A Multi-Level Analysis on School Connectedness, Family Support, and Adolescent Depression: Evidence from the National Longitudinal Study of Adolescent Health, 1995–1996
Abstract
1. Introduction
2. Methods
2.1. Data Source
2.2. Measures
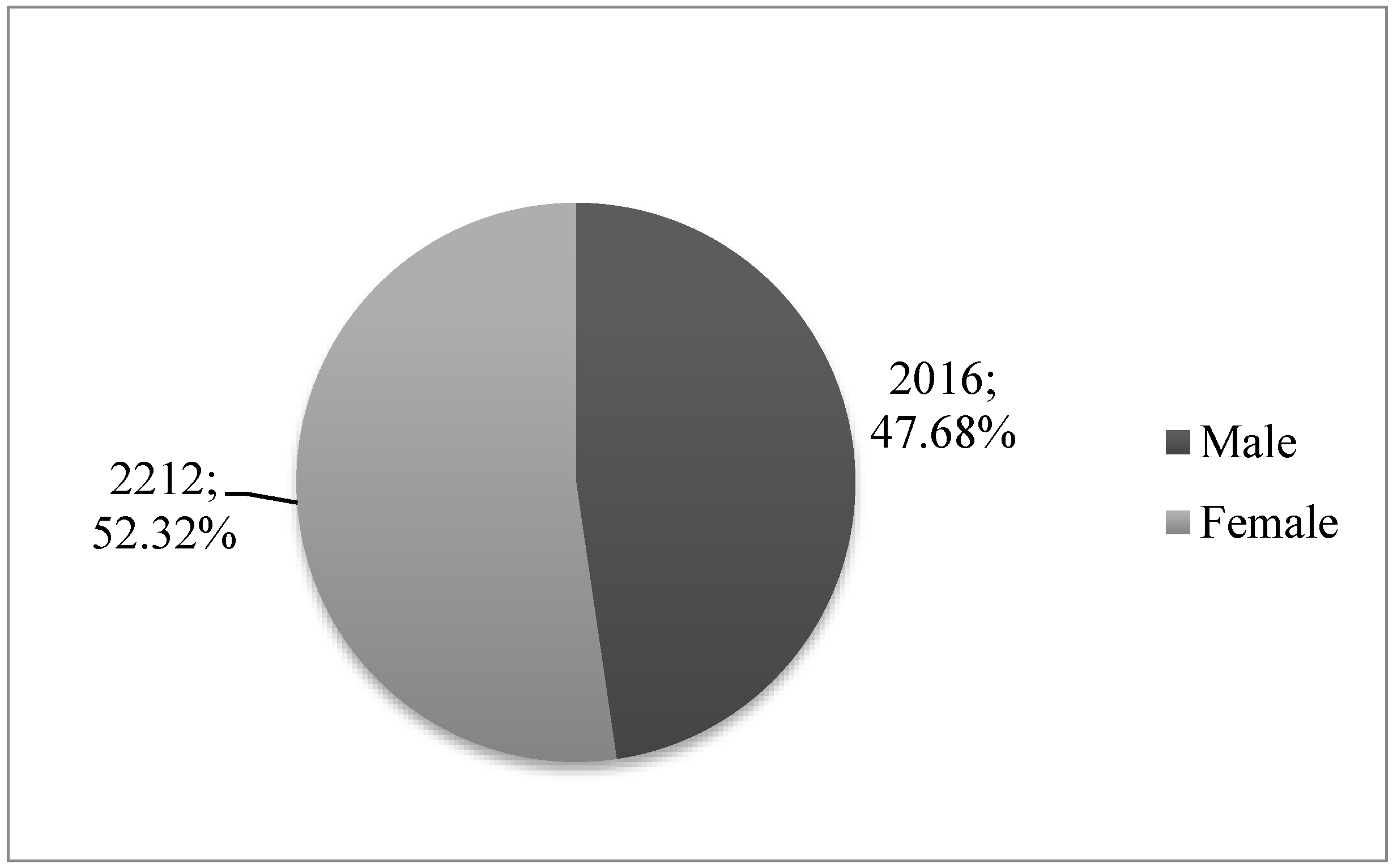
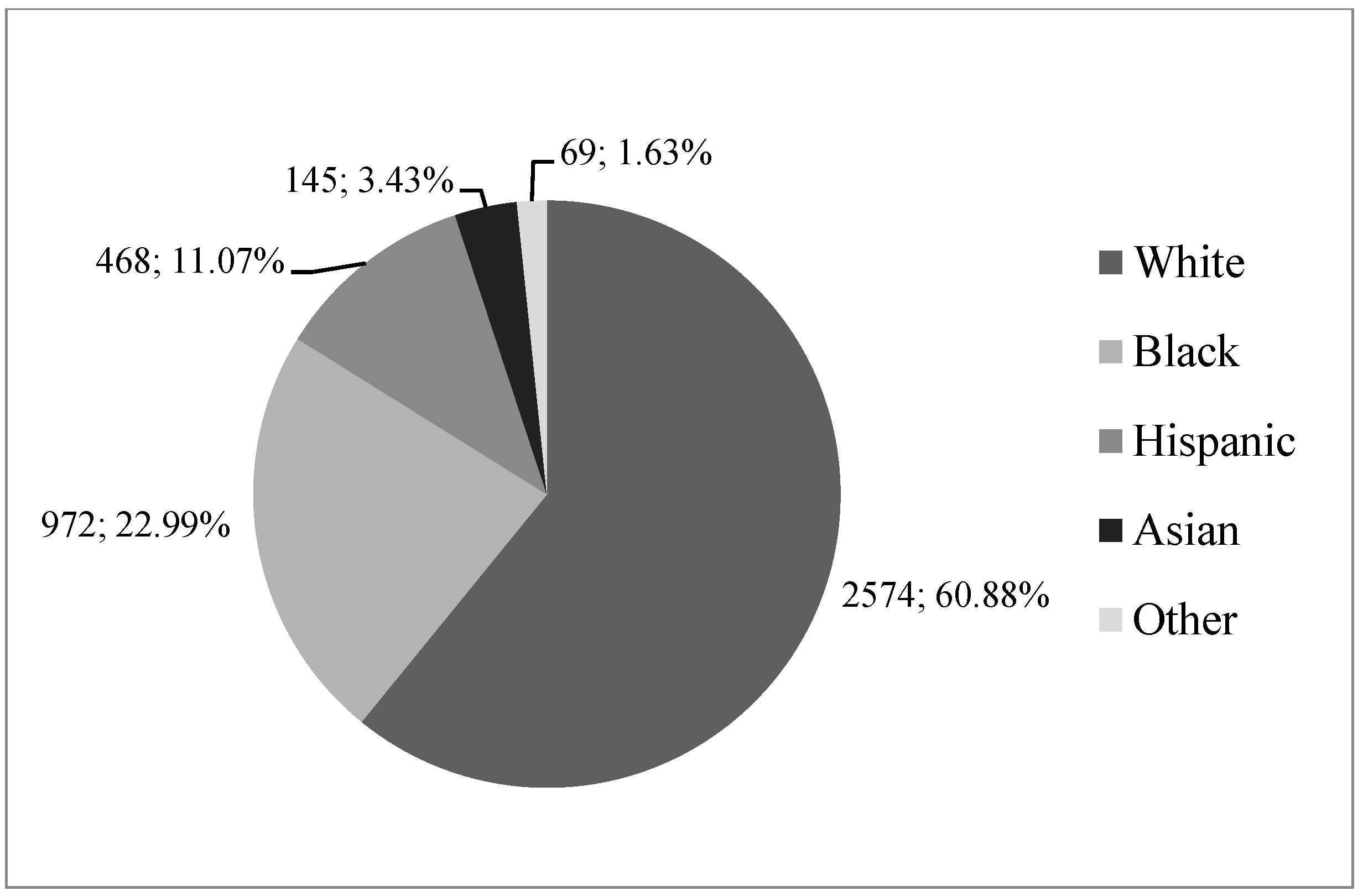
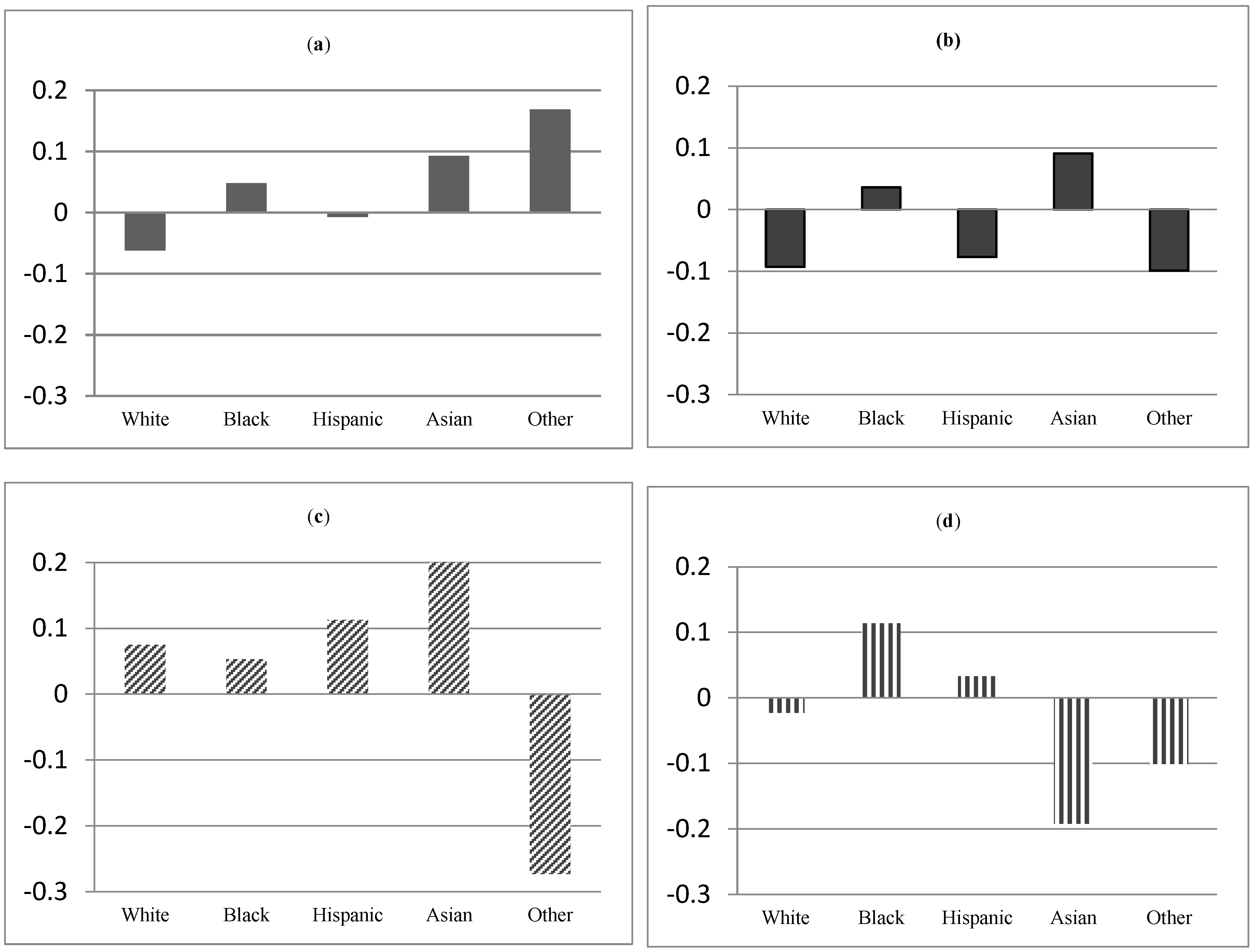
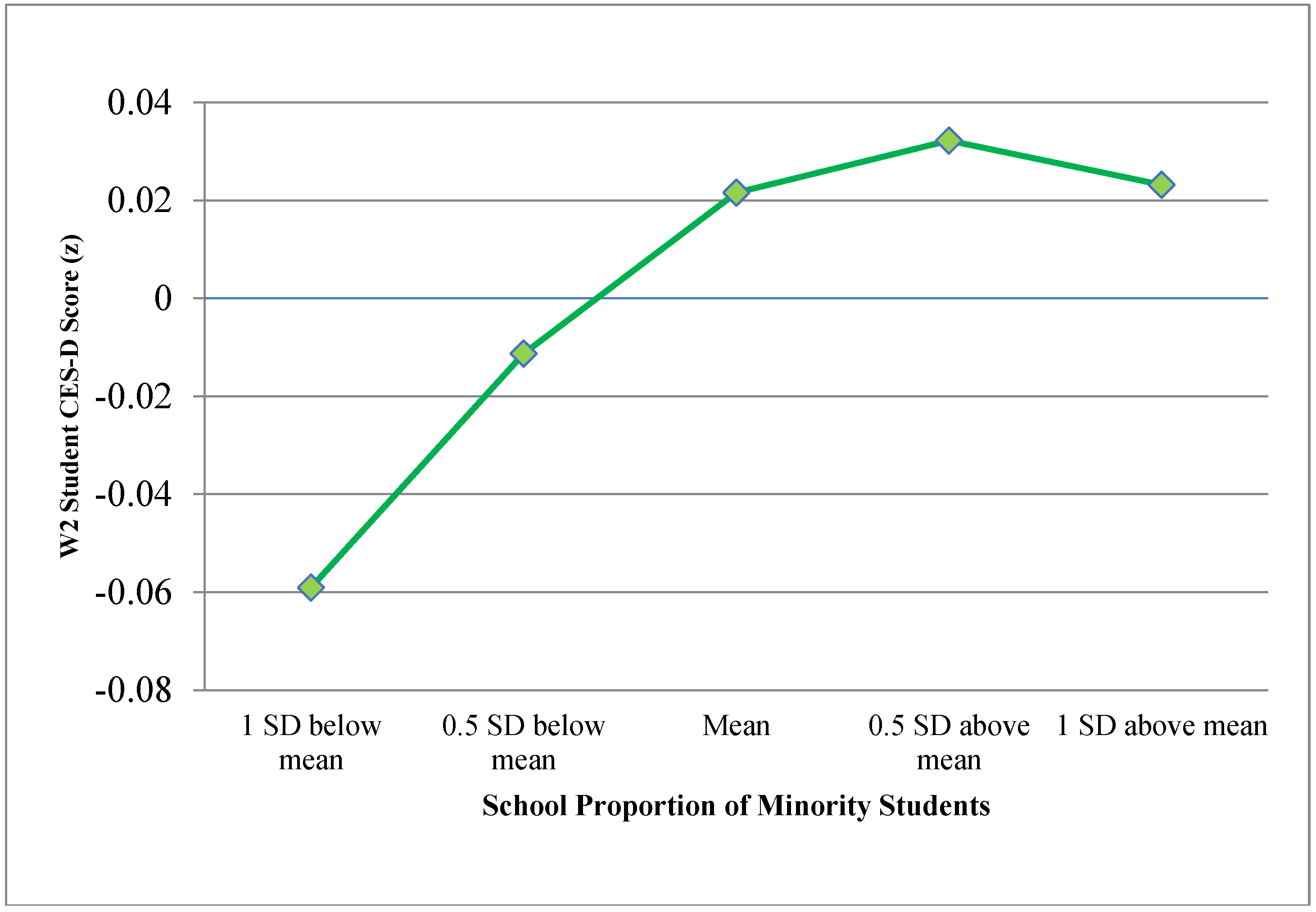
3. Results
4. Discussion
Compliance with Ethical Standards
Funding
Ethical Approval
Informed Consent
Acknowledgment
Conflicts of Interest
Appendix A
| Depressive Symptoms: CES-D Scale | |
| Having trouble falling asleep or staying asleep | |
| Frequency crying | |
| Bothered by things that usually don’t bother you | |
| Didn’t feel like eating, your appetite was poor | |
| Felt that could not shake off the blues, even with help from your family and your friends | |
| Felt that you were not as good as other people | |
| Had trouble keeping your mind on what you were doing | |
| Felt depressed | |
| Felt that you were too tired to do things | |
| Didn’t feel hopeful about the future | |
| Thought your life had been a failure | |
| Felt fearful | |
| Were not happy | |
| Talked less than usual | |
| Felt lonely | |
| People were not friendly to you | |
| Did not enjoy life | |
| Felt sad | |
| Felt that people dislike you | |
| It was hard to get started doing things | |
| Perceived Family Support | |
| Feel that your parents care about you? | |
| Feel that people in your family understand you? | |
| Feel that you want to leave home? | |
| Feel that you and your family have fun together? | |
| Feel that your family pays attention to you? | |
| School Connectedness Scale | |
| Feet close to people at your school | |
| Feel like you are part of your school | |
| Students at your school are not prejudiced | |
| Were happy to be at your school last year | |
| Teachers at your school treated students fairly last year | |
| Feel safe at your school | |
References
- Angley, Meghan, Anna Divney, Urania Magriples, and Trace Kershaw. 2015. Social support, family functioning and parenting competence in adolescent parents. Maternal and Child Health Journal 19: 67–73. [Google Scholar] [CrossRef] [PubMed]
- Avenevoli, Shelli, Joel Swendsen, Jian-Ping He, Marcy Burstein, and Kathleen Ries Merikangas. 2015. Major depression in the National Comorbidity Survey–Adolescent Supplement: Prevalence, correlates, and treatment. Journal of the American Academy of Child & Adolescent Psychiatry 54: 37–44. [Google Scholar] [CrossRef]
- Bennett, David S., Paul J. Ambrosini, Diana Kudes, Claudia Metz, and Harris Rabinovich. 2005. Gender differences in adolescent depression: Do symptoms differ for boys and girls? Journal of Affective Disorders 89: 35–44. [Google Scholar] [CrossRef] [PubMed]
- Blazer, Dan G., Ronald C. Kessler, Katherine A. McGonagle, and Marvin S. Swartz. 1994. The prevalence and distribution of major depression in a national community sample: The National Comorbidity Survey. American Journal of Psychiatry 151: 979–86. [Google Scholar] [CrossRef] [PubMed]
- Bond, Lyndal, Helen Butler, Lyndal Thomas, John Carlin, Sara Glover, Glenn Bowes, and George Patton. 2007. Social and school connectedness in early secondary school as predictors of late teenage substance use, mental health, and academic outcomes. Journal of Adolescent Health 40: 357.e9–357.e18. [Google Scholar] [CrossRef] [PubMed]
- Bowlby, John. 1978. Attachment theory and its therapeutic implications. Adolescent Psychiatry 6: 5–33. [Google Scholar]
- Chantala, Kim, and Joyce Tabor. 1999. National Longitudinal Study of Adolescent Health: Strategies to Perform a Design-Based Analysis Using the Add Health Data. Available online: http://citeseerx.ist.psu.edu/viewdoc/summary?doi=10.1.1.629.5502 (accessed on 24 April 2018).
- Colman, Ian, and Anushka Ataullahjan. 2010. Life course perspectives on the epidemiology of depression. The Canadian Journal of Psychiatry 55: 622–32. [Google Scholar] [CrossRef] [PubMed]
- Costello, Darcé M., Joel Swendsen, Jennifer S. Rose, and Lisa C. Dierker. 2008. Risk and protective factors associated with trajectories of depressed mood from adolescence to early adulthood. Journal of Consulting and Clinical Psychology 76: 173–83. [Google Scholar] [CrossRef] [PubMed]
- Crosnoe, Robert. 2009. Low-income students and the socioeconomic composition of public high schools. American Sociological Review 74: 709–30. [Google Scholar] [CrossRef] [PubMed]
- Diamond, Guy, Jody Russon, and Suzanne Levy. 2016. Attachment-Based Family Therapy: A Review of the Empirical Support. Family Process 55: 595–610. [Google Scholar] [CrossRef] [PubMed]
- Dunn, Valerie, and Ian M. Goodyer. 2006. Longitudinal investigation into childhood-and adolescence-onset depression: Psychiatric outcome in early adulthood. The British Journal of Psychiatry 188: 216–22. [Google Scholar] [CrossRef] [PubMed]
- Eccles, Jacquelynne S., and Robert W. Roeser. 2011. Schools as developmental contexts during adolescence. Journal of Research on Adolescence 21: 225–41. [Google Scholar] [CrossRef]
- Ewing, E. Stephanie Krauthamer, Guy Diamond, and Suzanne Levy. 2015. Attachment-based family therapy for depressed and suicidal adolescents: Theory, clinical model and empirical support. Attachment & Human Development 17: 136–56. [Google Scholar] [CrossRef]
- Fergusson, David M., Joseph M. Boden, and L. John Horwood. 2007. Recurrence of major depression in adolescence and early adulthood, and later mental health, educational and economic outcomes. The British Journal of Psychiatry 191: 335–42. [Google Scholar] [CrossRef] [PubMed]
- Goodenow, Carol. 1993. The psychological sense of school membership among adolescents: Scale development and educational correlates. Psychology in the Schools 30: 79–90. [Google Scholar] [CrossRef]
- Harris, Kathleen Mullan, and J. Richard Udry. 1998. National Longitudinal Study of Adolescent to Adult Health, Public Use Contextual Database, Wave I. Available online: http://www.thearda.com/Archive/Files/Descriptions/ADDHW1C.asp (accessed on 8 April 2018).
- Hyde, Janet Shibley, Amy H. Mezulis, and Lyn Y. Abramson. 2008. The ABCs of depression: Integrating affective, biological, and cognitive models to explain the emergence of the gender difference in depression. Psychological Review 115: 291–313. [Google Scholar] [CrossRef] [PubMed]
- Joyce, Hilary D., and Theresa J. Early. 2014. The impact of school connectedness and teacher support on depressive symptoms in adolescents: A multilevel analysis. Children and Youth Services Review 39: 101–7. [Google Scholar] [CrossRef] [PubMed]
- Kessler, Ronald C., Patricia Berglund, Olga Demler, Robert Jin, Kathleen R. Merikangas, and Ellen E. Walters. 2005. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry 62: 593–602. [Google Scholar] [CrossRef] [PubMed]
- Langille, Donald B., Mark Asbridge, Amber Cragg, and Daniel Rasic. 2015. Associations of school connectedness with adolescent suicidality: Gender differences and the role of risk of depression. The Canadian Journal of Psychiatry 60: 258–67. [Google Scholar] [CrossRef] [PubMed]
- Leavy, Richard L. 1983. Social support and psychological disorder: A review. Journal of Community Psychology 11: 3–21. [Google Scholar] [CrossRef]
- McNeely, Clea A., James M. Nonnemaker, and Robert W. Blum. 2002. Promoting school connectedness: Evidence from the national longitudinal study of adolescent health. Journal of School Health 72: 138–46. [Google Scholar] [CrossRef] [PubMed]
- Millings, Abigail, Rhiannon Buck, Alan Montgomery, Melissa Spears, and Paul Stallard. 2012. School connectedness, peer attachment, and self-esteem as predictors of adolescent depression. Journal of Adolescence 35: 1061–67. [Google Scholar] [CrossRef] [PubMed]
- National Institute of Mental Health. 2017a. Major Depression among Adults. Available online: https://www.nimh.nih.gov/health/statistics/prevalence/major-depression-among-adults.shtml (accessed on 8 June 2017).
- National Institute of Mental Health. 2017b. Major Depression among Adolescents. Available online: https://www.nimh.nih.gov/health/statistics/prevalence/major-depression-among-adolescents.shtml (accessed on 7 June 2017).
- Noller, Patricia, and Victor Callan. 2015. The Adolescent in the Family. Abingdon: Routledge. ISBN 978-1-317-35930-2. [Google Scholar]
- Oldfield, Jeremy, Neil Humphrey, and Judith Hebron. 2016. The role of parental and peer attachment relationships and school connectedness in predicting adolescent mental health outcomes. Child and Adolescent Mental Health 21: 21–29. [Google Scholar] [CrossRef]
- Oldfield, Jeremy, Andrew Stevenson, Emily Ortiz, and Bethany Haley. 2018. Promoting or suppressing resilience to mental health outcomes in at risk young people: The role of parental and peer attachment and school connectedness. Journal of Adolescence 64: 13–22. [Google Scholar] [CrossRef] [PubMed]
- Patten, Christi A., J. Christian Gillin, Arthur J. Farkas, Elizabeth A. Gilpin, Charles C. Berry, and John P. Pierce. 1997. Depressive symptoms in California adolescents: Family structure and parental support. Journal of Adolescent Health 20: 271–78. [Google Scholar] [CrossRef]
- Pedersen, Willy. 1994. Parental relations, mental health, and delinquency in adolescents. Adolescence 29: 975–90. [Google Scholar] [PubMed]
- Petersen, Anne C., Pamela A. Sarigiani, and Robert E. Kennedy. 1991. Adolescent depression: Why more girls? Journal of Youth and Adolescence 20: 247–71. [Google Scholar] [CrossRef] [PubMed]
- Ross, Catherine E., and John Mirowsky. 2006. Sex differences in the effect of education on depression: Resource multiplication or resource substitution? Social Science & Medicine 63: 1400–13. [Google Scholar] [CrossRef]
- Ross, Catherine E., John Mirowsky, and Karen Goldsteen. 1990. The impact of the family on health: The decade in review. Journal of Marriage and Family 52: 1059. [Google Scholar] [CrossRef]
- Saluja, Gitanjali, Ronaldo Iachan, Peter C. Scheidt, Mary D. Overpeck, Wenyu Sun, and Jay N. Giedd. 2004. Prevalence of and risk factors for depressive symptoms among young adolescents. Archives of Pediatrics & Adolescent Medicine 158: 760–65. [Google Scholar] [CrossRef]
- Sander, Janay B., and Carolyn A. McCarty. 2005. Youth depression in the family context: Familial risk factors and models of treatment. Clinical Child and Family Psychology Review 8: 203–19. [Google Scholar] [CrossRef] [PubMed]
- Sheeber, Lisa, Hyman Hops, Anthony Alpert, Betsy Davis, and Judy Andrews. 1997. Family support and conflict: Prospective relations to adolescent depression. Journal of abnormal child psychology 25: 333–44. [Google Scholar] [CrossRef] [PubMed]
- Shochet, Ian M., and Coral L. Smith. 2014. A prospective study investigating the links among classroom environment, school connectedness, and depressive symptoms in adolescents. Psychology in the Schools 51: 480–92. [Google Scholar] [CrossRef]
- Shochet, Ian M., Mark R. Dadds, David Ham, and Roslyn Montague. 2006. School connectedness is an underemphasized parameter in adolescent mental health: Results of a community prediction study. Journal of Clinical Child & Adolescent Psychology 35: 170–79. [Google Scholar] [CrossRef]
- Shochet, Ian M., Ross Homel, Wendell D. Cockshaw, and Danielle T. Montgomery. 2008. How do school connectedness and attachment to parents interrelate in predicting adolescent depressive symptoms? Journal of Clinical Child & Adolescent Psychology 37: 676–81. [Google Scholar]
- Walsemann, Katrina M., Bethany A. Bell, and Debeshi Maitra. 2011. The intersection of school racial composition and student race/ethnicity on adolescent depressive and somatic symptoms. Social Science & Medicine 72: 1873–83. [Google Scholar] [CrossRef][Green Version]
- World Health Organization. 2017. Depression and Other Common Mental Disorders: Global Health Estimates. Geneva: World Health Organization. [Google Scholar]
- Zahn-Waxler, Carolyn, Elizabeth A. Shirtcliff, and Kristine Marceau. 2008. Disorders of childhood and adolescence: Gender and psychopathology. Annual Review of Clinical Psychology 4: 275–303. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Yanhua, and Guoxiang Zhao. 2015. Emotion regulation and depressive symptoms: Examining the mediation effects of school connectedness in Chinese late adolescents. Journal of Adolescence 40: 14–23. [Google Scholar] [CrossRef] [PubMed]
- Zhu, Lin. 2017. Depression Risks and Correlates among Different Generations of Chinese Americans: The Effects of Relationships with Friends and Relatives. Social Sciences 6: 56. [Google Scholar] [CrossRef]
- Zhu, Lin. 2018. Depression Symptom Patterns and Social Correlates among Chinese Americans. Brain Sciences 8: 16. [Google Scholar] [CrossRef] [PubMed]
| 1 | Respondents who identified with multiple racial/ethnic groups were able to mark more than one answer in the survey. However, they were placed in a primary racial/ethnic category. Those who chose “Hispanic” were designated as Hispanic and eliminated from any other race categories; those who chose “black or African American” and other race were designated as black or African American, and eliminated from the other categories. The process was repeated for the other racial/ethnic categories in the following order: Asian, Native American, other, and white. In this study, Native Americans and other races were combined, because of the limited sample size. |
| 2 | I tested the interaction between W1 family support and race/ethnicity, the results of which not presented. The interaction terms are not significant, and the coefficients of other variables are the same as those in Model 3. |
| 3 | School-level proportion of minority students are grand-mean centered when entered into the models. The mean is −0.012, while the standard deviation is 0.176. Therefore, the proportion of minority students of the five schools presented in the figure are, from lowest to highest: −0.344, −0.188, −0.012, 0.164, and 0.319. |
| 4 |

| N | Mean | Min | Max | S.D. | |
|---|---|---|---|---|---|
| Dependent variable | |||||
| W2 CES-D score (z) | 4228 | −0.02 | −2.96 | 5.07 | 0.97 |
| Student-Level Predictors | |||||
| W1 Age | 4228 | 14.47 | 11 | 20 | 1.52 |
| W1 CES-D (z) | 4228 | −0.06 | −2.87 | 5.70 | 0.94 |
| W1 School connectedness (z) | 4228 | 0.07 | −3.64 | 2.02 | 0.97 |
| W1 Family support (z) | 4228 | 0.01 | −5.25 | 2.66 | 0.96 |
| School-Level Predictors | |||||
| School mean connectedness (z) | 132 | 0.02 | −0.62 | 0.76 | 0.32 |
| Prop. of minority | 132 | 0.39 | 0 | 1 | 0.33 |
| Coefficient (s.e.) | Model 1 | Model 2 | Model 3 |
|---|---|---|---|
| Student-level predictors | |||
| W1 CES-D score (z) | 0.477 *** (0.020) | 0.465 *** (0.020) | 0.465 *** (0.020) |
| Female | 0.230 *** (0.029) | 0.231 *** (0.029) | 0.232 *** (0.029) |
| Age | 0.020 (0.012) | 0.017 (0.013) | 0.016 (0.013) |
| W1 Family support (z) | −0.061 *** (0.018) | −0.048 * (0.019) | −0.049 ** (0.019) |
| W1 School connectedness (z) | −0.056 ** (0.019) | −0.054 ** (0.021) | |
| Race/ethnicity | |||
| White | Omitted | Omitted | Omitted |
| Black | 0.079 * (0.036) | 0.079 * (0.035) | 0.078 * (0.036) |
| Hispanic | 0.086 (0.058) | 0.089 (0.058) | 0.084 (0.060) |
| Asian | 0.058 (0.064) | 0.075 (0.063) | 0.105 † (0.064) |
| Other | 0.183 (0.121) | 0.175 (0.122) | 0.180 (0.124) |
| Intercept | −0.024 (0.016) | −0.021 (0.016) | −0.021 (0.016) |
| Intra-class interaction term | |||
| W1 School connectedness (z) × Black | 0.046 (0.057) | ||
| W1 School connectedness (z) × Hispanic | 0.048 (0.060) | ||
| W1 School connectedness (z) × Asian | −0.105 (0.077) | ||
| W1 School connectedness (z) × Other | 0.056 (0.118) | ||
| Model 4 | Model 5 | |
|---|---|---|
| Student-level predictors | ||
| W1 CES-D score | 0.463 *** (0.019) | 0.461 *** (0.019) |
| Female a | 0.232 *** (0.029) | 0.235 *** (0.028) |
| Age a | 0.022 (0.013) | 0.022 † (0.013) |
| W1 Family support (z) a | −0.048 * (0.019) | −0.047 ** (0.019) |
| W1 School connectedness (z) a | −0.062 *** (0.019) | −0.063 *** (0.018) |
| Race/ethnicity | ||
| White | Omitted | Omitted |
| Black b | 0.116 * (0.053) | 0.045 (0.064) |
| Hispanic b | 0.104 (0.068) | 0.035 (0.074) |
| Asian b | 0.087 (0.086) | 0.007 (0.124) |
| Other b | 0.175 (0.127) | 0.399 † (0.226) |
| School-level predictors | ||
| Intercept | 0.023 (0.029) | 0.020 (0.028) |
| School mean connectedness a | 0.094 † (0.055) | 0.096 † (0.055) |
| Prop. minority a | 0.115 * (0.055) | 0.119 * (0.054) |
| Prop. minority squared a | −0.359 † (0.215) | −0.328 (0.210) |
| Cross-level interaction terms | ||
| Black × Prop. minority | 0.087 (0.281) | |
| Black × Prop. minority squared | 0.709 (0.752) | |
| Hispanic × Prop. minority | −0.693 † (0.415) | |
| Hispanic × Prop. minority squared | 1.774 † (1.052) | |
| Asian × Prop. minority | 0.256 (0.466) | |
| Asian × Prop. minority squared | 0.470 (1.272) | |
| Other × Prop. minority | 1.202 * (0.541) | |
| Other × Prop. minority squared | −3.592 (0.057) |
© 2018 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhu, L. A Multi-Level Analysis on School Connectedness, Family Support, and Adolescent Depression: Evidence from the National Longitudinal Study of Adolescent Health, 1995–1996. Soc. Sci. 2018, 7, 72. https://doi.org/10.3390/socsci7050072
Zhu L. A Multi-Level Analysis on School Connectedness, Family Support, and Adolescent Depression: Evidence from the National Longitudinal Study of Adolescent Health, 1995–1996. Social Sciences. 2018; 7(5):72. https://doi.org/10.3390/socsci7050072
Chicago/Turabian StyleZhu, Lin. 2018. "A Multi-Level Analysis on School Connectedness, Family Support, and Adolescent Depression: Evidence from the National Longitudinal Study of Adolescent Health, 1995–1996" Social Sciences 7, no. 5: 72. https://doi.org/10.3390/socsci7050072
APA StyleZhu, L. (2018). A Multi-Level Analysis on School Connectedness, Family Support, and Adolescent Depression: Evidence from the National Longitudinal Study of Adolescent Health, 1995–1996. Social Sciences, 7(5), 72. https://doi.org/10.3390/socsci7050072





