Evaluation of Microstructure and Mechanical Properties of a Ti10Mo8Nb Alloy for Biomedical Applications
Abstract
:1. Introduction
2. Materials and Methods
2.1. Alloy Processing of Ti10Mo8Nb
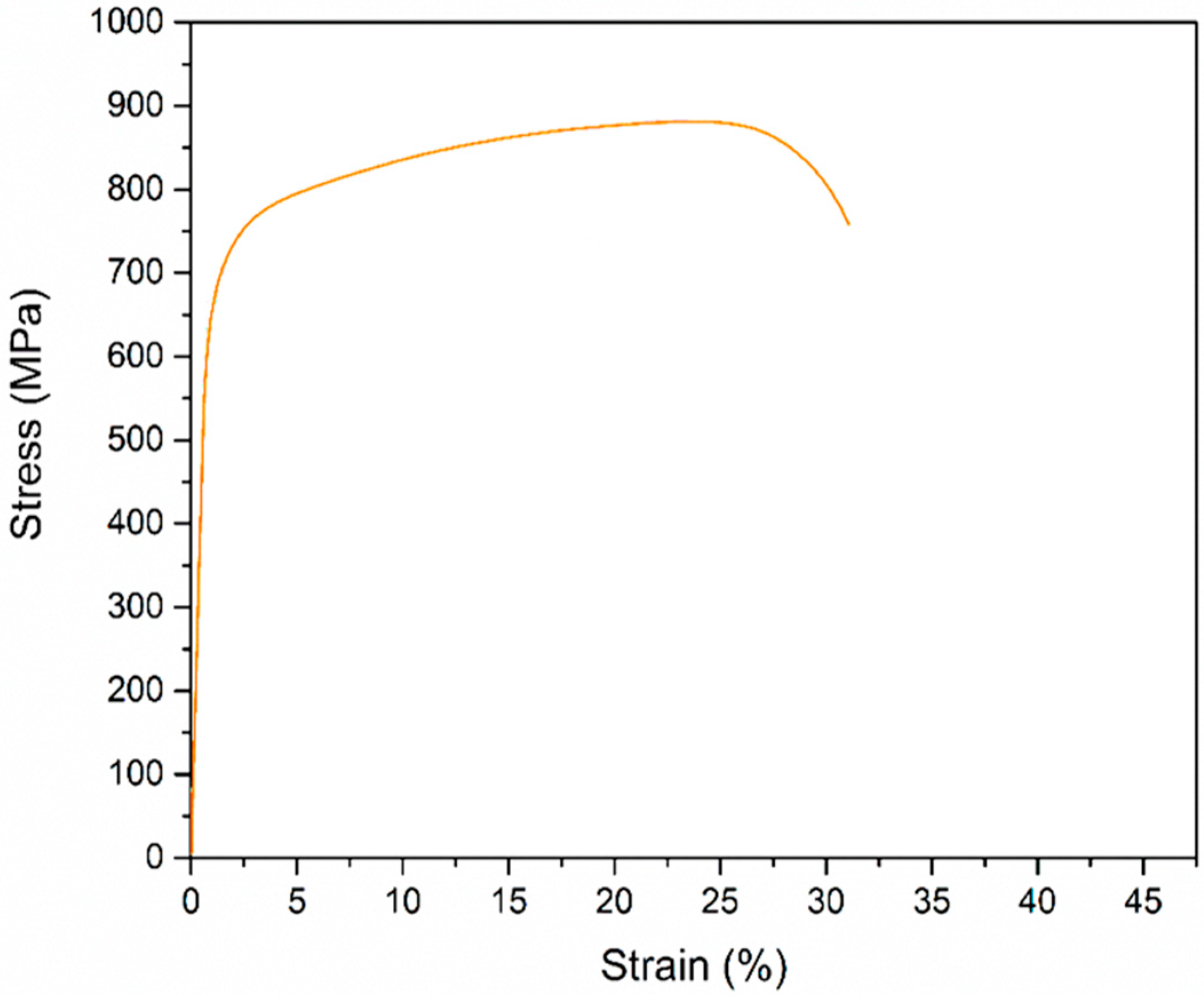
2.2. Tensile Test
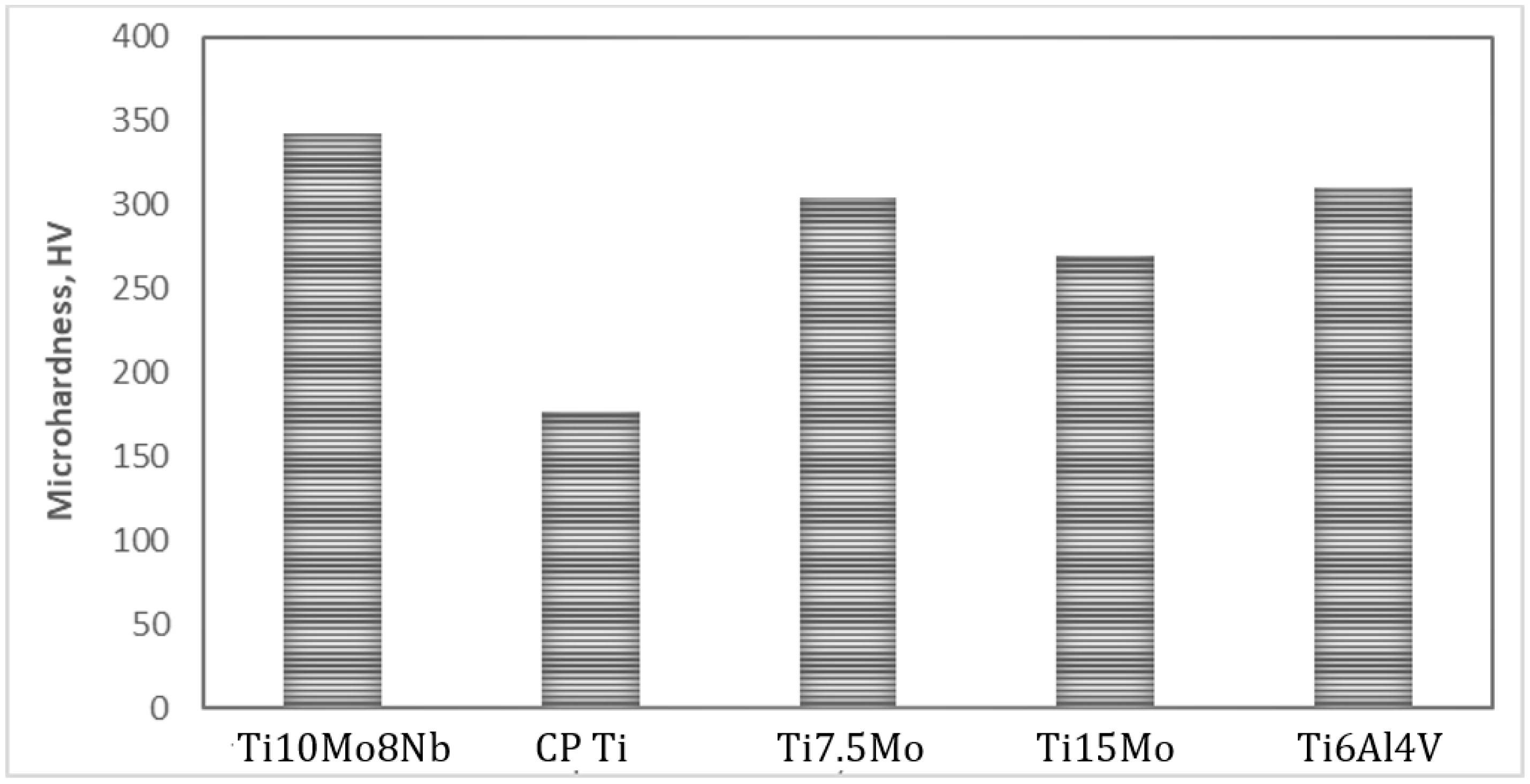
2.3. Microhardness Evaluation
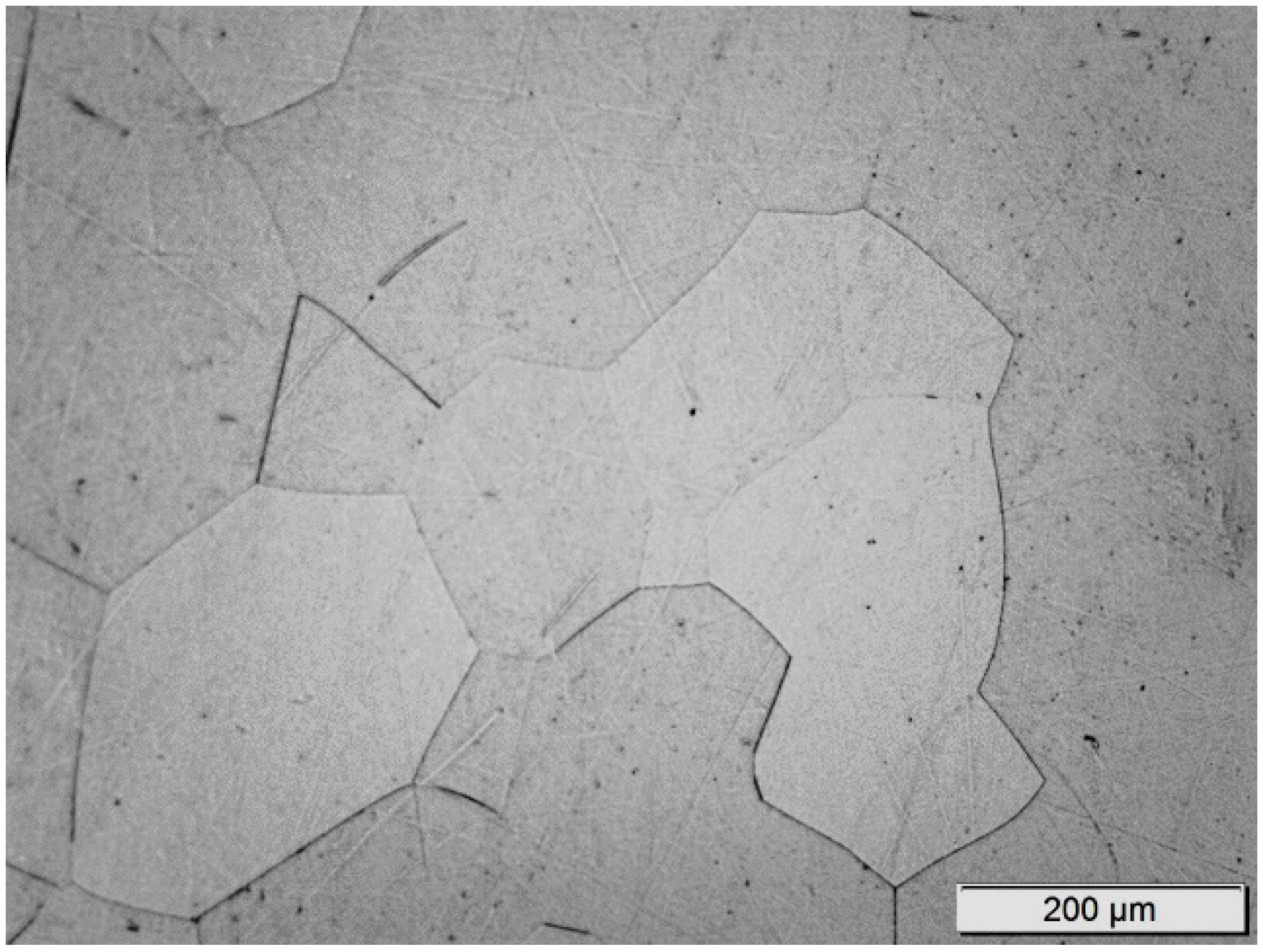
2.4. Microstructural Characterization
2.5. Fractography
2.6. X-ray Diffraction Analysis
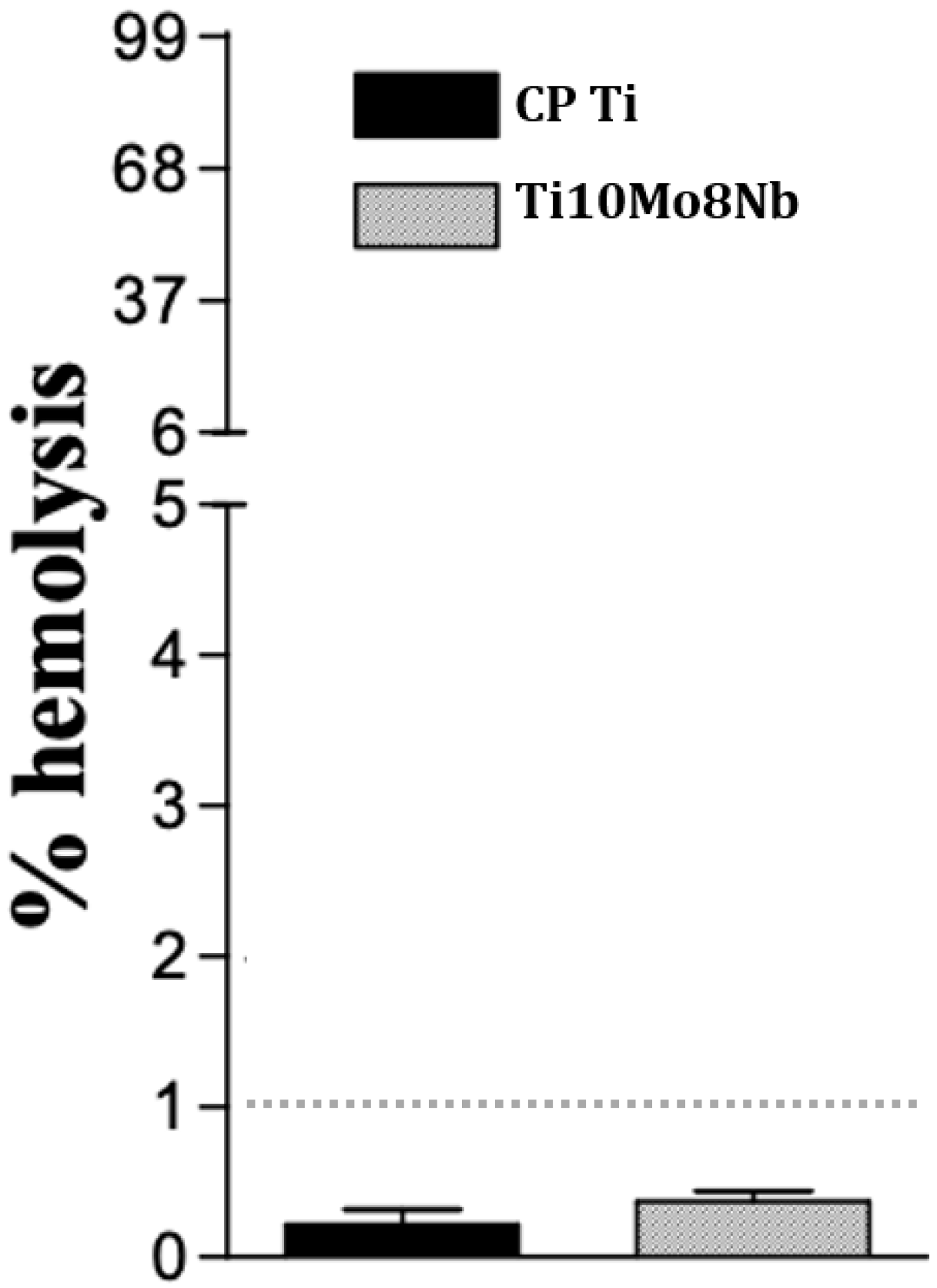
2.7. Hemolysis
3. Results and Discussion
| Alloys | Yield Strength (MPa) | Tensile Strength (MPa) | Elastic Modulus (GPa) | Elongation (%) | References |
|---|---|---|---|---|---|
| Ti10Mo8Nb | 691 ± 110 | 884 ± 75 | 91 ± 1 | 32 ± 8 | This study |
| CP Ti | 523 ± 11 | 673 ± 11 | 108 ± 4 | 24 ± 1 | Bocchetta P. et al. (2021), Sneddon S. et al. (2021), Weng W. et al. (2021), Souza B. L. et al. (2017), Ho W. et al. (2008) |
| Ti7.5Mo | 737 ± 18 | 1019 ± 15 | 70 ± 3 | 16 ± 1 | |
| Ti15Mo | 745 ± 13 | 921 ± 19 | 84 ± 1 | 25 ± 2 | |
| Ti6Al4V | 999 ± 13 | 1173 ± 17 | 113 ± 10 | 6 ± 1 |
4. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Dogra, S.; Dunstan, D.W.; Sugiyama, T.; Stathi, A.; Gardiner, P.A.; Owen, N. Active Aging and Public Health: Evidence, Implications, and Opportunities. Annu. Rev. Public Health 2022, 1, 439–459. [Google Scholar] [CrossRef] [PubMed]
- Gu, D.; Andreev, K.; Dupre, M.E. Major Trends in Population Growth Around the World. China CDC Wkly. 2021, 3, 604–613. [Google Scholar] [CrossRef] [PubMed]
- Guo, H.; Jiang, J.; Li, Y.; Liu, M.; Han, J. An Aging Giant at The Center of Global Warming: Population Dynamics and Its Effect on CO2 Emissions in China. Res. Sq. 2022, 1–26. [Google Scholar] [CrossRef]
- Dixon, A. The United Nations Decade of Healthy Ageing requires concerted global action. Nat. Aging 2021, 1, 2. [Google Scholar] [CrossRef]
- Massari, L.; Benazzo, F.; Falez, F.; Perugia, D.; Pietrogrande, L.; Setti, S.; Osti, R.; Vaienti, E.; Ruosi, C.; Cadossi, R. Biophysical stimulation of bone and cartilage: State of the art and future perspectives. Int. Orthop. 2019, 43, 539–551. [Google Scholar] [CrossRef] [Green Version]
- Herber, V.; Okutan, B.; Antonoglou, G.; Sommer, N.; Payer, M. Bioresorbable Magnesium-Based Alloys as Novel Biomaterials in Oral Bone Regeneration: General Review and Clinical Perspectives. J. Clin. Med. 2021, 10, 1842. [Google Scholar] [CrossRef] [PubMed]
- Marew, T.; Birhanu, G. Three dimensional printed nanostructure biomaterials for bone tissue engineering. Regen. Ther. 2021, 18, 102–111. [Google Scholar] [CrossRef]
- Zhou, J.; Zhang, Z.; Joseph, J.; Zhang, X.; Ferdows, B.E.; Patel, D.N.; Neal, D.; Chen, W.; Banfi, G.; Molinaro, R.; et al. Biomaterials and nanomedicine for bone regeneration: Progress and future prospects. Exploration 2021, 1, 20210011. [Google Scholar] [CrossRef]
- Sailer, I.; Karasan, D.; Todorovic, A.; Ligoutsikou, M.; Pjetursson, B.E. Prosthetic failures in dental implant therapy. Periodontology 2000 2022, 88, 130–144. [Google Scholar] [CrossRef]
- Lv, Y.; Wang, B.; Liu, G.; Tang, Y.; Lu, E.; Xie, K.; Lan, C.; Liu, J.; Qin, Z.; Wang, L. Metal Material, Properties and Design Methods of Porous Biomedical Scaffolds for Additive Manufacturing: A Review. Front. Bioeng. Biotechnol. 2021, 9, 641130. [Google Scholar] [CrossRef]
- Vahidshad, Y.; Khodabakhshi, A.H. Effect of Solution Treatment and Aging Temperature on α′ and Ti3Al(α2) Phase Formation and Mechanical Properties of Water-Quenched Ti–6Al–4V. Metallogr. Microstruct. Anal. 2022, 11, 59–71. [Google Scholar] [CrossRef]
- Rossi, M.; Amado, J.; Tobar, M.; Vicente, A.; Yañez, A.; Amigó, V. Effect of alloying elements on laser surface modification of powder metallurgy to improve surface mechanical properties of beta titanium alloys for biomedical application. J. Mater. Res. Technol. 2021, 14, 1222–1234. [Google Scholar] [CrossRef]
- Ali, T.; Wang, L.; Cheng, X.; Gu, D.; Zhou, Z.; Min, X. The effect of TiC on microstructure and mechanical properties of Ti-5553 beta phase titanium alloy. Mater. Des. 2022, 214, 110395. [Google Scholar] [CrossRef]
- Montiel-Flores, E.; Mejía-García, O.A.; Ordoñez-Librado, J.L.; Gutierrez-Valdez, A.L.; Espinosa-Villanueva, J.; Dorado-Martínez, C.; Reynoso-Erazo, L.; Tron-Alvarez, R.; Rodríguez-Lara, V.; Avila-Costa, M.R. Alzheimer-like cell death after vanadium pentoxide inhalation. Heliyon 2021, 7, e07856. [Google Scholar] [CrossRef]
- Feng, W.; Han, X.; Hu, H.; Chang, M.; Ding, L.; Xiang, H.; Chen, Y.; Li, Y. 2D vanadium carbide MXenzyme to alleviate ROS-mediated inflammatory and neurodegenerative diseases. Nat. Commun. 2021, 12, 2203. [Google Scholar] [CrossRef]
- Mohammad, N.; Ahmad, R.; Rosli, N.M.; Manan, M.A.; Marzuki, M.; Wahi, A. Sol gel deposited hydroxyapatite-based coating technique on porous titanium niobium for biomedical applications: A mini review. Mater. Today Proc. 2021, 41, 127–135. [Google Scholar] [CrossRef]
- Yolun, A.; Şimşek, M.; Kaya, M.; Annaç, E.E.; Köm, M.; Çakmak, Ö. Fabrication, characterization, and in vivo biocompatibility evaluation of titanium-niobium implants. Proc. Inst. Mech. Eng. Part H J. Eng. Med. 2020, 235, 99–108. [Google Scholar] [CrossRef]
- Omar, T.; Veiga, M.M. Is niobium critical for Canada? Extr. Ind. Soc. 2021, 8, 100898. [Google Scholar] [CrossRef]
- Li, H.-Y.; Zhao, R.-P.; Li, J.; Tamura, Y.; Spencer, C.; Stern, R.J.; Ryan, J.G.; Xu, Y.-G. Molybdenum isotopes unmask slab dehydration and melting beneath the Mariana arc. Nat. Commun. 2021, 12, 6015. [Google Scholar] [CrossRef]
- Zu, Y.; Yao, H.; Wang, Y.; Yan, L.; Gu, Z.; Chen, C.; Gao, L.; Yin, W. The age of bioinspired molybdenum-involved nanozymes: Synthesis, catalytic mechanisms, and biomedical applications. View 2021, 2, 20200188. [Google Scholar] [CrossRef]
- Glowka, K.; Zubko, M.; Świec, P.; Prusik, K.; Szklarska, M.; Chrobak, D.; Lábár, J.L.; Stróŝ, D. Influence of Molybdenum on the Microstructure, Mechanical Properties and Corrosion Resistance of Ti20Ta20Nb20(ZrHf)20−xMox (Where: X = 0, 5, 10, 15, 20) high entropy alloys. Materials 2022, 15, 393. [Google Scholar] [CrossRef] [PubMed]
- Redlich, C.; Schauer, A.; Scheibler, J.; Poehle, G.; Barthel, P.; Maennel, A.; Adams, V.; Weissgaerber, T.; Linke, A.; Quadbeck, P. In Vitro Degradation Behavior and Biocompatibility of Bioresorbable Molybdenum. Metals 2021, 11, 761. [Google Scholar] [CrossRef]
- Suresh, S.; Vinod, B.; Sujith, K.S.; Sudhakara, D. Investigation and performance of high niobium contain Ti-Al Alloys: Deformation behaviour and microstructural evolution. Mater. Today Proc. 2022. [Google Scholar] [CrossRef]
- Suesawadwanid, N.; Khantachawana, A.; Srirussamee, K.; Kondoh, K. Effect of Nb Content and water quenching on microstructure and mechanical properties of Ti-Nb alloys fabricated by spark plasma sintering. Powder Met. 2022, 1–13. [Google Scholar] [CrossRef]
- Rezende, M.C.R.A.; Felipe, J.C.; Nakazato, R.; Dutra, C.A.M.; Rangel, A.L.R.; Limírio, J.P.J.D.O.; Claro, A.P.R.A. Study of the Vickers hardness and corrosion behavior of experimental Ti-Mo alloy in dental office bleaching agents. Arch. Health Investig. 2017, 6. [Google Scholar] [CrossRef] [Green Version]
- Bocchetta, P.; Chen, L.-Y.; Tardelli, J.; Reis, A.; Almeraya-Calderón, F.; Leo, P. Passive Layers and Corrosion Resistance of Biomedical Ti-6Al-4V and β-Ti Alloys. Coatings 2021, 11, 487. [Google Scholar] [CrossRef]
- Xu, L.; Chen, Y.; Liu, Z.; Kong, F. The microstructure and properties of Ti–Mo–Nb alloys for biomedical application. J. Alloy. Compd. 2008, 453, 320–324. [Google Scholar] [CrossRef]
- Mohan, P.; Rajak, D.K.; Pruncu, C.I.; Behera, A.; Amigó-Borrás, V.; Elshalakany, A.B. Influence of β-phase stability in elemental blended Ti-Mo and Ti-Mo-Zr alloys. Micron 2020, 142, 102992. [Google Scholar] [CrossRef] [PubMed]
- Souza, B.L.M.d.; Nakazato, R.Z.; Claro, A.P.R.A.; Escada, A.L.d.A. Influência da agitação no crescimento de nanotubos de TiO2 na superfície de discos de titânio comercialmente puro. Matéria 2021, 26, 1–10. [Google Scholar] [CrossRef]
- Ho, W. Effect of omega phase on mechanical properties of Ti-Mo alloys for biomedical applications. J. Med. Biol. Eng. 2008, 28, 47–51. [Google Scholar]
- Yoon, S.; Schiffer, A.; Jang, I.G.; Lee, S.; Kim, T.-Y. Predictions of the elastic modulus of trabecular bone in the femoral head and the intertrochanter: A solitary wave-based approach. Biomech. Model. Mechanobiol. 2021, 20, 1733–1749. [Google Scholar] [CrossRef] [PubMed]
- Savio, D.; Bagno, A. When the Total Hip Replacement Fails: A Review on the Stress-Shielding Effect. Processes 2022, 10, 612. [Google Scholar] [CrossRef]
- Öhman-Mägi, C.; Holub, O.; Wu, D.; Hall, R.M.; Persson, C. Density and mechanical properties of vertebral trabecular bone—A review. JOR Spine 2021, 4, e1176. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Song, B.; Choi, S.-K.; Shi, Y. A topology strategy to reduce stress shielding of additively manufactured porous metallic biomaterials. Int. J. Mech. Sci. 2021, 197, 106331. [Google Scholar] [CrossRef]
- Sneddon, S.; Mulvihill, D.M.; Wielewski, E.; Dixon, M.; Rugg, D.; Li, P. Deformation and failure behaviour of a titanium alloy Ti-407 with reduced aluminium content: A comparison with Ti-6Al-4V in tension and compression. Mater. Charact. 2021, 172, 110901. [Google Scholar] [CrossRef]
- Weng, W.; Biesiekierski, A.; Lin, J.; Ozan, S.; Li, Y.; Wen, C. Development of beta-type Ti-Nb-Zr-Mo alloys for orthopedic applications. Appl. Mater. Today 2021, 22, 100968. [Google Scholar] [CrossRef]
- Alabort, E.; Tang, Y.; Barba, D.; Reed, R. Alloys-by-design: A low-modulus titanium alloy for additively manufactured biomedical implants. Acta Mater. 2022, 229, 117749. [Google Scholar] [CrossRef]
- Wandra, R.; Prakash, C.; Singh, S. Experimental investigation and optimization of surface roughness of β-Phase titanium alloy by ball burnishing assisted electrical discharge cladding for implant applications. Mater. Today Proc. 2021, 48, 975–980. [Google Scholar] [CrossRef]
- Kaouka, A.; Benarous, K.; Daas, A.; Tsipas, S.A. The Effects of Nb and Mo Addition on Microstructure and Mechanical Behaviour of Ti-6Al-4V Alloy. J. Surf. Sci. Technol. 2017, 33, 53–62. [Google Scholar] [CrossRef]
- Mandal, P.; Daniel, B.; Mathews, M.S.; Joseph, A.; Siby, C.; Devasia, J. Martensitic transformation in a α + β–Ti alloy after cryogenic treatment and its influencing to low elastic modulus biomaterials. Mater. Today Proc. 2021, 46, 2820–2826. [Google Scholar] [CrossRef]
- Hacisalihoglu, I.; Samancioglu, A.; Yildiz, F.; Purcek, G.; Alsaran, A. Tribocorrosion properties of different type titanium alloys in simulated body fluid. Wear 2015, 332–333, 679–686. [Google Scholar] [CrossRef]
- Raganya, M.L.; Moshokoa, N.M.; Obadele, B.; Olubambi, P.A.; Machaka, R. The microstructural and mechanical characterization of the β-type Ti-11.1Mo-10.8Nb alloy for biomedical applications. Iop Conf. Ser. Mater. Sci. Eng. 2019, 655, 012025. [Google Scholar] [CrossRef]
- Kolli, R.P.; Devaraj, A. A Review of Metastable Beta Titanium Alloys. Metals 2018, 8, 506. [Google Scholar] [CrossRef] [Green Version]
- Gabriel, S.; Panaino, J.; Santos, I.; Araujo, L.; Mei, P.; de Almeida, L.; Nunes, C. Characterization of a new beta titanium alloy, Ti–12Mo–3Nb, for biomedical applications. J. Alloy. Compd. 2012, 536, S208–S210. [Google Scholar] [CrossRef]
- Zamani, E.; Yahyaei, H.; Zamani, M. Evaluation of the mechanical properties and blood compatibility of Polycarbonate Urethane and fluorescent self-colored Polycarbonate Urethane as Polymeric Biomaterials. J. Polym. Res. 2021, 28, 112. [Google Scholar] [CrossRef]


Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Capellato, P.; Vilela, F.B.; Fontenele, A.H.P.; Silva, G.; da Silva, K.B.; Carobolante, J.P.A.; Bejarano, E.G.M.; de Lourdes Noronha Motta Melo, M.; Claro, A.P.R.A.; Sachs, D. Evaluation of Microstructure and Mechanical Properties of a Ti10Mo8Nb Alloy for Biomedical Applications. Metals 2022, 12, 1065. https://doi.org/10.3390/met12071065
Capellato P, Vilela FB, Fontenele AHP, Silva G, da Silva KB, Carobolante JPA, Bejarano EGM, de Lourdes Noronha Motta Melo M, Claro APRA, Sachs D. Evaluation of Microstructure and Mechanical Properties of a Ti10Mo8Nb Alloy for Biomedical Applications. Metals. 2022; 12(7):1065. https://doi.org/10.3390/met12071065
Chicago/Turabian StyleCapellato, Patricia, Filipe Bueno Vilela, Andres Henrique Palomo Fontenele, Gilbert Silva, Kerolene Barboza da Silva, João Pedro Aquiles Carobolante, Edwin Gilberto Medina Bejarano, Mirian de Lourdes Noronha Motta Melo, Ana Paula Rosifini Alves Claro, and Daniela Sachs. 2022. "Evaluation of Microstructure and Mechanical Properties of a Ti10Mo8Nb Alloy for Biomedical Applications" Metals 12, no. 7: 1065. https://doi.org/10.3390/met12071065
APA StyleCapellato, P., Vilela, F. B., Fontenele, A. H. P., Silva, G., da Silva, K. B., Carobolante, J. P. A., Bejarano, E. G. M., de Lourdes Noronha Motta Melo, M., Claro, A. P. R. A., & Sachs, D. (2022). Evaluation of Microstructure and Mechanical Properties of a Ti10Mo8Nb Alloy for Biomedical Applications. Metals, 12(7), 1065. https://doi.org/10.3390/met12071065