Cobalt (II) Chloride Regulates the Invasion and Survival of Brucella abortus 544 in RAW 264.7 Cells and B6 Mice
Abstract
:1. Introduction
2. Results
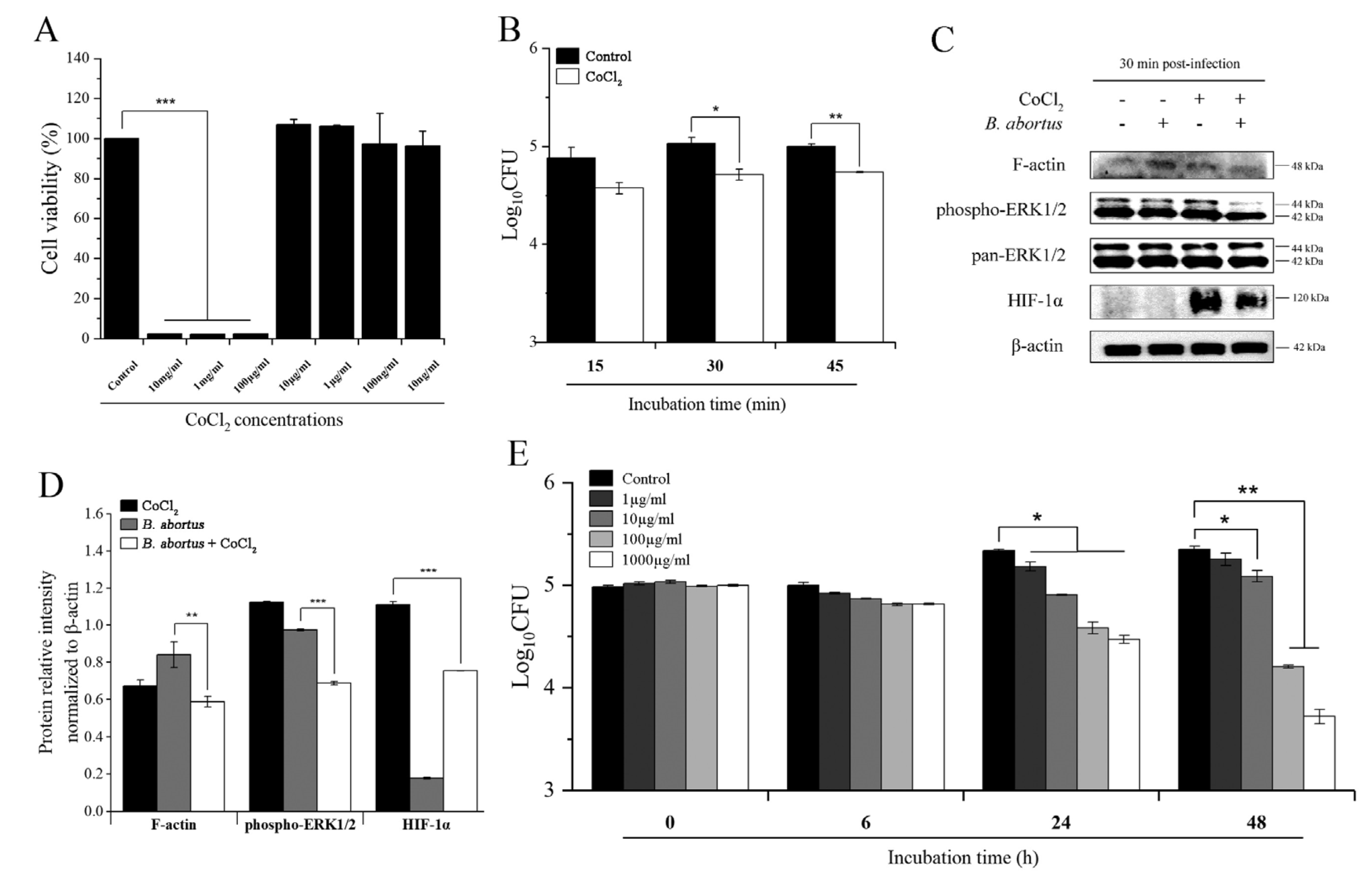
2.1. CoCl2 Treatment Inhibited the Invasion of B. abortus into RAW 264.7 Macrophage Cells and Affected Brucella survival in Axenic Culture
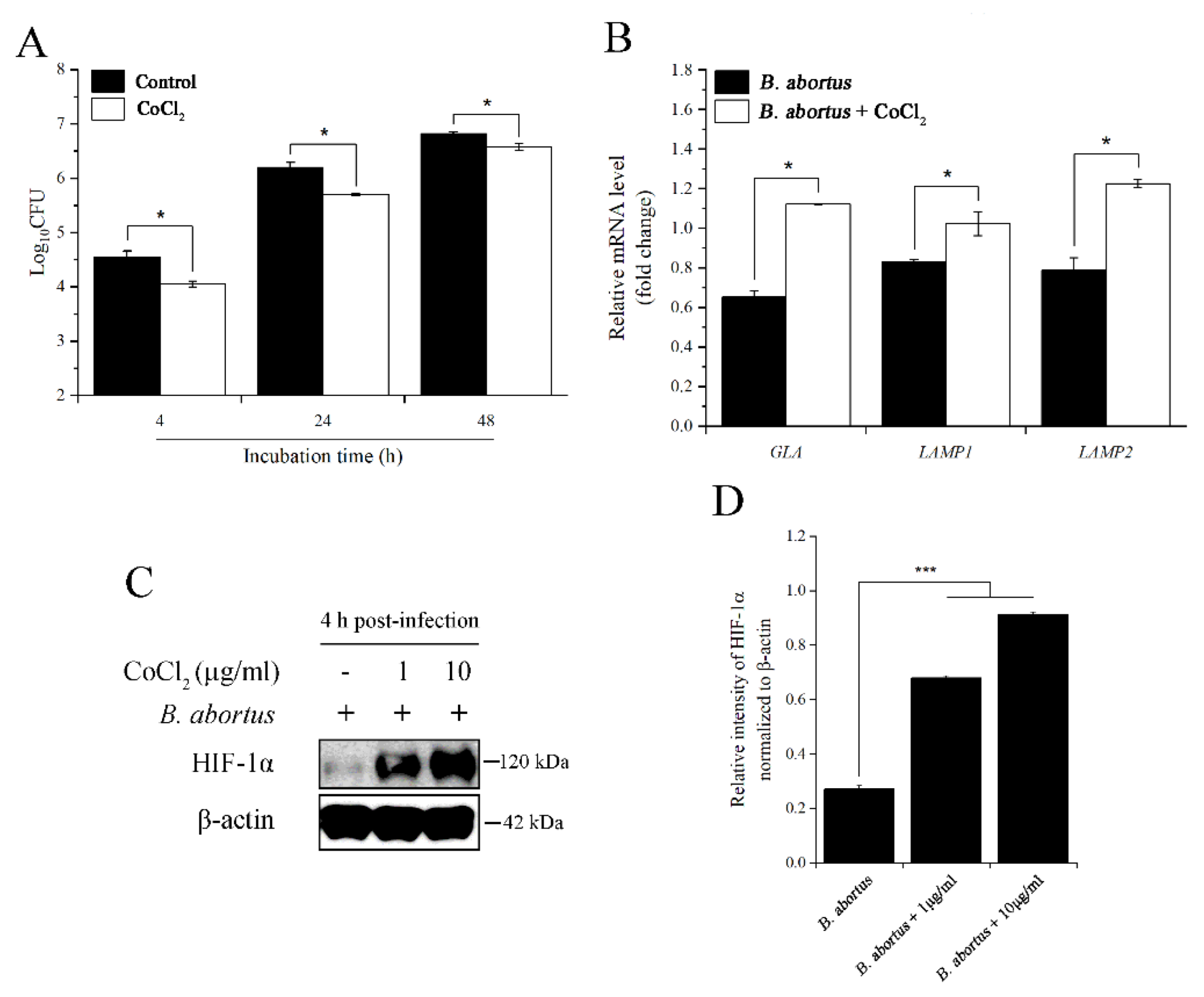
2.2. CoCl2 Treatment Affected the Survival of B. abortus in RAW 264.7 Macrophage Cells at 4 h pi
2.3. CoCl2 and HIF-1α Affected the Survival of B. abortus in RAW 264.7 Macrophage Cells at 24 h pi
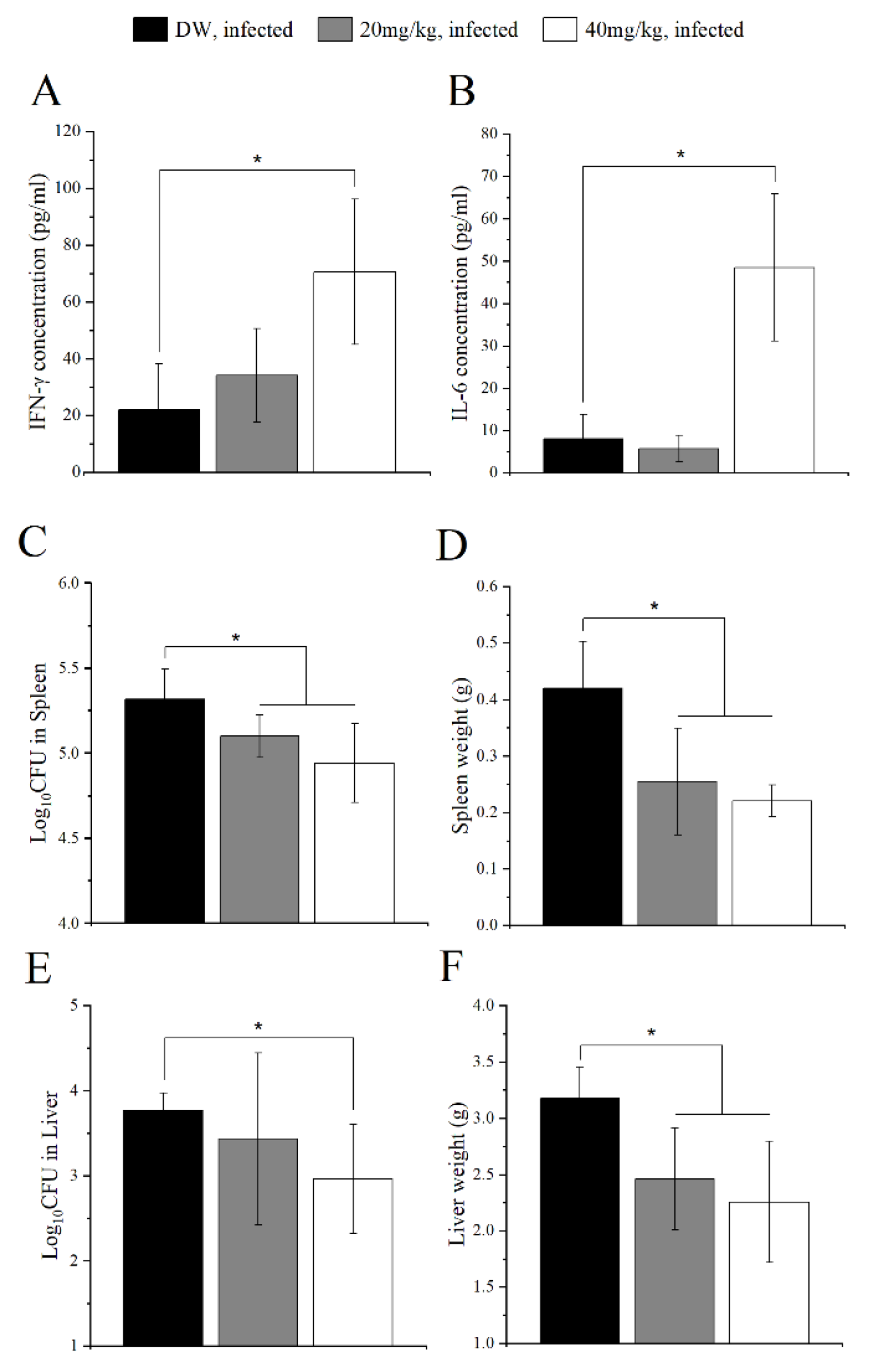
2.4. CoCl2 Administration Mediated Host Immunity against B. abortus Infection in Mice
3. Discussion
4. Materials and Methods
4.1. Cell Culture and Bacterial Growth Condition
4.2. CoCl2 Solution Preparation and Cell Viability Assessment Assay
4.3. Bacterial Invasion and Intracellular Growth Assay
4.4. Western Blot
4.5. Bactericidal Effect Assay
4.6. Ribonucleic Acid (RNA) Isolation and Quantitative Real-Time PCR
4.7. siRNA Knockdown
4.8. Mice Treatment with CoCl2 and Protection Experiment
4.9. Serum Cytokine Level Measurement
4.10. Statistical Analysis
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- El-Sayed, A.; Awad, W. Brucellosis: Evolution and expected comeback. Int. J. Vet. Sci. Med. 2018, 6, S31–S35. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- He, Y. Analyses of Brucella pathogenesis, host immunity, and vaccine targets using systems biology and bioinformatics. Front. Cell. Infect. Microbiol. 2012, 2, 2. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Addis, M. Public health and economic importance of Brucellosis: A review. Public. Policy. Adm. Res. 2015, 5, 68–84. [Google Scholar]
- Gonzalez-Espinoza, G.; Arce-Gorvel, V.; Memet, S.; Gorvel, J. Brucella: Reservoirs and niches in animals and humans. Pathogens 2021, 10, 186. [Google Scholar] [CrossRef]
- Roop, R.M., II; Barton, I.S.; Hopersberger, D.; Martin, D.W. Uncovering the hidden credentials of Brucella virulence. Microbiol. Mol. Biol. Rev. 2021, 85, e00021-19. [Google Scholar] [CrossRef]
- Simonsen, L.O.; Harbak, H.; Bennekou, P. Cobalt metabolism and toxicology-A brief update. Sci. Total. Environ. 2012, 432, 210–215. [Google Scholar] [CrossRef]
- Kobayashi, M.; Shimizu, S. Cobalt proteins. Eur. J. Biochem. 1999, 261, 1–9. [Google Scholar] [CrossRef]
- Barceloux, D.G.; Barceloux, D.D. Cobalt. J. Toxicol. Clin. Toxicol. 1999, 37, 201–216. [Google Scholar] [CrossRef]
- Huang, J.; Liu, L.; Feng, M.; An, S.; Zhou, M.; Li, Z.; Qi, J.; Shen, H. Effect of CoCl2 on fracture repair in a rat model of bone fracture. Mol. Med. Rep. 2015, 12, 5951–5956. [Google Scholar] [CrossRef] [Green Version]
- Bruggraber, S.F.A.; French, G.; Thompson, R.P.H.; Powell, J.J. Selective and effective bactericidal activity of the cobalt (II) cation against Helicobacter pylori. Helicobacter 2004, 9, 422–428. [Google Scholar] [CrossRef]
- Munoz-Sanchez, J.; Chanez-Cardenas, M.E. The use of cobalt chloride as a chemical hypoxia model. J. Appl. Toxicol. 2018, 39, 556–570. [Google Scholar] [CrossRef] [PubMed]
- Zinkernagel, A.S.; Johnson, R.S.; Nizet, V. Hypoxia inducible factor (HIF) function in innate immunity and infection. J. Mol. Med. 2007, 85, 1339–1346. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zenk, S.F.; Hauck, S.; Mayer, D.; Grieshober, M.; Stenger, S. Stabilization of Hypoxia-inducible factor promotes antimicrobial activity of human macrophages against Mycobacterium tuberculosis. Front. Immunol. 2021, 12, 678354. [Google Scholar] [CrossRef]
- Hwang, I.I.L.; Watson, I.R.; Der, S.D.; Ohh, M. Loss of VHL confers Hypoxia-inducible factor (HIF)-dependent resistance to vesicular stomatitis virus: Role of HIF in antiviral response. J. Virol. 2006, 80, 10712–10723. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Solera, J. Update on brucellosis: Therapeutic challenges. Int. J. Antimicrob. Agents. 2010, 36, S18–S20. [Google Scholar] [CrossRef] [Green Version]
- Kamaruzzaman, N.F.; Kendall, S.; Good, L. Targeting the hard to reach: Challenges and novel strategies in the treatment of intracellular bacterial infections. Br. J. Pharmacol. 2017, 174, 2225–2236. [Google Scholar] [CrossRef]
- Goodwin, Z.I.; Pascual, D.W. Brucellosis vaccines for livestock. Vet. Immunol. Immunopathol. 2016, 181, 51–58. [Google Scholar] [CrossRef] [Green Version]
- McCulloch, T.R.; Wells, T.J.; Souza-Fonseca-Guimaraes, F. Towards efficient immunotherapy for bacterial infection. Trends. Microbiol. 2021, 30, 158–169. [Google Scholar] [CrossRef]
- Mahey, S.; Kumar, R.; Arora, R.; Mahajan, J.; Arora, S.; Bhardwaj, R.; Thukral, A.K. Effect of cobalt(II) chloride hexahydrate on some human cancer cell lines. SpringerPlus 2016, 5, 930. [Google Scholar] [CrossRef] [Green Version]
- Li, Q.; Ma, R.; Zhang, M. CoCl2 increased the expression of hypoxic markers HIF-1α, VEGF and CXCR4 in breast cancer MCF-7 cells. Oncol. Lett. 2018, 15, 1119–1124. [Google Scholar] [CrossRef] [Green Version]
- Kwak, J.; Choi, S.J.; Oh, W.; Yang, Y.S.; Jeon, H.B.; Jeon, E.S. Cobalt chloride enhances the anti-inflammatory potency of human umbilical cord blood-derived mesenchymal stem cells through the ERK-HIF-1α-MicroRNA-146a-mediated signaling pathway. Stem. Cells. Int. 2018, 2018, 4978763. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Celli, J.; de Chastellier, C.; Franchini, D.M.; Pizarro-Cerda, J.; Moreno, E.; Gorvel, J.P. Brucella evades macrophage killing via VirB-dependent sustained interactions with the endoplasmic reticulum. J. Exp. Med. 2003, 198, 545–556. [Google Scholar] [CrossRef] [PubMed]
- dos Santos, S.A.; de Andrade Junior, D.R. HIF-1alpha and infectious diseases: A new frontier for the development of new therapies. Rev. Inst. Med. Trop. S. Paulo. 2017, 59, e93. [Google Scholar] [CrossRef] [PubMed]
- Hop, H.T.; Reyes, A.W.B.; Huy, T.X.N.; Arayan, L.T.; Min, W.; Lee, H.J.; Rhee, M.H.; Chang, H.H.; Kim, S. Activation of NF-ĸB-mediated TNF-induced antimicrobial immunity is required for the efficient Brucella abortus clearance in RAW 264.7 cells. Front. Cell. Infect. Microbiol. 2017, 7, 437. [Google Scholar] [CrossRef] [PubMed]
- Koo, I.C.; Ohol, Y.M.; Wu, P.; Morisaki, J.H.; Cox, J.S.; Brown, E.J. Role for lysosomal enzyme β-hexosaminidase in the control of mycobacteria infection. Proc. Natl. Acad. Sci. USA 2008, 105, 710–715. [Google Scholar] [CrossRef] [Green Version]
- Celli, J. Surviving inside a macrophage: The many ways of Brucella. Res. Microbiol. 2006, 157, 93–98. [Google Scholar] [CrossRef]
- Jiao, H.; Zhou, Z.; Li, B.; Xiao, Y.; Li, M.; Zeng, H.; Guo, X.; Gu, G. The mechanism of facultative intracellular parasitism of Brucella. Int. J. Mol. Sci. 2021, 22, 3673. [Google Scholar] [CrossRef]
- Lee, J.J.; Kim, D.H.; Kim, D.G.; Lee, H.J.; Min, W.; Rhee, M.H.; Cho, J.Y.; Watarai, M.; Kim, S. Toll-like receptor 4-linked Janus Kinase 2 signaling contributes to internalization of Brucella abortus by macrophages. Infect. Immun. 2013, 81, 2448–2458. [Google Scholar] [CrossRef] [Green Version]
- de Bagues, M.P.J.; Gross, A.; Terraza, A.; Dornand, J. Regulation of the mitogen-activated protein kinases by Brucella spp. expressing a smooth and rough phenotype: Relationship to pathogen invasiveness. Infect. Immun. 2005, 73, 3178–3183. [Google Scholar] [CrossRef] [Green Version]
- Rossi, A.; Lord, J. Adiponectin inhibits Neutrophil phagocytosis of Escherichia coli by inhibition of PKB and ERK 1/2 MAPK signalling and Mac-1 activation. PLoS ONE 2013, 8, e69108. [Google Scholar] [CrossRef] [Green Version]
- Murata, K.; Suzuki, H.; Okano, H.; Oyamada, T.; Yasuda, Y.; Sakamoto, A. Hypoxia-induced des-γ-carboxy prothrombin production in hepatocellular carcinoma. Int. J. Oncol. 2010, 36, 161–170. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Anand, R.J.; Gribar, S.C.; Li, J.; Kohler, J.W.; Branca, M.F.; Dubowski, T.; Sodhi, C.P.; Hackam, D.J. Hypoxia causes an increase in phagocytosis by macrophages in a HIF-1α-dependent manner. J. Leukoc. Biol. 2007, 82, 1257–1265. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lei, R.; Li, J.; Liu, F.; Li, W.; Zhang, S.; Wang, Y.; Chu, X.; Xu, J. HIF-1α promotes the keloid development through the activation of TGF-β/Smad and TLR4/MyD88/NF-κB pathways. Cell Cycle 2019, 18, 3239–3250. [Google Scholar] [CrossRef] [PubMed]
- Shweta; Mishra, K.P.; Chanda, S.; Singh, S.B.; Ganju, L. A comparative immunological analysis of CoCl2 treated cells with in vitro hypoxic exposure. Biometals 2015, 28, 175–185. [Google Scholar] [CrossRef] [PubMed]
- Smith, J.A.; Khan, M.; Magnani, D.D.; Harms, J.S.; Durward, M.; Radhakrishnan, G.K.; Liu, Y.; Splitter, G.A. Brucella induces an unfolded protein response via TcpB that supports intracellular replication in macrophages. PLoS Pathog. 2013, 9, e1003785. [Google Scholar] [CrossRef] [Green Version]
- Xiong, X.; Li, B.; Zhou, Z.; Gu, G.; Li, M.; Liu, J.; Jiao, H. The VirB system plays a crucial role in Brucella intracellular infection. Int. J. Mol. Sci. 2021, 22, 13637. [Google Scholar] [CrossRef]
- Gutierrez, M.G.; Mishra, B.B.; Jordao, L.; Elliott, E.; Anes, E.; Griffiths, G. NF-ĸB activation controls phagolysosome fusion-mediated killing of Mycobacteria by macrophages. J. Immunol. 2008, 181, 2651–2663. [Google Scholar] [CrossRef] [Green Version]
- Owada, S.; Endo, H.; Shida, Y.; Okada, C.; Ito, K.; Nezu, T.; Tatemichi, M. Autophagy-mediated adaptation of hepatocellular carcinoma cells to hypoxia-mimicking conditions constitutes an attractive therapeutic target. Oncol. Rep. 2018, 39, 1805–1812. [Google Scholar] [CrossRef]
- Lu, Y.; Gu, Y.; Ding, X.; Wang, J.; Chen, J.; Miao, C. Intracellular Ca2+ homeostasis and JAK1/STAT3 pathway are involved in the protective effect of propofol on BV2 microglia against hypoxia-induced inflammation and apoptosis. PLoS ONE 2017, 12, e0178098. [Google Scholar] [CrossRef] [Green Version]
- Knight, M.; Stanley, S. HIF-1α as a central mediator of cellular resistance to intracellular pathogens. Curr. Opin. Immunol. 2019, 60, 111–116. [Google Scholar] [CrossRef]
- Li, C.; Wang, Y.; Li, Y.; Yu, Q.; Jin, X.; Wang, X.; Jia, A.; Hu, Y.; Han, L.; Wang, J.; et al. HIF1α-dependent glycolysis promotes macrophage functional activities in protecting against bacterial and fungal infection. Sci. Rep. 2018, 8, 3603. [Google Scholar] [CrossRef] [PubMed]
- Siegert, I.; Schodel, J.; Nairz, M.; Schatz, V.; Dettmer, K.; Dick, C.; Kalucka, J.; Franke, K.; Ehrenschwender, M.; Schley, G.; et al. Ferritin-mediated iron sequestration stabilizes Hypoxia-inducible factor-1α upon LPS activation in the presence of ample oxygen. Cell. Rep. 2015, 13, 2048–2055. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, S.; Seong, K.; Kim, W.; Jung, J. Epigallocatechin gallate protects against hypoxia-induced inflammation in microglia via NF-ĸB suppression and Nrf-2/HO-1 activation. Int. J. Mol. Sci. 2022, 23, 4004. [Google Scholar] [CrossRef] [PubMed]
- Rius, J.; Guma, M.; Schachtrup, C.; Akassoglou, K.; Zinkernagel, A.S.; Nizet, V.; Johnson, R.S.; Haddad, G.G.; Karin, M. NF-ĸB links innate immunity to the hypoxic response through transcriptional regulation of HIF-1α. Nature 2008, 453, 807–811. [Google Scholar] [CrossRef] [Green Version]
- Chohan, Z.H.; Supuran, C.T. In-vitro antibacterial and cytotoxic activity of cobalt (ii), copper (ii), nickel (ii) and zinc (ii) complexes of the antibiotic drug cephalothin (Keflin). J. Enzyme. Inhib. Med. Chem. 2005, 20, 463–468. [Google Scholar] [CrossRef]
- Chohan, Z.H.; Pervez, H.; Rauf, A.; Khan, K.M.; Supuran, C.T. Antibacterial cobalt (II), copper (II), nickel (II) and zinc (II) complexes of mercaptothiadiazole-derived furanyl, thienyl, pyrrolyl, salicylyl and pyridinyl Schiff bases. J. Enzyme. Inhib. Med. Chem. 2006, 21, 193–201. [Google Scholar] [CrossRef]
- Altenbern, R.A.; Williams, D.R.; Ginoza, H.S. Effect of cobalt on population changes in Brucella abortus. J. Bacteriol. 1959, 77, 509. [Google Scholar] [CrossRef] [Green Version]
- Rani, A.; Prasad, S. CoCl2-induced biochemical hypoxia down regulates activities and expression of super oxide dismutase and catalase in cerebral cortex of mice. Neurochem. Res. 2014, 39, 1787–1796. [Google Scholar] [CrossRef]
- Matsumoto, K.; Fujishiro, H.; Satoh, M.; Himeno, S. DNA microarray analysis of the liver of mice treated with cobalt chloride. J. Toxicol. Sci. 2010, 35, 935–939. [Google Scholar] [CrossRef] [Green Version]
- Yang, C.; Ling, H.; Zhang, M.; Yang, Z.; Wang, X.; Zeng, F.; Wang, C.; Feng, J. Oxidative stress mediates chemical hypoxia-induced injury and inflammation by activating NF-κB-COX-2 pathway in HaCaT Cells. Mol. Cells. 2011, 31, 531–538. [Google Scholar] [CrossRef] [Green Version]
- Dorneles, E.M.S.; Teixeira-Carvalho, A.; Araujo, M.S.S.; Sriranganathan, N.; Lage, A.P. Immune response triggered by Brucella abortus following infection or vaccination. Vaccine 2015, 33, 3659–3666. [Google Scholar] [CrossRef]
- Hop, H.T.; Huy, T.X.N.; Reyes, A.W.B.; Arayan, L.T.; Vu, S.H.; Min, W.; Lee, H.J.; Kang, C.K.; Kim, D.H.; Tark, D.S.; et al. Interleukin 6 promotes Brucella abortus clearance by controlling bactericidal activity of macrophages and CD8+ T cell differentiation. Infect. Immun. 2019, 87, e00431-19. [Google Scholar] [CrossRef] [Green Version]
- Huy, T.X.N.; Reyes, A.W.B.; Hop, H.T.; Arayan, L.T.; Min, W.; Lee, H.J.; Rhee, M.H.; Chang, H.H.; Kim, S. Intracellular trafficking modulation by Ginsenoside Rg3 inhibits Brucella abortus uptake and intracellular survival within RAW 264.7 cells. J. Microbiol. Biotechnol. 2017, 27, 616–623. [Google Scholar] [CrossRef] [Green Version]
- Hop, H.T.; Reyes, A.W.B.; Huy, T.X.N.; Arayan, L.T.; Min, W.; Lee, H.J.; Rhee, M.H.; Chang, H.H.; Kim, S. Interleukin 10 suppresses lysosome-mediated killing of Brucella abortus in cultured macrophages. J. Biol. Chem. 2018, 293, 3134–3144. [Google Scholar] [CrossRef] [Green Version]

| Gene | Description | Forward Primer | Reverse Primer |
|---|---|---|---|
| GLA | Galactosidase, alpha | 5′-GGC CAT GAA GCT TTT GAG CAG AGA TAC-3′ | 5′-AGT CAA GGT TGC ACA TGA AAC GTT CCC-3′ |
| LAMP1 | Lysosomal-associated membrane protein 1 | 5′-GGC CGC TGC TCC TGC TGC TGC TGG CAG-3′ | 5′-ATA TCC TCT TCC AAA AGT AAT TGT GAG-3′ |
| LAMP2 | Lysosomal-associated membrane protein 2 | 5′-AGG GTA CTT GCC TTT ATG CAG AAT GGG-3′ | 5′-GTG TCG CCT TGT CAG GTA CTG AAT GG-3′ |
| HIF-1α | Hypoxia inducible factor 1, alpha subunit | 5′-TCC CAT ACA AGG CAG CAG AA-3′ | 5′-GTG CAG TAT TGT AGC CAG GC-3′ |
| TNF-α | Tumor necrosis factor, alpha | 5′-CAG GTT CTG TCC CTT TCA CTC ACT-3′ | 5′-GTT CAG TAG ACA GAA GAG CGT GGT-3′ |
| HEXB | Hexosaminidase B | 5′-CCC GGG CTG CTG CTG CTG CAG GCG CTG-3′ | 5′-GTG GAA TTG GGA CTG TGG TCG ATG CTG-3′ |
| β-ACTIN | Actin, beta | 5′-CGC CAC CAG TTC GCC ATG GA-3′ | 5′- TAC AGC CC GGG GAG CAT CGT-3′ |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Huy, T.X.N.; Nguyen, T.T.; Reyes, A.W.B.; Kim, H.; Min, W.; Lee, H.J.; Lee, J.H.; Kim, S. Cobalt (II) Chloride Regulates the Invasion and Survival of Brucella abortus 544 in RAW 264.7 Cells and B6 Mice. Pathogens 2022, 11, 596. https://doi.org/10.3390/pathogens11050596
Huy TXN, Nguyen TT, Reyes AWB, Kim H, Min W, Lee HJ, Lee JH, Kim S. Cobalt (II) Chloride Regulates the Invasion and Survival of Brucella abortus 544 in RAW 264.7 Cells and B6 Mice. Pathogens. 2022; 11(5):596. https://doi.org/10.3390/pathogens11050596
Chicago/Turabian StyleHuy, Tran X. N., Trang T. Nguyen, Alisha W. B. Reyes, Heejin Kim, WonGi Min, Hu J. Lee, John H. Lee, and Suk Kim. 2022. "Cobalt (II) Chloride Regulates the Invasion and Survival of Brucella abortus 544 in RAW 264.7 Cells and B6 Mice" Pathogens 11, no. 5: 596. https://doi.org/10.3390/pathogens11050596
APA StyleHuy, T. X. N., Nguyen, T. T., Reyes, A. W. B., Kim, H., Min, W., Lee, H. J., Lee, J. H., & Kim, S. (2022). Cobalt (II) Chloride Regulates the Invasion and Survival of Brucella abortus 544 in RAW 264.7 Cells and B6 Mice. Pathogens, 11(5), 596. https://doi.org/10.3390/pathogens11050596








