Analysis of Unmarried Adolescents and Modern Contraceptives Initiation in Nigeria: Evidence from 2018 NDHS
Abstract
:1. Introduction
Theoretical Framework
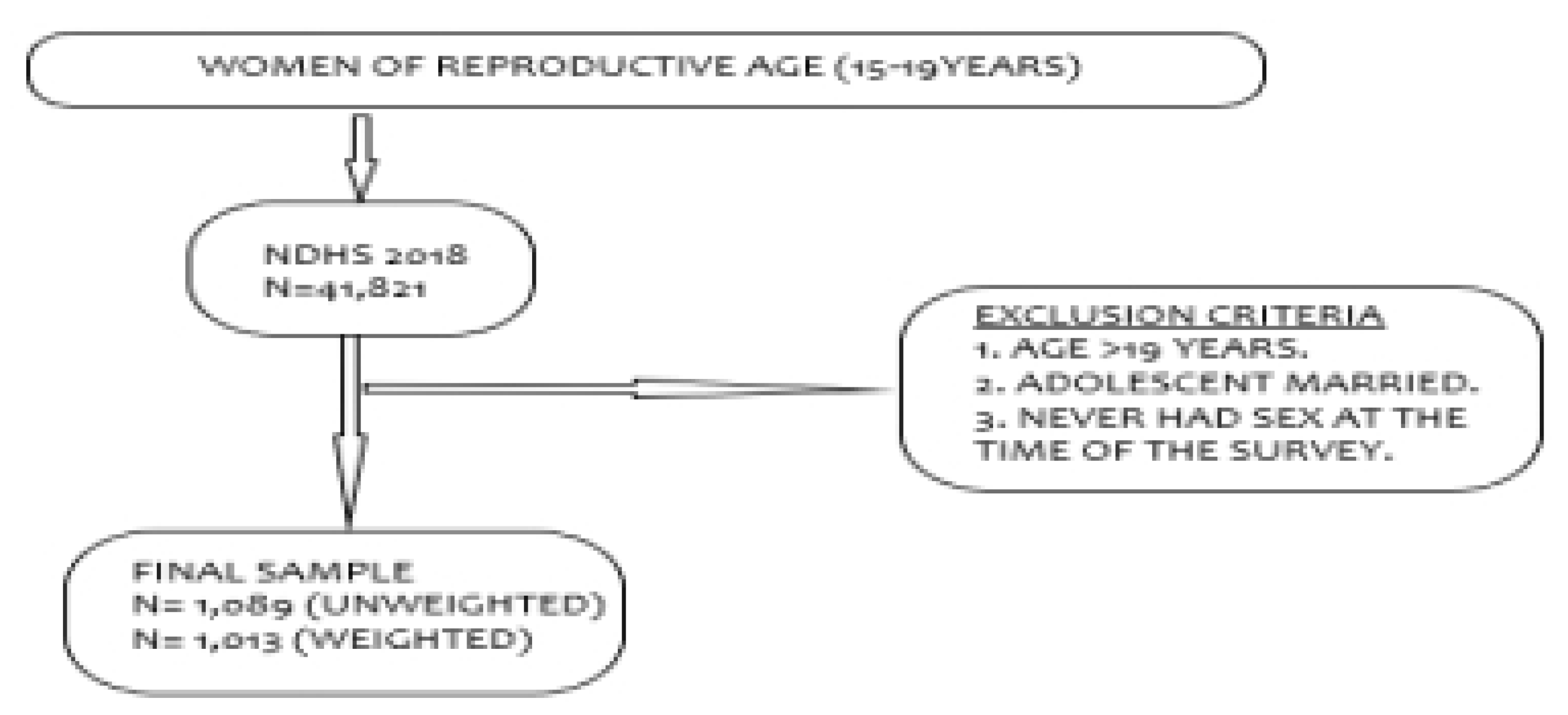
2. Data and Method
2.1. Study Variables
2.2. Data Management and Analysis
3. Findings
3.1. Description of the Respondents:
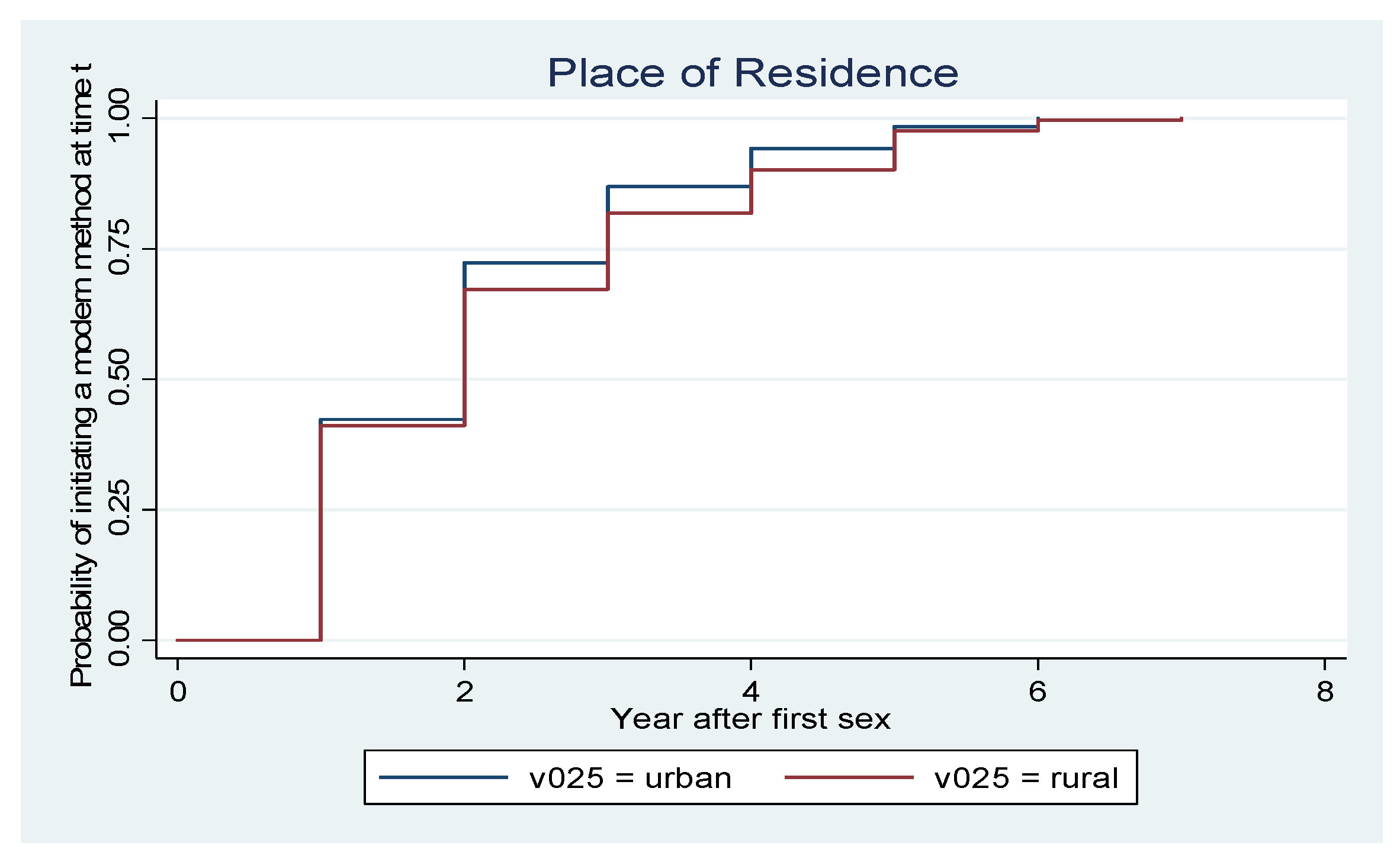
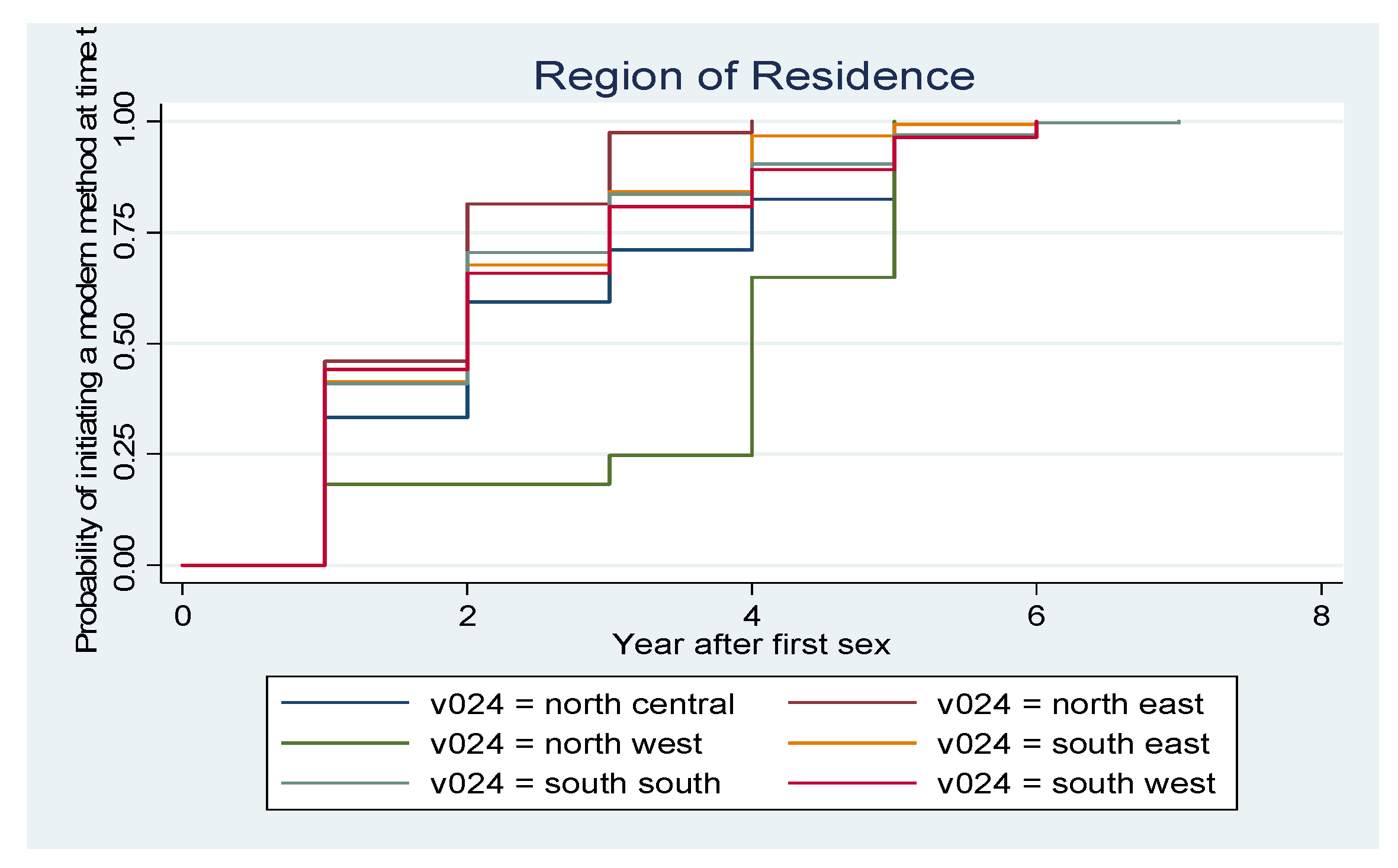
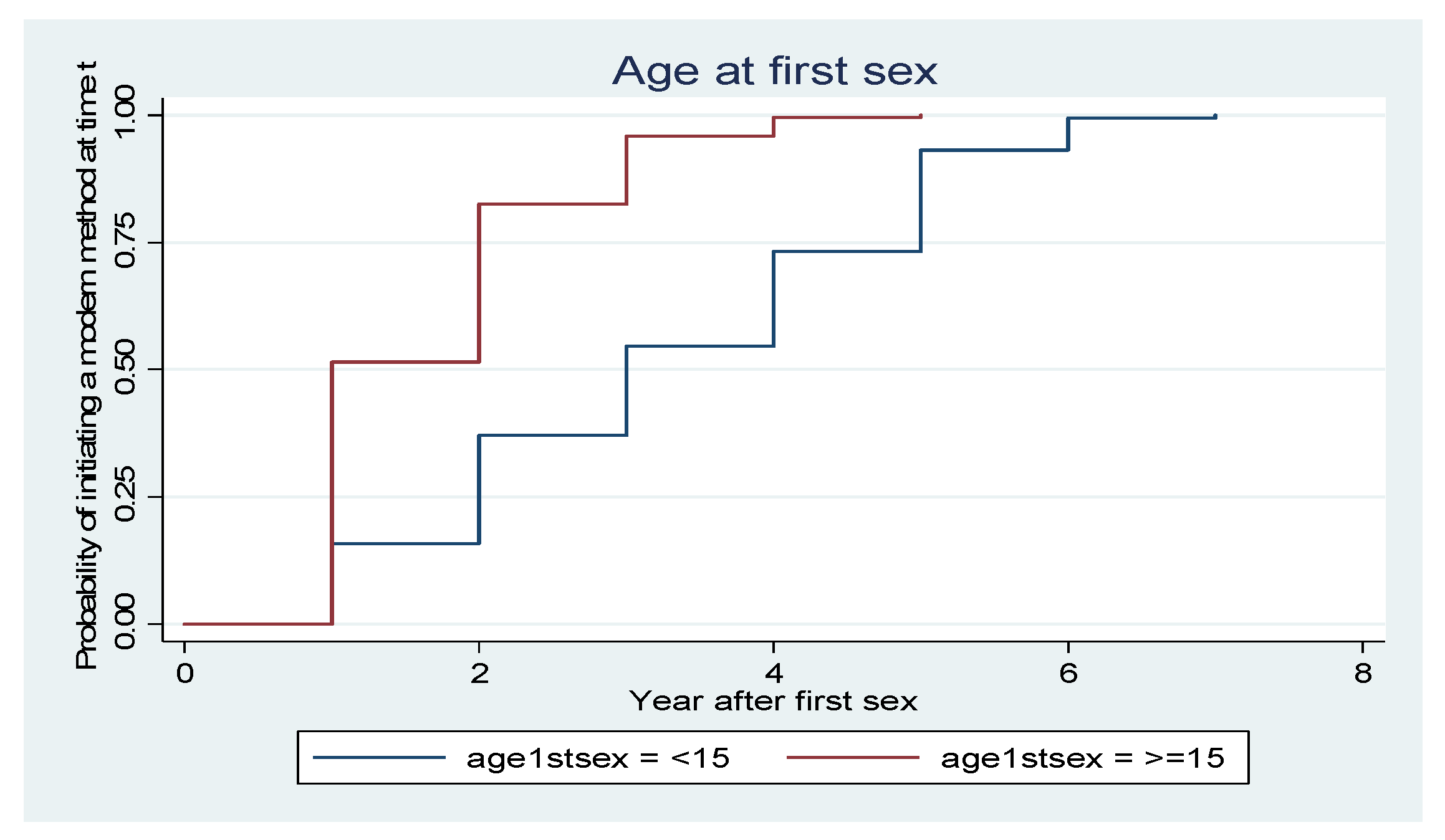
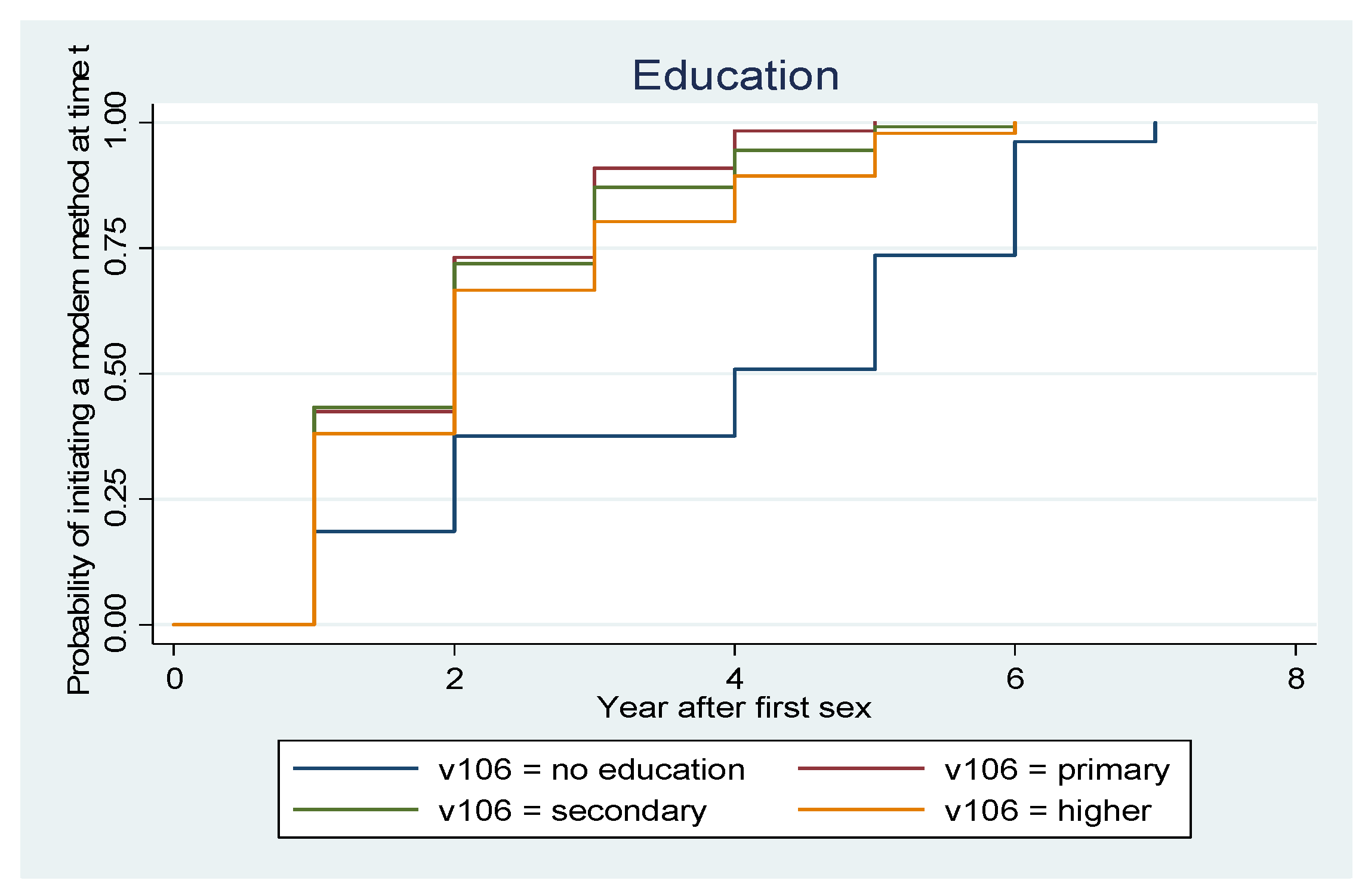
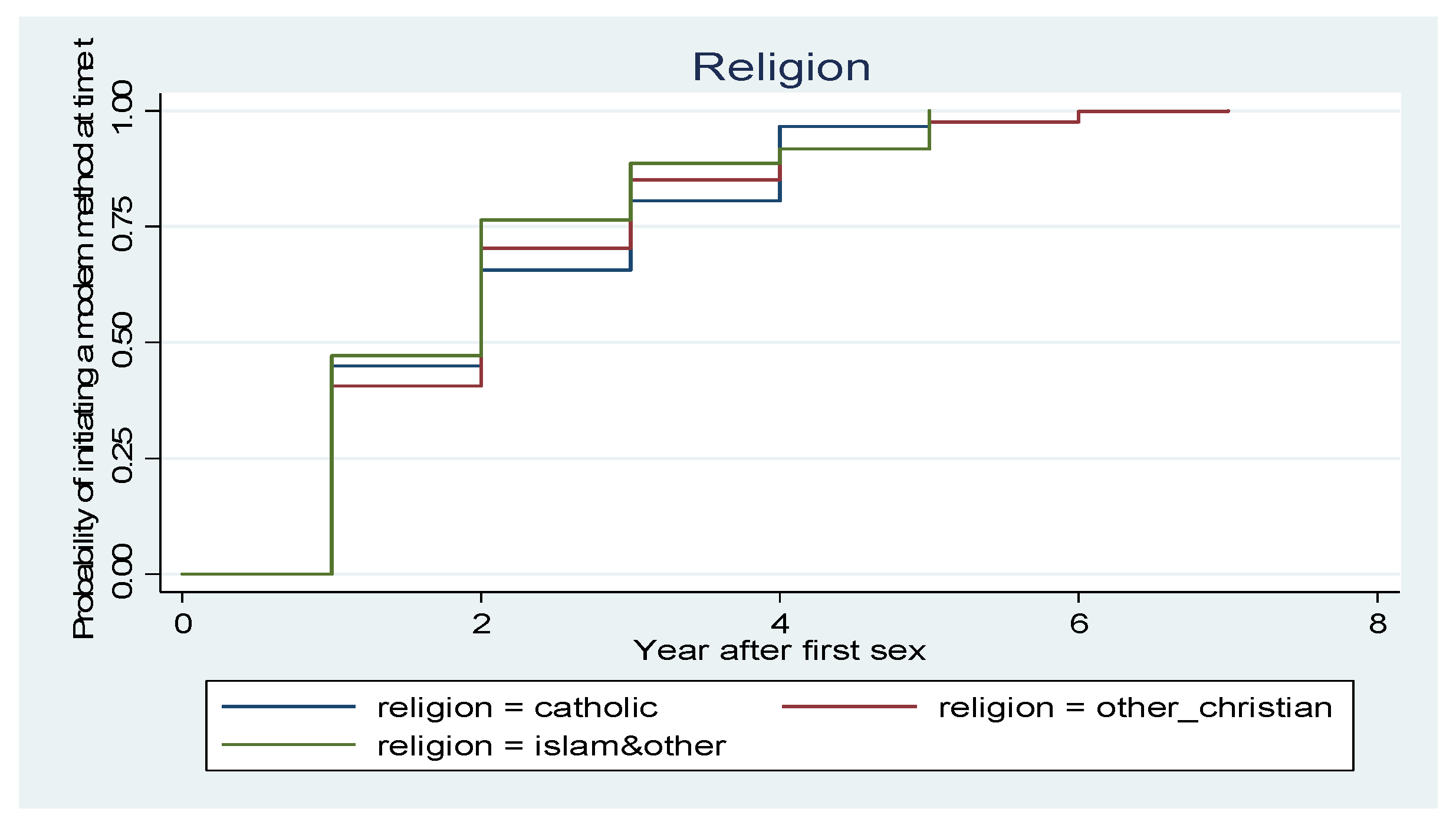
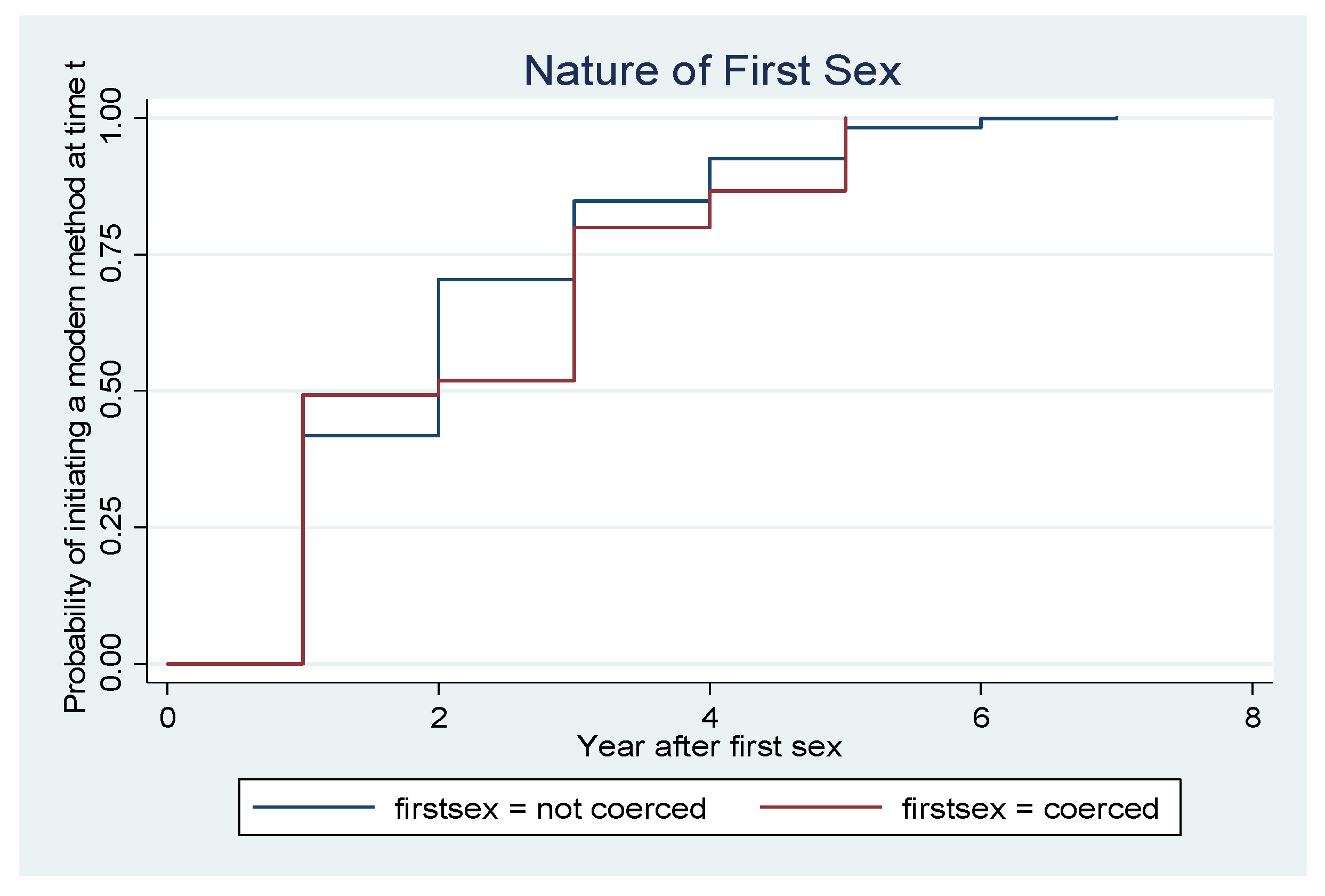
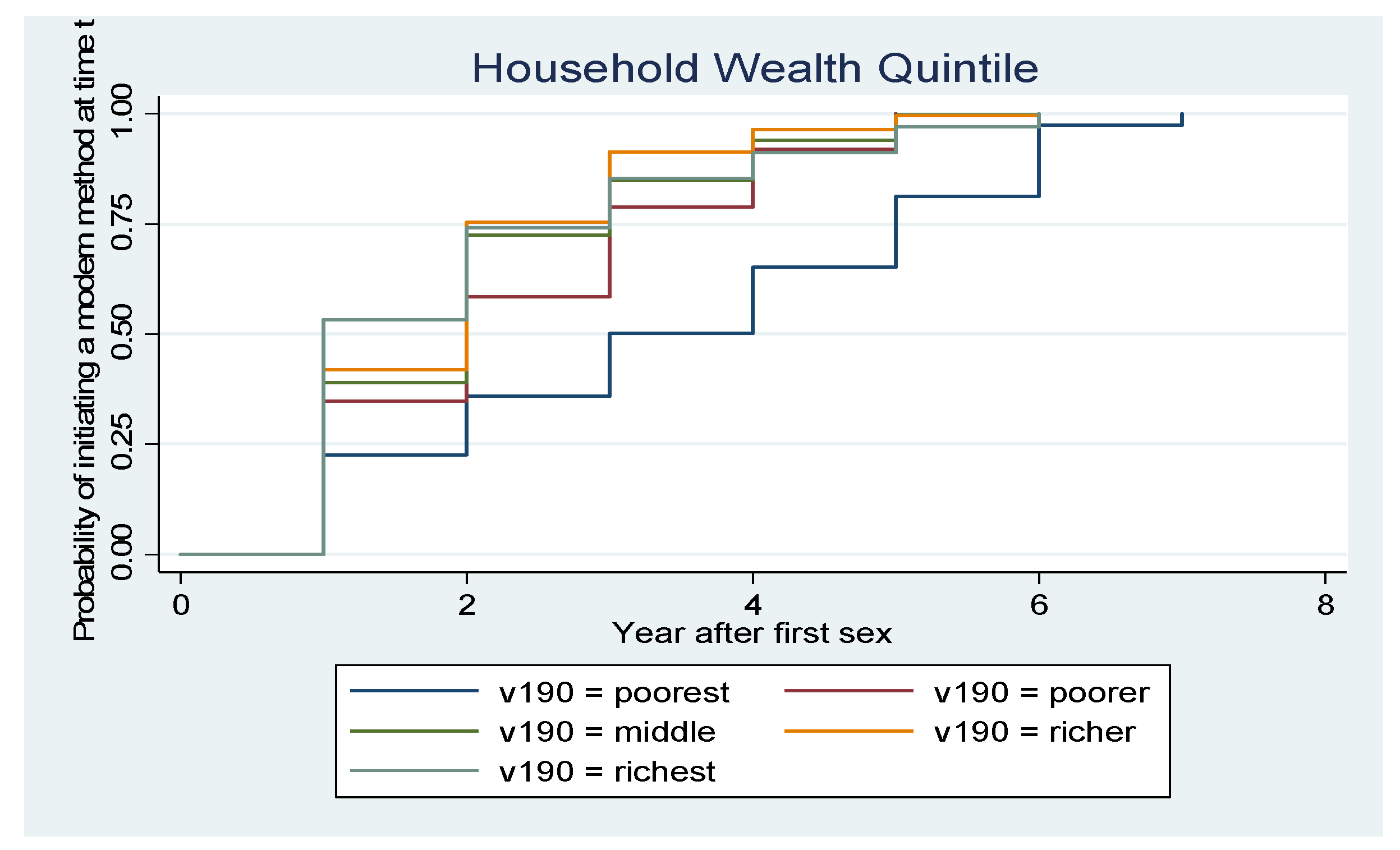
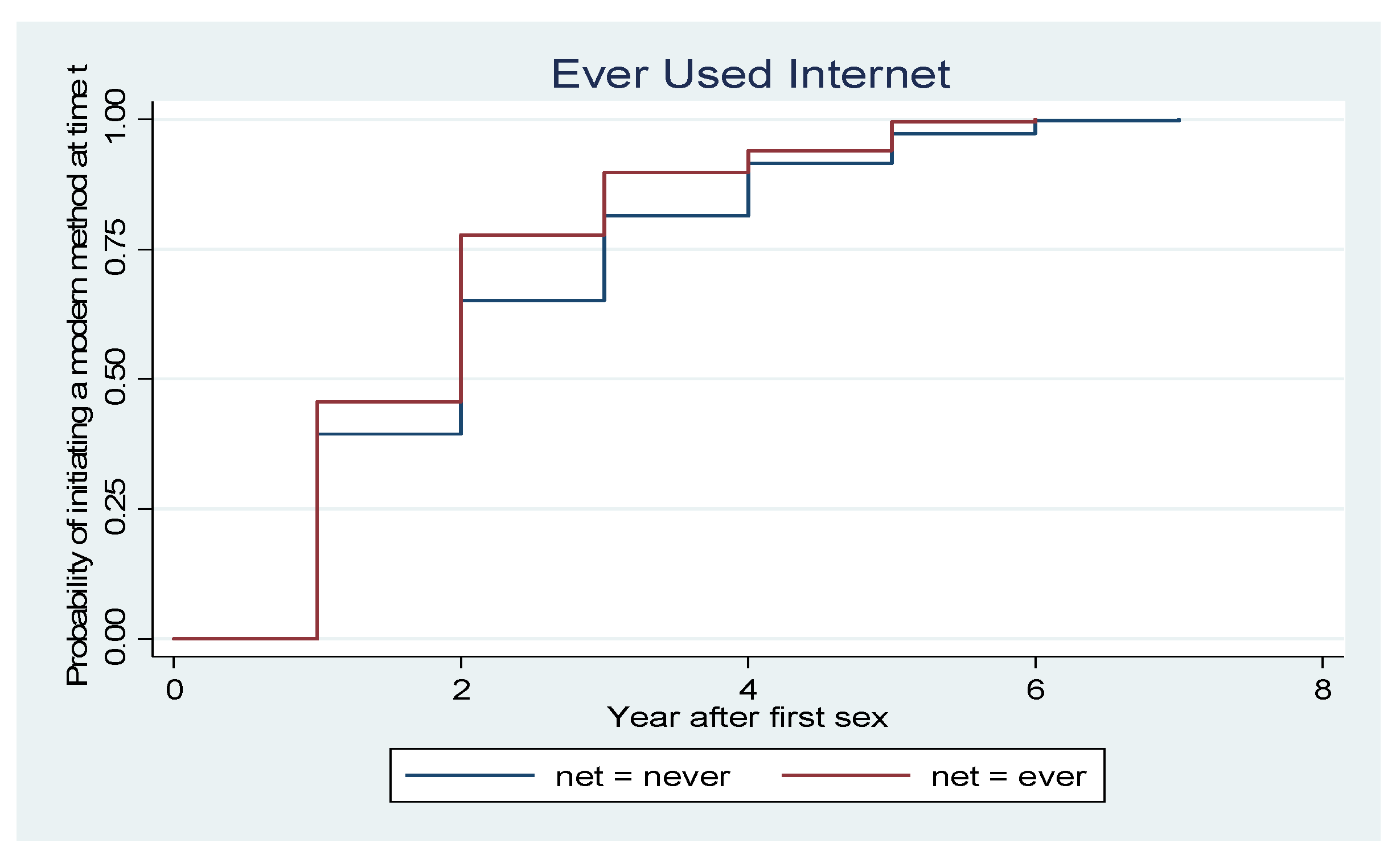
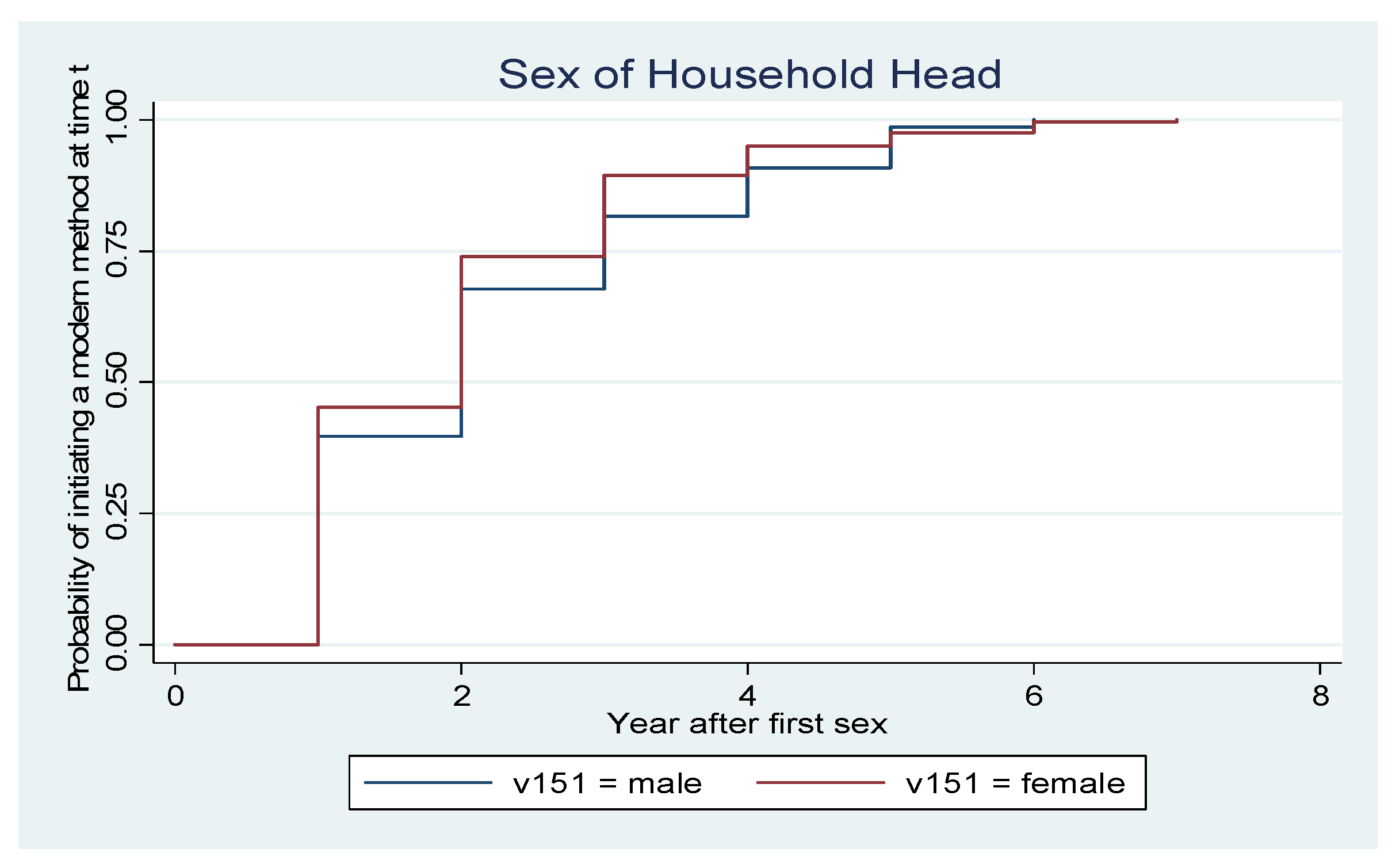
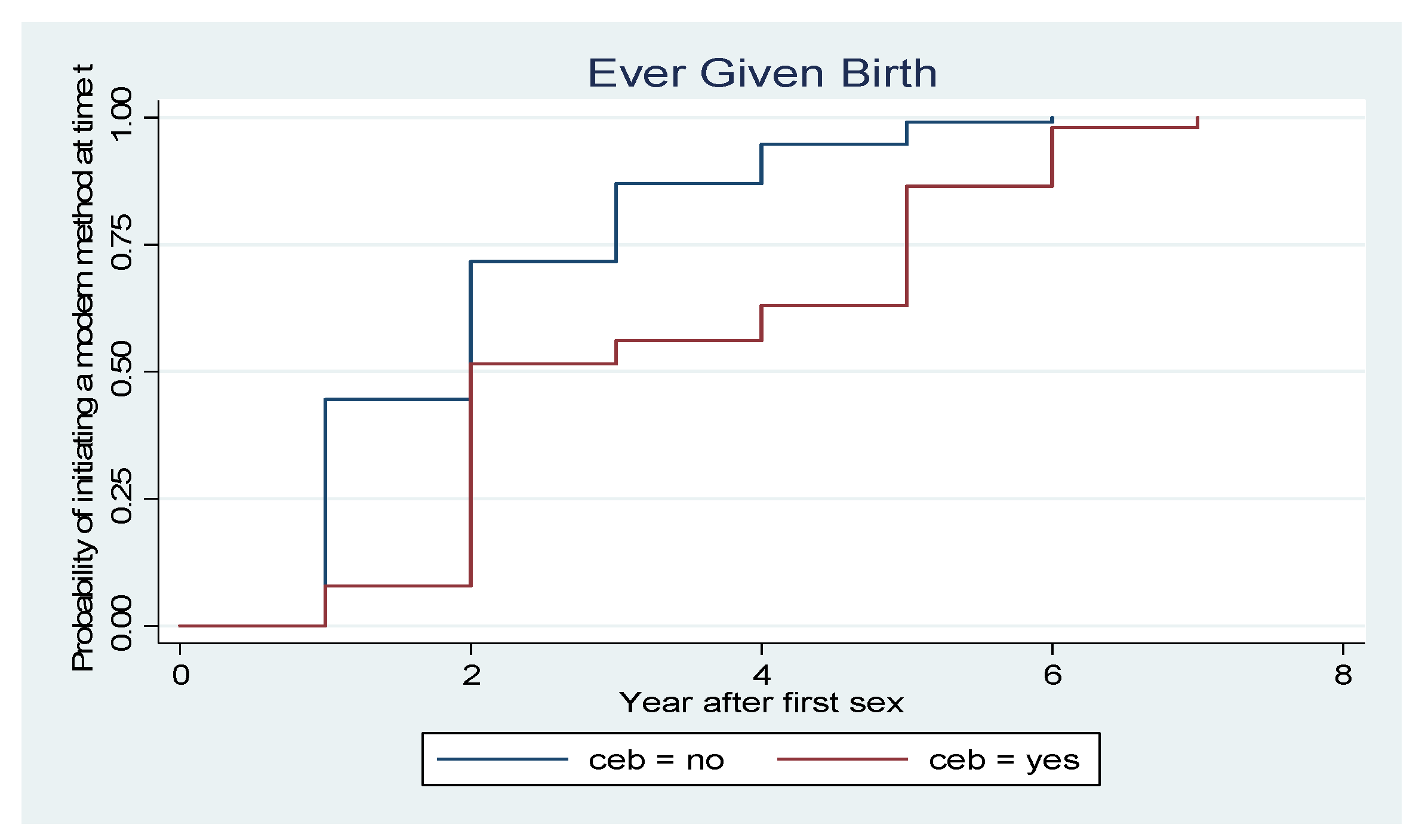
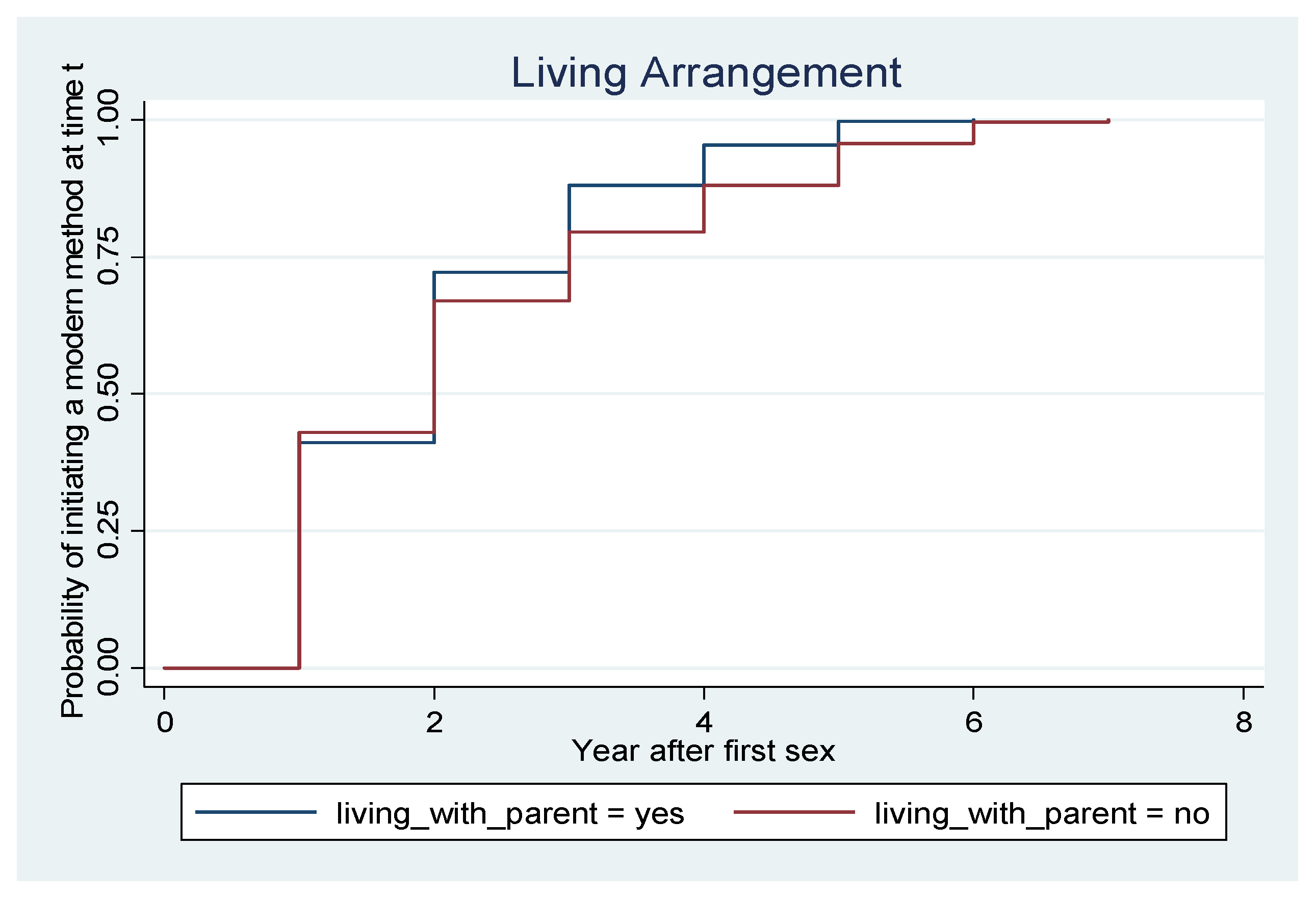
3.2. Timing of Initiation of a Modern Method of Contraception by Socio-Demographic Characteristics of Respondents
3.3. Incidence Rate and Risk Factors of Modern Contraceptive Uptake among Sexually Active Unmarried Adolescents Aged 15–19 Years in Nigeria
4. Discussions
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Abebe, Haftom Temesgen, Abate Bekelle Belachew, Letekirstos Gebreegziabher Gebretsadik, Yodit Zewdie Berhe, Haftu Berhe Gebru, Alemayohu Bayray Kahsay, and Atkilt Girma Gebrekidan. 2020. Contraceptive use and its determinants among adolescent women in Tigray, Ethiopia: A multilevel modeling. International Journal of Adolescent Medicine and Health. [Google Scholar] [CrossRef] [PubMed]
- Adedini, Sunday A., Stella Babalola, Charity Ibeawuchi, Olukunle Omotoso, Akinsewa Kiode, and Mojisola Odeku. 2018. Role of Religious Leaders in Promoting Contraceptive Use in Nigeria: Evidence From the Nigerian Urban Reproductive Health Initiative. Global Health, Science and Practice 6: 500–14. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Agyemang, Joyce, Newton Sam, Nkrumah Isaac, Tsoka-Gwegweni Joyce-Mahlako, and Cumber Samuel Nabile. 2019. Contraceptive use and associated factors among sexually active female adolescents in Atwima Kwanwoma District, Ashanti region-Ghana. Pan African Medical Journal 12: 182. [Google Scholar] [CrossRef] [PubMed]
- Ahinkorah, Bright Opoku. 2020. Predictors of modern contraceptive use among adolescent girls and young women in sub-Saharan Africa: A mixed effects multilevel analysis of data from 29 demographic and health surveys. Contracept Reprod Medicine 5: 32. [Google Scholar] [CrossRef]
- Appiah, Francis, Abdul-Aziz Seidu, Bright Opoku Ahinkorah, Linus Baatiema, and Edward Kwabena Ameyaw. 2020. Trends and determinants of contraceptive use among female adolescents in Ghana: Analysis of 2003–14 Demographic and Health Surveys. SSM—Population Health 10: 100554. [Google Scholar] [CrossRef] [PubMed]
- Bearak, Jonathan, Anna Popinchalk, Leontine Alkema, and Gilda Sedgh. 2018. Global, regional, and subregional trends in unintended pregnancy and its outcomes from 1990 to 2014: Estimates from a Bayesian hierarchical model. The Lancet Global Health 6: e380–e389. [Google Scholar] [CrossRef] [Green Version]
- Casey, Sara E., Meghan C. Gallagher, Jessica Kakesa, Anushka Kalyanpur, Jean-Baptiste Muselemu, Raoza Vololona Rafanoharana, and Nathaly Spilotros. 2020. Contraceptive use among adolescent and young women in North and South Kivu, Democratic Republic of the Congo: A cross-sectional population-based survey. PLoS Medicine 17: e1003086. [Google Scholar] [CrossRef]
- Cavazos-Rehg, Patricia A., Melissa J. Krauss, Edward L. Spitznagel, Mario Schootman, Jeffrey F. Peipert, Linda B. Cottler, and Laura Jean Bierut. 2010. Type of contraception method used at last intercourse and associations with health risk behaviors among US adolescents. Contraception 82: 549–55. [Google Scholar] [CrossRef] [Green Version]
- Chola, Mumbi, Khumbulani Hlongwana, and Themba G. Ginindza. 2020. Patterns, trends, and factors associated with contraceptive use among adolescent girls in Zambia (1996 to 2014): A multilevel analysis. BMC Women’s Health 20: 185. [Google Scholar] [CrossRef]
- Croft, Trevo, Sarah Bradley, and Courtney Allen. 2018. DHS Contraceptive Calendar Tutorial; Rockville. Available online: https://www.dhsprogram.com/data/calendar-tutorial/ (accessed on 20 July 2017).
- Cheedalla, Aneesha, Caroline Moreau, and Anne E. Burke. 2020. Sex education and contraceptive use of adolescent and young adult females in the United States: An analysis of the National Survey of Family Growth 2011–2017. Contracept X 20: 100048. [Google Scholar] [CrossRef]
- Darroch, Jacqueline E., Vanessa Woog, Akinrinola Bankole, and Lori S. Ashford. 2016. Costs and Benefits of Meeting the Contraceptive Needs of Adolescents. New York: Guttmacher Institute. [Google Scholar]
- Essiben, Félix, Pierre Marie Tebeu, Arielle Lando, Charlotte Tchente Nguefack, Rostand Njiki Dounou, and Robinson Mbu Enow. 2018. Evaluation of the Offer of Family Planning Services in a Rural Area of The Bamboutos Division in the West Region of Cameroon: A Cross Sectional Study. Health Sciences and Disease 19. Available online: https://www.hsd-fmsb.org/index.php/hsd/article/view/931?articlesBySameAuthorPage=2 (accessed on 14 March 2022).
- Exavery, Amon, Almany Malick Kanté, Mustafa Njozi, Kassimu Tani, Henry V. Doctor, Ahmed Hingora, and James F. Phillips. 2014. Predictors of mistimed, and unwanted pregnancies among women of childbearing age in Rufiji, Kilombero, and Ulanga districts of Tanzania. Reproductive Health 11: 1–9. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fagbamigbe, Adeniyi. 2021. How soon does modern contraceptive use starts after sexual debut in Africa? Survival analysis of timing and associated factors among never-in-union women. Scientific African 11: e00719. [Google Scholar] [CrossRef]
- Fagbamigbe, Adeniyi, Rotimi Afolabi, and Erhabor Idemudia. 2018. Demand and unmet needs of contraception among sexually active in-union women in Nigeria: Distribution, associated characteristics, barriers, and program implications. Sage Open 8: 2158244017754023. [Google Scholar] [CrossRef] [Green Version]
- Finer, Lawrence B., and Jesse M. Philbin. 2013. Sexual initiation, contraceptive use, and pregnancy among young adolescents. Pediatrics 131: 886–91. [Google Scholar] [CrossRef] [Green Version]
- Hounton, Sennen, Aluisio J. Barros, Agbessi Amouzou, Solomon Shiferaw, Abdoulaye Maïga, Akanni Akinyemi, Howard Friedman, and Desmond Koroma. 2015. Patterns and trends of contraceptive use among sexually active adolescents in Burkina Faso, Ethiopia, and Nigeria: Evidence from cross-sectional studies. Global Health Action 8: 29737. [Google Scholar] [CrossRef]
- Inchley, Jo, and Dorothy Currie. 2016. Growing Up Unequal: Gender and Socioeconomic Differences in Young People’s Health and Well-Being. Health Behaviour in School-Aged Children (HBSC) Study: International Report from the 2013/2014 Survey. Geneva: World Health Organization. [Google Scholar]
- Janz, Nancy K., Victoria L. Champion, and Victor J. Strecher. 2002. The health belief model. In Health Behavior and Health Education. Edited by Barbara K. Rimer, Karen Glanz Rimer and Frances Marcus Lewis. San Francisco: Jossey-Bass, pp. 45–66. [Google Scholar]
- Johnson, Ofonime E. 2017. Determinants of modern contraceptive uptake among Nigerian women: Evidence from the national demographic and health survey. African Journal of Reproductive Health 21: 89–95. [Google Scholar] [CrossRef]
- Koenig, Michael, Iryna Zablotska, Tom Lutalo, Fred Nalugoda, Jennifer Wagman, and Ron Gray. 2004. Coerced first intercourse and reproductive health among adolescent women in Rakai, Uganda. International Family Planning Perspectives 30: 156–63. [Google Scholar] [CrossRef]
- Lara, Lúcia A. S., and Carmita H. N. Abdo. 2016. Age at Time of Initial Sexual Intercourse and Health of Adolescent Girls. Journal of Pediatric and Adolescent Gynecology 29: 417–23. [Google Scholar] [CrossRef]
- Mardi, Afrouz, Abbas Ebadi, Shirin Shahbazi, and Zahra B. Moghadam. 2018. Factors influencing the use of contraceptives through the lens of teenage women: A qualitative study in Iran. BMC Public Health 18: 202. [Google Scholar] [CrossRef] [Green Version]
- Mensch, Barbara, Monica J. Grant, and Ann K. Blanc. 2006. The changing context of sexual initiation in sub-Saharan Africa. Population and Development Review 32: 699–727. [Google Scholar] [CrossRef]
- Mutumba, Massy, Eliud Wekesa, and Rob Stephenson. 2018. Community influences on modern contraceptive use among young women in low and middle-income countries: A cross-sectional multi-country analysis. BMC Public Health 18: 430. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nalwadda, Gorette, Florence Mirembe, Josaphat Byamugisha, and Elisabeth Faxelid. 2010. Persistent high fertility in Uganda: Young people recount obstacles and enabling factors to use of contraceptives. BMC Public Health 10: 530. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ngome, Enock, and Clifford Odimegwu. 2014. The social context of adolescent women’s use of modern contraceptives in Zimbabwe: A multilevel analysis. Reproductive Health 11: 64. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nsanya, Mussa Kelvin, Christina J. Atchison, Christian Bottomley, Aoife Margaret Doyle, and Saidi H. Kapiga. 2019. Modern contraceptive use among sexually active women aged 15–19 years in North-Western Tanzania: Results from the Adolescent 360 (A360) baseline survey. BMJ Open 9: e030485. [Google Scholar] [CrossRef]
- Oginni, Ayodeji B., Babatunde A. Ahonsi, and Adebajo Sylvia. 2015. Trend and Determinants of Unmet Need for Family Planning Services among Currently Married Women and Sexually Active Unmarried Women Aged 15–49 in Nigeria (2003–2013). African Population Studies 29: 1483–99. [Google Scholar] [CrossRef] [Green Version]
- Olaide, Ojoniyi, Kanayo Ogujiuba, and Nancy Stiegler. 2022. Susceptibility to Pregnancy and use of Modern Contraceptive in Nigeria amongst Adolescents. African Journal for Reproductive Health 26: 106–17. [Google Scholar]
- Ramathuba, Dora U., Lunic B. Khoza, and Mutshinyalo L. Netshikweta. 2012. Knowledge, attitudes and practice of secondary school girls towards contraception in Limpopo Province. Curationis 35: 45. [Google Scholar] [CrossRef]
- Singh, Susheela, and Jacqueline E. Darroch. 2012. Adding It Up: Costs and Benefits of Contraceptive Services-Estimates for 2012. New York: Guttmacher Institute and United Nations Population Fund (UNFPA), Available online: http://www.guttmacher.org/pubs/AIU-2012-estimates.pdf (accessed on 14 March 2022).
- Tabane, Ntswaleng S., and Mmapheko D. Peu. 2015. Perceptions of female teenagers in the Tshwane District on the use of contraceptives in South Africa. Curationis 38: 1–7. [Google Scholar] [CrossRef]
- Taylor-Seehafer, Margaret, and Lynn Rew. 2000. Risky sexual behavior among adolescent women. Journal for Specialists in Pediatric Nursing 5: 15–25. [Google Scholar] [CrossRef]
- Toffolutti, Veronica, Hai Ma, Giulia Menichelli, Ester Berlot, Letizia Mencarini, and Arnstein Aassve. 2020. How the internet increases modern contraception uptake: Evidence from eight sub-Saharan African countries. BMJ Global Health 5: e002616. [Google Scholar] [CrossRef] [PubMed]
- Urdinola, B. Piedad, and Carlos Ospino. 2015. Long-term consequences of adolescent fertility: The Colombian case. Demographic Research 32: 1487–518. [Google Scholar] [CrossRef] [Green Version]
- UNFPA. 2013. Adolescent Pregnancy: A Review of the Evidence. New York: UNFPA, Available online: https://www.unfpa.org/sites/default/files/pub-pdf/ADOLESCENT%20PREGNANCY_UNFPA.pdf (accessed on 14 March 2022).
- Wang, Chao, and Huimin Cao. 2019. Persisting Regional Disparities in Modern Contraceptive Use and Unmet Need for Contraception among Nigerian Women. BioMed Research International 2019: 9103928. [Google Scholar] [CrossRef] [PubMed]
| Variable | Frequency N = 1014 | Percentage % |
|---|---|---|
| CURRENT AGE | Mean = 17.6, SD = 1.2, RANGE = 15–19 | |
| AGE AT FIRST SEX | Mean = 15.7, SD = 1.6, RANGE = 8–19 | |
| AGE AT FIRST USE | Mean = 18.2, SD = 1.3, RANGE = 10–19 | |
| EDUCATION | ||
| No Education | 54 | 5.3 |
| Primary Education | 95 | 9.3 |
| Secondary Education | 807 | 79.5 |
| Tertiary | 58 | 5.8 |
| PLACE OF RESIDENCE | ||
| Urban | 518 | 51.0 |
| Rural | 495 | 49.0 |
| REGION | ||
| North Central | 224 | 22.1 |
| North East | 99 | 9.8 |
| North West | 36 | 3.6 |
| South East | 165 | 16.3 |
| South South | 262 | 25.8 |
| South West | 227 | 22.4 |
| RELIGION | ||
| Catholic | 187 | 18.4 |
| Other Christians | 617 | 60.9 |
| Islam and Other | 210 | 20.7 |
| HOUSEHOLD WEALTH QUINTILE | ||
| Poorest | 74 | 7.3 |
| Poorer | 159 | 15.7 |
| Middle | 263 | 25.9 |
| Richer | 288 | 28.4 |
| Richest | 231 | 22.8 |
| SEX OF HOUSEHOLD HEAD | ||
| Male | 656 | 66.7 |
| Female | 328 | 33.3 |
| LIVING ARRANGEMENT | ||
| Living with Parent | 665 | 67.6 |
| Not living with parent | 318 | 32.4 |
| BIRTH HISTORY | ||
| No | 888 | 90.4 |
| Yes | 94 | 9.6 |
| NATURE OF FIRST SEX | ||
| Forced | 31 | 3.1 |
| Not forced | 982 | 96.9 |
| Log-Rank Test for Equality of Survivor Functions for Place of Residence | ||
| Place of Residence | Event observed | Event expected |
| Urban | 1299 | 1244 |
| Rural | 975 | 1030 |
| Total | 2274 | 2274 |
| Chi2(1) = 10.29 Pr > chi2 = 0.001 | ||
| Log-Rank Test for Equality of Survivor Functions for Region | ||
| Region | Events observed | Events expected |
| North central | 143 | 174 |
| North east | 437 | 342 |
| North west | 17 | 32 |
| South east | 400 | 389 |
| South south | 893 | 926 |
| South west | 384 | 411 |
| Total | 2275 | 2275 |
| Chi2(5) = 81.35 Pr > chi2 = 0.000 | ||
| Log-Rank Test for Equality of Survivor Functions for Age at First Sex | ||
| Age at First Sex | Events observed | Events expected |
| Less than 15 years old | 618 | 1010 |
| 15 years old or above | 1657 | 1264 |
| Total | 2275 | 2275 |
| Chi2(1) = 630.23, Pr >chi2 = 0.000 | ||
| Log-Rank Test for Equality of Survivor Functions for Level of Education | ||
| Level of Education | Events observed | Events expected |
| No education | 85 | 177 |
| Primary education | 130 | 115 |
| Secondary education | 1812 | 1714 |
| At least Secondary education | 247 | 267 |
| Total | 2275 | 2275 |
| Chi2(3) = 138.01 Pr > 0.000 | ||
| Log-Rank Test for Equality of Survivor Functions of Modern Contraception by Religion | ||
| Religion | Events observed | Events observed |
| Catholic | 343 | 335 |
| Other Christian | 1729 | 1755 |
| Islam and others | 202 | 184 |
| Total | 2275 | 2275 |
| chi2(2) = 4.48 Pr > chi2 = 0.106 | ||
| Log-Rank Test for Equality of Survivor Functions for First Sexual Experience | ||
| First Sex coerced | Event observed | Events expected |
| No | 2245 | 2242 |
| Yes | 29 | 32 |
| Total | 2275 | 2275 |
| Chi2(1) = 0.56 Pr > chi2 = 0.4558 | ||
| Log-Rank Test for Equality of Survivor Functions for sex of household head | ||
| Male | 1375 | 1439 |
| Female | 899 | 836 |
| Total | 2275 | 2275 |
| Chi2(1) = 14.48 Pr > chi2 = 0.0001 | ||
| Log-Rank Test for Equality of Survivor Functions across Wealth Quintile | ||
| Wealth quintile | Events observed | Events expected |
| Poorest | 120 | 218 |
| Poorer | 298 | 330 |
| Middle | 517 | 504 |
| Richer | 830 | 745 |
| Richest | 509 | 478 |
| Total | 2275 | 2275 |
| chi2(4) = 134.68 Pr > chi2 = 0.000 | ||
| Birth History | ||
| No | 2108 | 1983 |
| Yes | 166 | 291 |
| Total | 2275 | 2275 |
| chi2(4) = 138.61 Pr > chi2 = 0.000 | ||
| Log-Rank Test for Equality of Survivor Functions for Internet Use Groups | ||
| Internet | Events observed | Events expected |
| Never | 1367 | 1463 |
| Ever | 907 | 811 |
| Total | 2275 | 2275 |
| chi2(1) = 33.81 Pr > chi2 = 0.000 | ||
| Log-Rank Test for Equality of Survivor Functions for Internet Use Groups | ||
| Live with parent | 1379 | 1294 |
| Live other relative | 895 | 980 |
| Total | 2275 | 2275 |
| chi2(1) = 33.81 Pr > chi2 = 0.000 | ||
| Survival Time | ||||||
|---|---|---|---|---|---|---|
| Using MC | Time @ Risk | Incidence Rate | No. of Subjects | 25% | 50% | 75% |
| 4840.62 | 0.4699 | 2274 | 1 | 2 | 3 | |
| Total | 4840.62 | 0.4699 | 2274 | 1 | 2 | 3 |
| Variables | Adjusted Hazard Ratio | 95% Confidence Interval |
|---|---|---|
| AGE AT FIRST SEX | ||
| Less than 15 years old | RC | |
| 15 years old or older | 2.964 * | 2.606–3.372 |
| CURRENT AGE | 0.696 * | 0.659–0.736 |
| REGION | ||
| North Central | RC | |
| North East | 1.164 | 0.939–1.443 |
| North West | 0.484 * | 0.283–0.825 |
| South East | 0.905 | 0.712–1.150 |
| South South | 0.957 | 0.784–1.168 |
| South West | 1.142 | 0.920–1.416 |
| PLACE OF RESIDENCE | ||
| Urban | RC | |
| Rural | 1.078 | 0.965–1.205 |
| LEVEL OF EDUCATION | ||
| No Education | RC | |
| Primary Education | 1.354 | 0.937–1.956 |
| Secondary Education | 1.148 | 0.820–1.606 |
| Tertiary | 1.029 | 0.707–1.497 |
| RELIGION | ||
| Catholic | RC | |
| Other Christians | 0.968 | 0.822–1.140 |
| Islam and others | 0.858 | 0.673–1.094 |
| EVER GIVEN BIRTH | ||
| No | RC | |
| Yes | 0.832 | 0.677–1.035 |
| SEX OF HOUSEHOLD HEAD | ||
| Male | RC | |
| Female | 1.108 | 0.997–1.231 |
| HOUSEHOLD WEALTH QUINTILE | ||
| Poorest | RC | |
| Poorer | 0.962 | 0.718–1.290 |
| Middle | 1.290 | 0.971–1.715 |
| Richer | 1.292 | 0.957–1.743 |
| Richest | 1.353 * | 1.005–1.821 |
| LIVING ARRANGEMENT | ||
| Living with parent | RC | |
| Not living with parent | 1.014 | 0.919–1.120 |
| INTERNET USE | ||
| Never | RC | |
| Ever | 1.190 * | 1.063–1.332 |
| FIRST SEXUAL EXPERIENCE | ||
| Not Coerced | RC | |
| Coerced | 1.078 | 0.724–1.604 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ogujiuba, K.; Ojoniyi, O.; Stiegler, N. Analysis of Unmarried Adolescents and Modern Contraceptives Initiation in Nigeria: Evidence from 2018 NDHS. Soc. Sci. 2022, 11, 282. https://doi.org/10.3390/socsci11070282
Ogujiuba K, Ojoniyi O, Stiegler N. Analysis of Unmarried Adolescents and Modern Contraceptives Initiation in Nigeria: Evidence from 2018 NDHS. Social Sciences. 2022; 11(7):282. https://doi.org/10.3390/socsci11070282
Chicago/Turabian StyleOgujiuba, Kanayo, Olaide Ojoniyi, and Nancy Stiegler. 2022. "Analysis of Unmarried Adolescents and Modern Contraceptives Initiation in Nigeria: Evidence from 2018 NDHS" Social Sciences 11, no. 7: 282. https://doi.org/10.3390/socsci11070282
APA StyleOgujiuba, K., Ojoniyi, O., & Stiegler, N. (2022). Analysis of Unmarried Adolescents and Modern Contraceptives Initiation in Nigeria: Evidence from 2018 NDHS. Social Sciences, 11(7), 282. https://doi.org/10.3390/socsci11070282






