Measuring Perceived Discrimination and Its Consequences for Latino Health
Abstract
1. Introduction
1.1. Health, Discrimination Stress, and Social Stratification
1.2. Key Issues in the Measurement of Perceived Discrimination
1.3. What Are Latinos and Their Experiences with Discrimination
1.4. Overview and Gaps in the Literature: The Effects of Discrimination on Health
1.5. Propositions, Research Questions and Hypothesis
- Are there sub-ethnic differences in reports of perceived discrimination between Latino groups?
- What is the factor structure of the EDS for all Latinos, and for Cubans, Mexicans, Puerto Ricans, and Latinos of other ethnic backgrounds?
- Does the relationship between discrimination and health (i.e., concurrent validity) depend on the scaling approach that is used?
- Specifically, what are the implications of using a composite scale approach compared to adopting a latent variable approach that accounts for measurement error, scale dimensionality, and skewed dichotomous factor indicators?
2. Materials and Methods
2.1. Measures
2.1.1. Dependent Variables
2.1.2. Independent Variables
2.1.3. Background Variables
2.1.4. Analytic Plan
3. Results
3.1. Descriptive Statistics
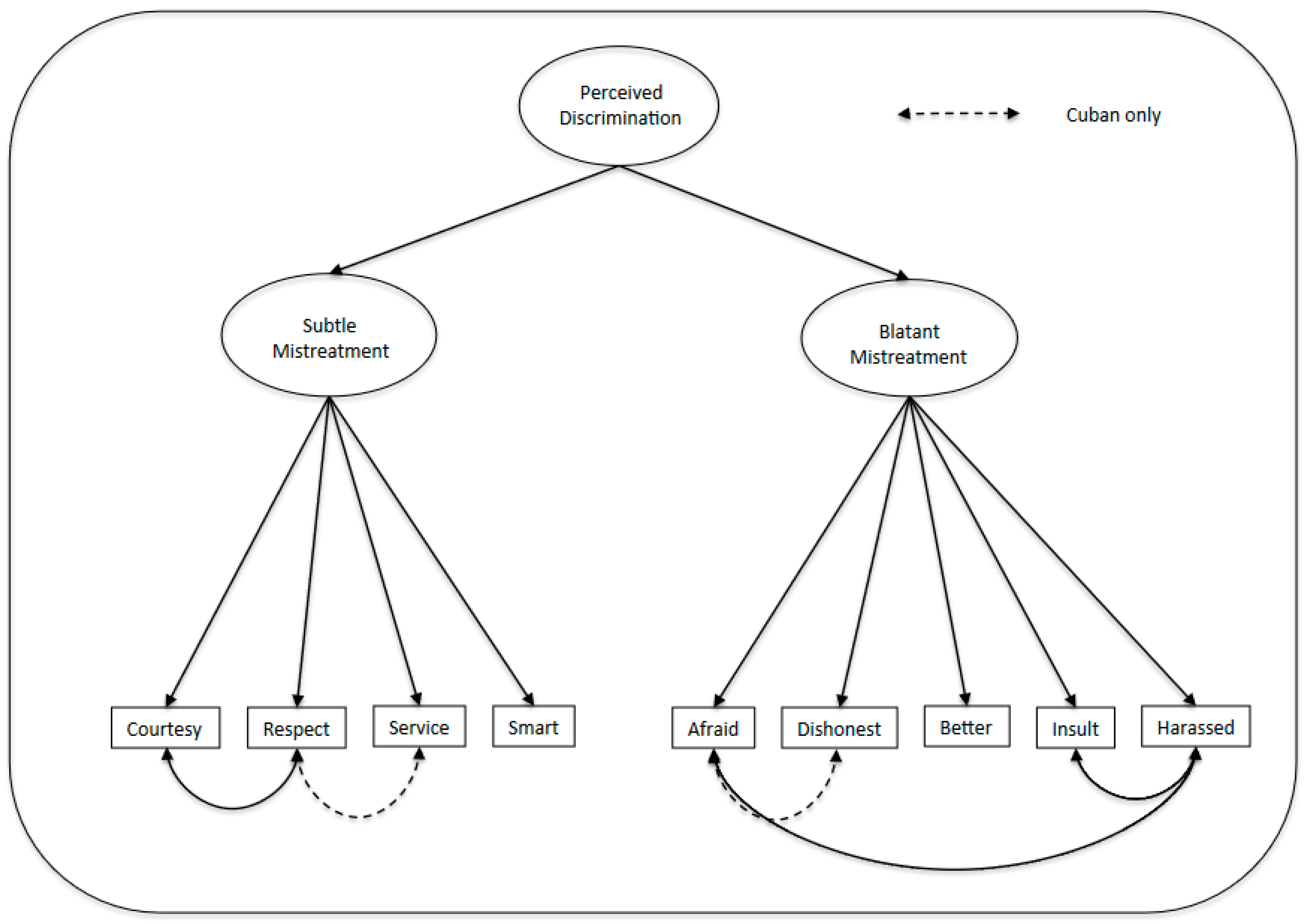
3.2. Confirmatory Factor Analysis
3.3. Concurrent Validity: Multivariate Relationship Between Discrimination and Health
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- The Leadership Conference. Cause for Concern: The State of Hate; The Leadership Conference Education Fund: Washington, DC, USA, 2024; Available online: https://civilrights.org/edfund/wp-content/uploads/sites/2/2024/05/CauseforConcern-TheStateofHate-2024.pdf (accessed on 15 October 2025).
- Molina, K.; Tan, K.; Chen, J.; Durazo-Arvizu, R.; Gallo, L.C.; Perreira, K.M.; Sanchez-Johnsen, L.; Zeng, D.; Pulgaron, E.; Delamater, A.; et al. Profiles of Structural Violence in Hispanic/Latino Immigrant and Non-Immigrant Parents: The Hispanic Community Health Study/Study of Latinos (HCHS/SOL) Youth Study. J. Immigr. Minor. Health 2025, 1–12. [Google Scholar] [CrossRef]
- Vargas, E.D.; Juarez, M.; Stone, L.C.; Lopez, N. Critical ‘Street Race’ Praxis: Advancing the Measurement of Racial Discrimination among Diverse Latinx Communities in the U.S. Crit. Public Health 2021, 31, 381–391. [Google Scholar] [CrossRef]
- Bonilla-Silva, E. Racism Without Racists: Color-Blind Racism and the Persistence of Racial Inequality in America; Rowman & Littlefield: Lanham, MD, USA, 2021. [Google Scholar]
- Krieger, N.; Bassett, M.T. Structural and Scientific Racism, Science, and Health—Evidence versus Ideology. N. Engl. J. Med. 2025, 393, 1145–1148. [Google Scholar] [CrossRef]
- Xu, S.; Widaman, K.F.; Patippe, C.; Cui, L.; Shi, X.; Krobath, D.M.; Cuevas, A.; Chang, V.W. Measurement Invariance of the Perceived Discrimination Scale across Race/Ethnicity and Sex: Findings from the Adolescent Brain and Cognitive Development (ABCD) Study. SSM Ment. Health 2025, 8, 100512. [Google Scholar] [CrossRef]
- Vallejo, J.A. Racist Policy Shocks in the United States and Latino Elites’ Identities and Actions: Prop 187, SB 1070, and Trump’s Racism. Am. Behav. Sci. 2025, 2, 1–18. [Google Scholar] [CrossRef]
- Ormiston, C.K.; Villalobos, K.; Montiel Ishino, F.A.; Williams, F. Association Between Discrimination and Depressive Symptoms Among Hispanic or Latino Adults During the COVID-19 Pandemic: Cross-Sectional Study. JMIR Form. Res. 2024, 8, e48076. [Google Scholar] [CrossRef]
- Borrell, L.N.; Markides, K.S. Will the Health Status of the Changing Hispanic Population Remain “Paradoxical”? Am. J. Public Health 2024, 114, S431–S435. [Google Scholar] [CrossRef] [PubMed]
- Krieger, N.; Smith, K.; Naishadham, D.; Hartman, C.; Barbeau, E.M. Experiences of Discrimination: Validity and Reliability of a Self-Report Measure for Population Health Research on Racism and Health. Soc. Sci. Med. 2005, 61, 1576–1596. [Google Scholar] [CrossRef]
- Williams, D.R.; Yu, Y.; Jackson, J.S.; Anderson, N.B. Racial Differences in Physical and Mental Health: Socio-Economic Status, Stress and Discrimination. J. Health Psychol. 1997, 2, 335–351. [Google Scholar] [CrossRef]
- Arellano-Morales, L.; Roesch, S.C.; Gallo, L.C.; Emory, K.T.; Molina, K.M.; Gonzalez, P.; Penedo, F.J.; Navas-Nacher, E.L.; Teng, Y.; Deng, Y.; et al. Prevalence and Correlates of Perceived Ethnic Discrimination in the Hispanic Community Health Study/Study of Latinos Sociocultural Ancillary Study. J. Lat. Psychol. 2015, 3, 160–176. [Google Scholar] [CrossRef]
- Brondolo, E.; Kelly, K.P.; Coakley, V.; Gordon, T.; Thompson, S.; Levy, E.; Cassells, A.; Tobin, J.N.; Sweeney, M.; Contrada, R.J. The Perceived Ethnic Discrimination Questionnaire: Development and Preliminary Validation of a Community Version. J. Appl. Soc. Psychol. 2005, 35, 335–365. [Google Scholar] [CrossRef]
- Lopez-Vergara, H.I.; Rozum, W.; Charvis, J.M.S.; Iacoi, S.; Vergara-Lopez, C.; Stein, L.A.R. Experiences of Discrimination and Alcohol Involvement Among Young Adults at the Intersection of Race/Ethnicity and Gender. J. Racial Ethn. Health Disparities 2025, 12, 3938–3954. [Google Scholar] [CrossRef]
- Barnes, L.; De Leon, C.F.; Wilson, R.S.; Bienias, J.; Bennett, D.A.; Evans, D.A. Racial Differences in Perceived Discrimination in a Community Population of Older Blacks and Whites. J. Aging Health 2004, 16, 315–337. [Google Scholar] [CrossRef]
- Guyll, M.; Mathews, K.; Bromberger, J.T. Discrimination and Unfair Treatment: Relationship to Cardiovascular Reactivity among African American and European Women. Health Psychol. 2001, 20, 315–325. [Google Scholar] [CrossRef]
- Noh, S.; Kaspar, V.; Wickrama, K.A.S. Overt and Subtle Racial Discrimination and Mental Health: Preliminary Findings for Korean Immigrants. Am. J. Public Health 2007, 97, 1269–1274. [Google Scholar] [CrossRef]
- Baker, F.B.; Kim, S.-H. Item Response Theory: Parameter Estimation Techniques, 2nd ed.; CRC Press: Boca Raton, FL, USA, 2004. [Google Scholar] [CrossRef]
- Paradies, Y.C. A Systematic Review of Empirical Research on Self-Reported Racism and Health. Int. J. Epidemiol. 2006, 35, 888–901. [Google Scholar] [CrossRef]
- Burgos, G.; Rivera, F.I.; Garcia, M.A. Contextualizing the Relationship between Culture and Puerto Rican Health: Towards a Place-Based Framework of Minority Health Disparities. Cent. J. Cent. Puerto Rican Stud. 2017, 29, 10–49. [Google Scholar]
- McCarty, R. Stress, Health, and Behavior; Guilford Press: New York, NY, USA, 2023. [Google Scholar] [CrossRef]
- Roach, E.L.; Haft, S.L.; Huang, J.; Zhou, Q. Systematic Review: The Association Between Race-Related Stress and Trauma and Emotion Dysregulation in Youth of Color. J. Am. Acad. Child. Adolesc. Psychiatry 2023, 62, 190–207. [Google Scholar] [CrossRef] [PubMed]
- Hartung, F.-M.; Renner, B. Perceived and Actual Social Discrimination: The Case of Overweight and Social Inclusion. Front. Psychol. 2013, 4, 147. [Google Scholar] [CrossRef] [PubMed]
- Harrell, S.P. A Multidimensional Conceptualization of Racism-Related Stress: Implications for the Well-Being of People of Color. Am. J. Orthopsychiatry 2000, 70, 42–57. [Google Scholar] [CrossRef]
- Turner, R.J.; Avison, W.R. Status Variations in Stress Exposure: Implications for the Interpretation of Research on Race, Socioeconomic Status, and Gender. J. Health Soc. Behav. 2003, 44, 488–505. [Google Scholar] [CrossRef] [PubMed]
- Romero, A.J.; Roberts, R.E. Stress Within a Bicultural Context for Adolescents of Mexican Descent. Cult. Divers. Ethn. Minor. Psychol. 2003, 9, 171–184. [Google Scholar] [CrossRef]
- Thoits, P.A. Treatment’s Role in Clinical and Perceived Recoveries from Mental Illness. Soc. Ment. Health 2023, 13, 169–186. [Google Scholar] [CrossRef]
- López-Cevallos, D.F.; Harvey, S.M. Psychometric Properties of a Healthcare Discrimination Scale Among Young-Adult Latinos. J. Racial Ethn. Health Disparities 2019, 6, 618–624. [Google Scholar] [CrossRef]
- Louie, P.; Upenieks, L. Vicarious Discrimination, Psychosocial Resources, and Mental Health among Black Americans. Soc. Psychol. Q. 2022, 85, 187–209. [Google Scholar] [CrossRef]
- Anim, S.B.; Spurlark, R.; Turkson-Ocran, R.-A.; Bohr, N.; Soco, C.; Simonovich, S.D. A Systematic Review of the Relationship Between Discrimination, Racism, and Type 2 Diabetes Healthcare Outcomes for Black Americans. J. Racial Ethn. Health Disparities 2023, 11, 2935–2944. [Google Scholar] [CrossRef] [PubMed]
- Meyer, I.H. Prejudice as Stress: Conceptual and Measurement Problems. Annu. J. Public Health 2003, 93, 262–265. [Google Scholar] [CrossRef] [PubMed]
- Ong, A.D.; Fuller-Rowell, T.; Burrow, A.L. Racial Discrimination and the Stress Process. J. Personal. Soc. Psychol. 2009, 96, 1259–1271. [Google Scholar] [CrossRef]
- Parent, C.; Ramírez, G.; Yang, C.; Grieb, S.M.; Saxton, R.E.; Martínez, D.A.; Page, K.R. Association of Intersectional Anticipated Discrimination with Mental Health Among Immigrant Latinos. Health Equity 2024, 8, 770–779. [Google Scholar] [CrossRef]
- Adem, M.; Rao, S.; Marrow, H.B.; García, M.J.; Okamoto, D.G. A Relational Approach to Perceived Discrimination: The Case of South Asian Indians. Soc. Psychol. Q. 2023, 86, 357–378. [Google Scholar] [CrossRef]
- Taylor, T.; Williams, C.; Makambi, K.; Mouton, C.; Harrell, J.; Cozier, Y.; Palmer, J.; Rosenberg, L.; Adams-Campbell, L. Racial Discrimination and Breast Cancer Incidence in US Black Women: The Black Women’s Health Study. Am. J. Epidemiol. 2007, 166, 46. [Google Scholar] [CrossRef]
- Brondolo, E.; ver Halen, N.B.; Pencille, M.; Beatty, D.; Contrada, R.J. Coping with Racism: A Selective Review of the Literature and a Theoretical and Methodological Critique. J. Behav. Med. 2009, 32, 64–88. [Google Scholar] [CrossRef]
- Krieger, N. Embodying Inequality: A Review of Concepts, Measures, and Methods for Studying Health Consequences of Discrimination. Int. J. Health Serv. 1999, 29, 295–352. [Google Scholar] [CrossRef]
- Shariff-Marco, S.; Breen, N.; Landrine, H.; Reeve, B.B.; Krieger, N.; Gee, G.C.; Williams, D.R.; Mays, V.M.; Ponce, N.A.; Alegría, M.; et al. Measuring Everyday Racial/Ethnic Discrimination in Health Surveys: How Best to Ask the Questions, in One or Two Stages, Across Multiple Racial/Ethnic Groups? Du Bois Rev. 2011, 8, 159–178. [Google Scholar] [CrossRef]
- Ren, X.S.; Amick, B.C.; Williams, D.R. Racial/Ethnic Disparities in Health: The Interplay between Discrimination and Socioeconomic Status. Ethn. Dis. 1999, 9, 151–165. [Google Scholar]
- Williams, D.R.; Mohammed, S.A. Discrimination and Racial Disparities in Health: Evidence and Needed Research. J. Behav. Med. 2009, 32, 20–47. [Google Scholar] [CrossRef]
- Pavalko, E.K.; Mossakowski, K.N.; Hamilton, V.J. Does Perceived Discrimination Affect Health? Longitudinal Relationships between Work Discrimination and Women’s Physical and Emotional Health. J. Health Soc. Behav. 2003, 44, 18–33. [Google Scholar] [CrossRef] [PubMed]
- Hogan, T.P.; Benjamin, A.; Brezinski, K.L. Reliability Methods: A Note on the Frequency of Use of Various Types. Educ. Psychol. Meas. 2000, 60, 523–531. [Google Scholar] [CrossRef]
- Novick, M.R.; Lewis, C. Coefficient Alpha and the Reliability of Composite Measurements. Psychometrika 1967, 32, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Becker, G. How Important Is Transient Error in Estimating Reliability? Going Beyond Simulation Studies. Psychol. Methods 2000, 5, 370–379. [Google Scholar] [CrossRef]
- Adams, J.P.; Dressler, W.W. Perceptions of Injustice in a Black Community: Dimensions and Variation. Human. Relat. 1988, 41, 753. [Google Scholar] [CrossRef]
- Battauz, M.; Bellio, R. Structural Modeling of Measurement Error in Generalized Linear Models with Rasch Measures as Covariates. Psychometrika 2011, 76, 40–56. [Google Scholar] [CrossRef]
- Klonoff, E.A.; Landrine, H.; Ullman, J.B. Racial Discrimination and Psychiatric Symptoms among Blacks. Cult. Divers. Ethn. Minor. Psychol. 1999, 5, 329–339. [Google Scholar] [CrossRef]
- Landrine, H.; Klonoff, E.; Corral, I.; Fernandez, S.; Roesch, S. Conceptualizing and Measuring Ethnic Discrimination in Health Research. J. Behav. Med. 2006, 29, 79–94. [Google Scholar] [CrossRef] [PubMed]
- Lucke, J.F. The α and the ω of Congeneric Test Theory: An Extension of Reliability and Internal Consistency to Heterogeneous Tests. Appl. Psychol. Meas. 2005, 29, 65–81. [Google Scholar] [CrossRef]
- Raykov, T.; Shrout, P.E. Reliability of Scales with General Structure: Point and Interval Estimation Using a Structural Equation Modeling Approach. Struct. Equ. Model. 2002, 9, 195–212. [Google Scholar] [CrossRef]
- Pachter, L.M.; Szalacha, L.A.; Bernstein, B.A.; Garcia Coll, C. Perceptions of Racism in Children and Youth (PRaCY): Properties of a Self-Report Instrument for Research on Children’s Health and Development. Ethn. Health 2010, 15, 36–46. [Google Scholar] [CrossRef] [PubMed]
- Essed, P. Understanding Everyday Racism: An Interdisciplinary Theory; Sage: Newbury Park, CA, USA, 1991. [Google Scholar] [CrossRef]
- Utsey, S.O.; Ponterotto, J.G. Development and Validation of the Index of Race-Related Stress (IRRS). J. Couns. Psychol. 1996, 43, 490–501. [Google Scholar] [CrossRef]
- Barnes, L.L.; Lewis, T.T.; Begeny, C.T.; Yu, L.; Bennett, D.A.; Wilson, R.S. Perceived Discrimination and Cognition in Older African Americans. J. Int. Neuropsychol. Soc. 2012, 18, 856–865. [Google Scholar] [CrossRef]
- Seabra, D.; Gato, J.; Petrocchi, N.; Carreiras, D.; Azevedo, J.; Martins, L.; Salvador, M.D.C. Everyday Discrimination Scale: Dimensionality in a Portuguese Community Sample and Specific Versions for Sexual and Gender Minority. Curr. Psychol. 2024, 43, 10850–10861. [Google Scholar] [CrossRef]
- Kazmierski, K.F.M.; Borelli, J.L.; Rao, U. Multidimensional Discrimination Distress, Controlling Parenting, and Parent-Adolescent Attachment Relationships: Racial/Ethnic Differences. J. Soc. Issues 2023, 79, 334–359. [Google Scholar] [CrossRef]
- Harnois, C.E. What Do We Measure When We Measure Perceptions of Everyday Discrimination? Soc. Sci. Med. 2022, 292, 114609. [Google Scholar] [CrossRef]
- Burgos, G.; Trillo, A.F. Latino Youth. In Blackwell Encyclopedia of Sociology; Ritzer, G., Ed.; Blackwell Publishers: Malden, MA, USA, 2016. [Google Scholar] [CrossRef]
- UCLA Latino Policy & Politics Institute. A Mosaic, Not a Monolith: A Profile of the U.S. Latino Population, 2000–2020. 2022. Available online: https://latino.ucla.edu/research/latino-population-2000-2020/ (accessed on 20 October 2025).
- U.S. Census Bureau. Hispanic Heritage Month 2025: Facts for Features. 2025. Available online: https://www.census.gov/newsroom/facts-for-features/2025/hispanic-heritage-month.html (accessed on 15 October 2025).
- González, J. Harvest of Empire: A History of Latinos in America, 2nd ed.; Penguin Books: New York, NY, USA, 2022. [Google Scholar]
- Feagin, J.R.; Cobas, J.A. Latinos Facing Racism: Discrimination, Resistance, and Endurance; Paradigm Publishers: Boulder, CO, USA, 2014. [Google Scholar] [CrossRef]
- Piña, G.; Martinez, G. Key Facts About U.S. Latinos. 2025. Available online: https://www.pewresearch.org/short-reads/2025/10/22/key-facts-about-us-latinos/ (accessed on 15 November 2025).
- Acuña, R. Occupied America: A History of Chicanos, 2nd ed.; Harper Collins Publishers: New York, NY, USA, 1981. [Google Scholar]
- Santiago, A.A.L.; Berg, U.D. Latinas/OS in New Jersey: Histories, Communities, and Cultures; Rutgers University Press: New Brunswick, NJ, USA, 2025. [Google Scholar]
- U.S. Census Bureau. Selected Population Profile. American Community Survey l Year Estimates, Table SO2O1. Available online: https://data.census.gov/table/ACSSPP1Y2010.S0201?t=-09 (accessed on 15 September 2025).
- Duany, J. Puerto Rico: What Everyone Needs to Know; Oxford University Press: New York, NY, USA, 2024. [Google Scholar] [CrossRef]
- Vélez, W.; Burgos, G. The Impact of Housing Segregation and Structural Factors on the Socioeconomic Performance of Puerto Ricans in the United States. Cent. J. Cent. Puerto Rican Stud. 2010, 22, 174–197. [Google Scholar]
- Logan, J.R.; Alba, R.D.; McNulty, T.L. Minorities in Global Cities: New York and Los Angeles; Urban Poverty and the Underclass; Mingione, E., Ed.; Wiley-Blackwell: Oxford, UK, 1996. [Google Scholar] [CrossRef]
- Moslimani, M.; Noe-Bustamante, L.; Shah, S. Puerto Ricans in the U.S. Pew Research Center. 2023. Available online: https://www.pewresearch.org/race-and-ethnicity/fact-sheet/us-hispanics-facts-on-puerto-rican-origin-latinos/ (accessed on 20 June 2025).
- Bardach, A.L. Wet Foot, Dry Foot … Wrong Foot. In The New Latino Studies Reader: A Twenty-First-Century Perspective; Gutiérrez, R.A., Almaguer, T., Eds.; University of California Press: Oakland, CA, USA, 2016; p. 622. [Google Scholar]
- Eckstein, S. The Immigrant Divide: How Cuban Americans Changed the U.S. and Their Homeland; Routledge: New York, NY, USA, 2009. [Google Scholar] [CrossRef]
- Burgos, G.; Trillo, A.F.; Venkatesh, A. Latino Segregation across New Jersey Counties: Are Latino Groups Becoming More or Less Residentially Segregated during the Last Four Decades? In Latinas/os in New Jersey: Histories, Communities, and Cultures; Lauria-Santiago, A., Berg, U., Eds.; Rutgers University Press: New Brunswick, NJ, USA, 2025. [Google Scholar]
- Kami, H. Diplomacy Meets Migration: US Relations with Cuba During the Cold War; Cambridge University Press: Cambridge, UK, 2018. [Google Scholar] [CrossRef]
- Burgos, G.; Rivera, F. The (In)Significance of Race and Discrimination among Latino Youth: The Case of Adolescent Depression. Soc. Focus 2009, 42, 29–50. [Google Scholar] [CrossRef][Green Version]
- Findling, M.G.; Bleich, S.N.; Casey, L.S.; Blendon, R.J.; Benson, J.M.; Sayde, J.M.; Miller, C. Discrimination in the United States: Experiences of Latinos. Health Serv. Res. 2019, 54 (Suppl. S2), 1409–1418. [Google Scholar] [CrossRef] [PubMed]
- Cano, M.; Perez Portillo, A.G.; Figuereo, V.; Rahman, A.; Reyes-Martínez, J.; Rosales, R.; Ángel Cano, M.; Salas-Wright, C.P.; Takeuchi, D.T. Experiences of Ethnic Discrimination Among US Hispanics: Intersections of Language, Heritage, and Discrimination Setting. Int. J. Intercult. Relat. 2021, 84, 233–250. [Google Scholar] [CrossRef] [PubMed]
- Marrow, H.B.; Okamoto, D.G.; García, M.J.; Adem, M.; Tropp, L.R. Skin Tone and Mexicans’ Perceptions of Discrimination in New Immigrant Destinations. Soc. Psychol. Q. 2022, 85, 374–385. [Google Scholar] [CrossRef]
- Odame, E.A.; Elhabashy, M.; Adzrago, D.; Chiangong, J.; Ormiston, C.K.; Williams, F. Mental Health Symptoms and Discrimination among Immigrant and US-Born Hispanic or Latino Adults during the COVID-19 Pandemic. BMC Psychol. 2025, 13, 504. [Google Scholar] [CrossRef]
- Andrade, N.; Ford, A.D.; Alvarez, C. Discrimination and Latino Health: A Systematic Review of Risk and Resilience. Hisp. Health Care Int. 2021, 19, 5–16. [Google Scholar] [CrossRef]
- Kim, S.; Lee, H.; Konlan, K.D. The Recent Trends in Discrimination and Health among Ethnic Minority Adolescents: An Integrative Review. BMC Public Health 2025, 25, 861. [Google Scholar] [CrossRef]
- Cobb, C.L.; Salas-Wright, C.P.; John, R.; Schwartz, S.J.; Vaughn, M.; Martínez, C.R.; Awad, G.; Pinedo, M.; Cano, M.Á. Discrimination Trends and Mental Health Among Native- and Foreign-Born Latinos: Results from National Surveys in 2004 and 2013. Prev. Sci. 2021, 22, 397–407. [Google Scholar] [CrossRef]
- Sabater Minarim, D.; Morgan, K.M.; Buckley, K.; Riviere, P.; Ochoa, C.; Deshler, L.N.; Duran, E.A.; Mehtsun, W.T.; Rose, B.S.; Banegas, M.P. Racial and Ethnic Disparities in Perceived Healthcare Discrimination and Health Outcomes. J. Gen. Intern. Med. 2025, 40, 2548–2557. [Google Scholar] [CrossRef]
- Massey, D.S.; Denton, N.A. American Apartheid: Segregation and the Making of the Underclass; Harvard University Press: Cambridge, MA, USA, 1993. [Google Scholar]
- Pettigrew, T.F.; Meertens, R.W. Subtle and Blatant Prejudice in Western Europe. Eur. J. Soc. Psychol. 1995, 25, 57–75. [Google Scholar] [CrossRef]
- Hamler, T.C.; Nguyen, A.W.; Keith, V.; Qin, W.; Wang, F. How Skin Tone Influences Relationships Between Discrimination, Psychological Distress, and Self-Rated Mental Health Among Older African Americans. J. Gerontol. B Psychol. Sci. Soc. Sci. 2022, 77, 2026–2037. [Google Scholar] [CrossRef] [PubMed]
- Monk, E.P. The Cost of Color: Skin Color, Discrimination, and Health among African-Americans. Am. J. Sociol. 2015, 121, 396–444. [Google Scholar] [CrossRef] [PubMed]
- Hunter, M. The Persistent Problem of Colorism: Skin Tone, Status, and Inequality. Sociol. Compass 2007, 1, 237–254. [Google Scholar] [CrossRef]
- Stanke, F.A.; Kuper, N.; Fetz, K.; Echterhoff, G. Discriminatory, yet Socially Accepted? Targets’ Perceptions of Subtle and Blatant Expressions of Ethno-Racial Prejudice. Front. Soc. Psychol. 2024, 2, 1343514. [Google Scholar] [CrossRef]
- Heeringa, S.G.; Wagner, J.; Torres, M.; Duan, N.; Adams, T.; Berglund, P. Sample Designs and Sampling Methods for the Collaborative Psychiatric Epidemiology Studies (CPES). Int. J. Methods Psychiatr. Res. 2004, 13, 221–240. [Google Scholar] [CrossRef]
- Berglund, P. Analysis of Complex Survey Data and Survival Analysis. CPES Training. 2008. Available online: https://www.slideserve.com/aric/analysis-of-complex-survey-data-and-survival-analysis (accessed on 31 March 2025).
- Asparouhov, T. Sampling Weights in Latent Variable Modeling. Struct. Equ. Model. A Multidiscip. J. 2005, 12, 411–434. [Google Scholar] [CrossRef]
- Landrine, H.; Klonoff, E.A. The Schedule of Racist Events: A Measure of Discrimination and a Study of Its Negative Physical and Mental Health Consequences. J. Black Psychol. 1996, 22, 144–168. [Google Scholar] [CrossRef]
- Pearlin, L.I.; Bierman, A. Current Issues and Future Directions in Research into the Stress Process. In Handbook of the Sociology of Mental Health; Aneshensel, C.S., Phelan, J.C., Bierman, A., Eds.; Springer: New York, NY, USA, 2013; pp. 325–340. [Google Scholar] [CrossRef]
- Burgess, R.A.; Chobhthaigh, S.N.; Biswal, B.; Ceccolini, D.; Fadipe, B.; Khan, D.; Aggarwal, N.; Pabla, I.; Solis, C.; Pillutla, R. Intersectional Discrimination, Exclusion and the Socio-Political Economy of Global Mental Health: A Systematic Scoping Review of the Literature. SSM Ment. Health 2025, 7, 100382. [Google Scholar] [CrossRef]
- Lee, J.H.; Lee, H.; Son, Y.; Kim, H.J.; Park, J.; Lee, H.; Fond, G.; Boyer, L.; Smith, L.; Rahmati, M. Racial Discrimination and Multiple Health Outcomes: An Umbrella Review of Systematic Reviews and Meta-Analyses. Med. Princ. Pract. 2025, 34, 138–151. [Google Scholar] [CrossRef] [PubMed]
- Blodgett, J.M.; Lachance, C.C.; Stubbs, B.; Co, M.; Wu, Y.-T.; Prina, M.; Tsang, V.W.L.; Cosco, T.D. A Systematic Review of the Latent Structure of the Center for Epidemiologic Studies Depression Scale (CES-D) amongst Adolescents. BMC Psychiatry 2021, 21, 197. [Google Scholar] [CrossRef] [PubMed]
- Radloff, L.S. The CES-D Scale. A Self-Report Depression Scale for Research in the General Population. Appl. Psychol. Meas. 1977, 1, 385–401. [Google Scholar] [CrossRef]
- Dimitrov, D.M. Comparing Groups on Latent Variables: A Structural Equation Modeling Approach. Work A J. Prev. Assess. Rehabil. 2006, 26, 429–436. [Google Scholar] [CrossRef]
- Springer, K.W.; Hauser, R.M. An Assessment of the Construct Validity of Ryff’s Scales of Psychological Well-Being: Method, Mode, and Measurement Effects. Soc. Sci. Res. 2006, 35, 1080–1102. [Google Scholar] [CrossRef]
- West, S.G.; Finch, J.F.; Curran, P.J. Structural Equation Models with Nonnormal Variables: Problems and Remedies. In Structural Equation Modeling: Concepts, Issues, and Application; Hoyle, R.H., Ed.; Sage: Thousand Oaks, CA, USA, 1995; pp. 56–75. [Google Scholar]
- Green, S.B.; Akey, T.M.; Fleming, K.K. Effect of the Number of Scale Points on Chi-Square Fit Indices in Confirmatory Factor Analysis. Struct. Equ. Model. 1997, 4, 108–120. [Google Scholar] [CrossRef]
- Finch, J.F.; West, S.G.; MacKinnon, D.P. Effects of Sample Size and Nonnormality on the Estimation of Mediated Effects in Latent Variable Models. Struct. Equ. Model. A Multidiscip. J. 1997, 4, 87–107. [Google Scholar] [CrossRef]
- Archibald, C.; Takamasa, E.J.; Fraser, A.M.; Metcalf, M.W.; Rogers, A.A.; Bean, R.A. Sticks and Stones May Break Bones, But Racism Breaks Spirits: Discrimination and BIPOC Adolescent Mental Health. Youth Soc. 2025, 57, 304–329. [Google Scholar] [CrossRef]
- Simmons, A.; Vasquez, A.; Green, K.; Christopher, M.; Colgan, D.D. The Impact of Ethnic Discrimination on Chronic Pain: The Role of Sex and Depression. Ethn. Health 2023, 28, 1053–1068. [Google Scholar] [CrossRef]
- Gee, G.C.; Spencer, M.S.; Chen, J.; Takeuchi, D. A Nationwide Study of Discrimination and Chronic Health Conditions among Asian Americans. Am. J. Public Health 2007, 97, 1275–1282. [Google Scholar] [CrossRef] [PubMed]
- Finch, B.K.; Hummer, R.A.; Kol, B.; Vega, W.A. The Role of Discrimination and Acculturative Stress in the Physical Health of Mexican Origin Adults. Hisp. J. Behav. Sci. 2001, 23, 399–429. [Google Scholar] [CrossRef]
- Quan, Y.; Wang, C. Collapsing or Not? A Practical Guide to Handling Sparse Responses for Polytomous Items. Methodology 2025, 21, 46–73. [Google Scholar] [CrossRef]
- DiStefano, C.; Shi, D.; Morgan, G.B. Collapsing Categories Is Often More Advantageous than Modeling Sparse Data: Investigations in the CFA Framework. Struct. Equ. Model. A Multidiscip. J. 2021, 28, 237–249. [Google Scholar] [CrossRef]
- Rhemtulla, M.; Brosseau-Liard, P.É.; Savalei, V. When Can Categorical Variables Be Treated as Continuous? A Comparison of Robust Continuous and Categorical SEM Estimation Methods under Suboptimal Conditions. Psychol. Methods 2012, 17, 354–373. [Google Scholar] [CrossRef]
- Lawrence, J.A.; Kawachi, I.; White, K.; Bassett, M.T.; Priest, N.; Masunga, J.G.; Cory, H.J.; Mita, C.; Williams, D.R. A Systematic Review and Meta-Analysis of the Everyday Discrimination Scale and Biomarker Outcomes. Psychoneuroendocrinology 2022, 142, 105772. [Google Scholar] [CrossRef] [PubMed]
- Pérez, D.J.; Fortuna, L.; Alegría, M. Prevalence and Correlates of Everyday Discrimination among U.S. Latinos. J. Community Psychol. 2008, 36, 421–433. [Google Scholar] [CrossRef]
- Ulusoy, N.; Nienhaus, A.; Brzoska, P. Investigating Discrimination in the Workplace. Translation and Validation of the Everyday Discrimination Scale for Nursing Staff in Germany. BMC Nurs. 2023, 22, 196. [Google Scholar] [CrossRef] [PubMed]
- Greenfield, B.L.; Elm, J.H.L.; Hallgren, K.A. Understanding Measures of Racial Discrimination and Microaggressions among American Indian and Alaska Native College Students in the Southwest United States. BMC Public Health 2021, 21, 1099. [Google Scholar] [CrossRef]
- Miguel-Alvaro, A.; Rodríguez-Medina, J.; González-Sanguino, C. Spanish Version of the Everyday Discrimination Scale (EDS-E): Factorial Structure and Scale Invariance in Spanish Adolescents. J. Clin. Med. 2025, 14, 2887. [Google Scholar] [CrossRef]
- Clark, R.; Coleman, A.P.; Novak, J.D. Brief Report: Initial Psychometric Properties of the Everyday Discrimination Scale in Black Adolescents. J. Adolesc. 2004, 27, 363–368. [Google Scholar] [CrossRef] [PubMed]
- Lewis, T.T.; Yang, F.M.; Jacobs, E.A.; Fitchett, G. Racial/Ethnic Differences in Responses to the Everyday Discrimination Scale: A Differential Item Functioning Analysis. Am. J. Epidemiol. 2012, 175, 391–401. [Google Scholar] [CrossRef] [PubMed]
- Kim, G.; Sellbom, M.; Ford, K.-L. Race/Ethnicity and Measurement Equivalence of the Everyday Discrimination Scale. Psychol. Assess. 2014, 26, 892–900. [Google Scholar] [CrossRef]
- Stucky, B.D.; Gottfredson, N.C.; Panter, A.T.; Daye, C.E.; Allen, W.R.; Wightman, L.F. An Item Factor Analysis and Item Response Theory-Based Revision of the Everyday Discrimination Scale. Cultur. Divers. Ethn. Minor. Psychol. 2011, 17, 175–185. [Google Scholar] [CrossRef]
- Feng, Y.; Cheon, Y.M.; Yip, T.; Cham, H. Multilevel IRT Analysis of the Everyday Discrimination Scale and the Racial/Ethnic Discrimination Index. Psychol. Assess. 2021, 33, 637–651. [Google Scholar] [CrossRef]
- Park, I.J.K.; Wang, L.; Williams, D.R.; Alegría, M. Coping with Racism: Moderators of the Discrimination-Adjustment Link Among Mexican-Origin Adolescents. Child. Dev. 2018, 89, e293–e310. [Google Scholar] [CrossRef] [PubMed]
- Pérez, D.; Sribney, W.M.; Rodríguez, M.A. Perceived Discrimination and Self-Reported Quality of Care among Latinos in the United States. J. Gen. Intern. Med. 2009, 24 (Suppl. S3), 548–554. [Google Scholar] [CrossRef]
- Lee, M.-A.; Ferraro, K.F. Perceived Discrimination and Health among Puerto Rican and Mexican Americans: Buffering Effect of the Lazo Matrimonial. Soc. Sci. Med. 2009, 68, 1966–1974. [Google Scholar] [CrossRef]
- StataCorp. Stata Statistical Software: Release 17, 17th ed.; Stata Corporation: College Station, TX, USA, 2021. [Google Scholar]
- King, M.; Goh, K.-L. Improvements to the Wald Test. In Handbook of Applied Econometrics and Statistical Inference; Ullah, A., Wan, A.T.K., Chaturvedi, A., Eds.; Marcel Dekker: New York, NY, USA, 2002; Chapter 12. [Google Scholar] [CrossRef]
- Long, S.J. Regression Models for Categorical and Limited Dependent Variables; Berk, R., Ed.; Advanced Quantitative Techniques; Sage: Thousand Oaks, CA, USA, 1997; Volume 7. [Google Scholar] [CrossRef]
- Muthén, L.K.; Muthén, B.O. Mplus Statistical Analysis with Latent Variables: User’s Guide; Muthén & Muthén: Los Angeles, CA, USA, 2023. [Google Scholar]
- Raykov, T.; Marcoulides, G.A. A First Course in Structural Equation Modeling, 2nd ed.; Lawrence Erlbaum Associates: Mahwah, NJ, USA, 2006. [Google Scholar] [CrossRef]
- Bentler, P.M. Comparative Fit Indexes in Structural Models. Psychol. Bull. 1990, 107, 238–246. [Google Scholar] [CrossRef]
- MacCallum, R.C.; Browne, M.W.; Sugawara, H.M. Power Analysis and Determination of Sample Size for Covariance Structure Modeling. Psychol. Methods 1996, 1, 130–149. [Google Scholar] [CrossRef]
- Steiger, J.H. Structural Model Evaluation and Modification: An Interval Estimation Approach. Multivar. Behav. Res. 1990, 25, 173–180. [Google Scholar] [CrossRef] [PubMed]
- Raftery, A.E. Bayesian Model Selection in Structural Equation Models. In Testing Structural Equation Models; Bollen, K.A., Ed.; Sage Publications: Newbury Park, CA, USA, 1993; pp. 163–180. [Google Scholar]
- Muthén, B.O.; Satorra, A. Complex Sample Data in Structural Equation Modeling. Sociol. Methodol. 1995, 25, 267–316. [Google Scholar] [CrossRef]
- Raykov, T. Bias-Corrected Estimation of Noncentrality Parameters of Covariance Structure Models. Struct. Equ. Model. A Multidiscip. J. 2005, 12, 120–129. [Google Scholar] [CrossRef]
- Raykov, T. On the Large-Sample Bias, Variance, and Mean Squared Error of the Conventional Noncentrality Parameter Estimator of Covariance Structure Models. Struct. Equ. Model. 2000, 7, 431–441. [Google Scholar] [CrossRef]
- Bonilla-Silva, E.; Dietrich, D. The Sweet Enchantment of Color-Blind Racism in Obamerica. Ann. Am. Acad. Political Sci. 2011, 634, 190–206. [Google Scholar] [CrossRef]
- Huynh, V.W. Ethnic Microaggressions and the Depressive and Somatic Symptoms of Latino and Asian American Adolescents. J. Youth Adolesc. 2012, 41, 831–846. [Google Scholar] [CrossRef]
- Hardeman, R.R.; Homan, P.A.; Chantarat, T.; Davis, B.A.; Brown, T.H. Improving the Measurement of Structural Racism to Achieve Antiracist Health Policy. Health Aff. 2022, 41, 179–186. [Google Scholar] [CrossRef]
- Gordon, I. Trump’s Immigration Police State Is Growing at Warp Speed. Mother Jones, 13 September 2025. Available online: https://www.motherjones.com/politics/2025/09/trump-287g-local-police-deportation-detention-ice/ (accessed on 2 October 2025).
- Hayes, G. Trump’s White Nationalist Agenda, Explained. Mother Jones, February 2025. Available online: https://www.motherjones.com/politics/2025/02/trumps-white-nationalist-agenda-explained/ (accessed on 15 May 2025).
- Yearby, R.; Lewis, C.; Gibson, C. Incorporating Structural Racism, Employment Discrimination, and Economic Inequities in the Social Determinants of Health Framework to Understand Agricultural Worker Health Inequities. Am. J. Public Health 2023, 113, S65–S71. [Google Scholar] [CrossRef]
- Zsembik, B.A.; Fennell, D. Ethnic Variation in Health and the Determinants of Health among Latinos. Soc. Sci. Med. 2005, 61, 53–63. [Google Scholar] [CrossRef]
- Paradies, Y.C.; Cunningham, J. Development and Validation of the Measure of Indigenous Racism Experiences (MIRE). Int. J. Equity Health 2008, 7, 9. [Google Scholar] [CrossRef]
- Roth, W.D. “There Is No Racism Here”: Understanding Latinos Perceptions of Color Discrimination Through Sending-Receiving Society Comparison. In Racism in the 21st Century: An Empirical Analysis of Skin Color; Hall, R.E., Ed.; Springer: New York, NY, USA, 2008; pp. 205–234. [Google Scholar] [CrossRef]
- Fuentes-Mayorga, N.; Burgos, G. Generation X and the Future Health of Latinos. Gener. J. Am. Soc. Aging 2017, 41, 58–67. [Google Scholar]
- Burgos, G.; Trillo, A.F. Stress and Health. In The Wiley Blackwell Encyclopedia of Health, Illness, Behavior, and Society; Cockerham, W.C., Gabe, J., Quah, S., Ryan, J.M., Eds.; John Wiley & Sons: Chichester, UK, 2025. [Google Scholar] [CrossRef]
- McNeilly, M.D.; Anderson, N.B.; Armstead, C.A.; Clark, R.; Corbett, M.; Robinson, E.L.; Pieper, C.F.; Lepisto, E.M. The Perceived Racism Scale: A Multidimensional Assessment of the Experience of White Racism among African Americans. Ethn. Dis. 1996, 6, 154–166. [Google Scholar] [PubMed]
- Poteat, V.P.; Spanierman, L.B. Further Validation of the Psychosocial Costs of Racism to Whites Scale Among Employed Adults. Couns. Psychol. 2008, 36, 871–894. [Google Scholar] [CrossRef]
- Forman, T.A. The Social Psychological Costs of Racial Segmentation in the Workplace: A Study of African Americans’ Well-Being. J. Health Soc. Behav. 2003, 44, 332–352. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Shariff-Marco, S.; Ellis, E.; Sangaramoorthy, M.; Jain, J.; Thomsen, C.; Ambrosone, C.; Kushi, L.; Kroenke, C.; Gomez, S.L. Abstract B040: The Impact of Racial/Ethnic Discrimination and Residential Segregation on Cancer Survivorship. Cancer Epidemiol. Biomark. Prev. 2020, 29 (Suppl. S1), B040. [Google Scholar] [CrossRef]
| Cubans | Puerto Ricans | Mexicans | Other Latinos | All Latinos | |
|---|---|---|---|---|---|
| N = 577 | N = 495 | N = 868 | N = 614 | N = 2554 | |
| Dependent Variables | |||||
| Depressive Symptoms | 0.153 | 0.185 M, O | 0.133 | 0.13 | 1.146 |
| Chronic Physical Health (1 = yes, 0 = no) | 0.651 M | 0.680 M, O | 0.564 | 0.589 | 0.587 |
| Perceived Discrimination | |||||
| Courtesy | 1.911 P, M, O | 2.470 M | 2.176 | 2.272 | 2.29 |
| Disrespect | 1.761 P, M, O | 2.225 M | 2.039 | 2.065 | 2.129 |
| Service | 1.647 P, M, O | 2.083 M, O | 1.887 | 1.875 | 1.964 |
| Not Smart | 1.644 P, M, O | 2.220 M | 1.99 | 2.013 | 2.101 |
| Afraid | 1.458 P, M, O | 1.956 M, O | 1.641 | 1.822 | 1.807 |
| Dishonest | 1.404 P, M, O | 1.821 M | 1.596 | 1.677 | 1.699 |
| Better | 1.557 P, M, O | 2.092 M | 1.883 | 1.969 | 1.993 |
| Insult | 1.321 P, M, O | 1.747 | 1.594 | 1.608 | 1.677 |
| Harassed | 1.222 P, M, O | 1.539 M | 1.343 | 1.414 | 1.436 |
| Background Variables | |||||
| Age | 38.3 | 37.9 | 37.4 | 37.9 | 37.6 |
| Gender (1 = Male) | 0.517 | 0.516 | 0.522 | 0.523 | 0.521 |
| Marital Status | |||||
| Married/Cohabitating (unmarried) | 0.608 M, O | 0.542 M | 0.691 O | 0.575 | 0.639 |
| Divorced | 0.165 | 0.169 | 0.121 O | 0.168 | 0.141 |
| Never Married | 0.226 | 0.288 M, | 0.186 O | 0.256 | 0.218 |
| Educational status | |||||
| High school or less | 0.205 P, M, O | 0.316 M | 0.522 O | 0.341 | 0.434 |
| High school graduate | 0.272 | 0.305 M | 0.244 | 0.241 | 0.251 |
| Some college | 0.267 M | 0.266 M | 0.159 O | 0.28 | 0.21 |
| College graduate or more | 0.254 P, M, O | 0.112 M | 0.072 O | 0.137 | 0.104 |
| Household income | |||||
| Less than $15,000 | 0.218 | 0.248 | 0.296 | 0.235 | 0.27 |
| $15,000–$35,000 | 0.237 M | 0.225 M | 0.308 | 0.261 | 0.283 |
| $35–$75,000 | 0.26 | 0.298 | 0.259 | 0.313 | 0.279 |
| $75,000 or more | 0.283 M | 0.227 M | 0.134 | 0.189 | 0.166 |
| Employed | 0.67 | 0.612 | 0.621 | 0.657 | 0.633 |
| Unemployed | 0.064 | 0.071 | 0.071 | 0.086 | 0.076 |
| Not in labor force | 0.265 | 0.315 | 0.307 | 0.255 | 0.291 |
| English language proficiency (1 = Yes) | 0.502 P | 0.657 M, O | 0.404 O | 0.518 | 0.467 |
| Generational Status | |||||
| First Generation or Foreign Born | 0.761 P, M, O | 0.405 M, O | 0.563 | 0.608 | 0.57 |
| Second Generation | 0.232 P | 0.369 M, O | 0.22 | 0.168 | 0.221 |
| Third Generation | 0.006 P, M, O | 0.224 | 0.215 | 0.222 | 0.208 |
| Strong Ethnic Identity (1 = Yes) | 0.919 M, O | 0.88 | 0.86 | 0.854 | 0.863 |
| Continuous Factor Indicators | Categorical Factor Indicators | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| χ2 | DF | RMSEA | CFI | BIC | χ2 | DF | RMSEA | CFI | |
| L-1. Single Factor Model | 561.149 * | 27 | 0.090 | 0.874 | 48,044.608 | 1128.780 * | 27 | 0.129 | 0.968 |
| L-2. Single Factor Model w/correlated errors | 139.758 * | 24 | 0.044 | 0.973 | 46,474.553 | 274.270 * | 24 | 0.065 | 0.993 |
| L-3. Two Factor Model | 344.856 * | 26 | 0.071 | 0.925 | 47,157.945 | 607.333 * | 26 | 0.095 | 0.983 |
| L-4. Two Factor Model w/correlated errors | 49.477 * | 23 | 0.022 | 0.994 | 46,144.285 | 70.248 * | 23 | 0.029 | 0.999 |
| L-5. Second-order factor | 369.194 * | 27 | 0.072 | 0.919 | 47,196.792 | 1427.927 * | 27 | 0.145 | 0.959 |
| L-6. Second-order factor w/correlated errors | 84.690 * | 24 | 0.032 | 0.986 | 46,250.991 | 1311.529 * | 24 | 0.148 | 0.963 |
| C-1. Single Factor Model | 182.617 | 27 | 0.101 | 0.794 | 9593.038 | 207.774 * | 27 | 0.109 | 0.952 |
| C-2. Single Factor Model w/correlated errors | 62.724 | 21 | 0.059 | 0.946 | 9077.138 | 65.808 * | 21 | 0.062 | 0.988 |
| C-3. Two Factor Model | 115.896 | 26 | 0.078 | 0.881 | 9278.403 | 138.964 * | 26 | 0.088 | 0.970 |
| C-4. Two Factor Model w/correlated errors | 52.400 | 22 | 0.049 | 0.960 | 9020.822 | 50.916 * | 22 | 0.048 | 0.992 |
| C-5. Second-order factor | 122.890 | 27 | 0.079 | 0.873 | 9293.591 | 292.358 * | 27 | 0.132 | 0.930 |
| C-6. Second-order factor w/correlated errors | 62.669 | 23 | 0.055 | 0.948 | 9048.521 | 231.752 * | 23 | 0.127 | 0.945 |
| M-1. Single Factor Model | 298.996 | 27 | 0.110 | 0.880 | 16,016.956 | 473.407 * | 27 | 0.141 | 0.973 |
| M-2. Single Factor Model w/correlated errors | 91.125 | 24 | 0.058 | 0.970 | 15,557.183 | 129.071 * | 24 | 0.073 | 0.994 |
| M-3. Two Factor Model | 190.680 | 26 | 0.087 | 0.928 | 15,750.638 | 250.542 * | 26 | 0.102 | 0.986 |
| M-4. Two Factor Model w/correlated errors | 41.129 | 23 | 0.046 | 0.992 | 15,445.714 | 46.649 * | 23 | 0.035 | 0.999 |
| M-5. Second-order factor | 204.299 | 27 | 0.089 | 0.922 | 15,762.364 | 606.527 * | 27 | 0.161 | 0.964 |
| M-6. Second-order factor w/correlated errors | 60.169 | 24 | 0.043 | 0.984 | 15,479.137 | 531.809 * | 24 | 0.159 | 0.969 |
| P-1. Single Factor Model | 187.105 | 27 | 0.112 | 0.830 | 9805.920 | 210.462 * | 27 | 0.120 | 0.956 |
| P-2. Single Factor Model w/correlated errors | 69.626 | 24 | 0.064 | 0.952 | 9523.171 | 100.542 * | 24 | 0.082 | 0.982 |
| P-3. Two Factor Model | 119.367 | 26 | 0.088 | 0.901 | 9658.646 | 138.299 * | 26 | 0.096 | 0.973 |
| P-4. Two Factor Model w/correlated errors | 43.997 | 23 | 0.044 | 0.978 | 9473.655 | 51.050 * | 23 | 0.051 | 0.993 |
| P-5. Second-order factor | 128.591 | 27 | 0.09 | 0.892 | 9671.849 | 237.946 * | 27 | 0.129 | 0.949 |
| P-6. Second-order factor w/correlated errors | 60.606 | 24 | 0.057 | 0.961 | 9505.863 | 206.941 * | 24 | 0.127 | 0.956 |
| O-1. Single Factor Model | 183.956 | 27 | 0.099 | 0.855 | 11,874.541 | 365.420 * | 27 | 0.146 | 0.954 |
| O-2. Single Factor Model with correlated errors | 45.425 | 24 | 0.039 | 0.980 | 11,399.613 | 104.958 * | 24 | 0.076 | 0.989 |
| O-3. Two Factor Model | 116.268 | 26 | 0.077 | 0.917 | 11,623.695 | 206.398 * | 26 | 0.108 | 0.976 |
| O-4. Two Factor Model w/correlated errors | 23.565 | 23 | 0.006 | 0.999 | 11,327.920 | 40.410 * | 23 | 0.036 | 0.998 |
| O-5. Second-order factor | 121.909 * | 27 | 0.077 | 0.912 | 11,629.806 | 405.408 * | 27 | 0.154 | 0.949 |
| O-6. Second-order factor with correlated errors | 32.499 | 24 | 0.024 | 0.992 | 11,350.686 | 384.518 * | 24 | 0.159 | 0.951 |
| Alpha Scale (Model 1) | Single Factor (Model 2) | Single Factor Model with Correlated Errors (Model 3) | Two Factor Model (Model 4) | Two Factor Model with Correlated Errors (Model 5) | Second Order Factor (Model 6) | Second Order Factor with Correlated Errors (Model 7) | |||
|---|---|---|---|---|---|---|---|---|---|
| Subtle Mistreatment | Blatant Mistreatment | Subtle Mistreatment | Blatant Mistreatment | ||||||
| All Latinos | 0.136 *** (0.046) | 0.135 *** (0.034) | 0.139 *** (0.042) | 0.074 (0.082) | 0.067 (0.094) | 0.088 (0.155) | 0.055 (0.153) | 0.141 *** (0.031) | 0.143 *** (0.032) |
| Cubans | 0.144 (0.140) | 0.128 * (0.072) | 0.131 * (0.178) | 0.104 (0.165) | 0.060 (0.191) | 0.113 (0.391) | 0.020 (0.385) | 0.134 * (0.066) | 0.195 * (0.066) |
| Mexicans | 0.148 *** (0.058) | 0.156 *** (0.040) | 0.161 *** (0.082) | 0.123 (0.143) | 0.039 (0.178) | 0.181 (0.252) | −0.017 (0.262) | 0.165 *** (0.038) | 0.165 *** (0.038) |
| Puerto Ricans | 0.222 ** (0.125) | 0.211 *** (0.084) | 0.220 *** (0.106) | 0.083 (0.189) | 0.141 (0.245) | 0.102 (0.371) | 0.124 (0.378) | 0.224 *** (0.078) | 0.225 ** (0.079) |
| Other Latinos | 0.125 (0.100) | 0.108 * (0.067) | 0.109 * (0.081) | −0.026 (0.172) | 0.137 (0.179) | −0.069 (0.315) | 0.179 (0.288) | 0.113 * (0.061) | 0.113 * (0.061) |
| Alpha Scale (Model 1) | Single Factor (Model 2) | Single Factor Model with Correlated Errors (Model 3) | Two Factor Model (Model 4) | Two Factor Model with Correlated Errors (Model 5) | Second Order Factor (Model 6) | Second Order Factor with Correlated Errors (Model 7) | |||
|---|---|---|---|---|---|---|---|---|---|
| Subtle Mistreatment | Blatant Mistreatment | Subtle Mistreatment | Blatant Mistreatment | ||||||
| All Latinos | 0.235 *** (0.050) | 0.234 *** (0.035) | 0.241 *** (0.041) | 0.221 ** (0.094) | 0.025 (0.106) | 0.301 * (0.164) | −0.053 (0.160) | 0.243 *** (0.032) | 0.246 *** (0.032 |
| Cubans | 0.047 (0.151) | 0.036 (0.059) | 0.038 (0.066) | 0.407 *** (0.135) | −0.373 ** (0.148) | 0.914 ** (0.441) | −0.878 ** (0.408) | 0.037 (0.054) | 0.041 (0.053) |
| Mexicans | 0.268 *** (0.079) | 0.280 *** (0.043) | 0.286 *** (0.050) | 0.062 (0.112) | 0.228 ** (0.116) | 0.047 (0.196) | 0.244 (0.184) | 0.290 *** (0.038) | 0.293 *** (0.038) |
| Puerto Ricans | 0.107 (0.094) | 0.110 * (0.055) | 0.110 * (0.069) | 0.239 * (0.128) | −0.127 (0.173) | 0.350 (0.247) | −0.239 (0.262) | 0.144 * (0.052) | 0.144 * (0.052) |
| Other Latinos | 0.268 *** (0.110) | 0.251 *** (0.052) | 0.258 *** (0.060) | 0.519 *** (0.127) | −0.258 ** (0.140) | 0.838 *** (0.231) | −0.576 ** (0.226) | 0.262 *** (0.049) | 0.265 *** (0.049) |
| Chronic Health Problems | Depression | |||
|---|---|---|---|---|
| Subtle Mistreatment | Blatant Mistreatment | Subtle Mistreatment | Blatant Mistreatment | |
| Factor | Factor | Factor | Factor | |
| All Latinos | 0.137 *** | 0.133 *** | 0.253 *** | 0.218 *** |
| 0.041 | 0.042 | 0.041 | 0.044 | |
| Cubans | 0.129 * | 0.124 | 0.085 | −0.023 |
| 0.031 | 0.08 | 0.062 | 0.061 | |
| Mexicans | 0.166 *** | 0.146 *** | 0.267 *** | 0.286 *** |
| 0.045 | 0.059 | 0.055 | 0.052 | |
| Puerto Ricans | 0.212 *** | 0.218 ** | 0.137 ** | 0.076 |
| 0.095 | 0.115 | 0.058 | 0.082 | |
| Other Latinos | 0.09 | 0.117 * | 0.323 *** | 0.176 |
| 0.088 | 0.075 | 0.059 | 0.07 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Burgos, G.; Trillo, A. Measuring Perceived Discrimination and Its Consequences for Latino Health. Societies 2025, 15, 333. https://doi.org/10.3390/soc15120333
Burgos G, Trillo A. Measuring Perceived Discrimination and Its Consequences for Latino Health. Societies. 2025; 15(12):333. https://doi.org/10.3390/soc15120333
Chicago/Turabian StyleBurgos, Giovani, and Alex Trillo. 2025. "Measuring Perceived Discrimination and Its Consequences for Latino Health" Societies 15, no. 12: 333. https://doi.org/10.3390/soc15120333
APA StyleBurgos, G., & Trillo, A. (2025). Measuring Perceived Discrimination and Its Consequences for Latino Health. Societies, 15(12), 333. https://doi.org/10.3390/soc15120333






