Synergistic In Vitro Antimicrobial Activity of Triton X-100 and Metformin against Enterococcus faecalis in Normal and High-Glucose Conditions
Abstract
:1. Introduction
2. Materials and Methods
2.1. Antibacterial Activities of TX-100, Met, and TX-100 + Met against Planktonic E. faecalis
2.1.1. Minimum Inhibitory Concentration (MIC) and Minimum Bactericidal Concentration Required to Kill 99% Bacteria (MBC99)
2.1.2. Synergistic Antibacterial Activities of TX-100 and Met against E. faecalis
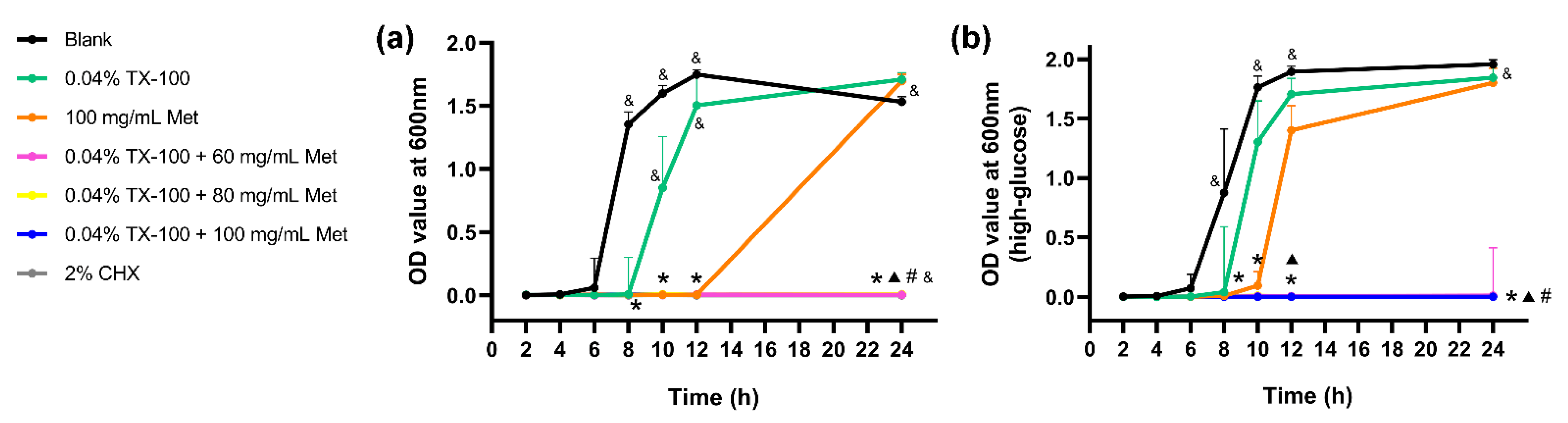
2.1.3. Dynamic Time-Killing Assays
2.2. Antibiofilm Activities of TX-100, Met, and TX-100 + Met against E. faecalis Biofilm
2.2.1. Inhibition of Bacterial Attachment
2.2.2. Biofilm Disruption Assay
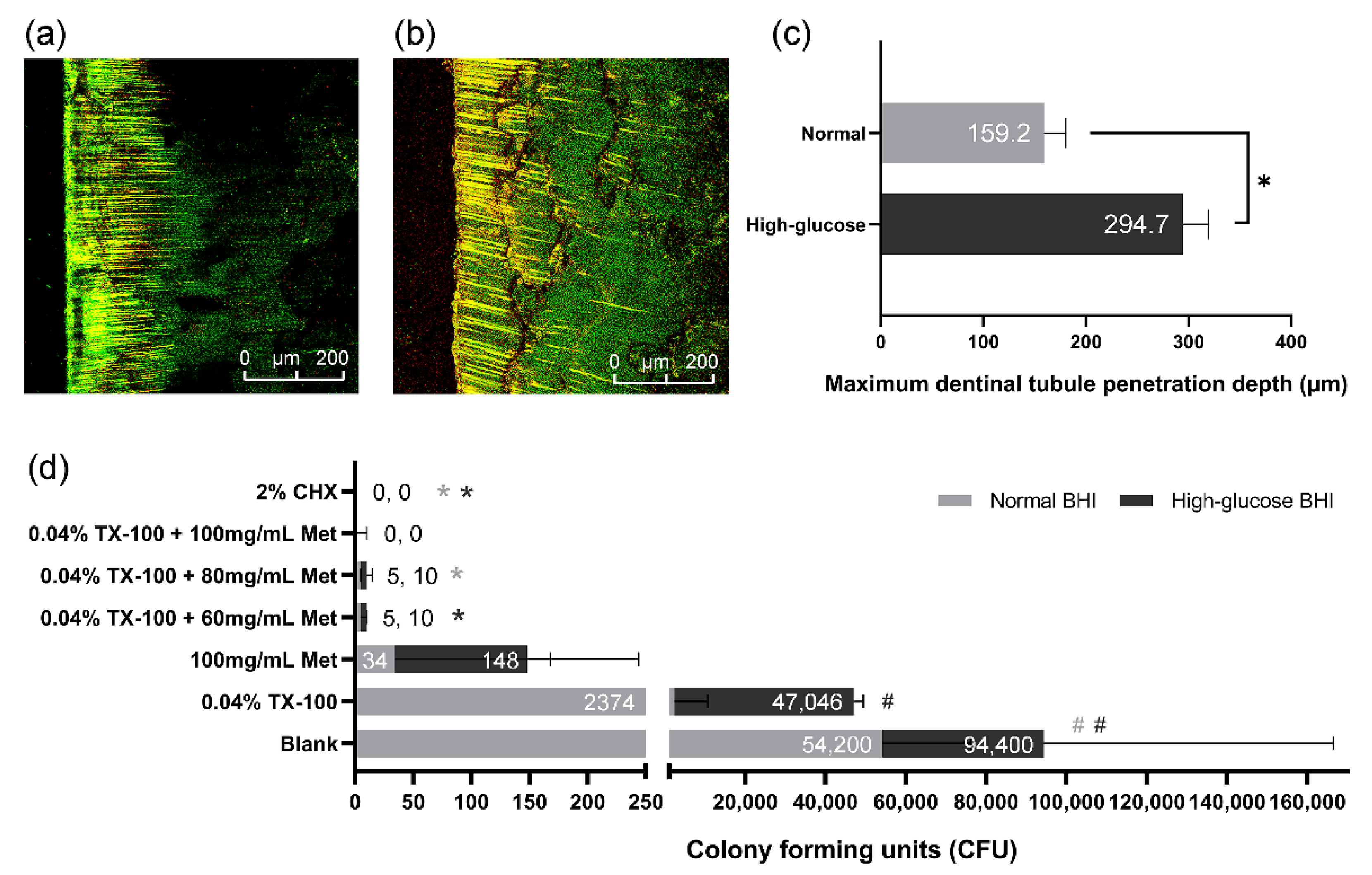
2.3. Antimicrobial Effect against E. faecalis on Dentin
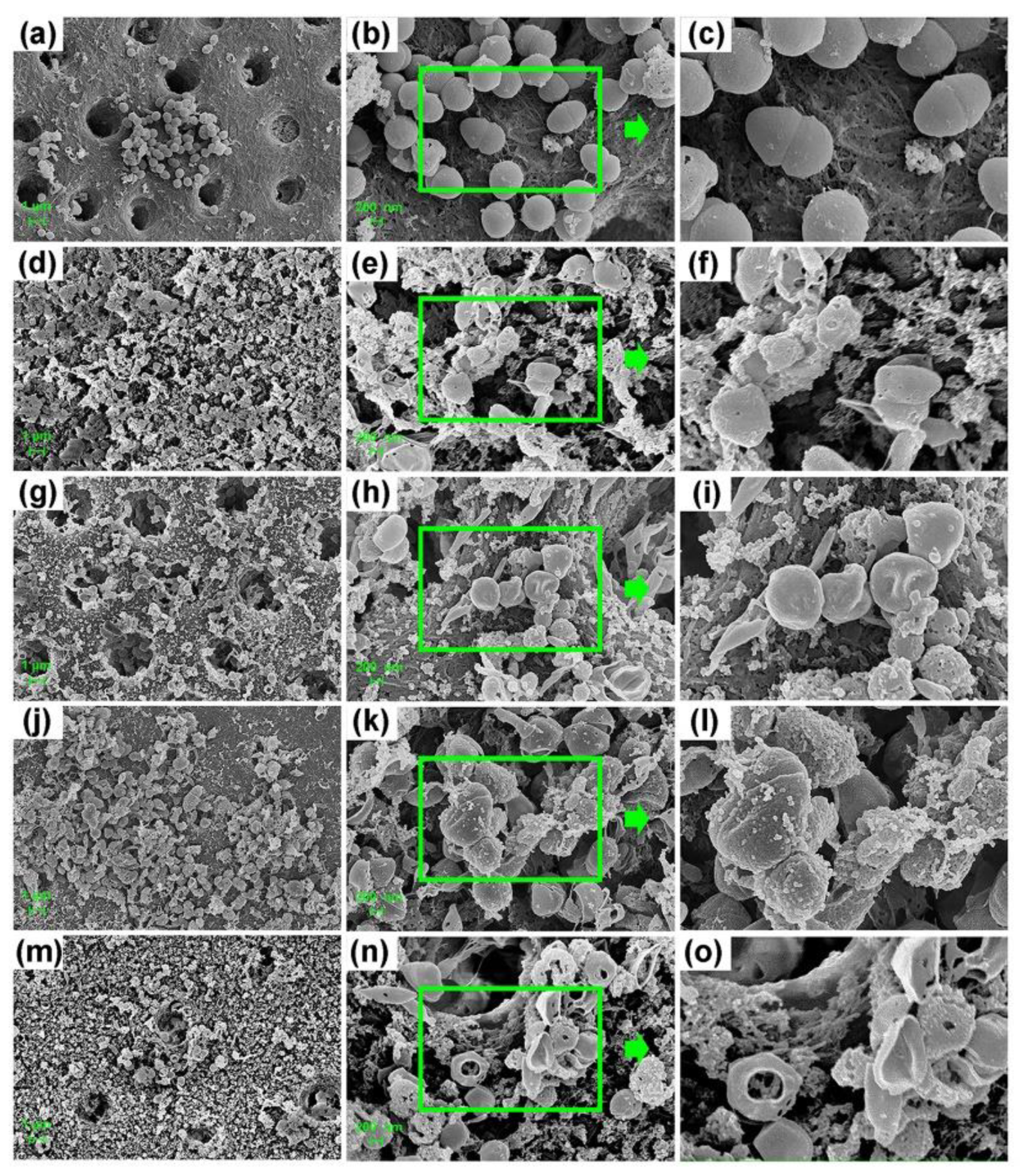
2.3.1. E. faecalis on the Dentin Surface
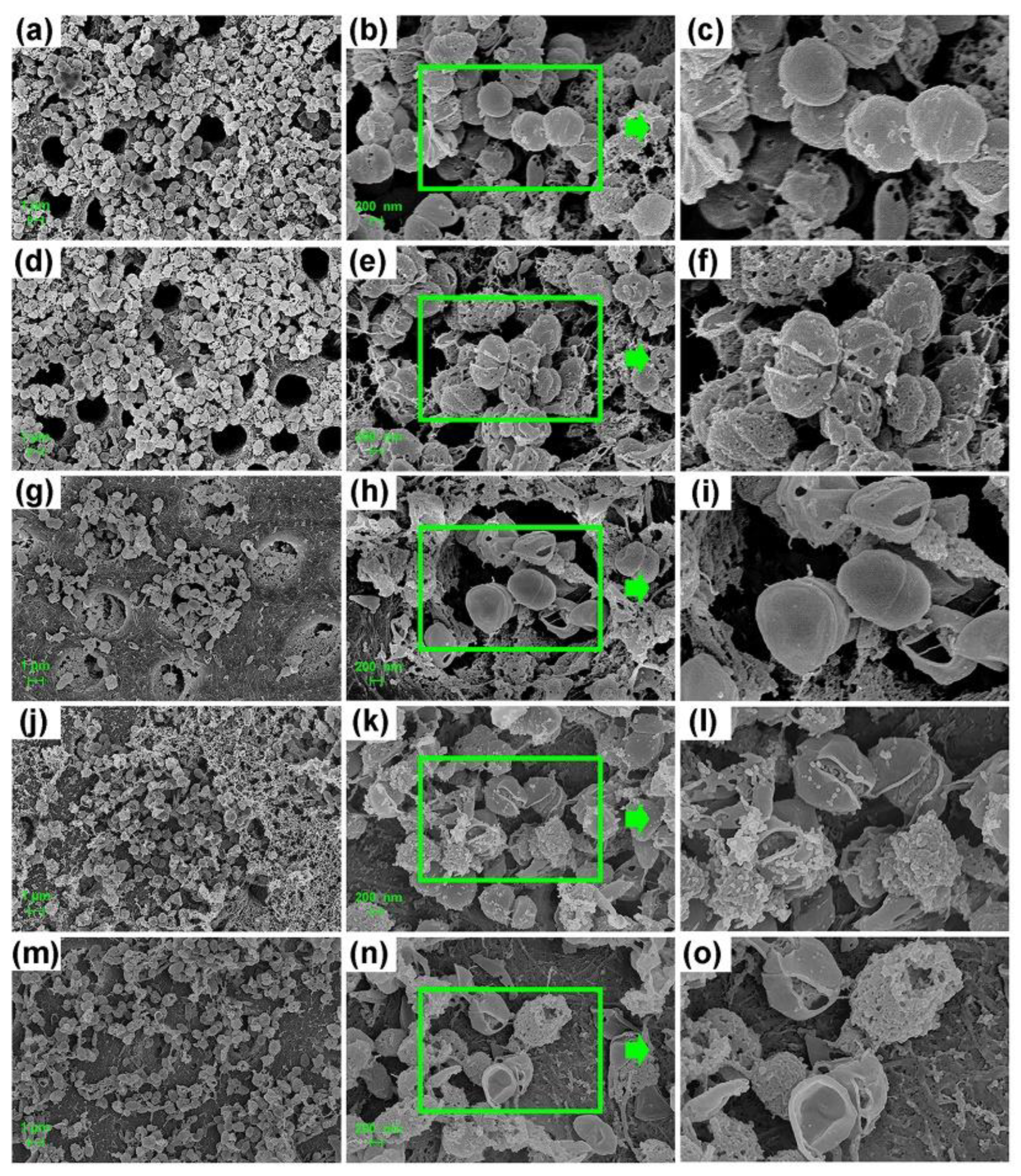
2.3.2. E. faecalis in the Dentinal Tubules
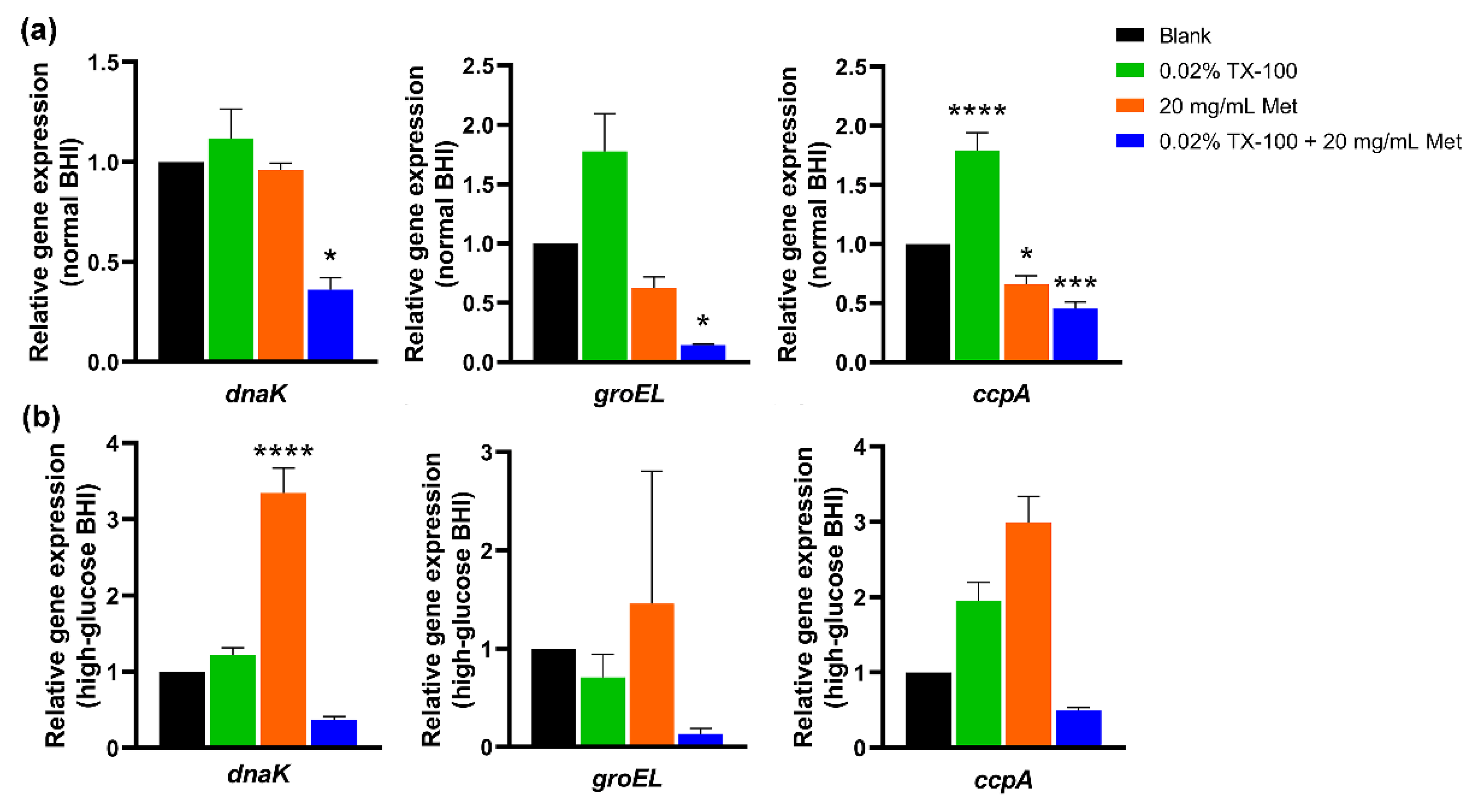
2.4. In Vitro Gene Expression Assay
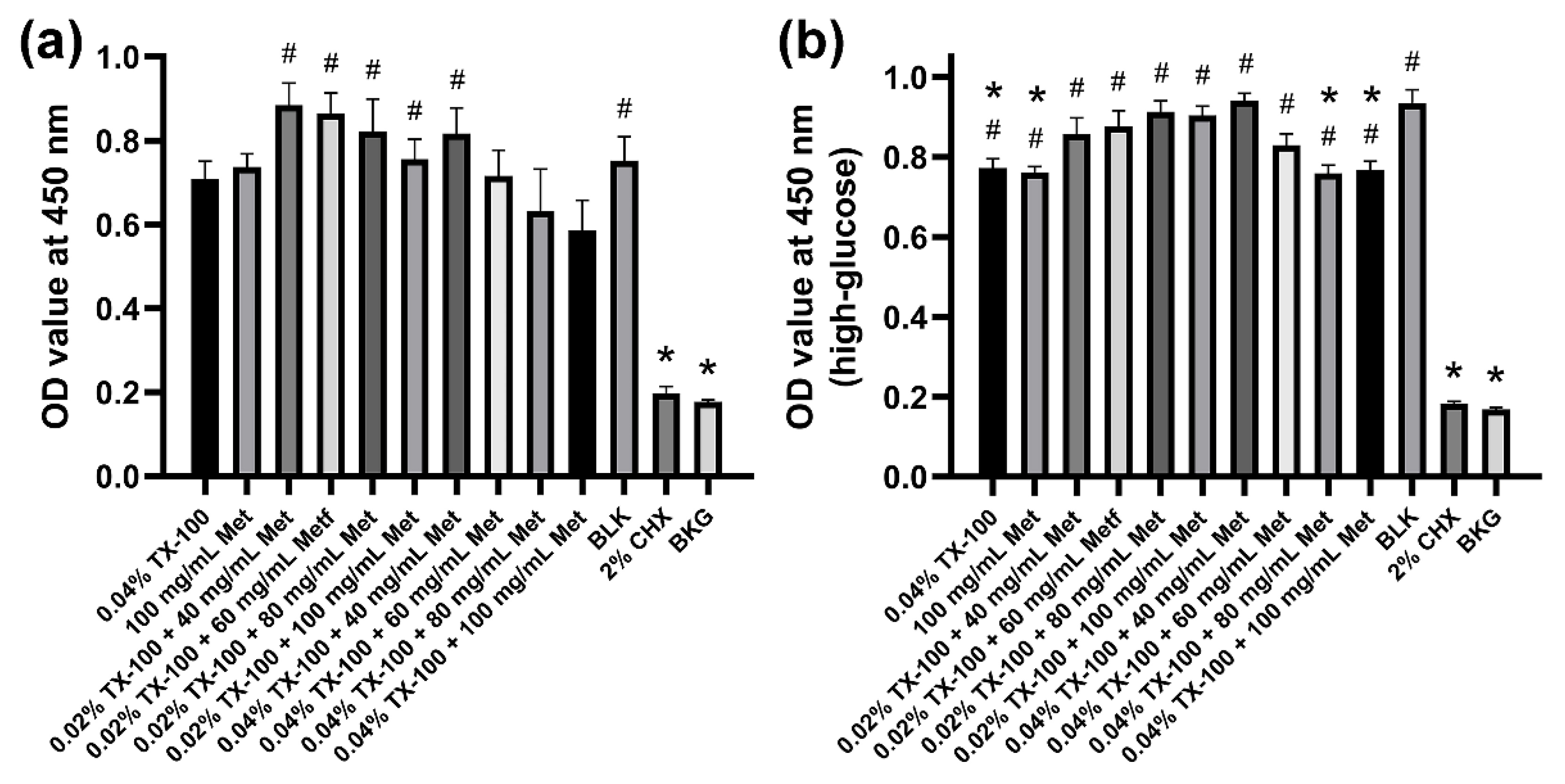
2.5. Cytotoxicity Test
2.6. Statistical Analysis
3. Results
3.1. Antibacterial Activities of TX-100, Met, and TX-100 + Met against Planktonic E. faecalis
3.2. Antibiofilm Activities of TX-100, Met, and TX-100 + Met against E. faecalis Biofilm
3.3. Antimicrobial Effect against E. faecalis on Dentin
3.4. In Vitro Gene Expression Assay
3.5. Cytotoxicity Test
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- De Paz, L.E.C.; Dahlén, G.; Molander, A.; Möller, Å.; Bergenholtz, G. Bacteria recovered from teeth with apical periodontitis after antimicrobial endodontic treatment. Int. Endod. J. 2003, 36, 500–508. [Google Scholar] [CrossRef]
- Molander, A.; Reit, C.; Dahlén, G.; Kvist, T. Microbiological status of root-filled teeth with apicalperiodontitis. Int. Endod. J. 1998, 31, 1–7. [Google Scholar] [CrossRef]
- Rôças, I.N.; Siqueira, J.F.J.; Santos, K.R. Association of Enterococcus faecalis with different forms of periradicular diseases. J. Endod. 2004, 30, 315–320. [Google Scholar] [CrossRef]
- Siqueira, J.F.J.; Rôças, I.N. Polymerase chain reaction-based analysis of microorganisms associated with failed endodontic treatment. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2004, 97, 85–94. [Google Scholar] [CrossRef]
- Estrela, C.; Silva, J.A.; de Alencar, A.H.; Leles, C.R.; Decurcio, D.A. Efficacy of sodium hypochlorite and chlorhexidine against Enterococcus faecalis—A systematic review. J. Appl. Oral Sci. Rev. Fob 2008, 16, 364–368. [Google Scholar] [CrossRef] [PubMed]
- Stuart, C.H.; Schwartz, S.A.; Beeson, T.J.; Owatz, C.B. Enterococcus faecalis: Its role in root canal treatment failure and current concepts in retreatment. J. Endod. 2006, 32, 93–98. [Google Scholar] [CrossRef] [PubMed]
- Machado, V.; Botelho, J.; Proença, L.; Alves, R.; Oliveira, M.J.; Amaro, L.; Águas, A.; Mendes, J.J. Periodontal status, perceived stress, diabetes mellitus and oral hygiene care on quality of life: A structural equation modelling analysis. BMC Oral Health 2020, 20, 229. [Google Scholar] [CrossRef] [PubMed]
- Cerda, J.; Vázquez de la Torre, C.; Malacara, J.M.; Nava, L.E. Periodontal disease in non-insulin dependent diabetes mellitus (NIDDM). The effect of age and time since diagnosis. J. Periodontol. 1994, 65, 991–995. [Google Scholar] [CrossRef] [PubMed]
- Iacopino, A.M.; Cutler, C.W. Pathophysiological Relationships Between Periodontitis and Systemic Disease: Recent Concepts Involving Serum Lipids. J. Periodontol. 2000, 71, 1375–1384. [Google Scholar] [CrossRef] [PubMed]
- Iwama, A.; Nishigaki, N.; Nakamura, K.; Imaizumi, I.; Shibata, N.; Yamasaki, M.; Nakamura, H.; Kameyama, Y.; Kapila, Y. The effect of high sugar intake on the development of periradicular lesions in rats with type 2 diabetes. J. Dent. Res. 2003, 82, 322–325. [Google Scholar] [CrossRef]
- Lima, S.M.F.; Grisi, D.C.; Kogawa, E.M.; Franco, O.L.; Peixoto, V.C.; Gonçalves-Júnior, J.F.; Arruda, M.P.; Rezende, T.M.B. Diabetes mellitus and inflammatory pulpal and periapical disease: A review. Int. Endod. J. 2013, 46, 700–709. [Google Scholar] [CrossRef] [PubMed]
- Arya, S.; Duhan, J.; Tewari, S.; Sangwan, P.; Ghalaut, V.; Aggarwal, S. Healing of Apical Periodontitis after Nonsurgical Treatment in Patients with Type 2 Diabetes. J. Endod. 2017, 43, 1623–1627. [Google Scholar] [CrossRef]
- Fouad, A.F.; Burleson, J. The effect of diabetes mellitus on endodontic treatment outcome: Data from an electronic patient record. J. Am. Dent. Assoc. 2003, 134, 43–51. [Google Scholar] [CrossRef] [Green Version]
- Siqueira, J.F.J.; Rôças, I.N.; Marceliano-Alves, M.F.; Pérez, A.R.; Ricucci, D. Unprepared root canal surface areas: Causes, clinical implications, and therapeutic strategies. Braz. Oral Res. 2018, 32, e65. [Google Scholar] [CrossRef] [Green Version]
- Bernardi, S.; Anderson, A.; Macchiarelli, G.; Hellwig, E.; Cieplik, F.; Vach, K.; Al-Ahmad, A. Subinhibitory antibiotic concentrations enhance biofilm formation of clinical enterococcus faecalis isolates. Antibiotics 2021, 10, 874. [Google Scholar] [CrossRef] [PubMed]
- Neu, H.C. The crisis in antibiotic resistance. Science. 1992, 257, 1064–1073. [Google Scholar] [CrossRef] [Green Version]
- Smith, R.A.; M’ikanatha, N.M.; Read, A.F. Antibiotic Resistance: A Primer and Call to Action. Health Commun. 2015, 30, 309–314. [Google Scholar] [CrossRef] [Green Version]
- DeFronzo, R.A.; Goodman, A.M. Efficacy of metformin in patients with non-insulin-dependent diabetes mellitus. The Multicenter Metformin Study Group. N. Engl. J. Med. 1995, 333, 541–549. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ramachandran, A.; Snehalatha, C.; Mary, S.; Mukesh, B.; Bhaskar, A.D.; Vijay, V. The Indian Diabetes Prevention Programme shows that lifestyle modification and metformin prevent type 2 diabetes in Asian Indian subjects with impaired glucose tolerance (IDPP-1). Diabetologia 2006, 49, 289–297. [Google Scholar] [CrossRef] [Green Version]
- Wang, G.; Lin, F.; Wan, Q.; Wu, J.; Luo, M. Mechanisms of action of metformin and its regulatory effect on microRNAs related to angiogenesis. Pharmacol. Res. 2021, 164, 105390. [Google Scholar] [CrossRef]
- Malik, F.; Mehdi, S.F.; Ali, H.; Patel, P.; Basharat, A.; Kumar, A.; Ashok, F.; Stein, J.; Brima, W.; Malhotra, P.; et al. Is metformin poised for a second career as an antimicrobial? Diabetes. Metab. Res. Rev. 2018, 34, e2975. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rena, G.; Hardie, D.G.; Pearson, E.R. The mechanisms of action of metformin. Diabetologia 2017, 60, 1577–1585. [Google Scholar] [CrossRef] [Green Version]
- Tahrani, A.A.; Varughese, G.I.; Scarpello, J.H.; Hanna, F.W.F. Metformin, heart failure, and lactic acidosis: Is metformin absolutely contraindicated? BMJ 2007, 335, 508–512. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Elgendy, M.; Cirò, M.; Hosseini, A.; Weiszmann, J.; Mazzarella, L.; Ferrari, E.; Cazzoli, R.; Curigliano, G.; DeCensi, A.; Bonanni, B.; et al. Combination of Hypoglycemia and Metformin Impairs Tumor Metabolic Plasticity and Growth by Modulating the PP2A-GSK3β-MCL-1 Axis. Cancer Cell 2019, 35, 798–815.e5. [Google Scholar] [CrossRef]
- Lv, Z.; Guo, Y. Metformin and Its Benefits for Various Diseases. Front. Endocrinol. 2020, 11, 191. [Google Scholar] [CrossRef] [PubMed]
- Drzewoski, J.; Hanefeld, M. The current and potential therapeutic use of metformin—The good old drug. Pharmaceuticals 2021, 14, 121–154. [Google Scholar] [CrossRef]
- Khajuria, D.K.; Patil, O.N.; Karasik, D.; Razdan, R. Development and evaluation of novel biodegradable chitosan based metformin intrapocket dental film for the management of periodontitis and alveolar bone loss in a rat model. Arch. Oral Biol. 2018, 85, 120–129. [Google Scholar] [CrossRef]
- Bai, Y.; Park, I.S.; Lee, S.J.; Bae, T.S.; Watari, F.; Uo, M.; Lee, M.H. Aqueous dispersion of surfactant-modified multiwalled carbon nanotubes and their application as an antibacterial agent. Carbon N. Y. 2011, 49, 3663–3671. [Google Scholar] [CrossRef]
- Cho, G.; Kwon, J.; Soh, S.M.; Jang, H.; Mitchell, R.J. Sensitivity of predatory bacteria to different surfactants and their application to check bacterial predation. Appl. Microbiol. Biotechnol. 2019, 103, 8169–8178. [Google Scholar] [CrossRef]
- Karuppiah, S.; Thangaraj, S.; Arunachalam Palaniappan, S.; Olapalayam Lakshmanan, S. Influence of surfactants on structural, morphological, optical and antibacterial properties of SnO2 nanoparticles. IET Nanobiotechnol. 2019, 13, 952–956. [Google Scholar] [CrossRef]
- Lee, Y.S.; Lee, D.Y.; Kim, Y.B.; Lee, S.W.; Cha, S.W.; Park, H.W.; Kim, G.S.; Kwon, D.Y.; Lee, M.H.; Han, S.H. The mechanism underlying the antibacterial activity of shikonin against methicillin-resistant staphylococcus aureus. Evid. Based Complement. Altern. Med. eCAM 2015, 2015, 520578. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Omri, A.; Ravaoarinoro, M.; Poisson, M. Incorporation, release and in-vitro antibacterial activity of liposomal aminoglycosides against pseudomonas aeruginosa. J. Antimicrob. Chemother. 1995, 36, 631–639. [Google Scholar] [CrossRef]
- Richardson, K.E.; Xue, Z.; Huang, Y.; Seo, Y.; Lapitsky, Y. Physicochemical and antibacterial properties of surfactant mixtures with quaternized chitosan microgels. Carbohydr. Polym. 2013, 93, 709–717. [Google Scholar] [CrossRef] [PubMed]
- Komatsuzawa, H.; Sugai, M.; Shirai, C.; Suzuki, J.; Hiramatsu, K.; Suginaka, H. Triton X-100 alters the resistance level of methicillin-resistant Staphylococcus aureus to oxacillin. FEMS Microbiol. Lett. 1995, 134, 209–212. [Google Scholar] [CrossRef] [PubMed]
- Fuss, Z.; Mizrahi, A.; Lin, S.; Cherniak, O.; Weiss, E.I. A laboratory study of the effect of calcium hydroxide mixed with iodine or electrophoretically activated copper on bacterial viability in dentinal tubules. Int. Endod. J. 2002, 35, 522–526. [Google Scholar] [CrossRef] [PubMed]
- Lin, S.; Levin, L.; Peled, M.; Weiss, E.I.; Fuss, Z. Reduction of viable bacteria in dentinal tubules treated with clindamycin or tetracycline. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2003, 96, 751–756. [Google Scholar] [CrossRef]
- Gomes, B.P.F.A.; Souza, S.F.C.; Ferraz, C.C.R.; Teixeira, F.B.; Zaia, A.A.; Valdrighi, L.; Souza-Filho, F.J. Effectiveness of 2% chlorhexidine gel and calcium hydroxide against Enterococcus faecalis in bovine root dentine in vitro. Int. Endod. J. 2003, 36, 267–275. [Google Scholar] [CrossRef] [PubMed]
- Fan, W.; Huang, Z.; Fan, B. Effects of prolonged exposure to moderate static magnetic field and its synergistic effects with alkaline pH on Enterococcus faecalis. Microb. Pathog. 2018, 115, 117–122. [Google Scholar] [CrossRef]
- Isoda, K.; Young, J.L.; Zirlik, A.; MacFarlane, L.A.; Tsuboi, N.; Gerdes, N.; Schönbeck, U.; Libby, P. Metformin inhibits proinflammatory responses and nuclear factor-κB in human vascular wall cells. Arterioscler. Thromb. Vasc. Biol. 2006, 26, 611–617. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bak, E.J.; Park, H.G.; Kim, M.; Kim, S.W.; Kim, S.; Choi, S.-H.; Cha, J.-H.; Yoo, Y.-J. The Effect of Metformin on Alveolar Bone in Ligature-Induced Periodontitis in Rats: A Pilot Study. J. Periodontol. 2010, 81, 412–419. [Google Scholar] [CrossRef]
- Tendolkar, P.M.; Baghdayan, A.S.; Gilmore, M.S.; Shankar, N. Enterococcal surface protein, Esp, enhances biofilm formation by Enterococcus faecalis. Infect. Immun. 2004, 72, 6032–6039. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, M.A.; Rosa, V.; Min, K.S. Characterization of Enterococcus faecalis in different culture conditions. Sci. Rep. 2020, 10, 21867. [Google Scholar] [CrossRef]
- Liu, Y.X.; Cao, Q.M.; Ma, B.C. Pathogens distribution and drug resistance in patients with acute cerebral infarction complicated with diabetes and nosocomial pulmonary infection. BMC Infect. Dis. 2019, 19, 603–608. [Google Scholar] [CrossRef]
- Parsell, D.A.; Lindquist, S. The function of heat-shock proteins in stress tolerance: Degradation and reactivation of damaged proteins. Annu. Rev. Genet. 1993, 27, 437–496. [Google Scholar] [CrossRef]
- Rince, A.; Flahaut, S.; Auffray, Y. Identification of general stress genes in Enterococcus faecalis. Int. J. Food Microbiol. 2000, 55, 87–91. [Google Scholar] [CrossRef]
- Leboeuf, C.; Leblanc, L.; Auffray, Y.; Hartke, A. Characterization of the ccpA gene of Enterococcus faecalis: Identification of starvation-inducible proteins regulated by ccpA. J. Bacteriol. 2000, 182, 5799–5806. [Google Scholar] [CrossRef] [Green Version]
- Seidl, K.; Stucki, M.; Ruegg, M.; Goerke, C.; Wolz, C.; Harris, L.; Berger-Bächi, B.; Bischoff, M. Staphylococcus aureus CcpA affects virulence determinant production and antibiotic resistance. Antimicrob. Agents Chemother. 2006, 50, 1183–1194. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bayerl, T.; Klose, G.; Blanck, J.; Ruckpaul, K. Interaction of nonionic detergents with phospholipids in hepatic microsomes at subsolubilizing concentrations as studied by 31P-NMR. Biochim. Biophys. Acta 1986, 858, 285–293. [Google Scholar] [CrossRef]
- Schnaitman, C.A. Solubilization of the cytoplasmic membrane of Escherichia coli by Triton X-100. J. Bacteriol. 1971, 108, 545–552. [Google Scholar] [CrossRef] [Green Version]
- Colavita, F.; Quartu, S.; Lalle, E.; Bordi, L.; Lapa, D.; Meschi, S.; Vulcano, A.; Toffoletti, A.; Bordi, E.; Paglia, M.G.; et al. Evaluation of the inactivation effect of Triton X-100 on Ebola virus infectivity. J. Clin. Virol. 2017, 86, 27–30. [Google Scholar] [CrossRef] [PubMed]
- Sudbrack, T.P.; Archilha, N.L.; Itri, R.; Riske, K.A. Observing the solubilization of lipid bilayers by detergents with optical microscopy of GUVs. J. Phys. Chem. B 2011, 115, 269–277. [Google Scholar] [CrossRef] [PubMed]
- Chivatxaranukul, P.; Dashper, S.G.; Messer, H.H. Dentinal tubule invasion and adherence by Enterococcus faecalis. Int. Endod. J. 2008, 41, 873–882. [Google Scholar] [CrossRef] [PubMed]
- Haapasalo, M.; Ørstavik, D. In vitro Infection and Disinfection of Dentinal Tubules. J. Dent. Res. 1987, 66, 1375–1379. [Google Scholar] [CrossRef] [PubMed]

| Gene | Primer Sequence | Amplicon Size (bp) | Reference | |
|---|---|---|---|---|
| 16S | 16Sf | TCAAAGGAGAAGTTCGGGTCATTTCG | 136 | This study |
| 16Sr | TTCTTATGCTTGCGGTGGGACTTC | |||
| dnaK | dnaKf | ACAGCCGGTGATAACAACCT | 152 | [38] |
| dnaKr | TGGCAAGCTGATTTGTGTGC | |||
| groEL | groELf | ACCTGATGAAACAGCAGCGA | 136 | [38] |
| groELr | TGCTGGAGCCAACCCATTAG | |||
| ccpA | ccpAf | AATAAGCGCATTGACACGGC | 226 | This study |
| ccpAr | ATTTGGCTGATCGTGTCCGT | |||
| Groups | E. faecalis in Normal BHI | E. faecalis in High-Glucose BHI | ||
|---|---|---|---|---|
| MIC | MBC99 | MIC | MBC99 | |
| TX-100 (%v/v) | - | - | - | - |
| Met (mg/mL) | 100 | 160 | 100 | 180 |
| 0.02% TX-100 + Met (mg/mL) | 20 | 30 | 20 | 50 |
| 0.04% TX-100 + Met (mg/mL) | 20 | 30 | 20 | 40 |
| Groups | E. faecalis in Normal BHI | E. faecalis in High-Glucose BHI | ||
|---|---|---|---|---|
| MBIC50 | MBRC50 | MBIC50 | MBRC50 | |
| TX-100 (%v/v) | - | - | - | - |
| Met (mg/mL) | 100 | 200 | 100 | 300 |
| 0.02% TX-100 + Met (mg/mL) | 40 | 40 | 40 | 60 |
| 0.04% TX-100 + Met (mg/mL) | 10 | 40 | 20 | 60 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
He, X.; Jin, S.; Fan, W.; Fan, B. Synergistic In Vitro Antimicrobial Activity of Triton X-100 and Metformin against Enterococcus faecalis in Normal and High-Glucose Conditions. Microorganisms 2022, 10, 124. https://doi.org/10.3390/microorganisms10010124
He X, Jin S, Fan W, Fan B. Synergistic In Vitro Antimicrobial Activity of Triton X-100 and Metformin against Enterococcus faecalis in Normal and High-Glucose Conditions. Microorganisms. 2022; 10(1):124. https://doi.org/10.3390/microorganisms10010124
Chicago/Turabian StyleHe, Xinling, Siqi Jin, Wei Fan, and Bing Fan. 2022. "Synergistic In Vitro Antimicrobial Activity of Triton X-100 and Metformin against Enterococcus faecalis in Normal and High-Glucose Conditions" Microorganisms 10, no. 1: 124. https://doi.org/10.3390/microorganisms10010124
APA StyleHe, X., Jin, S., Fan, W., & Fan, B. (2022). Synergistic In Vitro Antimicrobial Activity of Triton X-100 and Metformin against Enterococcus faecalis in Normal and High-Glucose Conditions. Microorganisms, 10(1), 124. https://doi.org/10.3390/microorganisms10010124








