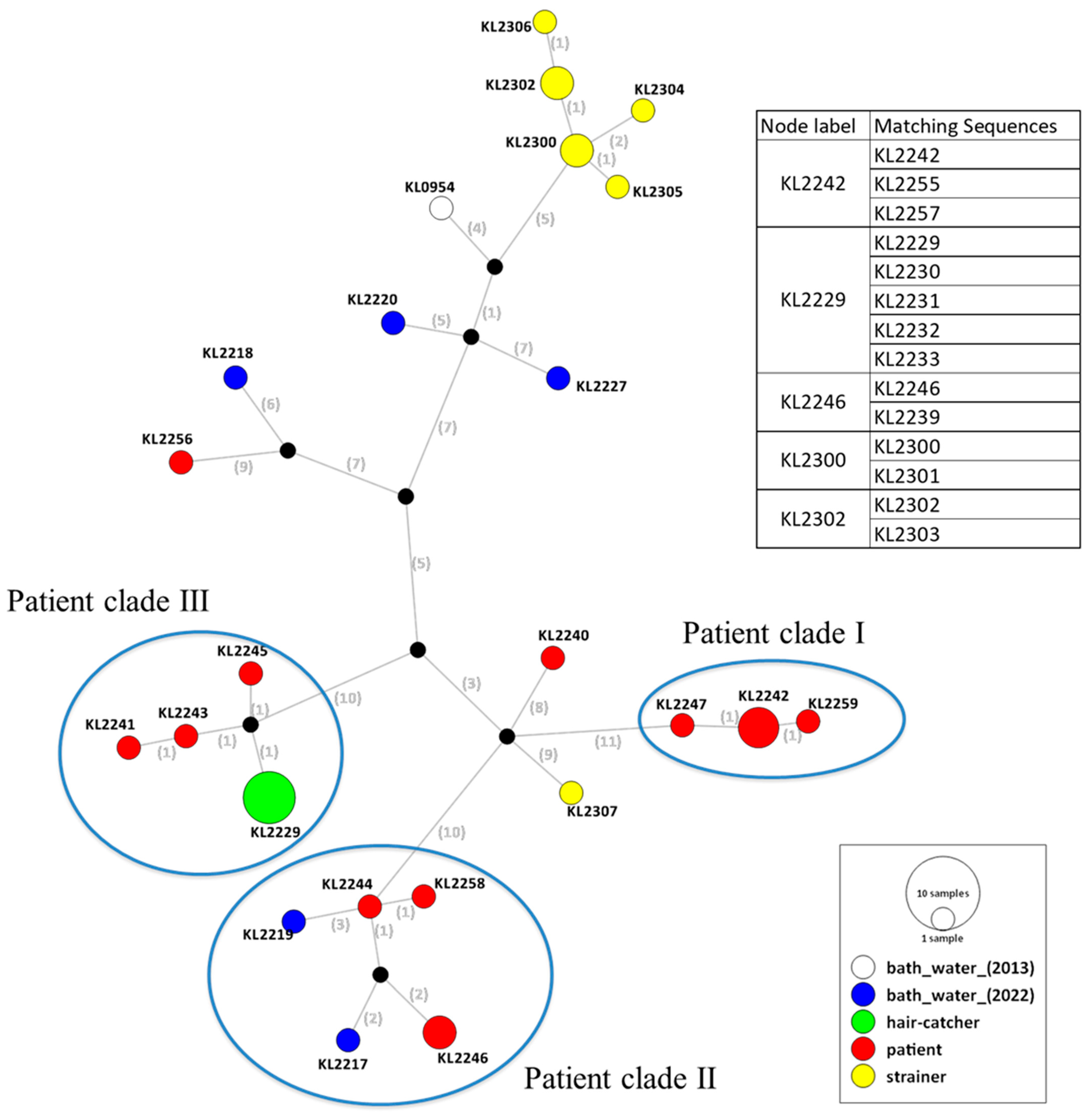
Investigation of a Legionella pneumophila Outbreak at a Bath Facility in Japan Using Whole-Genome Sequencing of Isolates from Clinical and Environmental Samples
Abstract
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Yu, V.L.; Stout, J.E. Community-Acquired Legionnaires Disease: Implications for Underdiagnosis and Laboratory Testing. Clin. Infect. Dis. 2008, 46, 1365–1367. [Google Scholar] [CrossRef] [PubMed]
- Yu, V.L.; Plouffe, J.F.; Pastoris, M.C.; Stout, J.E.; Schousboe, M.; Widmer, A.; Summersgill, J.; File, T.; Heath, C.M.; Paterson, D.L.; et al. Distribution of Legionella species and Serogroups Isolated by Culture in Patients with Sporadic Community-Acquired Legionellosis: An International Collaborative Survey. J. Infect. Dis. 2002, 186, 127–128. [Google Scholar] [CrossRef] [PubMed]
- Gaia, V.; Fry, N.K.; Afshar, B.; Lück, P.C.; Meugnier, H.; Etienne, J.; Peduzzi, R.; Harrison, T.G. Consensus sequence-based scheme for epidemiological typing of clinical and environmental isolates of Legionella pneumophila. J. Clin. Microbiol. 2005, 43, 2047–2052. [Google Scholar] [CrossRef] [PubMed]
- Ratzow, S.; Gaia, V.; Helbig, J.H.; Fry, N.K.; Lück, P.C. Addition of neuA, the gene encoding N-acylneuraminate cytidylyl transferase, increases the discriminatory ability of the consensus sequence-based scheme for typing Legionella pneumophila serogroup 1 strains. J. Clin. Microbiol. 2007, 45, 1965–1968. [Google Scholar] [CrossRef] [PubMed]
- National Institute of Infectious Diseases; Tuberculosis and Infectious Diseases Control Division; Ministry of Health, Labour and Welfare. Legionellosis, April 1999. Infect. Agents Surveill. Rep. 2000, 21, 186–187. Available online: http://idsc.nih.go.jp/iasr/21/247/tpc247.htmlExternalLink (accessed on 9 May 2016).
- Amemura-Maekawa, J.; Kura, F.; Chida, K.; Ohya, H.; Kanatani, J.I.; Isobe, J.; Tanaka, S.; Nakajima, H.; Hiratsuka, T.; Yoshino, S.; et al. Legionella pneumophila and Other Legionella species Isolated From Legionellosis Patients in Japan between 2008 and 2016. Appl. Environ. Microbiol. 2018, 84, e00721-18. [Google Scholar] [CrossRef] [PubMed]
- Kozak, N.A.; Benson, R.F.; Brown, E.; Alexander, N.T.; Taylor, T.H., Jr.; Shelton, B.G.; Fields, B.S. Distribution of Lag-1 Alleles and Sequence-Based Types Among Legionella pneumophila Serogroup 1 Clinical and Environmental Isolates in the United States. J. Clin. Microbiol. 2009, 47, 2525–2535. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Yoshimura, D.; Kajitani, R.; Gotoh, Y.; Katahira, K.; Okuno, M.; Ogura, Y.; Hayashi, T.; Itoh, T. Evaluation of SNP Calling Methods for Closely Related Bacterial Isolates and a Novel High-Accuracy Pipeline: BactSNP. Microb. Genom. 2019, 5, e000261. [Google Scholar] [CrossRef] [PubMed]
- Croucher, N.J.; Page, A.J.; Connor, T.R.; Delaney, A.J.; Keane, J.A.; Bentley, S.D.; Parkhill, J.; Harris, S.R. Rapid Phylogenetic Analysis of Large Samples of Recombinant Bacterial Whole Genome Sequences Using Gubbins. Nucleic Acids Res. 2015, 43, e15. [Google Scholar] [CrossRef] [PubMed]
- Raphael, B.H.; Baker, D.J.; Nazarian, E.; Lapierre, P.; Bopp, D.; Kozak-Muiznieks, N.A.; Morrison, S.S.; Lucas, C.E.; Mercante, J.W.; Musser, K.A.; et al. Genomic Resolution of Outbreak-Associated Legionella pneumophila Serogroup 1 Isolates From New York State. Appl. Environ. Microbiol. 2016, 82, 3582–3590. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Kuroki, T.; Amemura-Maekawa, J.; Ohya, H.; Furukawa, I.; Suzuki, M.; Masaoka, T.; Aikawa, K.; Hibi, K.; Morita, M.; Lee, K.I.; et al. Outbreak of Legionnaire’s Disease Caused by Legionella pneumophila Serogroups 1 and 13. Emerg. Infect. Dis. 2017, 23, 349–351. [Google Scholar] [CrossRef] [PubMed]
- Qin, T.; Yan, G.; Ren, H.; Zhou, H.; Wang, H.; Xu, Y.; Zhao, M.; Guan, H.; Li, M.; Shao, Z. High Prevalence, Genetic Diversity and Intracellular Growth Ability of Legionella in Hot Spring Environments. PLoS ONE 2013, 8, e59018. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nakanishi, N.; Komatsu, S.; Tanaka, S.; Mukai, K.; Nomoto, R. Investigation of a Legionella pneumophila Outbreak at a Bath Facility in Japan Using Whole-Genome Sequencing of Isolates from Clinical and Environmental Samples. Microorganisms 2023, 11, 28. https://doi.org/10.3390/microorganisms11010028
Nakanishi N, Komatsu S, Tanaka S, Mukai K, Nomoto R. Investigation of a Legionella pneumophila Outbreak at a Bath Facility in Japan Using Whole-Genome Sequencing of Isolates from Clinical and Environmental Samples. Microorganisms. 2023; 11(1):28. https://doi.org/10.3390/microorganisms11010028
Chicago/Turabian StyleNakanishi, Noriko, Shoko Komatsu, Shinobu Tanaka, Kengo Mukai, and Ryohei Nomoto. 2023. "Investigation of a Legionella pneumophila Outbreak at a Bath Facility in Japan Using Whole-Genome Sequencing of Isolates from Clinical and Environmental Samples" Microorganisms 11, no. 1: 28. https://doi.org/10.3390/microorganisms11010028
APA StyleNakanishi, N., Komatsu, S., Tanaka, S., Mukai, K., & Nomoto, R. (2023). Investigation of a Legionella pneumophila Outbreak at a Bath Facility in Japan Using Whole-Genome Sequencing of Isolates from Clinical and Environmental Samples. Microorganisms, 11(1), 28. https://doi.org/10.3390/microorganisms11010028




