Revisiting the Correlation Between Vaccine Acceptance and Trust in Hospitals: Lessons from the COVID-19 Pandemic
Abstract
1. Theoretical Framework: Explaining Vaccine Hesitancy
- (1)
- The main gap in this scientific literature is that it tends to treat all vaccines as a collective entity, without considering the specific type of vaccine or acknowledging the historical failures of certain vaccines that have been officially recognized.
- (2)
- Another gap is the non-specific and sometimes overly simplistic classification of people and their understanding of vaccines and vaccination. This approach overlooks the subjective and social realities of individuals, reducing them to their social-demographic profile and their decision to receive or not receive a vaccine.
- (3)
- The reasons and factors contributing to vaccine and vaccination hesitancy are often listed without a deep understanding of which populations hold which reasons and why. The focus is more on the reasons for non-vaccination rather than gaining insight into the specific factors influencing the opinion of different population groups.
- Communication models: This set of models emphasizes the importance of the communication channel through which information about the vaccine, virus, pandemic, and vaccination process is conveyed and shared. The source of information plays a significant role in shaping opinions [19,20]. In 2024, another umbrella review showed that, so far, studies on COVID-19 vaccine hesitancy have pinpointed information dissemination and misinformation as the main causes [22].
- Psychosociological models: These models focus on the explanatory power of psychosociological variables that are associated with acceptance or hesitancy towards vaccination [21].
- Conspiracy models: These models posit that attitudinal variations towards vaccination are primarily influenced by a lack of trust in authorities, the propagation of conspiracy theories, and the belief in hidden intentions associated with the organization of the vaccination process by those in power [12,13,14,15].
2. Materials and Methods
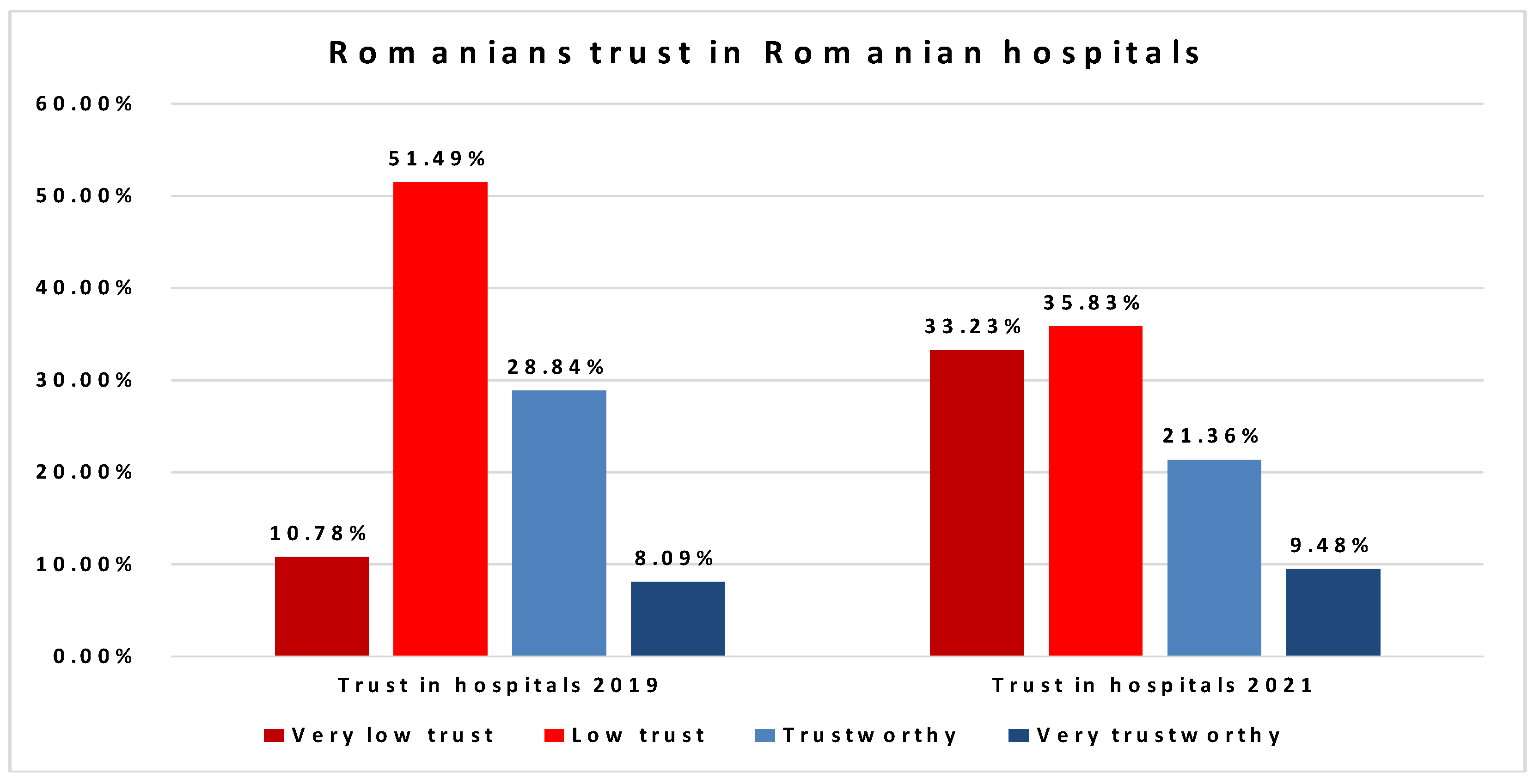
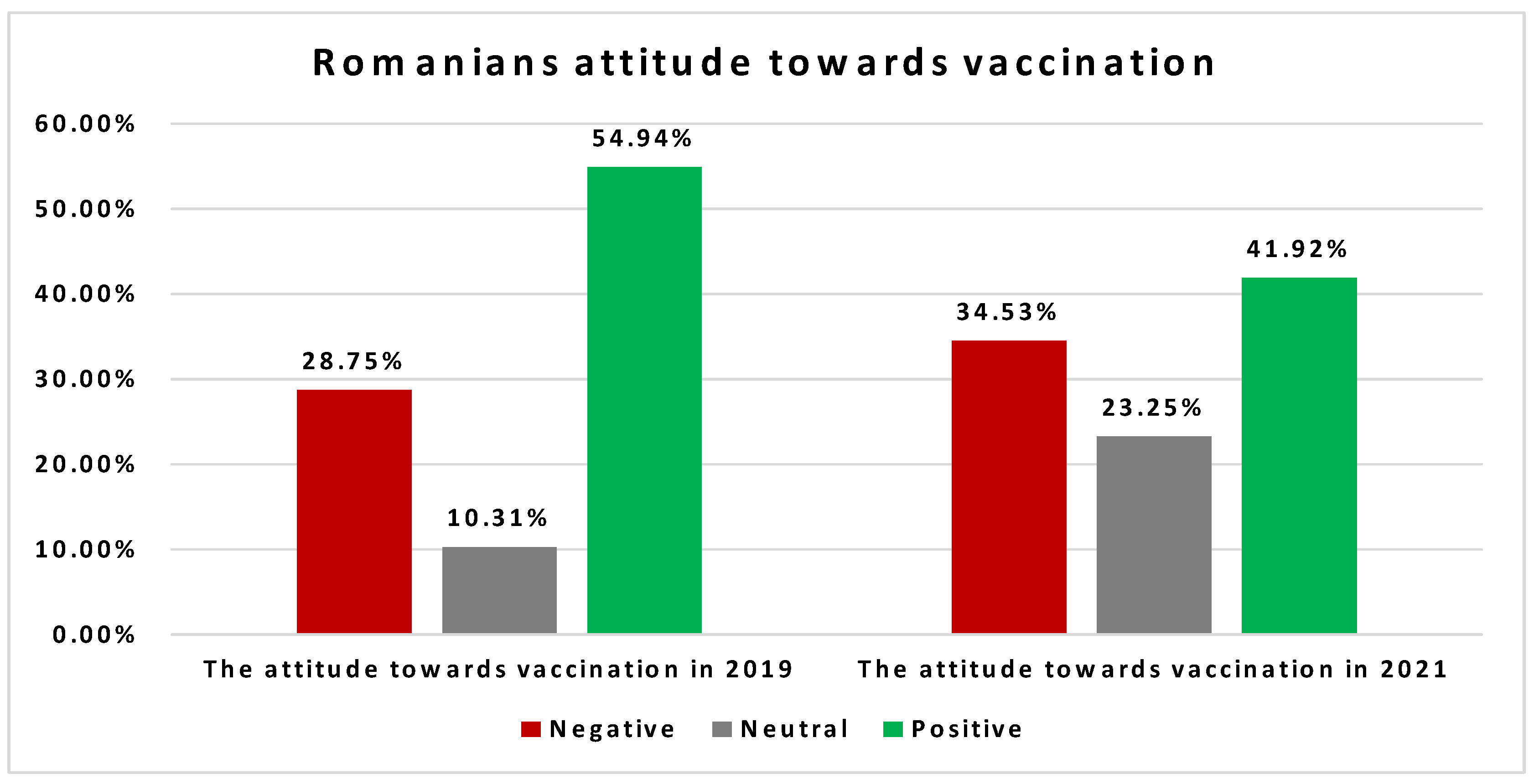
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- MacDonald, N.E.; Eskola, J.; Liang, X.; Chaudhuri, M.; Dube, E.; Gellin, B.; Goldstein, S.; Larson, H.; Manzo, M.L.; Reingold, A.; et al. Vaccine hesitancy: Definition, scope and determinants. Vaccine 2015, 33, 4161–4164. [Google Scholar] [CrossRef] [PubMed]
- Dubé, E.; Gagnon, D.; Nickels, E.; Jeram, S.; Schuster, M. Mapping vaccine hesitancy—Country-specific characteristics of a global phenomenon. Vaccine 2014, 32, 6649–6654. [Google Scholar] [CrossRef] [PubMed]
- European Comission. Vaccination Programmes and Health Systems in the Europena Union. In Report of the Expert Panel on Effective Ways of Investing in Health; Publication Office of the European Union: Luxembourg, 2018. [Google Scholar]
- Crescitelli, M.D.; Ghirotto, L.; Sisson, H.; Sarli, L.; Artioli, G.; Bassi, M.C.; Appicciutoli, G.; Hayter, M. A meta-synthesis study of the key elements involved in childhood vaccine hesitancy. Public Health 2020, 180, 38–45. [Google Scholar] [CrossRef]
- Chung, Y.; Schamel, J.; Fisher, A.; Frew, P.M. Influences on Immunization Decision-Making among US Parents of Young Children. Matern. Child Health J. 2017, 21, 2178–2187. [Google Scholar] [CrossRef] [PubMed]
- European Centre for Disease Prevention and Control (ECDC). Rapid Literature Review on Motivating Hesitant Population Groups in Europe to Vaccinate; Technical Report; ECDC: Stockholm, Sweden, 2015.
- Larson, H.J.; Jarrett, C.; Eckersberger, E.; Smith, D.M.D.; Paterson, P. Understanding vaccine hesitancy around vaccines and vaccination from a global perspective: A systematic review of published literature, 2007–2012. Vaccine 2014, 32, 2150–2159. [Google Scholar] [CrossRef] [PubMed]
- Gilkey, M.B.; Magnus, B.E.; Reiter, P.L.; McRee, A.-L.; Dempsey, A.F.; Brewer, N.T. The Vaccination Confidence Scale: A brief measure of parents’ vaccination beliefs. Vaccine 2014, 32, 6259–6265. [Google Scholar] [CrossRef]
- Cristea, D.; Petrescu, D.A.; Ghișoiu, C. Vaccine Refusal in Romania. An Estimation Based on Public Opinion Surveys. Proc. Rom. Acad. Ser. B Chem. Life Sci. Geosci. 2021, 23, 25–32. [Google Scholar]
- Goldenberg, M.J. Vaccines, values and science. CMAJ 2019, 191, E397–E398. [Google Scholar] [CrossRef]
- Boshra, M.S.; Hussein, R.R.S.; Mohsen, M.; Elberry, A.A.; Altyar, A.E.; Tammam, M.; Sarhan, R.M. A battle against COVID-19: Vaccine hesitancy and awareness with a comparative study between Sinopharm and AstraZeneca. Vaccines 2022, 10, 292. [Google Scholar] [CrossRef]
- Park, H.K.; Ham, J.H.; Jang, D.H.; Lee, J.Y.; Jang, W.M. Political ideologies, government trust, and COVID-19 vaccine hesitancy in South Korea: A cross-sectional survey. Int. J. Environ. Res. Public Health 2021, 18, 10655. [Google Scholar] [CrossRef]
- Savoia, E.; Su, M.; Piltch-Loeb, R.; Masterson, E.; Testa, M.A. COVID-19 vaccine early skepticism, misinformation and informational needs among essential workers in the USA. Int. J. Environ. Res. Public Health 2021, 18, 13244. [Google Scholar] [CrossRef]
- Wynen, J.; de Beeck, S.O.; Verhoest, K.; Glavina, M.; Six, F.; Van Damme, P.; Beutels, P.; Hendrickx, G.; Pepermans, K. Taking a COVID-19 vaccine or not? Do trust in government and trust in experts help us to understand vaccination intention? Adm. Soc. 2022, 54, 1875–1901. [Google Scholar] [CrossRef]
- Yang, Z.; Luo, X.; Jia, H. Is it all a conspiracy? Conspiracy theories and people’s attitude to COVID-19 vaccination. Vaccines 2021, 9, 1051. [Google Scholar] [CrossRef]
- AlShurman, B.A.; Khan, A.F.; Mac, C.; Majeed, M.; Butt, Z.A. What demographic, social, and contextual factors influence the intention to use COVID-19 vaccines: A scoping review. Int. J. Environ. Res. Public Health 2021, 18, 9342. [Google Scholar] [CrossRef] [PubMed]
- Kosarkova, A.; Malinakova, K.; van Dijk, J.P.; Tavel, P. Vaccine refusal in the czech republic is associated with being spiritual but not religiously affiliated. Vaccines 2021, 9, 1157. [Google Scholar] [CrossRef]
- Sallam, M.; Al-Sanafi, M.; Sallam, M. A global map of COVID-19 vaccine acceptance rates per country: An updated concise narrative review. J. Multidiscip. Healthc. 2022, 15, 21–45. [Google Scholar] [CrossRef] [PubMed]
- Garett, R.; Young, S.D. Online misinformation and vaccine hesitancy. Transl. Behav. Med. 2021, 11, 2194–2199. [Google Scholar] [CrossRef]
- Baraybar-Fernández, A.; Arrufat-Martín, S.; Rubira-García, R. Public information, traditional media and social networks during the COVID-19 crisis in Spain. Sustainability 2021, 13, 6534. [Google Scholar] [CrossRef]
- Cristea, D.; Ilie, D.-G.; Constantinescu, C.; Fîrțală, V. Vaccinating against COVID-19: The correlation between pro-vaccination attitudes and the belief that our peers want to get vaccinated. Vaccines 2021, 9, 1366. [Google Scholar] [CrossRef]
- Rahbeni, T.A.; Satapathy, P.; Itumalla, R.; Marzo, R.R.; Mugheed, K.A.; Khatib, M.N.; Gaidhane, S.; Zahiruddin, Q.S.; Rabaan, A.A.; Alrasheed, H.A.; et al. COVID-19 vaccine hesitancy: Umbrella review of systematic reviews and meta-analysis. JMIR Public Health Surveill. 2024, 10, e54769. [Google Scholar] [CrossRef]
- Lee, C.; Whetten, K.; Omer, S.; Pan, W.; Salmon, D. Hurdles to herd immunity: Distrust of government and vaccine refusal in the US, 2002–2003. Vaccine 2016, 34, 3972–3978. [Google Scholar] [CrossRef] [PubMed]
- Larson, H.J.; Clarke, R.M.; Jarrett, C.; Eckersberger, E.; Levine, Z.; Schulz, W.S.; Paterson, P. Measuring trust in vaccination: A systematic review. Hum. Vaccines Immunother. 2018, 14, 1599–1609. [Google Scholar] [CrossRef]
- Nowak, S.A.; Gidengil, C.A.; Parker, A.M.; Matthews, L.J. Association among trust in health care providers, friends, and family, and vaccine hesitancy. Vaccine 2021, 39, 5737–5740. [Google Scholar] [CrossRef]
- Silver, D.; Kim, Y.; McNeill, E.; Piltch-Loeb, R.; Wang, V.; Abramson, D. Association between COVID-19 vaccine hesitancy and trust in the medical profession and public health officials. Prev. Med. 2022, 164, 107311. [Google Scholar] [CrossRef] [PubMed]
- Casiday, R.; Cresswell, T.; Wilson, D.; Panter-Brick, C. A survey of UK parental attitudes to the MMR vaccine and trust in medical authority. Vaccine 2006, 24, 177–184. [Google Scholar] [CrossRef]
- Trent, M.; Seale, H.; Chughtai, A.A.; Salmon, D.; MacIntyre, C.R. Trust in government, intention to vaccinate and COVID-19 vaccine hesitancy: A comparative survey of five large cities in the United States, United Kingdom, and Australia. Vaccine 2022, 40, 2498–2505. [Google Scholar] [CrossRef] [PubMed]
- Vasile, M.; Jderu, G.; Cristea, D. Trust in the Public Health System and Seasonal-Influenza Vaccination. Transylvanian Review of Administrative Sciences. 2024, pp. 113–129. Available online: https://rtsa.ro/tras/index.php/tras/article/view/772 (accessed on 17 March 2024). [CrossRef]
- Toró, T.; Székely, I.G.; Kiss, T.; Geambașu, R. Inherent Attitudes or Misplaced Policies? Explaining COVID-19 Vaccine Hesitancy in Romania. East Eur. Politics-Soc. Cult. 2024, 38, 1093–1116. [Google Scholar] [CrossRef]
- Li, C.; Su, Z.; Chen, Z.; Cao, J.; Xu, F. Trust of healthcare workers in vaccines may enhance the public’s willingness to vaccinate. Hum. Vaccines Immunother. 2022, 18, 2158669. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Williamson, L.D.; Tarfa, A. Examining the relationships between trust in providers and information, mistrust, and COVID-19 vaccine concerns, necessity, and intentions. BMC Public Health 2022, 22, 1–12. [Google Scholar] [CrossRef]
- Cristea, D.; Jderu, G.; Petrescu, D.A. Percepția vaccinării și comportamentele legate de vaccinare în România. In Raport și Recomandări; Inscop Research: București, Romania, 2019. [Google Scholar]
- Dungaciu, D.; Cristea, D. Barometrul de Securitate a României, National Representative Sociological Survey; LARICS: Bucharest, Romania, 2021. [Google Scholar]
- Marinthe, G.; Brown, G.; Cristea, M.; Kutlaca, M. Predicting vaccination hesitancy: The role of basic needs satisfaction and institutional trust. Vaccine 2024, 42, 3592–3600. [Google Scholar] [CrossRef]
- WHO. Ten Threats to Global Health in 2019. Available online: https://www.who.int/news-room/spotlight/ten-threats-to-global-health-in-2019 (accessed on 29 April 2025).
- Fairhead, J.; Leach, M. Vaccine Anxieties: Global Science, Child Health and Society; Routledge: London, UK, 2012. [Google Scholar]
- Galagali, P.M.; Kinikar, A.A.; Kumar, V.S. Vaccine hesitancy: Obstacles and challenges. Curr. Pediatr. Rep. 2022, 10, 241–248. [Google Scholar] [CrossRef] [PubMed]
- Vuolanto, P.; Almeida, A.N.; Anderson, A.; Auvinen, P.; Beja, A.; Bracke, P.; Cardano, M.; Ceuterick, M.; Correia, T.; De Vito, E.; et al. Trust matters: The addressing vaccine hesitancy in Europe study. Scand. J. Public Health 2024, 52, 379–390. [Google Scholar] [CrossRef] [PubMed]
- Leblang, D.; Smith, M.D.; Wesselbaum, D. Trust in institutions affects vaccination campaign outcomes. Trans. R. Soc. Trop. Med. Hyg. 2024, 118, 720–728. [Google Scholar] [CrossRef] [PubMed]
- Aguinaga-Ontoso, I.; Guillen-Aguinaga, S.; Guillen-Aguinaga, L.; Alas-Brun, R.; Guillen-Aguinaga, M.; Onambele, L.; Aguinaga-Ontoso, E.; Rayón-Valpuesta, E.; Guillen-Grima, F. The Impact of COVID-19 on DTP3 Vaccination Coverage in Europe (2012–2023). Vaccines 2024, 13, 6. [Google Scholar] [CrossRef]
- Luca, C.; Azoicăi, D.; Alexa, I.H.; Vâță, A.; Cucoș, N.; Pascariu, A.; Hunea, I. Cultural Perspectives on Vaccination—An Ethical Dilemma? J. Intercult. Manag. Ethics 2020, 3, 19–27. [Google Scholar] [CrossRef]
| Vaccine Hesitancy Determinants Matrix | |
|---|---|
| Contextual influences Influences arising due to historic, socio-cultural, environmental, health system/institutional, economic or political factors | a. Communication and media environment b. Influential leaders, immunization programme gatekeepers and anti- or pro-vaccination lobbies c. Historical influences d. Religion/culture/gender/socio-economic e. Politics/policies f. Geographic barriers g. Perception of the pharmaceutical industry |
| Individual and group influences Influences arising from personal perception of the vaccine or influences of the social/peer environment | a. Personal, family and/or community members’ experience with vaccination, including pain b. Beliefs, attitudes about health and prevention c. Knowledge/awareness d. Health system and providers—trust and personal experience e. Risk/benefit (perceived, heuristic) f. Immunization as a social norm vs. not needed/harmful |
| Vaccine/vaccination—specific issues directly related to vaccine or vaccination | a. Risk/benefit (epidemiological and scientific evidence) b. Introduction of a new vaccine or new formulation or a new recommendation for an existing vaccine c. Mode of administration d. Design of vaccination programme/Mode of delivery (e.g., routine programme or mass vaccination campaign) e. Reliability and/or source of supply of vaccine and/or vaccination equipment f. Vaccination schedule g. Costs h. The strength of the recommendation and/or knowledge base and/or attitude of healthcare professionals |
| Trust in Hospitals in 2019 | Attitude Towards Vaccination in 2019 | ||
|---|---|---|---|
| Trust in hospitals in 2019 | Pearson Correlation | 1 | 0.265 |
| Sig. (2-tailed) | 0.000 | ||
| N | 2098 | 1972 | |
| Attitude towards vaccination in 2019 | Pearson Correlation | 0.265 | 1 |
| Sig. (2-tailed) | 0.000 | ||
| N | 1972 | 1988 | |
| Trust in Hospitals in 2021 | Attitude Towards Vaccination in 2021 | ||
|---|---|---|---|
| Trust in hospitals in 2021 | Pearson Correlation | 1 | −0.058 |
| Sig. (2-tailed) | 0.069 | ||
| N | 1001 | 998 | |
| Attitude towards vaccination in 2021 | Pearson Correlation | −0.058 | 1 |
| Sig. (2-tailed) | 0.069 | ||
| N | 998 | 999 | |
| TV News | Information from Friends | Information from Facebook | From Family | From Governmental Websites | ||
|---|---|---|---|---|---|---|
| Attitude towards vaccination in 2021 | Pearson Correlation | 0.050 | −0.021 | −0.080 | 0.069 | −0.003 |
| Sig. (2-tailed) | 0.113 | 0.516 | 0.011 | 0.029 | 0.932 | |
| N | 999 | 999 | 999 | 999 | 999 | |
| Confidence in the Government | Confidence in the President | Confidence in Parliament | ||
|---|---|---|---|---|
| Attitude towards vaccination in 2021 | Pearson Correlation | 0.179 | 0.209 | 0.146 |
| Sig. (2-tailed) | 0.000 | 0.000 | 0.000 | |
| N | 997 | 997 | 997 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Marinescu, V.; Cristea, D.; Fox, B.; Ilie, D.-G.; Rodideal, A.A.; Marinache, R. Revisiting the Correlation Between Vaccine Acceptance and Trust in Hospitals: Lessons from the COVID-19 Pandemic. Societies 2025, 15, 183. https://doi.org/10.3390/soc15070183
Marinescu V, Cristea D, Fox B, Ilie D-G, Rodideal AA, Marinache R. Revisiting the Correlation Between Vaccine Acceptance and Trust in Hospitals: Lessons from the COVID-19 Pandemic. Societies. 2025; 15(7):183. https://doi.org/10.3390/soc15070183
Chicago/Turabian StyleMarinescu, Valentina, Darie Cristea, Bianca Fox, Dragoș-Georgian Ilie, Anda Anca Rodideal, and Ramona Marinache. 2025. "Revisiting the Correlation Between Vaccine Acceptance and Trust in Hospitals: Lessons from the COVID-19 Pandemic" Societies 15, no. 7: 183. https://doi.org/10.3390/soc15070183
APA StyleMarinescu, V., Cristea, D., Fox, B., Ilie, D.-G., Rodideal, A. A., & Marinache, R. (2025). Revisiting the Correlation Between Vaccine Acceptance and Trust in Hospitals: Lessons from the COVID-19 Pandemic. Societies, 15(7), 183. https://doi.org/10.3390/soc15070183







