Cross-Disciplinary Rapid Scoping Review of Structural Racial and Caste Discrimination Associated with Population Health Disparities in the 21st Century
Abstract
1. Introduction
Study Objectives
- To collate the literature evidence on the background realities of historical and structural racial and caste discrimination causing geographic, demographic, and socio-economic inequities and resulting in population health disparities at the societal level in the context of three case-study countries.
- To draw major themes of societal health disparities based on the theories, emerging concepts, various components, and determinants associated with structural racism and casteism.
- To consolidate a set of recommendations for reparative policy changes to help in learning from the evidence of existential realities, and unlearn and challenge the historical structural racial and caste discrimination systems that lead to population health disparities in the context of the 21st century.
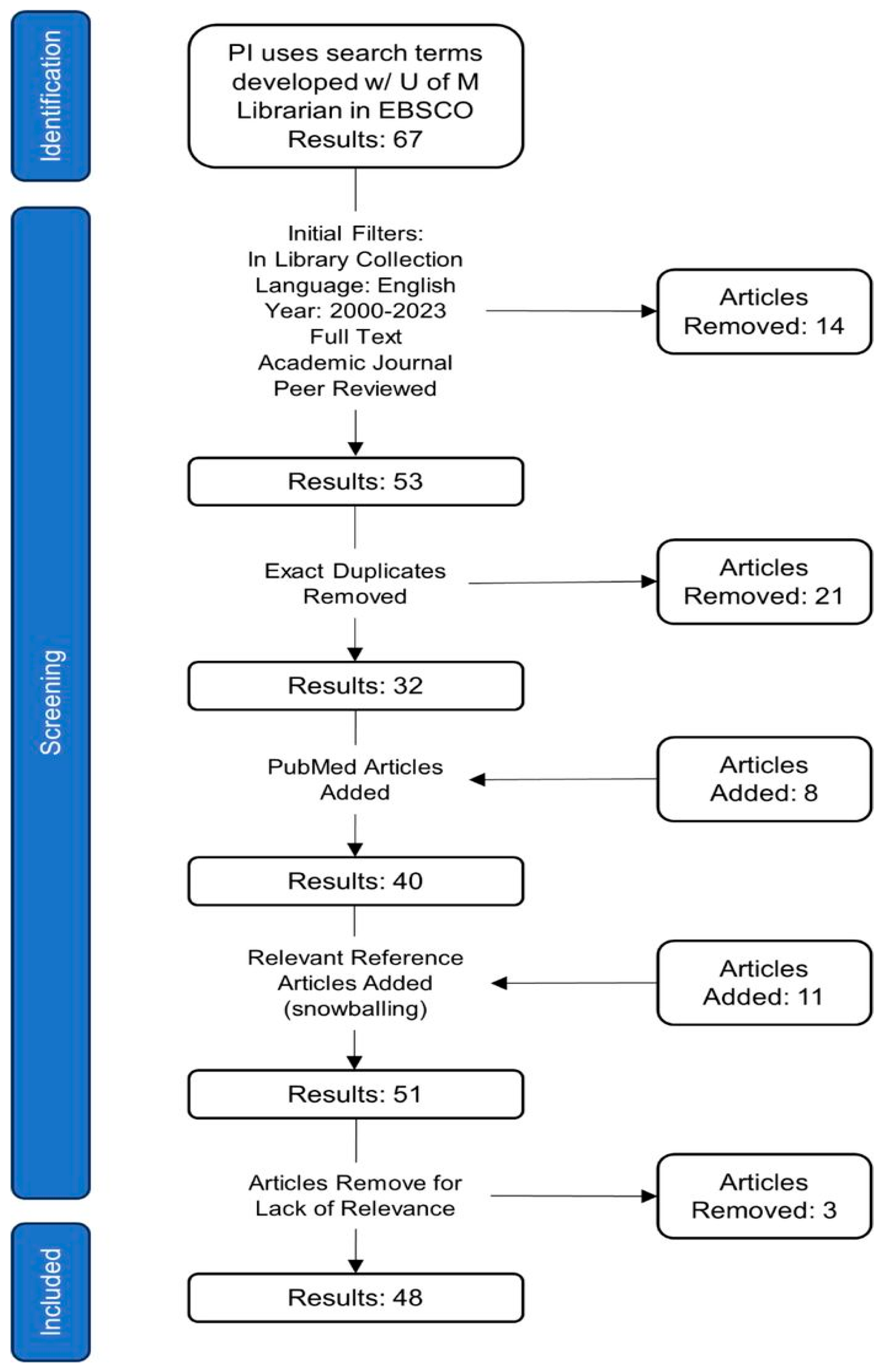
2. Materials and Methods
3. Results and Discussion
3.1. Health Disparities across Various Forms of Racism and Casteism
3.1.1. Health Disparities Impacting Black African Americans
3.1.2. Health Disparities Impacting Indigenous Peoples
3.1.3. Racism-Related Health Disparities Impacting Other Ethnic Groups
3.1.4. Caste-Based Health Disparities and the Link between Casteism, Transnational Casteism, and Racism
Transnational Casteism
3.2. Theoretical Underpinning
3.3. Issues of Science
3.3.1. Genetic Variations
3.3.2. Genetic Testing
3.3.3. Epigenetic Changes
3.3.4. Psychosocial Stresses, Allostatic Load, and Telomere Shortening
3.4. Social Determinants of Health and Structural Determinants of Health Disparities
3.5. Discussion of Major Issues in the Review
3.6. Limitations of This Review
3.7. Reparative Policy Considerations
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Zhang, L.R.; Rasali, D. Life expectancy ranking of Canadians among the populations in selected OECD countries and its dis-parities among British Columbians. Arch. Public Health 2015, 73, 17. [Google Scholar] [CrossRef] [PubMed]
- Zandy, M.; Zhang, L.R.; Kao, D.; Rajabali, F.; Turcotte, K.; Zheng, A.; Oakey, M.; Smolina, K.; Pike, I.; Rasali, D. Area-based socioeconomic disparities in mortality due to unintentional injury and youth suicide in British Columbia, 2009–2013. Health Promot. Chronic Dis. Prev. Can. 2019, 39, 35–44. [Google Scholar] [CrossRef] [PubMed]
- GBD US Health Disparities Collaborators. Life expectancy by county, race, and ethnicity in the USA, 2000–19: A systematic analysis of health disparities. Lancet 2022, 400, 25–38. [Google Scholar] [CrossRef] [PubMed]
- Relova, S.; Joffres, Y.; Rasali, D.; Zhang, L.R.; McKee, G.; Janjua, N. British Columbia’s Index of Multiple Deprivation for Community Health Service Areas. Data 2022, 7, 24. [Google Scholar] [CrossRef]
- CDC. CDC Health Disparities and Inequalities Report—United States, 2011; Centers for Disease Control and Prevention, US Department of Health and Human Services: Atlanta, GA, USA, 2011.
- Rasali, D.; Zhang, R.; Guram, K.; Gustin, S.; Hay, D.I. Priority Health Equity Indicators for British Columbia: Selected Indicators Report; Provincial Health Services Authority, Population and Public Health Program: Vancouver, BC, USA, 2016. [Google Scholar]
- Rasali, D.; Kao, D.; Fong, D.; Qiyam, L. Priority Health Equity Indicators for British Columbia: Preventable and Treatable Premature Mortality; BC Center for Disease Control, Provincial Health Services Authority: Vancouver, BC, USA, 2019. [Google Scholar]
- Melton-Fant, C. Health Equity and the Dynamism of Structural Racism and Public Policy. Milbank Q. 2022, 100, 628–649. [Google Scholar] [CrossRef]
- Bailey, Z.D.; Krieger, N.; Agénor, M.; Graves, J.; Linos, N.; Bassett, M.T. Structural Racism and Health Inequities in the USA: Evidence and Interventions. Lancet 2017, 389, 1453–1463. [Google Scholar] [CrossRef]
- Reich, D. Who We Are and How We Got Here: Ancient DNA and the New Science of the Human Past; Oxford University Press: Oxford, UK, 2018; ISBN 9780192554383. [Google Scholar]
- Narasimhan, V.M.; Patterson, N.; Moorjani, P.; Rohland, N.; Bernardos, R.; Mallick, S.; Lazaridis, I.; Nakatsuka, N.; Olalde, I.; Lipson, M.; et al. The Formation of Human Populations in South and Central Asia. Science 2019, 365, eaat7487. [Google Scholar] [CrossRef]
- Yengde, S. Global Castes. Ethn. Racial Stud. 2021, 45, 340–360. [Google Scholar] [CrossRef]
- Kowner, R.; Demel, W. Chapter 1: Introduction. In Race and Racism in Modern East Asia: Interactions, Nationalism, Gender and Lineage; Brill: Boston, MA, USA, 2015; ISBN 9789004292925. [Google Scholar]
- Bassett, M.T. Racism and Caste: Lessons for the USA. Lancet 2021, 397, 187–188. [Google Scholar] [CrossRef]
- Wallis, M.; Fleras, A. Introduction: Conceptualizing the Politics of Race: Taking Race Seriously. In The Politics of Race in Canada; Oxford University Press: Oxford, MA, USA, 2009; pp. x–xxiv. [Google Scholar]
- Rasali, D.P. California’s Anti-Caste Discrimination Bill Could Lead to Humanity’s Health Equity. Available online: https://www.dignitypost.com/news/2023/09/99 (accessed on 29 October 2023).
- Knox, R. The Races of Men: A Fragment; Henry Renshaw: London, UK, 1850. [Google Scholar]
- de Gobineau, A. The Inequality of Human Races, Adrian Collins, Translator, 1st English ed.; William Heinemann: London, UK, 1915. [Google Scholar]
- Poliakov, L. The Aryan Myth: A History of Racist and Nationalist Ideas in Europe; Basic Books, Inc.: New York, NY, USA, 1974; ISBN 9780465004522. [Google Scholar]
- Bista, D.B. Fatalism and Development; Orient Blackswan: Hyderabad, India, 1991; ISBN 9788125001881. [Google Scholar]
- Kirmayer, L.J.; Gone, J.P.; Moses, J. Rethinking Historical Trauma. Transcult. Psychiatry 2014, 51, 299–319. [Google Scholar] [CrossRef]
- Krieger, N. Discrimination and Health Inequities. Int. J. Health Serv. 2014, 44, 643–710. [Google Scholar] [CrossRef] [PubMed]
- Browne, A.J. Moving beyond Description: Closing the Health Equity Gap by Redressing Racism Impacting Indigenous Populations. Soc. Sci. Med. 2017, 184, 23–26. [Google Scholar] [CrossRef] [PubMed]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef] [PubMed]
- Bloche, M.G. Health Care Disparities—Science, Politics, and Race. N. Engl. J. Med. 2004, 350, 1568–1570. [Google Scholar] [CrossRef] [PubMed]
- Gee, G.C.; Ford, C.L. Structural Racism and Health Inequities. Du Bois Rev. Soc. Sci. Res. Race 2011, 8, 115–132. [Google Scholar] [CrossRef]
- Browne, A.J.; Varcoe, C.; Lavoie, J.; Smye, V.; Wong, S.T.; Krause, M.; Tu, D.; Godwin, O.; Khan, K.; Fridkin, A. Enhancing Health Care Equity with Indigenous Populations: Evidence-Based Strategies from an Ethnographic Study. BMC Health Serv. Res. 2016, 16, 544. [Google Scholar] [CrossRef]
- Williams, D.R.; Lawrence, J.A.; Davis, B.A. Racism and Health: Evidence and Needed Research. Annu. Rev. Public Health 2019, 40, 105–125. [Google Scholar] [CrossRef]
- Martinez, A.; de la Rosa, R.; Mujahid, M.; Thakur, N. Structural Racism and Its Pathways to Asthma and Atopic Dermatitis. J. Allergy Clin. Immunol. 2021, 148, 1112–1120. [Google Scholar] [CrossRef]
- Diaz, A.A.; Thakur, N.; Celedón, J.C. Lessons Learned from Health Disparities in Coronavirus Disease-2019 in the United States. Clin. Chest Med. 2022, 44, 425–434. [Google Scholar] [CrossRef]
- Sweeting, J.A.; Akinyemi, A.A.; Holman, E.A. Parental Preconception Adversity and Offspring Health in African Americans: A Systematic Review of Intergenerational Studies. Trauma Violence Abus. 2023, 24, 152483802210743. [Google Scholar] [CrossRef]
- Hurd, N.M.; Young, A. Introduction to the Special Issue: Advancing Racial Justice in Clinical Child and Adolescent Psychology. J. Clin. Child Adolesc. Psychol. 2023, 52, 311–327. [Google Scholar] [CrossRef] [PubMed]
- Subica, A.M.; Link, B.G. Cultural Trauma as a Fundamental Cause of Health Disparities. Soc. Sci. Med. 2022, 292, 114574. [Google Scholar] [CrossRef] [PubMed]
- Zhou, X.; Wodtke, G.T. Income Stratification among Occupational Classes in the United States. Soc. Forces 2018, 97, 945–972. [Google Scholar] [CrossRef]
- Soled, D.R.; Chatterjee, A.; Olveczky, D.; Lindo, E.G. The Case for Health Reparations. Front. Public Health 2021, 9, 664783. [Google Scholar] [CrossRef] [PubMed]
- Jacoby, S.F.; Dong, B.; Beard, J.H.; Wiebe, D.J.; Morrison, C.N. The Enduring Impact of Historical and Structural Racism on Urban Violence in Philadelphia. Soc. Sci. Med. 2018, 199, 87–95. [Google Scholar] [CrossRef]
- Tiedt, J.A.; Brown, L.A. Allostatic Load: The Relationship between Chronic Stress and Diabetes in Native Americans. J. Theory Constr. Test. 2014, 18, 22–27. [Google Scholar]
- Keyes, C.L.M. The Black-White Paradox in Health: Flourishing in the Face of Social Inequality and Discrimination. J. Personal. 2009, 77, 1677–1706. [Google Scholar] [CrossRef]
- Goodman, A.; Fleming, K.; Markwick, N.; Morrison, T.; Lagimodiere, L.; Kerr, T. “They Treated Me like Crap and I Know It Was Because I Was Native”: The Healthcare Experiences of Aboriginal Peoples Living in Vancouver’s Inner City. Soc. Sci. Med. 2017, 178, 87–94. [Google Scholar] [CrossRef]
- McKinney, L.P.; Gerbi, G.B.; Caplan, L.S.; Claridy, M.D.; Rivers, B.M. Predictors of Genetic Beliefs toward Cancer Risk Perceptions among Adults in the United States: Implications for Prevention or Early Detection. J. Genet. Couns. 2020, 29, 494–504. [Google Scholar] [CrossRef]
- Parra-Cardona, R.; López-Zerón, G.; Leija, S.G.; Maas, M.K.; Villa, M.; Zamudio, E.; Arredondo, M.; Yeh, H.; Domenech Rodríguez, M.M. A Culturally Adapted Intervention for Mexican-Origin Parents of Adolescents: The Need to Overtly Address Culture and Discrimination in Evidence-Based Practice. Fam. Process 2018, 58, 334–352. [Google Scholar] [CrossRef]
- Parkman, A.A.; Foland, J.; Anderson, B.; Duquette, D.; Sobotka, H.; Lynn, M.; Nottingham, S.; Dotson, W.D.; Kolor, K.; Cox, S.L. Public Awareness of Genetic Nondiscrimination Laws in Four States and Perceived Importance of Life Insurance Protections. J. Genet. Couns. 2015, 24, 512–521. [Google Scholar] [CrossRef] [PubMed]
- Shaw, S.J.; Armin, J. The Ethical Self-Fashioning of Physicians and Health Care Systems in Culturally Appropriate Health Care. Cult. Med. Psychiatry 2011, 35, 236–261. [Google Scholar] [CrossRef] [PubMed]
- Geronimus, A.T.; Hicken, M.T.; Pearson, J.A.; Seashols, S.J.; Brown, K.L.; Cruz, T.D. Do US Black Women Experience Stress-Related Accelerated Biological Aging? Hum. Nat. 2010, 21, 19–38. [Google Scholar] [CrossRef] [PubMed]
- Williams, P.H. Policy Framework for Rare Disease Health Disparities. Policy Politics Nurs. Pract. 2011, 12, 114–118. [Google Scholar] [CrossRef] [PubMed]
- Lee, C. “Race” and “Ethnicity” in Biomedical Research: How Do Scientists Construct and Explain Differences in Health? Soc. Sci. Med. 2009, 68, 1183–1190. [Google Scholar] [CrossRef]
- Sankar, P.; Cho, M.K.; Condit, C.M.; Hunt, L.M.; Koenig, B.; Marshall, P.; Lee, S.S.J.; Spicer, P. Genetic Research and Health Disparities. JAMA 2004, 291, 2985. [Google Scholar] [CrossRef]
- Farmer, M.M.; Ferraro, K.F. Are Racial Disparities in Health Conditional on Socioeconomic Status? Soc. Sci. Med. 2005, 60, 191–204. [Google Scholar] [CrossRef]
- Thapa, T.B. Living with Diabetes: Lay Narratives as Idioms of Distress among the Low-Caste Dalit of Nepal. Med. Anthropol. 2014, 33, 428–440. [Google Scholar] [CrossRef]
- Sims, C.M. Ethnic Notions and Healthy Paranoias: Understanding of the Context of Experience and Interpretations of Healthcare Encounters among Older Black Women. Ethn. Health 2010, 15, 495–514. [Google Scholar] [CrossRef]
- Jackson, F.L.C. Ethnogenetic Layering (EL): An Alternative to the Traditional Race Model in Human Variation and Health Disparity Studies. Ann. Hum. Biol. 2008, 35, 121–144. [Google Scholar] [CrossRef][Green Version]
- Kaplan, J.M. When Socially Determined Categories Make Biological Realities. Monist 2010, 93, 281–297. [Google Scholar] [CrossRef]
- Powell-Young, Y.M.; Spruill, I.J. Views of Black Nurses toward Genetic Research and Testing. J. Nurs. Scholarsh. 2013, 45, 151–159. [Google Scholar] [CrossRef] [PubMed]
- Cabassa, L.J. Integrating cross-cultural Psychiatry into the study of mental health disparities. Am. J. Public Health. Lett. 2003, 93, 1034. [Google Scholar] [CrossRef] [PubMed]
- Giddings, L.S. A Theoretical Model of Social Consciousness. Adv. Nurs. Sci. 2005, 28, 224–239. [Google Scholar] [CrossRef] [PubMed]
- Kohrt, B.A.; Speckman, R.A.; Kunz, R.D.; Baldwin, J.L.; Upadhaya, N.; Acharya, N.R.; Sharma, V.D.; Nepal, M.K.; Worthman, C.M. Culture in Psychiatric Epidemiology: Using Ethnography and Multiple Mediator Models to Assess the Relationship of Caste with Depression and Anxiety in Nepal. Ann. Hum. Biol. 2009, 36, 261–280. [Google Scholar] [CrossRef]
- Beletsky, L.; Grau, L.E.; White, E.; Bowman, S.; Heimer, R. The Roles of Law, Client Race and Program Visibility in Shaping Police Interference with the Operation of US Syringe Exchange Programs. Addiction 2010, 106, 357–365. [Google Scholar] [CrossRef]
- Vervoort, D.; Kimmaliardjuk, D.M.; Ross, H.J.; Fremes, S.E.; Ouzounian, M.; Mashford-Pringle, A. Access to Cardiovascular Care for Indigenous Peoples in Canada: A Rapid Review. CJC Open 2022, 4, 782–791. [Google Scholar] [CrossRef]
- Martin, C.L.; Ghastine, L.; Lodge, E.K.; Dhingra, R.; Ward-Caviness, C.K. Understanding Health Inequalities through the Lens of Social Epigenetics. Annu. Rev. Public Health 2022, 43, 235–254. [Google Scholar] [CrossRef]
- Krieger, N. Stormy Weather: Race, Gene Expression, and the Science of Health Disparities. Am. J. Public Health 2005, 95, 2155–2160. [Google Scholar] [CrossRef]
- Arjunan, A.; Darnes, D.R.; Sagaser, K.G.; Svenson, A.B. Addressing Reproductive Healthcare Disparities through Equitable Carrier Screening: Medical Racism and Genetic Discrimination in United States’ History Highlights the Needs for Change in Obstetrical Genetics Care. Societies 2022, 12, 33. [Google Scholar] [CrossRef]
- Chuang, E.; Yu, S.; Georgia, A.; Nymeyer, J.; Williams, J. A Decade of Studying Drivers of Disparities in End-of-Life care for Black Americans: Using the NIMHD Framework for Health Disparities Research to Map the Path Ahead. J. Pain Symptom Manag. 2022, 64, e43–e52. [Google Scholar] [CrossRef] [PubMed]
- Mehra, R.; Alspaugh, A.; Dunn, J.T.; Franck, L.S.; McLemore, M.R.; Keene, D.E.; Kershaw, T.S.; Ickovics, J.R. “‘Oh Gosh, Why Go?’ Cause They Are Going to Look at Me and Not Hire”: Intersectional Experiences of Black Women Navigating Employment during Pregnancy and Parenting. BMC Pregnancy Childbirth 2023, 23, 17. [Google Scholar] [CrossRef] [PubMed]
- Small, P.M. Achieving equity and agreement: The importance of inclusion of marginalized groups in hospital policy initiatives. Voices Bioeth. 2020. [Google Scholar] [CrossRef]
- Azhar, S.; Farina, A.; Alvarez, A.R.G.; Klumpner, S. Asian in the Time of COVID-19: Creating a Social Work Agenda for Asian American and Pacific Islander Communities. Soc. Work. 2021, 67, 58–68. [Google Scholar] [CrossRef] [PubMed]
- Thapa, R.; van Teijlingen, E.; Regmi, P.R.; Heaslip, V. Caste Exclusion and Health Discrimination in South Asia: A Systematic Review. Asia Pac. J. Public Health 2021, 33, 101053952110146. [Google Scholar] [CrossRef]
- Mégret, F.; Dutta, M. Transnational Discrimination: The Case of Casteism and the Indian Diaspora. Transnatl. Leg. Theory 2023, 13, 391–430. [Google Scholar] [CrossRef]
- Yelton, B.; Friedman, D.B.; Noblet, S.; Lohman, M.C.; Arent, M.A.; Macauda, M.M.; Sakhuja, M.; Leith, K.H. Social Determinants of Health and Depression among African American Adults: A Scoping Review of Current Research. Int J Env. Res Public Health 2022, 19, 1498. [Google Scholar] [CrossRef]
- Rasali, D.P.; Li, C.; Mak, S.; Rose, C.; Janjua, N.; Patrick, D. Correlations of COVID-19 Incidence with Neighborhood Demographic Factors in BC. Ann. Epidemiol. 2021, 61, 17. [Google Scholar] [CrossRef]
- Viladrich, A. Sinophobic Stigma Going Viral: Addressing the Social Impact of COVID-19 in a Globalized World. Am. J. Public Health 2021, 111, 876–880. [Google Scholar] [CrossRef]
- Mannor, K.M.; Malcoe, L.H. Uses of Theory in Racial Health Disparities Research: A Scoping Review and Application of Public Health Critical Race Praxis. Ann. Epidemiol. 2021, 66, 56–64. [Google Scholar] [CrossRef]
- White, K.; Lawrence, J.A.; Tchangalova, N.; Huang, S.J.; Cummings, J.L. Socially-Assigned Race and Health: A Scoping Review with Global Implications for Population Health Equity. Int. J. Equity Health 2020, 19, 25. [Google Scholar] [CrossRef] [PubMed]
- Ford, C.L.; Airhihenbuwa, C.O. Critical Race Theory, Race Equity, and Public Health: Toward Antiracism Praxis. Am. J. Public Health 2010, 100, S30–S35. [Google Scholar] [CrossRef] [PubMed]
- Sotero, M. A Conceptual Model of Historical Trauma: Implications for Public Health Practice and Research. J. Health Disparities Res. Pract. 2006, 1, 93–108. [Google Scholar]
- Marmot, M.; Allen, J.J. Social Determinants of Health Equity. Am. J. Public Health 2014, 104, S517–S519. [Google Scholar] [CrossRef]
| Final SN | Author(s) (Citation Year) | Studied Country/ies | Race, Ethnicity, or Caste under Study | Themes Extracted |
|---|---|---|---|---|
| 1 | Sweeting et al. (2023) | United States | African Americans; White Americans | Parental preconception adversity; Epigenetic effects on health and disease; Structural racism as a root cause; Theoretical considerations [31] |
| 2 | Hurd and Young (2023) | United States | African Americans; Latino Americans; Native Americans; White Americans | Education and clinical child and adolescent psychology; Global Diversity Equity and Inclusion (DEI); Decentering whiteness; Discrimination (overrepresentation in punitive measures); Healthcare: access, clinicians’ bias, and representation among providers; Mental health; Policy implications; Research needs; Socio-economic factors [32] |
| 3 | Subica and Link (2022) | United States | African Americans; Native Americans; White Americans | Cultural/historical trauma; Cultural trauma– mechanism of affecting health disparities; Fundamental cause theory [33] |
| 4 | Zhou and Wodtke (2019) | United States | Economic Class | Income class stratification and racial class stratification; Resource distribution—social stratification decline; Resource distribution—Socio-economic inequality [34] |
| 5 | Soled et al. (2021) | United States | African Americans; Native Americans; White Americans | Reparations; Role of medicine and pseudo-science [35] |
| 6 | Jacoby et al. (2018) | United States (Philadelphia) | African Americans; Latino Americans; White Americans | Crime; Gun violence; Present-day impacts of historical discrimination; Racial health disparities; Redlining [36] |
| 7 | Tiedt and Brown (2014) | United States | African Americans; Latino Americans; White Americans | Historical trauma and present-day discrimination as a source of chronic stress in Native Americans; Impact of stress (allostatic load) on diabetes rates [37] |
| 8 | Keyes (2009) | United States | African Americans; White Americans | Health outcome impacts—coping and resilience; Health outcome impacts—mental health extent of discrimination; Health outcome impacts—morbidity and mortality; Health outcome impacts—risk factors [38] |
| 9 | Goodman et al. (2017) | Canada (Vancouver) | Indigenous Canadians; White Canadians | Indigenous healthcare: experience and outcomes; risk factors (alcohol), race-based adverse treatment; health outcomes, stereotypes and stigma; interrelated stigma and intersectional approaches; patients’ stories [39] |
| 10 | McKinney et al. (2020) | United States | African Americans; Asian and Pacific Islanders (API); Latino Americans; Native Americans; Non-Hispanic White Americans | Genetic variations—genetic testing, stigma, genetic counseling, distrust among minorities, and cultural competency training; Social cognitive theory [40] |
| 11 | Browne et al. (2016) | Canada | Indigenous Canadians; White Canadians | Indigenous healthcare—10 strategies to optimize effectiveness of healthcare; Structural violence—population and public health as a major determinant of the distribution and outcomes of social and health inequities [27] |
| 12 | Parra-Cardona et al. (2018) | United States | Mexican Americans; Non-Hispanic White Americans | Cultural adaptation; Mental health disparities—Mental health services in Latino immigrant communities [41] |
| 13 | Parkman et al. (2015) | United States | Connecticut, Michigan, Ohio, and Oregon Residents | Genetic privacy; Anti-genetic discrimination policy [42] |
| 14 | Shaw and Armin (2011) | United States | People of Color Generally; White Americans | Cultural adaptation; Physician training; Corporatization of social justice interventions [43] |
| 15 | Geronimus et al. (2010) | United States | African American Women; White American Women | Black–White health disparities; Intersection of race and gender discrimination; Accelerated biological aging in Black women [44] |
| 16 | Williams (2011) | United States | N/A | Government funding—impact on medical research; Anti-genetic discrimination police [45] |
| 17 | Lee (2009) | United States | African Americans; API; Latino Americans; Native Americans; Non-Hispanic White Americans | Use of race and ethnicity in biomedical research; Lack of a biological basis for race; Race as a proxy for socio-economic status, culture, and history [46] |
| 18 | Sankar et al. (2004) | United States | African Americans; Latino Americans; Native Americans; Non-Hispanic White Americans | Link between racial discrimination, poverty, and health disparities; Genetic research; Public health policy; Scientific racism [47] |
| 19 | Farmer and Ferraro (2005) | United States | African Americans; White Americans | Health outcomes in Black Americans; SES—interaction of SES in racial health disparities and interaction with education is the largest [48] |
| 20 | Browne (2017) | Australia, Canada, New Zealand, United States | Indigenous People; White Americans; Australians; Canadians: and Kiwis | Indigenous healthcare in the Anglophone Western hemisphere; race-based adverse treatment; Health outcomes and stereotypes; Historical injustice; Socio-economic factors [23] |
| 21 | Thapa (2014) | Nepal | Brahman; Kshatriya (Chhetri); Dalit; Vaishya | Caste system in Nepal; Systemic discrimination; Allostatic load; Anti-Dalit discrimination; Diabetes; Cultural narratives [49] |
| 22 | Sims (2010) | United States | African American Women; White Americans | Health outcomes in Black Americans; Discrimination—impact on trust in healthcare providers [50] |
| 23 | Jackson (2008) | United States | N/A | Alternatives to race as a model of human diversity; Historical origin of racism [51] |
| 24 | Kaplan (2010) | United States | African Americans; White Americans | Race as a folk category; Black–White health disparities; Lack of a biological basis for racial categories; Impact of racism on public health outcomes [52] |
| 25 | Powell-Young and Spruill (2013) | United States | African Americans | Genetic discrimination; Minority representation among healthcare professionals; African American views of genetic testing/research [53] |
| 26 | Bloche (2004) | United States | People of Color; White Americans | Systemic racism; Ignoring race-based disparities in healthcare to justify public health policies that perpetuate race-based disparities; Ideological interference with public health policy [25] |
| 27 | Cabassa (2003) | United States | N/A | Practitioner bias in mental healthcare; Multidisciplinary approach to finding the root of mental health disparity [54] |
| 28 | Giddings (2005) | United States | People of Color; White Americans | Transcultural nursing; Cultural adaptation by healthcare professionals; Social consciousness; Gender roles in healthcare; Marginalization; Traditional constructs in nursing [55] |
| 29 | Kohrt et al. (2009) | Nepal | Brahman; Chhetri; Dalit; Janajati | Caste-based discrimination in Nepal; Mental health—stresses [56] |
| 30 | Beletsky and Grau (2010) | United States | African American; Latino Americans; Non-Hispanic White Americans | Racial profiling; Police tactics—impact on the use of substance abuse-related health services by marginalized groups; Syringe exchanges; Harm reduction; War on drugs [57] |
| 31 | Vervoort et al. (2022) | Canada | Indigenous Canadians; Non-Indigenous Canadians | Indigenous healthcare: cardiovascular healthcare, accessibility, literacy and awareness, cardiovascular health disparities; morbidity and mortality disparities [58] |
| 32 | Bailey et al. (2017) | United States | African Americans; API Americans; Latino Americans; Indigenous Americans; Non-Hispanic White Americans | Impact of structural racism on health outcomes and disparities [9] |
| 33 | Martin et al. (2022) | United States | African Americans; White Americans | Social epigenetics; DNAm: Allostatic load, impact of stress, SES, childhood and adulthood exposure to racism, and social environment; Epigenetic link to race-based health disparities; Impact of stress on the epigenome [59] |
| 34 | Diaz et al. (2023) | United States | African Americans; Indigenous Americans; Latino Americans; Non-Hispanic White Americans | Structural and social determinants of health; Disparities in COVID-19 care/vaccination rates; Impact of racism and implicit bias on COVID-19 care [30] |
| 35 | Williams et al. (2019) | United States | African Americans; Indigenous Americans; Latino Americans; Non-Hispanic White Americans | Racism and health; Cultural racism; Structural or institutional racism; Residential racial segregation; Segregation and health; Segregation and health—epidemiological evidence [28] |
| 36 | Krieger (2005) | United States | African Americans; White Americans | Origins of racial classifications; Lack of biological basis for race; Contemporary research on US racial attitudes; Climate and race; Race and political ideology [60] |
| 37 | Martinez et al. (2021) | United States | African Americans; Indigenous Americans; Latino Americans; Non-Hispanic White Americans | Asthma and atopic dermatitis—racial disparities; Impacts of structural racism (e.g., residential segregation; socio-economic position; mass incarceration) on health outcomes, epigenome, and the microbiome; Allostatic load [29] |
| 38 | Arjunan et al. (2022) | United States | African American; API Americans; Jewish Americans; Latino Americans; Non-Hispanic White Americans | Medical racism and genetic discrimination in obstetrics; Racism and genetics; Institutional racism practiced in professional medical organizations [61] |
| 39 | Gee and Ford (2011) | United States | African Americans; API Americans; Arab Americans; Indigenous Americans; Latino Americans; Non-Hispanic White Americans | Racism—link to health disparities; Impact of structural racism (e.g., social segregation and immigration policy in Digital Spaces) on health; Intergenerational drag—generational impact of racism [26] |
| 40 | Chuang et al. (2022) | United States | African Americans; White Americans | Meta-study of racial disparities in end-of-life care; Behavioral basis for disparities; Environmental (physical and socio-cultural) basis for disparities; Provider bias [62] |
| 41 | Mehra et al. (2023) | United States | African American Women; White Women | Intersectionality; Pregnancy discrimination in employment—intersection with racial discrimination [63] |
| 42 | Small (2020) | United States | N/A | Marginalized groups representation hospital policy initiatives; COVID-19 [64] |
| 43 | Azhar et al. (2022) | United States | API Americans; White Americans | COVID-19 disparities—impact on Asian American and Pacific Islander communities; Anti-Asian xenophobia and COVID-19; Policy recommendations [65] |
| 44 | Thapa et al. (2021) | India, Nepal | Brahmins; Kshatriyas; Vaishyas; Dalits | Caste and health discrimination; Caste stigma; Economic inequality; Culture and beliefs [66] |
| 45 | Yengde (2022) | India, Nepal, United States | Brahmins; Dalits; African Americans; White Americans; | Global caste; Race and caste; Comparative analysis of global caste systems [12] |
| 46 | Narasimhan (2019) | South Asia, India | Ancestral North Indians; Ancestral South Indians | Ancient human migration in Eurasia; Spread of agriculture; Genetics and anthropology [11] |
| 47 | Mégret and Dutta (2022) | India, United States, United Kingdom | Brahmins; Dalits; Indian Diaspora | Anti-caste discrimination law; Casteism within Indian diaspora communities; Impact of global mobility on discrimination; Transnational caste discrimination [67] |
| 48 | Yelton et al. (2022) | United States | African Americans; White Americans | Depression; Social determinants of health; Socio-economic status and health; Education access and quality; Neighborhood and built Environment; Healthcare access and quality [68] |
| Areas of Reparative Policy Changes | Recommended Example Domains Based on the Reviews |
|---|---|
| 1. Advancement and funding availability in health disparity research |
|
| 2. Development of organizational structures, programs, and processes for reparative policies to support health equity |
|
| 3. Advancing racial justice in population health |
|
| 4. Addressing targeted cultural trauma for the restoration of damaged cultural modes |
|
| 5. Ensuring an equitable healthcare system for all | |
| 6. Addressing genetic discriminations |
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rasali, D.P.; Woodruff, B.M.; Alzyoud, F.A.; Kiel, D.; Schaffzin, K.T.; Osei, W.D.; Ford, C.L.; Johnson, S. Cross-Disciplinary Rapid Scoping Review of Structural Racial and Caste Discrimination Associated with Population Health Disparities in the 21st Century. Societies 2024, 14, 186. https://doi.org/10.3390/soc14090186
Rasali DP, Woodruff BM, Alzyoud FA, Kiel D, Schaffzin KT, Osei WD, Ford CL, Johnson S. Cross-Disciplinary Rapid Scoping Review of Structural Racial and Caste Discrimination Associated with Population Health Disparities in the 21st Century. Societies. 2024; 14(9):186. https://doi.org/10.3390/soc14090186
Chicago/Turabian StyleRasali, Drona P., Brendan M. Woodruff, Fatima A. Alzyoud, Daniel Kiel, Katharine T. Schaffzin, William D. Osei, Chandra L. Ford, and Shanthi Johnson. 2024. "Cross-Disciplinary Rapid Scoping Review of Structural Racial and Caste Discrimination Associated with Population Health Disparities in the 21st Century" Societies 14, no. 9: 186. https://doi.org/10.3390/soc14090186
APA StyleRasali, D. P., Woodruff, B. M., Alzyoud, F. A., Kiel, D., Schaffzin, K. T., Osei, W. D., Ford, C. L., & Johnson, S. (2024). Cross-Disciplinary Rapid Scoping Review of Structural Racial and Caste Discrimination Associated with Population Health Disparities in the 21st Century. Societies, 14(9), 186. https://doi.org/10.3390/soc14090186







