Abstract
The paper focuses on the association between Bulgarian adolescents’ health risk behaviours (cigarette smoking, vaping, alcohol use and drunkenness) and biopsychosocial factors at individual and interpersonal levels, using data from the pre-pandemic and the pandemic periods, i.e. Health Behaviour in School-aged Children (HBSC) study (2018) and the study of adolescent health and well-being in the context of the COVID-19 pandemic (2022/2023). Logistic regression models reveal a positive association with age in both periods, decreasing gender difference in smoking, presistant effect of family structure, strengthened effect of the material status of the family and a differenciating effect of ethnicity at the end of the pandemic. Family support is positively asociated with substance (mis)use in both periods. At the end of the pandemic generalized anxiety is positively associated with substance (mis)use, loneliness has a negative association with drunkenness, and limited social interaction and vaping are in a positive relationship. The experience of COVID-19 infection in the family is associated with higher risk of smoking, while treatment in hospital for COVID-19 of the adolescent or a family member is associated with a higher risk of vaping and drunkenness. Interactions with COVID-19 experience and psychosocial variables reveal a divergence in health risk behaviours, including also engagement in substance (mis)use. Effective interventions, targeting the identified risk factors and risk groups, are needed for promotion of healthy lifestyles among adolescents.
1. Introduction
The global health crisis caused by the COVID-19 pandemic affected all spheres of society and changed the traditional arrangements in which young people develop their personalities and social behaviours. The COVID-19 pandemic posited multiple challenges on young people’s relationships with family and peers, schooling practices, leisure activities, inclusion and participation in the social community and social networks. The adverse socioeconomic effect of the pandemic and the increasing poverty, remote schooling, and social isolation from peers and friends had multiple implications associated with (mental) health risks.
The biopsychosocial model [1] and the social-ecological model [2] are theoretical frameworks providing explanation of the interdependence between the outlined effects of the pandemic on societal systems and social practices and adolescent health behaviours and mental health. These theoretical models emphasise the role of social factors in the development and maintenance of health and disease. The social-ecological model focuses on the interaction of individual (e.g., gender, age, ethnicity), interpersonal (e.g., relationships with family and friends), community (e.g., schools, neighbourhoods) and societal factors (e.g., social norms, policies, legislation) and their association with health behaviours and mental health. The biopsychosocial model highlights the interaction of biological (e.g., virus, infection, severe disease), psychological (e.g., psychological stress, emotional experiences, behavioural responses during the pandemic) and social factors.
Bulgaria is among the countries that were strongly affected by the COVID-19 pandemic and its socioeconomic implications. High excess mortality was caused by insufficient testing, delayed lockdown measures, low capacity of the healthcare system to handle the cases requiring hospitalisation, exceptionally low vaccination rates and prevailing public mistrust in the effectiveness of the governmental measures aiming to curb the pandemic [3,4]. In Bulgaria, the first major epidemic wave was recorded at the end of 2020, followed by two waves in 2021 and another one in early 2022 [5]. Analyses of mortality show that Bulgaria lost 19,004 lives during its first major COVID-19 wave in 2020. After the next two consecutive waves up to the end of March 2022, this number increased to 68,569 [5], p. 6. After March 2022, the number of recorded COVID-19 cases decreased and the restrictions relaxed. Some of the relaxation measures included reopening of the schools and restoration of in-person learning. Increasing poverty and social inequalities and the limited access to educational resources, healthcare and social services of families and children evolved in parallel with the structural difficulties to curb the health crisis. Young people’s social interactions through outdoor activities such as sports, hobbies and meetings with friends were challenged by the imposed measures of social isolation and the digital shift [4,6]. The prolonged time spent online for studies and leisure and the remarkable increase in social media use had a controversial effect on young people’s (mental) health. On the one hand, digitalisation helped children and adolescents to continue their studies and educational activities and partly compensated social isolation due to restricted physical contacts [7]. On the other hand, the excessive use of social media and the prolonged screening time augmented the risks related to cyberbullying, access to materials with violent and sexual content, and participation in life-threatening games that can cause self-harm or disinformation [8]. In many cases, the increased time spent online worsened young people’s mental health by increasing the sense of social isolation, depression and anxiety, and loss of real-time social experiences, skills, and habits [9]. Studies also reveal that a ‘shadow’ pandemic evolved in parallel with the global health crisis associated with increased sedentary behaviours [10], family conflicts due to the overlapping tasks of parenting, schooling and work from home [11], and worsened quality of education, particularly for children and youth from low-resource families [12], etc.
Research on the prevalence of health risk behaviours among young people during the COVID-19 pandemic uncovers mixed trends of (e-)cigarette smoking and (excessive) alcohol consumption in industrialised countries. Studies found a decreasing trend in alcohol consumption among adolescents, revealing the importance of face-to-face social interactions with peers and the socialising patterns of this health risk behaviour [13]. In certain countries, the prevalence of alcohol consumption remained at its pre-pandemic levels, which was explained with the decreased availability and the limited access to alcoholic beverages [14,15]. In other countries, higher substance use was associated with higher anxiety and depression experienced by young people during the pandemic [16]. Diverging trends in certain health risk behaviours were also identified, revealing that tobacco smoking among adolescents decreased, while the use of e-cigarettes followed an upward trend [17]. Growing concerns about the lung-damaging effect of COVID-19 and the limited socialising options had a depressive effect on the prevalence of tobacco use among young people [17,18]. Studies also reveal that passive smoking increased during the pandemic due to the prolonged time spent at home, which, in the case of smoking adult family members, can have negative implications for young people’s health [19]. A systematic review on substance use among youth during the COVID-19 pandemic found a prevailing decline in certain substance use behaviours such as alcohol, cannabis, tobacco, e-cigarettes/vaping and an increase in drug use, leading to the conclusion on the multidimensional character of the changes in the social lives and well-being of young people during the pandemic and its complex effect of health risk behaviours [20]. Studies also identified coping mechanisms associated with substance use during the pandemic, especially among young people with a history of pre-pandemic substance use [21,22]. In certain countries, the decline in perceived availability and the social distancing policies intensified efforts to obtain substances [15]. Thus, the pandemic-related restrictions and the limited social interactions were followed by development of alternative strategies to access substances. The physical inaccessibility and insufficiency of support services were also identified as factors associated with substance use among young people during the pandemic [23].
Little is known about the factors associated with substance (mis)use among Bulgarian adolescents during the COVID-19 pandemic. The existing studies prevailingly focus on mental health, online education and educational outcomes [24,25] and do not address young peoples’ health risk behaviours during the pandemic. Following the biopsychosocial model [1] and the social-ecological model [2], the aim of this paper is to study the association between Bulgarian adolescents’ health risk behaviours (cigarette smoking, vaping (e-cigarette smoking), alcohol consumption and excessive alcohol use (drunkenness)) and biopsychosocial factors at the individual and interpersonal levels by comparing data from the pre-pandemic and the pandemic periods. Sociodemographic factors include gender, age and ethnicity at the individual level and structure and material status of the family at the interpersonal level. Psychosocial factors include adolescent mental health (generalised anxiety and loneliness) at the individual level and perceived family support and limited social interaction with people outside the household at the interpersonal level. Biopsychological factors include experience of COVID-19 infection or treatment in hospital for COVID-19 of the adolescent or a family member. For the pre-pandemic period, we estimate a baseline model used for compassion that includes gender, age, family structure, material status of the family and loneliness. The preliminary analysis shows that the factors with a strong association with adolescent health risk behaviours during the pandemic are family support and generalised anxiety. Apart from studying the main effect of the biopsychosocial factors, we also focus the analysis on the interdependence between health risk behaviours, the experience of COVID-19 in the family, perceived family support, and generalised anxiety, and estimate predicted probabilities of the risk of cigarette smoking, vaping, alcohol use and drunkenness from the interaction models.
2. Materials and Methods
In the present study, we use the datasets from two surveys on adolescent health risk behaviours conducted before and at the end of the COVID-19 pandemic. We use the data from the Health Behaviour in School-aged Children (HBSC) study conducted in 2018, which provides information about adolescent health risk behaviours before the pandemic. The survey was implemented by the Institute for Population and Human Studies at the Bulgarian Academy of Sciences. HBSC-2018 is a national representative survey that covers students at ages 11, 13 and 15 years. The Health Behaviour in School-aged Children (HBSC) study is a WHO collaborative cross-national survey of school-aged children’s health and well-being, examined in their social context, conducted every four years in approximately 50 countries of the European WHO Region and Canada. Data are collected in all the participating countries through self-report school-based surveys, using a standard methodology described in the HBSC 2017/2018 international study protocol [26]. Each country uses random sampling to select a proportion of adolescents aged 11, 13 and 15 years, aiming to achieve representative samples of approximately 1550 adolescents in each age group. The Bulgarian 2017/2018 HBSC sample was based on a list of all schools that have classes in 5, 7 and 9 grades—the three grades/school years that most closely match 11, 13 and 15 year olds. All students who were present and whose parents had given written consent completed the online questionnaire. The final sample comprised 4548 students, of whom 48.4% were boys and 51.6% were girls. The mean age of the students was 13.5 (SD ±1.65).
The analysis of Bulgarian adolescents’ health risk behaviours is also based on a study aiming to explore adolescent health and well-being in the context of the COVID-19 pandemic. It was implemented by the Institute for Population and Human Studies at the Bulgarian Academy of Sciences and was funded by the Bulgarian National Science Fund. This school-based study was conducted in Bulgaria at the end of school year 2021/2022 (June 2022) and in school year 2022/2023. The schools were opened throughout the data collection period and the prevailing attitude in the society was that it was the end of the pandemic. Public health measures were followed less strictly. The aim of this study is to explore the overall effects of the pandemic on adolescents’ lives as evaluated by adolescents. Participants were asked to have in mind the entire period since the beginning of the pandemic when responding to the questions. This study included a nationally representative sample of early to middle adolescents, based on a random selection of schools from a list of all schools in Bulgaria (special schools excluded) in the 28 districts of the country. An online questionnaire was administered in the schools after parental consent had been obtained. The initial data were cleaned for age inconsistencies and only students aged 11–16 years were selected for the present analysis. The sample includes 3345 pupils aged 11–16 years. The mean age of the students is 13.5 years (SD ± 1.74) and the sample is equally distributed by gender. The data were examined by cross-tabulations and logical checks of the (composite) variables used in the analysis. The use of an online questionnaire minimised errors in the individual records related to invalid responses (e.g., out of range values and violated skip patterns). Both surveys used in the present study have a similar sample design. The variables selected for the analysis are also similar in terms of questions and response options (except the measure of loneliness). There is also a slight difference in age groups. HBSC includes 11-, 13- and 15-year-old students. These surveys cover the period before and at the end of the pandemic, so they are comparable on a group level.
Research shows that the complex environments of health risk behaviours require advanced analysis techniques, such as Machine Learning or Artificial Intelligence. The potential of these methods is demonstrated in a recent study exploring the impact that the COVID-19 pandemic on tobacco sales in different provinces in Spain [27]. In the present study, we apply logistic regression models for each of the studied health risk behaviours. The dependent variables in the models are cigarette smoking, vaping (e-cigarette smoking), alcohol use and excessive alcohol consumption (drunkenness). The modelling procedure is the following. At first, we estimate a baseline model from the pre-pandemic data that allows for comparison of the change in selected independent variables. As a next step, we test the main effects of biopsychosocial factors at the individual and interpersonal levels by using data collected at the end of the pandemic. We extend the analysis by focusing on the interdependence between adolescent health risk behaviours, the experience of COVID-19 in the family (infection or hospitalisation of the adolescent or a family member) and selected mental health variables. In particular, we first study the interaction between health risk behaviours, perceived family support and the experience of COVID-19 infection in the family. Afterwards, we explore the interdependence between adolescent health risk behaviours, generalised anxiety and the experience of COVID-19 infection or treatment in hospital for COVID-19 of the adolescent or a family member. As a final step, we estimate from the interaction models the predicted probabilities of cigarette smoking, vaping (e-cigarette smoking), alcohol use and excessive alcohol consumption (drunkenness) in selected groups of adolescents based on their experience with COVID-19 infection or hospitalisation, perceived family support and anxiety. We control for the missing values by coding them as separate categories and include them in the models.
2.1. Health Risk Behaviours
The studied health risk behaviours are examined through adolescent-appropriate measures developed and validated within the Health Behaviour in School-aged Children (HBSC) study [26].
The dependent variable in the models of cigarette smoking is constructed from the question “How often do you smoke tobacco at present?”. The response categories are: “Every day”, “At least once a week, but not every day”, “Less than once a week”, and “I do not smoke”. This variable was recoded and two groups were created. The first group includes young people who do not smoke cigarettes at present (the response option “I do not smoke”). The second group includes students who smoke cigarettes. It combines the response options “Every day”, “At least once a week, but not every day”, and “Less than once a week”. The risk of cigarette smoking is estimated at two time points, before and at the end of the pandemic.
The dependent variable in the models of vaping (e-cigarette smoking) is based on the question “How many days (if any) have you smoked e-cigarettes in the past 30 days?”. The response categories are: “Never”, “1–2 days”, “3–5 days”, “6–9 days”, “10–19 days”, “20–29 days”, and “30 days (or more)”. The response categories of this variable were dichotomised, and two groups were created. The first group includes adolescents who never smoked e-cigarettes (response option “Never”). The second group includes students who smoked e-cigarettes. It combines the response options “1–2 days”, “3–5 days”, “6–9 days”, “10–19 days”, “20–29 days”, and “30 days (or more)”. The risk of vaping is modelled only at the end of the pandemic based on the survey on adolescent health and well-being in the context of the COVID-19 pandemic since there is no information in HBSC-2018.
The dependent variable in the models of alcohol consumption is a composite measure of the beverage-specific frequency of alcohol use. The question measuring alcohol consumption is: “At present, how often do you drink anything alcoholic, such as beer, wine, spirits, alcopops, any other drink that contains alcohol?”. The response categories are “Every day”, “Every week”, “Every month”, “Rarely”, and “Never”. The response categories have been recoded, creating two groups. The first group includes students who report that they rarely or never drank alcohol. This group combines the response options “Every day” and “Every week” for any type of alcohol. The second group includes students who report that they drank alcohol. It combines the response options “Every month”, “Rarely”, and “Never” for each type of alcohol. The risk of alcohol use is estimated at two time points, before and at the end of the pandemic.
The dependent variable in the models of excessive alcohol consumption (drunkenness) is based on the question “Have you ever had so much alcohol that you were really drunk in the last 30 days?”. The response options are: “Never”, “Once”, “2–3 times”, “4–10 times”, and “More than 10 times”. The variable was recoded and two groups were created. The first one includes the students who never got drunk (response option “Never”). The second group includes students who got drunk once or more times. It combines the response option “1–2 days”, “3–5 days”, “6–9 days”, “10–19 days”, “20–29 days”, and “30 days (or more)”. The risk of drunkenness is estimated at two time points, before and at the end of the pandemic.
2.2. Sociodemographic Factors
The independent variables at the individual level include gender and age of the adolescent and belonging to ethnic minority. HBSC-2018 includes students aged 11, 13 and 15 years old. The survey on adolescent health and well-being in the context of the COVID-19 pandemic includes the age groups of 11–12, 13–14 and 15–16-year-old students. Ethnicity is measured by the question “Which language do you speak at home?” with response options Bulgarian, Turkish, Roma, and Other. Due to the small number of responses in the category, “Other” it is recoded as missing. Information on ethnic belonging is available only in the survey on adolescent health and well-being in the context of the COVID-19 pandemic.
Sociodemographic variables at the interpersonal level include the structure and the material status of the family. Family structure is a composite measure that comprises the groups of students who live with two parents at home or with one parent, in foster care or with other relatives [26]. These variables are available in both datasets.
The material status of the family is created as a categorical variable based on the Family Affluence Scale, third revision (FAS III) [28,29]. FAS III combines different material possessions in the family: number of computers owned by the family, number of cars, number of bathrooms, number of travels/holidays abroad, having own bedroom, and having a dishwasher. The total scale score ranges from 0 to 13. The scores from 0 to 4 create the group of low material status families. The scores 5–9 form the group of the families with medium affluence, and the scores 10–13—the families with high affluence. This variable is available in both datasets.
2.3. Psychosocial Factors
The variables measuring adolescent mental health are generalised anxiety and loneliness. Generalised anxiety is measured by the generalised anxiety disorder scale (GAD-7) [30]—a tool that can be used for diagnosis, screening and measurement of the severity as well as for measuring the course of generalised anxiety disorder. GAD-7 has demonstrated good psychometric properties in research with adolescents [31]. It includes the following seven items, exploring the most important diagnostic criteria of generalised anxiety disorder according to the DSM-IV and ICD-10 criteria: “How often, over the past 2 weeks, have you been bothered by: “Feeling nervous, anxious or on edge”, “Not being able to stop or control worrying”, “Worrying too much about different things”, “Trouble relaxing”, “Being so restless that it is hard to sit still”, “Becoming easily annoyed or irritable”, and “Feeling afraid as if something awful might happen?”. The response options are: “Not at all”, “Several days”, “More than half of the days”, and “Nearly every day”. A sum score of ≥11 points measures moderate anxiety and a sum score of ≥17 points measures severe anxiety. The scale is available only in the survey on adolescent health and well-being in the context of the COVID-19 pandemic.
Loneliness is measured by the question “In the past 12 months, how often have you felt lonely?” [32]. The response options “Never”, “Rarely”, and “Sometimes” define the normative level of loneliness. The response options “Most of the time” and “Always” indicate potentially harmful feelings that can have negative health implications (negatives forms of loneliness). In the analysis of the pre-pandemic period we use also a variable available in HBSC-2018 that measures loneliness by the questions “Please, indicate how often you have felt lonely during the past week” with the following response options: “Rarely or none of the time (less than 1 day)”, “Some or a little of the time (1–2 days)”, “Occasionally or a moderate amount of time (3–4 days)”, and “All of the time (5–7 days)”. The response options “Occasionally or a moderate amount of time (3–4 days)” and “All of the time (5–7 days)” are combined in the group of students with negative levels of loneliness and the other categories form the group of adolescents with normative levels of loneliness.
Family support, measuring the perceived availability of emotional support and help in family, is a subscale of the Multidimensional Scale of Perceived Social Support—MSPSS [33]. It is a sum of four items assessed on a 7-point Likert scale with responses ranging from “Very strongly disagree” to “Very strongly agree”. The items of the scale are: “My family really tries to help me”, “I get the emotional help and support I need from my family”, “I can talk about my problems with my family” and “My family is willing to help me make decisions”. A cut-off score of 5.5 points defines high/low family support. This variable is available in both datasets.
Limited social interaction with people outside the household is measured through a scale developed specifically for the study of adolescent health and well-being in the context of the COVID-19 pandemic (2022/2023). It reflects the experience of missing face-to-face contact with significant others (family members outside the household, friends, schoolmates, and teachers) during the pandemic. It comprises three items: “During the pandemic, I missed face-to-face meetings and the time with my grandparents (and other elderly or sick relatives)”, “During the pandemic, I missed face-to-face meetings and the time together with my friends”, and “During the pandemic, I missed the meetings with classmates and teachers at school”. The 5-point response scale ranges from “Never“ to “All the time”. The mean is used as a cut-off point that defines two groups of students—those who less frequently missed face-to-face contact with significant others and the group of young people who often missed such contact during the pandemic.
2.4. Biopsychological Factors
Young people’s experience with COVID-19 infection and treatment in hospital for COVID-19 is evaluated by two measures developed by the authors. The first one assesses if the adolescent or someone in the family ever had COVID-19: “Were you or anyone in your close family (i.e., parent, sibling or grandparent) ever test positive for COVID-19?”. The responses are grouped in the following categories: the adolescent or someone else in the family had COVID-19 infection; neither the adolescent, nor a family member was infected or the student does not know about this.
The second variable included in the analysis reflects the experience of treatment in hospital for COVID-19 of the adolescent or a family member. The question asked for the experience with hospitalisation is: “Were you or anyone in your close family (i.e., parent, sibling or grandparent) treated in hospital for COVID-19?”. The responses were grouped in the following categories: the adolescent or someone else in the family was treated in hospital for COVID-19; neither the adolescent, nor a family member was hospitalised or the respondent does not know about this.
3. Results
Table 1 presents the distribution of the main variables used in the analysis. The results show that, before the pandemic, alcohol consumption was the most prevalent risk behaviour among Bulgarian adolescents (28.9%), followed by drunkenness (16.3%) and cigarette smoking (12.4%). There is no information about the prevalence of vaping in the pre-pandemic period. At the end of the pandemic, vaping (22.5%) was the most prevalent health risk behaviour, followed by alcohol consumption (21.5%), drunkenness (20.7%), and cigarette smoking (19.2%).

Table 1.
Descriptive statistics of the main variables used in the analysis of Bulgarian adolescents’ health risk behaviours.
Information about ethnic belonging was not collected in HBSC-2018. The distribution from the survey conducted at end of the pandemic shows that most of the adolescents (83.9%) have Bulgarian ethnicity, while 16.1% belong to ethnic minorities (Turkish or Roma).
During the pandemic, most adolescents (74.5%) lived in a two-parent family, while in 2018 the share of young people living in this type of family was slightly higher (78.4%).
In more than half of the families (61.5%), a family member or the adolescent was infected with COVID-19 (23.2% of the adolescents were infected). In 24.4% of the families, a family member or the adolescent was treated in hospital for COVID-19 (4.9% of the adolescents report that they were treated in hospital for COVID-19).
At the end of the pandemic, a large proportion of adolescents demonstrated severe (44.3%) or moderate (27.7%) symptoms of generalised anxiety and almost half of the students reported that they missed the face-to-face meetings with close family members, friends, schoolmates and teachers at school. These variables are available only in the survey on adolescent health and well-being in the context of the COVID-19 pandemic (2022/2023).
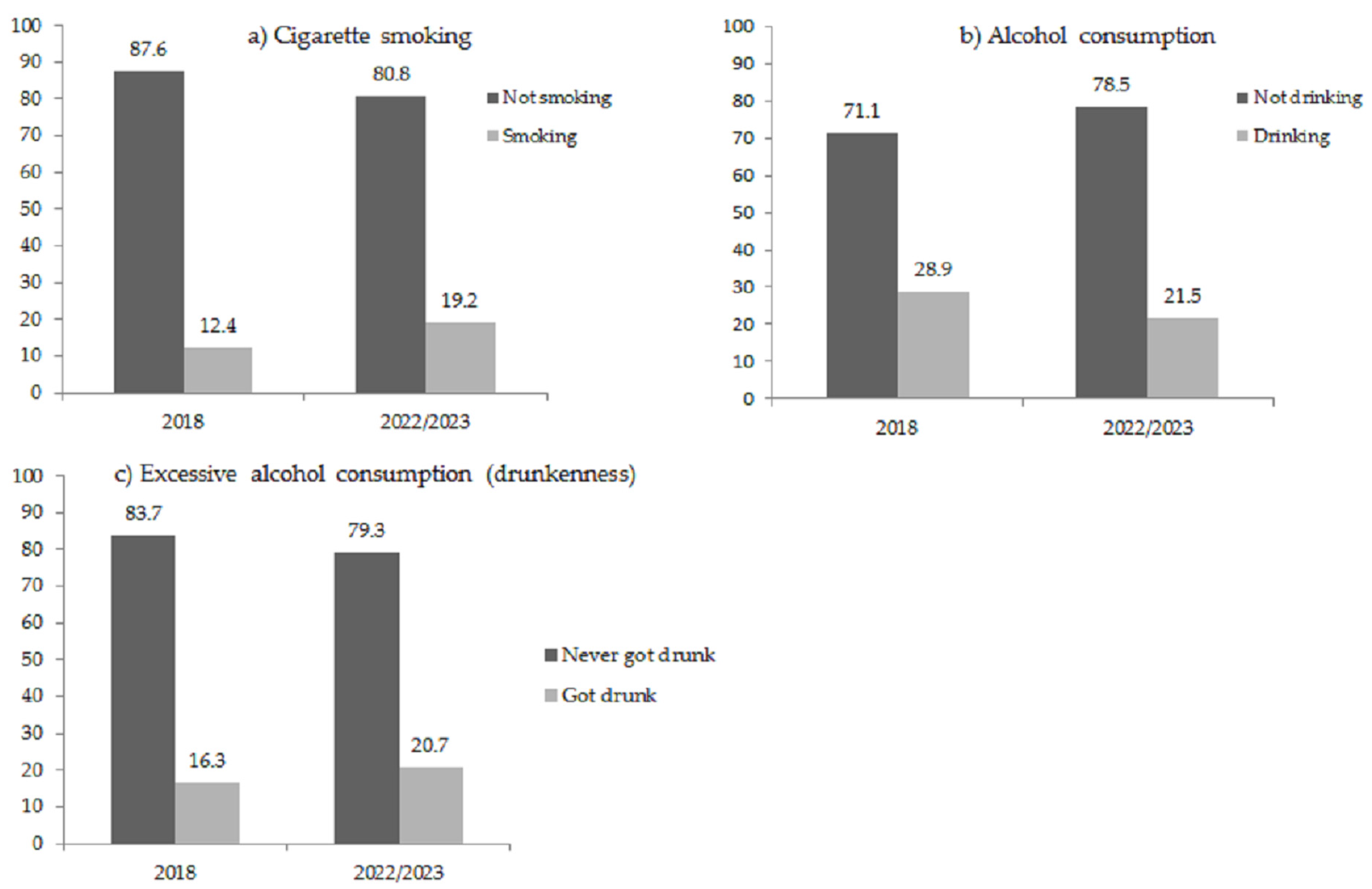
Figure 1 reveals that cigarette smoking increased from 12.4% in 2018 to 19.2% in 2022/2023. The share of students who frequently drink alcohol decreased from 28.9% in 2018 to 21.5% at the end of the pandemic. The excessive alcohol use (drunkenness) increased from 16.3% to 20.7%. There are no comparable data on the prevalence of vaping during the pre-pandemic period but data from European School Survey Project on Alcohol and Other Drugs (ESPAD) conducted in 2019 show that 13.4% of the young people aged 15–16 currently use e-cigarettes. In 2022/2023, the percentage of vapers in this age group was 32.1% although the survey data are not fully comparable [34].
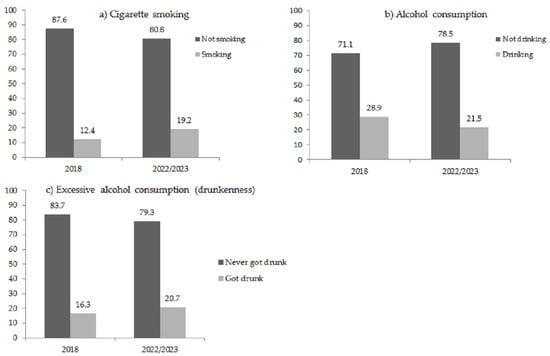
Figure 1.
Time trends of cigarette smoking, alcohol consumption and excessive alcohol use (drunkenness) among Bulgarian adolescents (%). The first panel (a) compares cigarette smoking estimated from HBSC-2018 and the survey on adolescent health and well-being in the context of the COVID-19 pandemic (2022/2023). The second panel (b) includes comparison of alcohol consumption estimated from HBSC-2018 and the survey on adolescent health and well-being in the context of the COVID-19 pandemic (2022/2023). The third panel (c) compares drunkenness estimated from HBSC-2018 and the survey on adolescent health and well-being in the context of the COVID-19 pandemic (2022/2023).
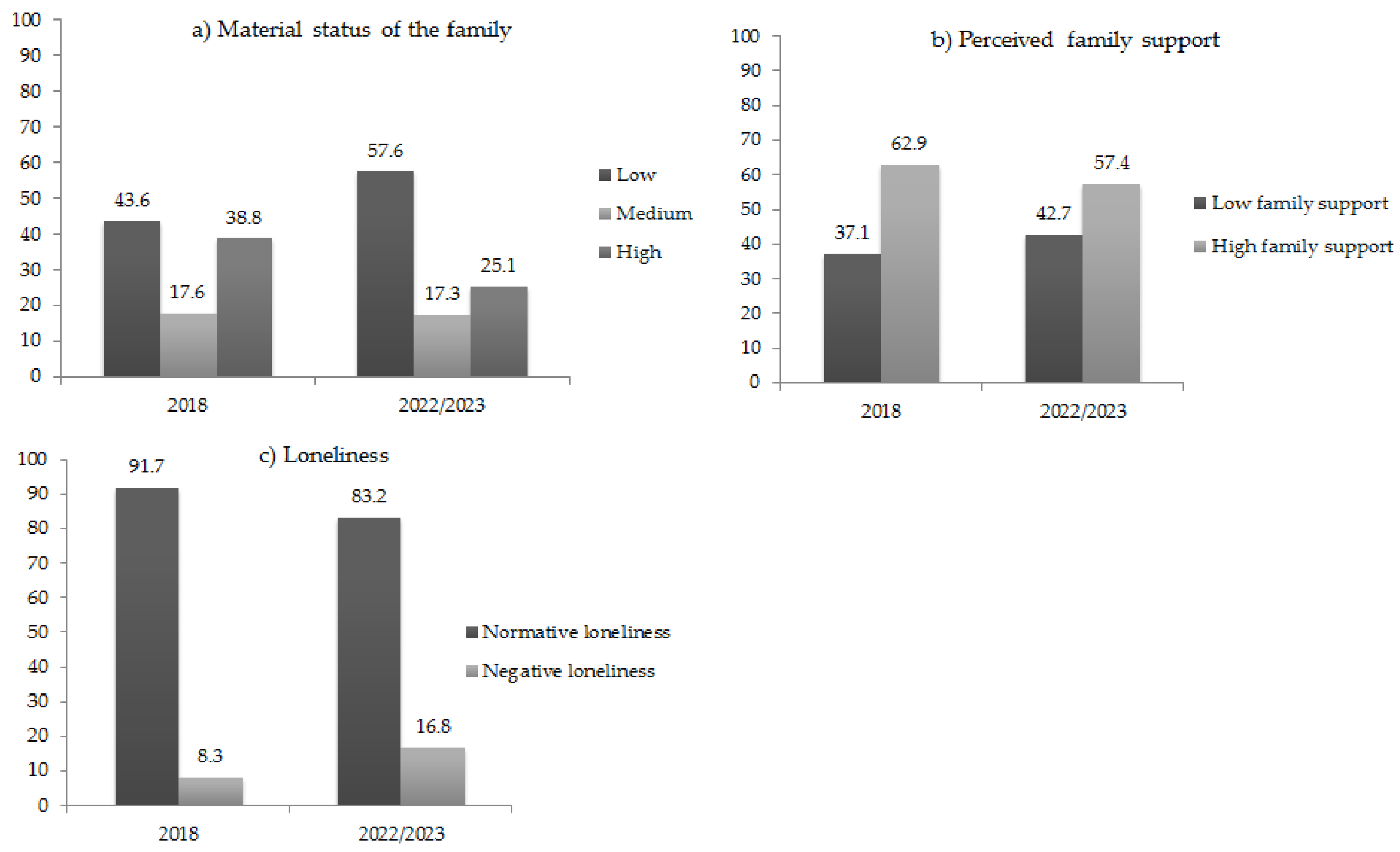
Figure 2 shows that the share of low material status families increased from 43.6% in 2018 to 57.6% in 2022/2023, revealing the negative socioeconomic implications of the pandemic. The share of high material status families decreased from 38.8% in 2018 to 25.1% in 2022/2023.
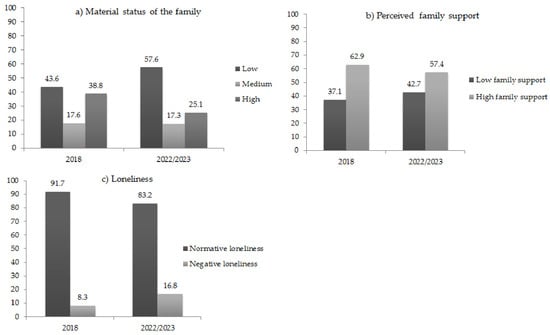
Figure 2.
The material status of the family, perceived family support and loneliness among Bulgarian adolescents in 2018 and 2022/2023 (%). The first panel (a) compares the material status of the family estimated from HBSC-2018 and the survey on adolescent health and well-being in the context of the COVID-19 pandemic (2022/2023). The second panel (b) compares perceived family support estimated from HBSC-2018 and the survey on adolescent health and well-being in the context of the COVID-19 pandemic (2022/2023). The third panel (c) compares loneliness estimated from HBSC-2018 and the survey on adolescent health and well-being in the context of the COVID-19 pandemic (2022/2023). HBSC-2018 includes a measure of loneliness that differs from the measure used in the survey on adolescent health and well-being in the context of the COVID-19 pandemic (2022/2023).
The comparison reveals also negative changes in adolescent mental health. Substantial increase is observed in the share of students living in low support families (37.1% in 2018 and 42.7% in 2022/2023). A 2-fold increase was observed in the share of young people who experienced negative forms of loneliness (from 8.3% in 2018 to 16.8% in 2022/2023). However, there are differences in the measures of loneliness used in the surveys.
3.1. Cigarette Smoking among Bulgarian Adolescents
The results from the logistic regression model of cigarette smoking among Bulgarian adolescents (model 2a in Table 2) show that, in 2018, the risk of smoking was significantly lower among boys compared to girls (reference group). Age has a significant positive association with the risk of cigarette smoking. In the pre-pandemic period, students who lived in single-parent families/foster care/with other relatives were significantly more likely to smoke cigarettes compared to those living with two parents (reference group). The material status of the family has no significant relationship with cigarette smoking. Students who live in low support families are significantly more likely to smoke cigarettes (reference group—adolescents living in high support families). Loneliness has no significant association with the risk of smoking in the pre-pandemic period.

Table 2.
Logistic regression models of cigarette smoking of Bulgarian adolescents.
Compared to the baseline model 2a, the analysis of the factors associated with the risk of smoking at the end of the pandemic reveals that there is no significant gender difference. The students aged 15–16 years old are significantly more likely to smoke cigarettes (model 2b in Table 2) compared to the youngest age group of 11–12 year olds (reference group). Young people from the Roma minority are also more likely to smoke cigarettes compared to students with Bulgarian ethnicity (reference group).
Similarly to the relationship observed in the pre-pandemic period, adolescents living in single-parent families/foster care/with other relatives have significantly higher odds of cigarette smoking (reference category—students living with two parents). Compared to the baseline model 2a, the analysis of the data from the period at the end of the pandemic reveals significantly increasing socioeconomic differences in the risk of smoking (model 2b). Students from high material status families are significantly more likely to smoke cigarettes compared to young people form medium status families (reference group). Young people who reported low family support at the end of the pandemic have significantly higher odds of cigarette smoking compared to students from high support families (reference group). This relationship is similar to that found in the pre-pandemic period.
The experience with COVID-19 infection of the adolescent or a family member is significantly associated with lower risk of cigarette smoking, while the experience of treatment in hospital does not have a significant effect. The absence of social contacts with significant others during the pandemic is not significantly associated with the risk of smoking.
Generalised anxiety has a significant relationship with cigarette smoking. Students with moderate or severe anxiety have significantly higher odds of smoking compared to young people with low anxiety (reference group). The association between generalised anxiety and the risk of cigarette smoking is estimated only at the end of the pandemic. Model 2b in Table 2 shows also that, at the end of the pandemic, loneliness is not significantly associated with the risk of cigarette smoking. Differences in the measures available in the datasets limit the comparison.
Next, model 2c tests the interdependence between cigarette smoking, family support and the experience of COVID-19 infection of the adolescent or a family member. The results show that students from low support families have significantly higher odds of cigarette smoking in both conditions of presence or absence of such experience. (The reference category includes adolescents living in high support families and having no experience with COVID-19 infection in family, or they do not know about this).
As a next step, we test the interdependence between the experience of COVID-19 infection and generalised anxiety (model 2d). The odds of cigarette smoking significantly increase among young people with severe or moderate anxiety in both conditions of presence or absence of experience with COVID-19 infection in the family. (The reference group includes adolescents with low anxiety, having no experience with COVID-19 infection in the family, or they do not know about this).
In model 2e, we test the interaction between generalised anxiety and the experience of treatment in hospital for COVID-19 of the adolescent or a family member. Young people with moderate or severe anxiety have significantly higher odds of cigarette smoking in both conditions of presence or absence of experience with treatment in hospital for COVID-19. (The reference group includes students with low anxiety, having no experience with treatment in hospital for COVID-19, including treatment of a family member, or they do not know about this).
3.2. Electronic Cigarette Smoking among Bulgarian Adolescents
In the next part of this study, we focus on the factors associated with e-cigarette use among Bulgarian adolescents at the end of the pandemic since there are no available data from the pre-pandemic period (Table 3). The results from model 3a reveal that there is no significant gender difference in e-cigarette smoking. The increase in age is significantly associated with higher odds of vaping, being highest in the oldest age group (15–16 year olds). Young people with Roma ethnicity have significantly higher odds of e-cigarette smoking compared to adolescents from the Bulgarian ethnic group (reference category).

Table 3.
Logistic regression models of electronic cigarette smoking of Bulgarian adolescents.
Students living in single-parent families/foster care/with other relatives are significantly more likely to smoke cigarettes compared to young people, living with two parents (reference group). Young people from low material status families are significantly less likely to smoke e-cigarettes, while, among adolescents from affluent families, the risk is significantly higher compared to the reference group (students from medium status families). Young people from low support families are significantly more likely to smoke e-cigarettes compared to adolescents from high support families (reference group). The limited social interaction with significant others during the pandemic is significantly associated with a higher risk of vaping.
The experience with COVID-19 infection in family is not in a significant relationship with vaping. However, the treatment in hospital for COVID-19 has a significant effect, showing that young people who were hospitalised or a family member was treated in hospital for COVID-19 are significantly more likely to use e-cigarettes. (The reference group includes students who were hospitalised or a family member was treated in hospital for COVID-19, or they do not know about this).
Young people with moderate or severe anxiety are significantly more likely to smoke e-cigarettes compared to students with low anxiety (reference category). Loneliness is not significantly associated with the risk of vaping.
In model 3b, we test the interaction between the experience with COVID-19 infection in family, family support and vaping. The odds of vaping are significantly higher among young people from low support families in both conditions of presence or absence of experience with COVID-19 infection in the family. (The reference category includes adolescents from high support families, having no experience with COVID-19 infection in the family, or they do not know about this).
In model 3c, we test the interdependence between the experience of COVID-19 infection, generalised anxiety and vaping. Adolescents with moderate or severe anxiety are significantly more likely to smoke e-cigarettes in both conditions of presence or absence of experience of COVID-19 infection in the family. (The reference group includes young people with low anxiety, having no experience with COVID-19 infection in the family, or they do not know about this).
Finally, model 3d tests the interdependence between treatment in hospital for COVID-19, generalised anxiety and vaping. Adolescents with moderate or severe anxiety are significantly more likely to use e-cigarettes in both conditions of presence or absence of experience of treatment in hospital for COVID-19. The risk of vaping is also significantly higher among students with low anxiety, who were treated, or a family member was hospitalised for COVID-19. (The reference group includes adolescents with low anxiety, having no experience with treatment in hospital for COVID-19, including treatment of a family member, or they do not know about this).
3.3. Alcohol Consumption among Bulgarian Adolescents
The results from the analysis of the factors associated with alcohol consumption among Bulgarian adolescents are presented in Table 4. The results from the baseline model 5a reveal that, in the pre-pandemic period, boys had significantly higher odds of alcohol use compared to girls (reference group). Age has a significant positive association with the risk of alcohol consumption. In the pre-pandemic period, students who lived in single-parent families/foster care/with other relatives were significantly more likely to drink alcohol compared to those living with two parents (reference group). Adolescents living in high material status families are significantly more likely to drink alcohol compared to students from medium status families (reference group). Young people from low support families are significantly more likely to drink alcohol compared to those living in high support families (reference group). In the pre-pandemic period, loneliness has a significant positive association with the risk of alcohol use.

Table 4.
Logistic regression models of alcohol consumption of Bulgarian adolescents.
Next, model 4b reveals that similarly to the pre-pandemic period, at the end of the pandemic, boys were significantly more likely to report higher alcohol use compared to girls (reference group). Age dependence remains similar. The group of 15–16-year-old students has significantly higher odds of alcohol consumption compared to the youngest age group (10–11 year olds—reference category). The risk of alcohol use is significantly higher among Roma adolescents compared to students with Bulgarian ethnicity (reference group).
Similarly to the pre-pandemic period, young people living with one parent/foster care/with other relatives have significantly higher risk of alcohol consumption compared to students living with both parents (reference group). Adolescents from less affluent families are significantly less likely to drink alcohol compared to young people from medium status families (reference group). In the pre-pandemic period, the differences between students from low and medium status families were not significant. The risk remains significantly higher among students from affluent families.
Similarly to the pre-pandemic period, young people living in low support families have significantly higher odds of alcohol use compared to students from high support families (reference group). Limited social interaction with significant others during the pandemic has no significant relationship with alcohol use. Moderate and severe anxiety is significantly associated with a higher risk of alcohol use. In the pre-pandemic period, negative forms of loneliness are associated with significantly lower risk of alcohol use. At the end of the pandemic, the difference is not statistically significant. Differences in the measures used in the surveys may affect these results.
There is no significant association between the experience of COVID-19 infection in the family or treatment in hospital for COVID-19 of the adolescent or a family member and alcohol consumption.
In model 4c, we test the interaction between family support, the experience of COVID-19 infection of the adolescent or a family member, and alcohol consumption. Low family support is significantly associated with a higher risk of alcohol use in both conditions of presence or absence of experience with COVID-19 infection in the family. (The reference category includes adolescents from high support families, having no experience with COVID-19 infection in the family, or they do not know about this).
The results from the interaction between the experience with COVID-19 infection in the family and generalised anxiety presented in model 4d reveal that young people with moderate or severe anxiety are significantly more likely to drink alcohol in both conditions of presence or absence of experience with COVID-19 infection in family. (The reference group includes adolescents with low anxiety, having no experience with COVID-19 infection in family, or they do not know about this).
Next, model 4e shows that young people with moderate or severe anxiety have significantly higher odds of alcohol use in both conditions of presence or absence of experience of treatment in hospital for COVID-19, including treatment of a family member. (The reference group includes adolescents with low anxiety, having no experience with treatment in hospital for COVID-19, including treatment of a family member, or they do not know about this).
3.4. Excessive Alcohol Use (Drunkenness) among Bulgarian Adolescents
In the next step of the analysis, we focus on the factors associated with excessive alcohol consumption (drunkenness) among Bulgarian adolescents (Table 5). The results from the baseline model 5a reveal that, in the pre-pandemic period, boys were significantly more likely to report alcohol misuse compared to girls (reference group). Age has a significant positive association with the risk of drunkenness. In the pre-pandemic period, students who lived in single-parent families/foster care/with other relatives were significantly more likely to report alcohol misuse compared to those living with two parents (reference group). High material status of the family is positively associated with the risk of alcohol misuse. Young people from low support families are significantly more likely to report alcohol misuse compared to those living in high support families (reference group). Loneliness has a significant positive association with the risk of alcohol misuse in the pre-pandemic period.

Table 5.
Logistic regression models of excessive alcohol use (drunkenness) of Bulgarian adolescents.
The results from model 5b reveal that similarly to the pre-pandemic period, the risk of alcohol misuse is significantly higher among boys compared to girls (reference group) at the end of the pandemic. The age dependence remains similar. The group of 15–16-year-old students has significantly higher odds of alcohol misuse compared to 11–12-year-old students (reference group). Roma adolescents are significantly more likely to report alcohol misuse compared to students with Bulgarian ethnicity.
Similarly to the pre-pandemic period, young people living with one parent/foster care/with other relatives have significantly higher risk of alcohol misuse compared to students living with both parents (reference group). The results from model 5b reveal increasing socioeconomic differences in the risk of alcohol misuse during the pandemic. The risk significantly decreases among adolescents from less affluent families compared to young people from medium status families (reference group). In the pre-pandemic period, the differences between these groups are not statistically significant. In the group of students from more affluent families, the risk of alcohol misuse remains significantly higher.
Similarly to the pre-pandemic period, young people from low support families are significantly more likely to report alcohol misuse compared to adolescents from high support families (reference category). Limited social interaction with significant others during the pandemic is not significantly associated with alcohol misuse.
The experience of COVID-19 infection in the family has no significant relationship with excessive alcohol use, while the experience of hospitalisation is associated with significantly higher risk.
Adolescents with moderate or severe anxiety are significantly more likely to report alcohol misuse compared to young people with low anxiety (reference group). In the pre-pandemic period, the association between loneliness and the risk of alcohol misuse is significant and positive. At the end of the pandemic, negative forms of loneliness have a significant negative relationship with drunkenness. Differences in the measures available in the surveys may affect these results.
In the next step of the analysis, we test the interaction between perceived family support, the experience of COVID-19 infection in the family, and alcohol misuse (model 5c). Adolescents living in low support families are significantly more likely to report alcohol misuse in both conditions of presence or absence of experience of COVID-19 infection in the family. (The reference group includes students from high support families, having no experience with COVID-19 infection in the family, or they do not know about this).
In model 5d, we test the interdependence between generalised anxiety, the experience with COVID-19 infection in the family, and alcohol misuse. Young people with moderate or severe anxiety are significantly more likely to report excessive alcohol use in both conditions of presence or absence of an experience with COVID-19 infection in the family. (The reference group includes adolescents with low anxiety, having no experience with COVID-19 infection in the family, or they do not know about this).
Finally, in model 5e, we test the interaction between the experiences of treatment in hospital for COVID-19 of the adolescent or a family member, generalised anxiety and alcohol misuse. Young people with moderate or severe anxiety have significantly higher odds of excessive alcohol use in both conditions of presence or absence of experience with treatment in hospital for COVID-19, including of a family member. (The reference group includes adolescents with low anxiety, having no experience with treatment in hospital for COVID-19, including of a family member, or they do not know about this).
3.5. Predicted Probabilities of Substance (Mis)Use at Different Levels of Perceived Family Support and Generalized Anxiety among Adolescents with Different Experiences of COVID-19 Infection in the Family or Treatment in Hospital for COVID-19, including Treatment in Hospital of a Family Member
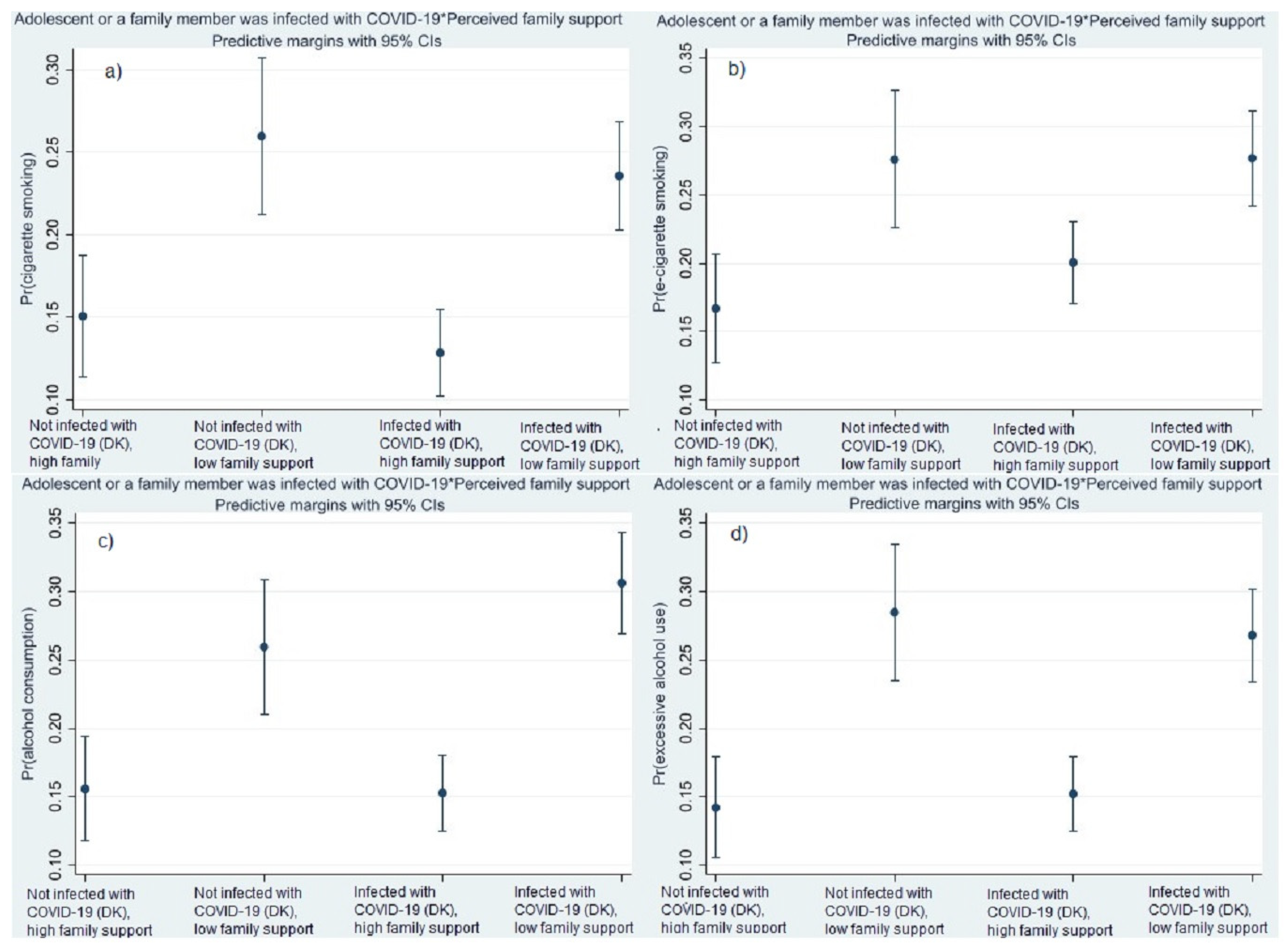
In the final step of the analysis, we estimate the predicted probabilities of cigarette smoking, vaping (e-cigarette smoking), alcohol consumption and excessive alcohol use (drunkenness) at different levels of perceived family support among adolescents with different experiences of COVID-19 infection in the family. The predicted probabilities are estimated from the survey on adolescent health and well-being in the context of the COVID-19 pandemic (2022/2023) (models 2c, 3c, 4c and 5c in Table 2, Table 3, Table 4 and Table 5).
The results reveal that the probabilities of cigarette smoking and alcohol misuse are highest among students from low support families who did not experience COVID-19 infection in the family (Figure 3a,d). The probability of vaping is highest in both groups of students from low support families, with and without experience of COVID-19 infection in the family (Figure 3b). The predicted probability of alcohol use is highest among students from low support families who experienced COVID-19 infection in the family Figure 3c).
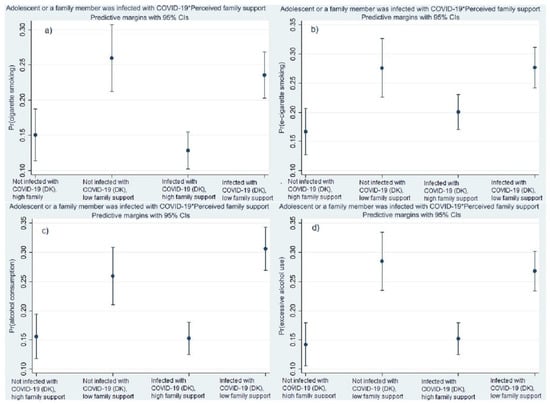
Figure 3.
Predicted probabilities of cigarette smoking (a), vaping (b), alcohol consumption (c) and excessive alcohol use (drunkenness) (d) at different levels of perceived family support among adolescents with different experience of COVID-19 infection in the family estimated from the survey on adolescent health and well-being in the context of the COVID-19 pandemic (2022/2023). The predicted probabilities are estimated from the models 2c, 3c, 4c and 5c in Table 2, Table 3, Table 4 and Table 5.
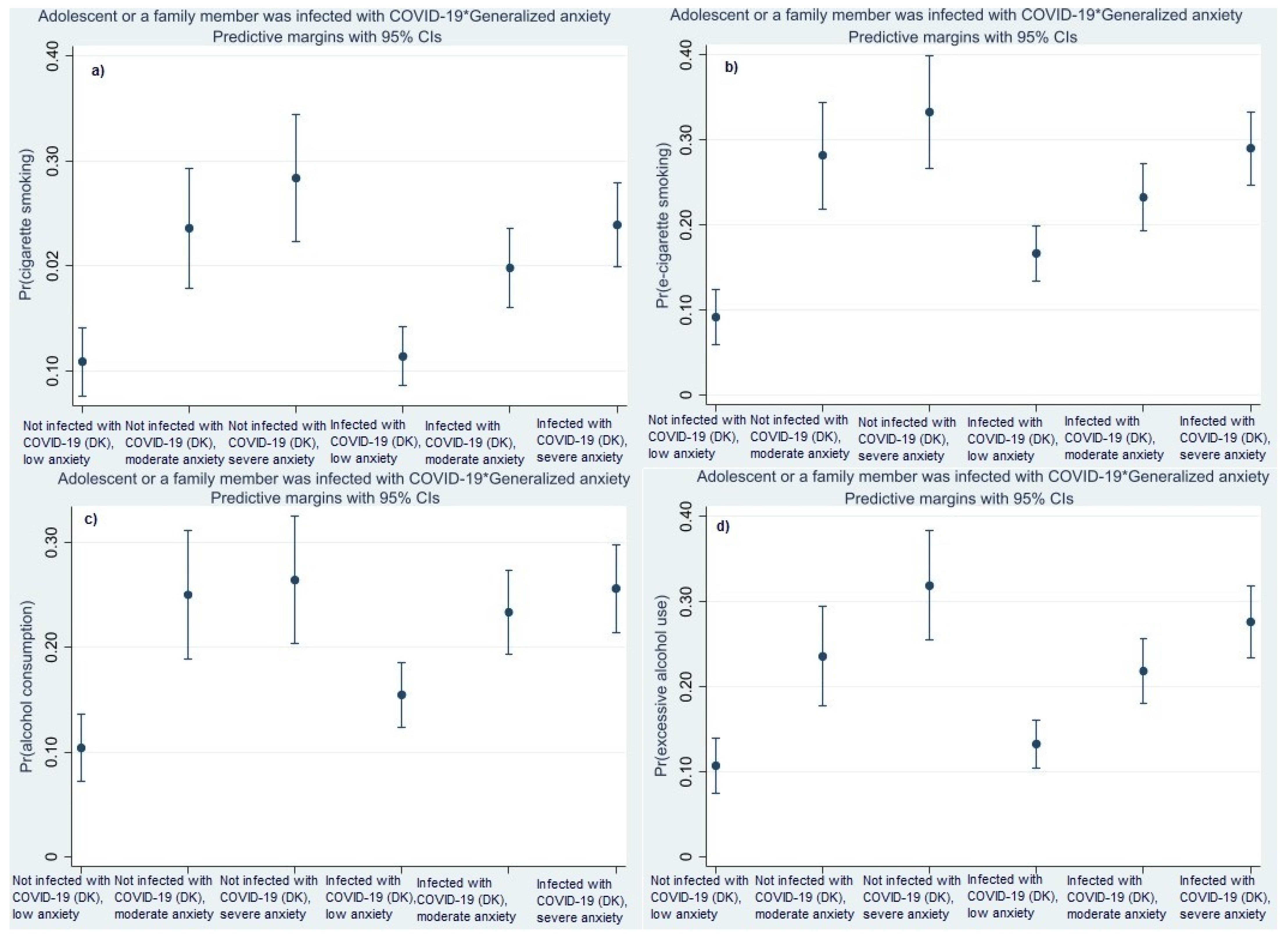
The predicted probabilities of cigarette smoking, vaping and alcohol misuse are highest among students with severe anxiety symptoms who did not experience COVID-19 infection in the family (Figure 4a,b,d). The predicted probability of alcohol consumption is highest in both groups of students with severe anxiety symptoms, with and without experience COVID-19 infection in the family (Figure 4c).
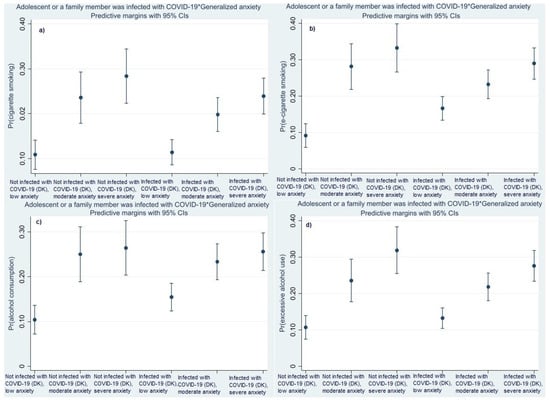
Figure 4.
Predicted probabilities of cigarette smoking (a), vaping (b), alcohol consumption (c) and excessive alcohol use (drunkenness) (d) at different levels of generalised anxiety among adolescents with different experience of COVID-19 infection in the family estimated from the survey on adolescent health and well-being in the context of the COVID-19 pandemic (2022/2023). The predicted probabilities are estimated from the models 2d, 3d, 4d and 5d in Table 2, Table 3, Table 4 and Table 5.
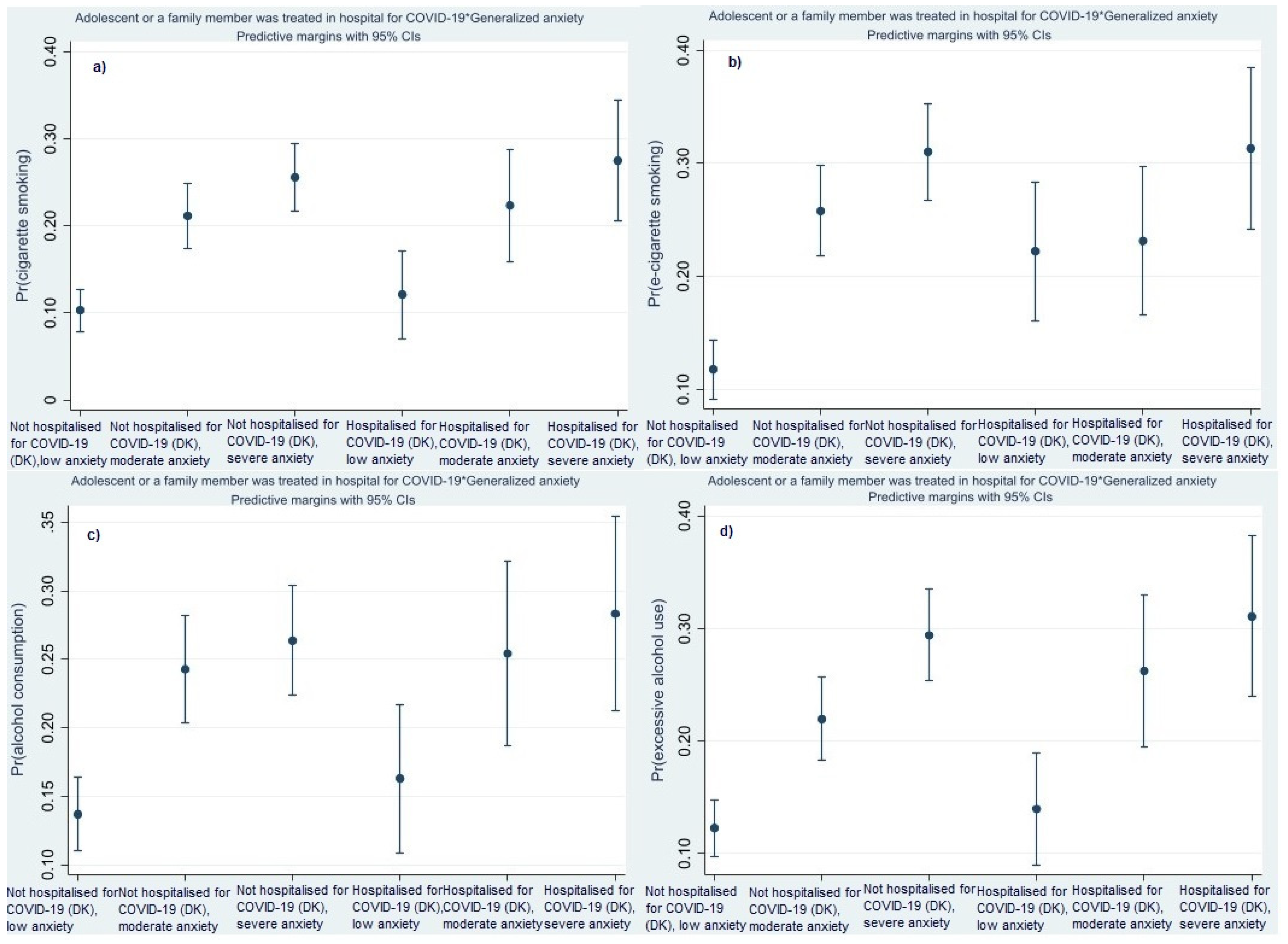
The predicted probability of cigarette smoking, alcohol consumption and drunkenness are highest in the group of students with severe anxiety symptoms who have experience with hospitalisation for COVID-19 (Figure 5a,c,d). The predicted probability of vaping is highest in both groups of students with severe anxiety symptoms, with and without experience of hospitalisation for COVID-19 including treatment in hospital of a family member (Figure 5b).
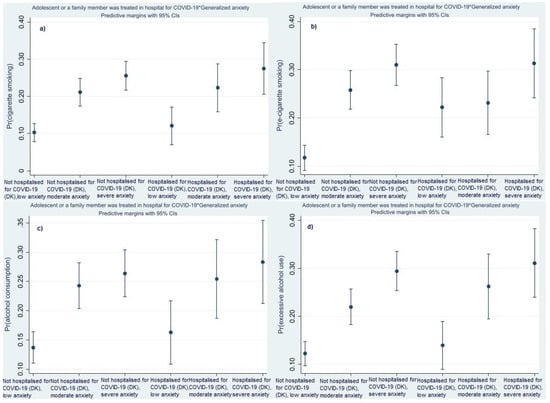
Figure 5.
Predicted probabilities of cigarette smoking (a), vaping (b), alcohol consumption (c) and excessive alcohol use (drunkenness) (d) at different levels of generalised anxiety among adolescents with different experience of treatment in hospital for COVID-19, including treatment in hospital of a family member estimated from the survey on adolescent health and well-being in the context of the COVID-19 pandemic (2022/2023). The predicted probabilities are estimated from the models 2e, 3e, 4e and 5e in Table 2, Table 3, Table 4 and Table 5.
4. Discussion
The present study focuses on the association between Bulgarian adolescents’ health risk behaviours (cigarette smoking, vaping (e-cigarette smoking), alcohol consumption and excessive alcohol use (drunkenness)) and biopsychosocial factors at the individual and interpersonal levels. The effect of the studied factors is evaluated by comparison with pre-pandemic data, which allows for a more dynamic perspective to adolescent health risk behaviours. The trends in the prevalence of the studied risk behaviours reveal an increase in cigarette smoking and excessive alcohol consumption (drunkenness) and a decrease in alcohol use. Diverging trends in substance use were found also in other surveys on young people’s health risk behaviours conducted in the pre-pandemic period such as the ESPAD survey [34]. There are no comparable data on vaping covering the pre-pandemic period and the factors associated with this health risk behaviour are studied at the end of the pandemic although ESPAD data from 2019 suggest for an increasing trend [34]. The trends also reveal a deterioration of the material status of the families and in young people’s mental health related to an increase in the share of students reporting low family support. Data on loneliness are not fully comparable.
The results from the multivariate analysis uncover significant gender differences in young people’s substance (mis)use. In the pre-pandemic period, the risk of cigarette smoking was significantly lower among boys compared to girls. At the end of the pandemic, gender differences in cigarette smoking was not statistically significant. At the end of the pandemic, gender differences in the risk of vaping was not statistically significant. In the case of alcohol (mis)use, the risk was significantly higher among boys compared to girls in both periods. Studies on adolescent health risk behaviours conducted in the pre-pandemic period in Bulgaria reveal that the risk of cigarette smoking was higher among girls, while the risk of alcohol consumption and alcohol misuse prevailed among boys [35]. Existing research found mixed trends in alcohol consumption among boys and girls during the pandemic. In certain countries, the risk of alcohol (mis)use was higher among boys [36]. In the case of Bulgarian adolescents, gender differences in the risk of alcohol (mis)use remained similar in both periods before and at the end of the pandemic. Studies found also increasing nicotine dependence among young people in certain countries during the pandemic related to an increased use of e-cigarettes [37]. In the case of Bulgarian adolescents, the gender difference in cigarette smoking was not statistically significant at the end of the pandemic unlike during the pre-pandemic period. This result shows that disproportional changes took place in cigarette smoking among boys and girls in Bulgaria.
In both periods, higher age is associated with an increase in substance (mis)use. Research shows that, in middle adolescence, smoking and alcohol consumption increasingly become socialising activities in young people’s interactions. Substance use serves as a means for gaining popularity and acceptance in peer groups [38]. The results from the present study show that the dependence between age and health risk behaviours is observed also in conditions of limited outdoor activities and face-to-face peer contact during the pandemic. In line with existing research, the results from the present study underline the need of an age-tailored approach in the interventions, aiming to reduce the prevalence of substance (mis)use among young people [17].
Ethnicity has a significant relationship with cigarette smoking, vaping, alcohol consumption and alcohol misuse at the end of the pandemic period. The risk of smoking, vaping and alcohol (mis)use is significantly higher among young people from the Roma ethnic group. Living in socially and economically disadvantaged communities, Roma adolescents are exposed from an early age to severe material deprivation, poverty, and limited access to health, educational and social services [39]. These socioeconomic disadvantages were greater during the pandemic which, in the case of Bulgarian minority youth, is associated also with an increased risk of substance (mis)use. Data on ethnic differences in adolescents’ health risk behaviours in the pre-pandemic period are not available for compassion.
Adolescents living in single-parent family, in foster care or with other relatives are more likely to engage in substance (mis)use in the two periods, before and at the end of the pandemic. Research finds higher emotional instability among children, living in single-parent households during the pandemic [40]. Higher economic vulnerability and emotional distress of single parents affects negatively young people’s mental health, increasing the risk of engagement in substance (mis)use [41].
The COVID-19 pandemic is associated with growing economic hardships in many countries, including Bulgaria, and deterioration of the material status of the families. The present study reveals that socioeconomic differences in adolescent health risk behaviours increased at the end of the pandemic. In the pre-pandemic period, the risk of alcohol misuse is significantly higher among adolescents from high material status families. In the case of smoking and alcohol consumption, the differences are not statistically significant. At the end of the pandemic Bulgarian adolescents from affluent families have significantly higher risk of smoking, vaping and alcohol (mis)use. In the same period, the risk of vaping, alcohol use and drunkenness significantly decreases among young people from low material status families. Studies conducted in Bulgaria and in other Eastern European countries in the pre-pandemic period uncover also a significant positive association between family affluence and the risk of cigarette smoking and alcohol consumption [42,43,44]. Existing studies show that unemployment of parents, deprivation, economic hardship and adolescents’ perceptions of family wealth are significantly associated with depression among young people, concluding that social and economic conditions are critical determinants of adolescents’ (mental) health during the pandemic [45,46].
Studies show that perceived family support is one of the significant predictors of general risk behaviours, cigarette smoking, alcohol consumption, drunkenness, and cannabis use during the pandemic [47]. Frequent family conflicts and a strained relationship with parents during the pandemic are associated with an increase in substance use among young people during this period [48]. Studies conducted in the period before the pandemic in Bulgaria uncover also a strong preventive effect of family support on adolescent health risk behaviours [49]. The results from the present study are in line with these finding, showing that low family support is associated with a higher risk of cigarette smoking, vaping and alcohol (mis)use among Bulgarian adolescents in both studied periods.
Studies reveal that worsened anxiety symptoms are associated with significantly higher risk of substance use during the pandemic [50,51]. Higher anxiety and loneliness in girls compared to boys is found among Bulgarian adolescents during the pandemic [52]. The present study uncovers also that moderate and severe anxiety is associated with a higher risk of cigarette smoking, vaping and alcohol (mis)use among young people in Bulgaria at the end of the pandemic. There are no available data on generalised anxiety in the pre-pandemic period.
Loneliness is a risk factor for poor mental health and substance use among young people [53,54]. Research shows that, during the pandemic, loneliness was often provoked by limited social interaction, imposed isolation and restricted socialising activities, which decreased the frequency of substance use [55]. In line with these studies, the present analysis reveals that, at the end of the pandemic, young people in Bulgaria who experienced negative forms of loneliness are less likely to engage in alcohol misuse. In the pre-pandemic period, negative forms of loneliness are associated with significantly higher risk of alcohol use and drunkenness. Difference in the measures used in the surveys limit the comparability of these results.
Limited social interaction with significant others is associated with a higher risk of vaping. Unsatisfactory contacts and relationships with family members, peers and friends during the pandemic increased the sense of social isolation in young people. At the same time, research shows that lower engagement in face-to-face socialising activities during the pandemic limits the access to substances, leading to lower substance use [56].
Young people who experienced COVID-19 infection in the family are less likely to smoke cigarettes, while the experience of treatment in hospital for COVID-19 of the adolescent or a family member, being treated in hospital, is associated with a higher risk of vaping and alcohol misuse. The predicted probabilities from the models with interaction between health risk behaviours, family support and the experience of COVID-19 infection in the family uncover that the negative experience with COVID-19 infection in the family have a depressive effect on health risk behaviours but the risk remains high among students from low support families. The predicted probabilities from the models with interaction between health risk behaviours, generalised anxiety and the experience of COVID-19 infection in the family shows that generalised anxiety and the experience of COVID-19 infection in the family have a depressive effect on substance use, but the risk remains high in the group of students with severe anxiety symptoms. Keeping in mind that only 4.9% of the sampled students were treated in hospital for COVID-19, in the case of hospitalisation the positive association with substance use can be explained as a coping mechanism in conditions of serious illness of a family member. Substance use as coping mechanism against the negative implications of the pandemic was also identified in existing studies, showing that coping was more common among young people who used the substances before the pandemic [57]. The interdependence between the experience of COVID-19 infection or treatment in hospital, anxiety and health risk behaviours among Bulgarian adolescents found in the present study is in line with these findings, showing that the stressful experiences with the virus are associated with a divergence in health risk behaviours, which also includes engagement in substance (mis)use. Research reveals a complex relationship between health risk behaviours, anxiety and fears from COVID-19 infection among adolescents, dependent also on the pre-pandemic substance use habits [58]. In particular, adolescents who smoked cigarettes before the pandemic had lower anxiety and fear from the virus, while young people who reduced smoking during the pandemic had lower coronavirus anxiety and higher coronavirus fears [58].
The findings from the present study suggest that the stressful experience of the COVID-19 pandemic may not necessarily make young people less engaged in substance (mis)use. Increasing health concerns, higher anxiety, low family support and negative experiences with COVID-19 infection and treatment in hospital of close family members have a diverging effect on adolescents’ health risk behaviours. Contextual factors and popular beliefs that certain substances are “less harmful” for health and the weak restrictions on their sales in the country create also a permissive environment, alleviating the access of the Bulgarian adolescents to different nicotine and alcoholic products. Research shows examples of the contextual factors, such as the policies of the tobacco companies during the COVID-19 pandemic in Spain, advertising the use of heated tobacco products as a replacement of the traditional cigarettes, which influenced the patterns of tobacco use [27,59]. Big companies such as Philip Morris International promoted heated tobacco product IQOS as a less harmful alternative to the regular cigarettes, which generated a false perception about its harmless effect [60]. According to ESPAD survey data from 2019 41.7% of the 15–16-year-old respondents in Bulgaria reported that that it would be very easy for to them to get cigarettes if they want and for 53.5% it would not be a problem to get spirits [61].
5. Conclusions
The present study explores health risk behaviours of (electronic) cigarette smoking and (excessive) alcohol consumption among Bulgarian adolescents during the COVID-19 pandemic and their associations with biopsychosocial factors at the individual and interpersonal levels. The effect of the studied factors is evaluated by comparison with pre-pandemic data. The prolonged social isolation, the risk of COVID-19 infection, the limited opportunities for face-to-face contact with significant others are associated with changes in young people’s behavioural health and increasing vulnerability of the adolescents during the pandemic. Low family support and higher anxiety stand out as risk factors strongly associated with substance (mis)use among Bulgarian students during the pandemic. However, concerns related to COVID-19 infection and the experience of serious illness in the family, leading to hospitalisation for COVID-19 are not necessarily associated with lower substance use. The results from the present study can serve as a baseline for future studies exploring the dynamics in the patterns of substance use among young people in the post-pandemic period.
5.1. Limitations of This Study
This study is based on two cross-sectional surveys with a similar sample design and selected variables for the analysis. This does not allow us to explore causality but the data allow for group-level comparisons. There are slight differences in the age groups in the surveys used in the present analysis. The measures of loneliness are also different. Information on vaping, ethnic belonging and generalised anxiety is not available from HBSC-2018.
5.2. Implications for Practice
The results from the present study reveal the need for effective and tailor-based interventions, offsetting the adverse social and psychological implications of the pandemic on young people’s health and well-being and, particularly, on their behavioural health and substance (mis)use. These interventions should consider the major role of familial factors in early to middle adolescence, particularly of low family support, which is associated with higher risk for cigarette smoking, vaping, alcohol consumption and drunkenness. The interventions should focus also on a specific group of young people at increased risk, i.e., different ages, genders and ethnic minorities (Roma teenagers in particular). The interventions should address the differential effect of socioeconomic inequalities (family affluence) on adolescents’ health risk behaviours. Adolescent anxiety exacerbated during the pandemic is associated with higher risk for engaging in the aforementioned health risk behaviours. The interventions should also target adolescent poor mental health as a risk factor for substance (mis)use. The results can be used for the development of programmes for prevention of health risks and psychosocial support of young people in times of large-scale health crises and societal disruptions such as the COVID-19 pandemic.
Author Contributions
Conceptualization, E.D. and A.A.-K.; methodology, E.D. and A.A.-K.; software, E.D.; validation, E.D. and A.A.-K.; formal analysis, E.D.; investigation, A.A.-K. and E.D.; resources, A.A.-K. and E.D.; data curation, A.A.-K. and E.D.; writing—original draft preparation, E.D. and A.A.-K.; writing—review and editing, E.D. and A.A.-K.; visualization, E.D.; supervision, A.A.-K.; project administration, A.A.-K.; funding acquisition, A.A.-K. and E.D. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the Bulgarian National Science Fund, Project No. KП-06-H55/7, within Competition for financial support of basic research projects—2021.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Ethics Committee of the Institute for Population and Human Studies at the Bulgarian Academy of Sciences (protocol code RD-5-90/5 May 2022).
Informed Consent Statement
Informed consent was obtained from the adolescents involved in the study and from their parents.
Data Availability Statement
The data presented in this study are available on request from the corresponding author. The data are not publicly available due to ethical restrictions (data contain sensitive personal information).
Conflicts of Interest
The authors declare no conflict of interest.
References
- Engel, G.L. The need for a new medical model: A challenge for biomedicine. Science 1977, 4286, 129–136. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention. The Social-Ecological Model: A Framework for Prevention. Atlanta (GA): Centers for Disease Control and Prevention. 2007. Available online: https://www.cdc.gov/violenceprevention/about/social-ecologicalmodel.html (accessed on 12 July 2023).
- Rangachev, A.; Marinov, G.K.; Mladenov, M. The demographic and geographic impact of the COVID pandemic in Bulgaria and Eastern Europe in 2020. Sci. Rep. 2020, 12, 6333. [Google Scholar] [CrossRef] [PubMed]
- Džakula, A.; Banadinović, M.; Lovrenčić, I.L.; Vajagić, M.; Dimova, A.; Rohova, M.; Minev, M.; Scintee, S.G.; Vladescu, C.; Farcasanu, D.; et al. A comparison of health system responses to COVID-19 in Bulgaria, Croatia and Romania in 2020. Health Policy 2022, 5, 456–464. [Google Scholar] [CrossRef]
- Rangachev, A.; Marinov, G.K.; Mladenov, M. The impact and progression of the covid-19 pandemic in Bulgaria in its first two years. Vaccines 2022, 10, 1901. [Google Scholar] [CrossRef] [PubMed]
- Summary of the Research Results of the Subjective Assessment and the Reactions of Teenagers in the Situation of Emergency Condition Related to COVID-19. UNICEF-Bulgaria Report. 2019. Available online: https://www.unicef.org/bulgaria/media/7851/file/BGR-COVID-and-teenagers-report.pdf (accessed on 12 July 2023).
- COVID-19 and Its Impact on Keeping Children Safe Online. UNICEF-Bulgaria Report. 2019. Available online: https://www.unicef.org/bulgaria/media/7181/file (accessed on 12 July 2023).
- Growing Up in a Connected World. Innocenti Research Report. 2019. Available online: https://www.unicef-irc.org/publications/pdf/GKO%20Summary%20Report.pdf (accessed on 12 July 2023).
- Smith, L.; Jacob, L.; Trott, M.; Yakkundi, A.; Butler, L.; Barnett, Y.; Armstrong, N.C.; McDermott, D.; Schuch, F.; Meyer, J.; et al. The association between screen time and mental health during COVID-19: A cross sectional study. Psychiatry Res. 2020, 292, 113333. [Google Scholar] [CrossRef]
- Bates, L.C.; Zieff, G.; Stanford, K.; Moore, J.B.; Kerr, Z.Y.; Hanson, E.D.; Barone Gibbs, B.; Kline, C.E.; Stoner, L. COVID-19 impact on behaviors across the 24-hour day in children and adolescents: Physical activity, sedentary behavior, and sleep. Children 2020, 7, 138. [Google Scholar] [CrossRef]
- Wang, Z.; Yeung, P.L.; Gao, X. Under the same roof: Parents’ COVID-related stress mediates the associations between household crowdedness and young children’s problem behaviors during social distancing. Curr. Res. Soc. Psych. 2021, 2, 100022. [Google Scholar] [CrossRef]
- Whitley, J.; Miriam, H.; Beauchamp, M.H.; Brown, C. The impact of COVID-19 on the learning and achievement of vulnerable Canadian children and youth. Facets 2021, 6, 1693. [Google Scholar] [CrossRef]
- Spinka, S.; Philippon, A.; Nezet, O.; Janssen, E.; Eroukmanoff, V.; Godeau, E. Alcohol, Tobacco and Cannabis Use among Ninth Grade Students (14–15-Year-Olds) in 2021. First Results of the EnCLASS Survey among 2000 Ninth Grade Students. Tendances 2021, 148. Available online: https://www.documentation-administrative.gouv.fr/adm-01859734/document (accessed on 12 June 2023).
- Schiliro, M.; Vogel, E.R.; Paolini, L.; Pabelick, C.M. Cigarette smoke exposure, pediatric lung disease, and COVID-19. Front. Physiol. 2021, 12, 652198. [Google Scholar] [CrossRef]
- Miech, R.; Patrick, M.E.; Keyes, K.; O’Malley, P.M.; Johnston, L. Adolescent drug use before and during U.S. national COVID-19 social distancing policies. Drug Alcohol Depend. 2021, 226, 108822. [Google Scholar] [CrossRef] [PubMed]
- Villanti, A.C.; LePine, S.E.; Peasley-Miklus, C.; West, J.C.; Roemhildt, M.; Williams, R.; Copeland, W.E. COVID-related distress, mental health, and substance use in adolescents and young adults. Child. Adolesc. Ment. Health 2022, 2, 138–145. [Google Scholar] [CrossRef] [PubMed]
- Wise, J. Drop in smoking and drug use among school children but increase in vaping, survey shows. BMJ 2022, 378, o2174. [Google Scholar] [CrossRef]
- Lee, S.; Choi, M.; Kim, D.; Shin, J.; Kim, J. Did the COVID-19 lockdown reduce smoking rate in adolescents? Int. J. Environ. Res. Public Health 2022, 1, 139. [Google Scholar] [CrossRef] [PubMed]
- Osinibi, M.; Gupta, A.; Harman, K.; Bossley, C.; Bossley, C. Increased exposure to tobacco smoke for children during the COVID-19 era. Eur. Respir. J. 2021, 58, OA2579. [Google Scholar] [CrossRef]
- Layman, H.M.; Thorisdottir, I.E.; Halldorsdottir, T.; Sigfusdottir, I.D.; Allegrante, J.P.; Kristjansson, A.L. Substance use among youth during the COVID-19 pandemic: A systematic review. Curr. Psychiatry Rep. 2022, 6, 307–324. [Google Scholar] [CrossRef]
- Patrick, M.E.; Parks, M.J.; Fairlie, A.M.; Kreski, N.T.; Keyes, K.M.; Miech, R. Using substances to cope with the COVID-19 pandemic: U.S. national data at age 19 years. J. Adolesc. Health 2022, 2, 340–344. [Google Scholar] [CrossRef]
- Prowse, R.; Sherratt, F.; Abizaid, A.; Gabrys, R.L.; Hellemans, K.G.C.; Patterson, Z.R.; McQuaid, R.J. Coping with the COVID-19 pandemic: Examining gender differences in stress and mental health among university students. Front. Psychiatry 2021, 12, 650759. [Google Scholar] [CrossRef]
- Zolopa, C.; Burack, J.A.; O’Connor, R.M.; Corran, C.; Lai, J.; Bomfim, E.; DeGrace, S.; Dumont, J.; Larney, S.; Wendt, D. Changes in youth mental health, psychological wellbeing, and substance use during the COVID-19 pandemic: A rapid review. Adolescent. Res. Rev. 2022, 7, 161–177. [Google Scholar] [CrossRef]
- Velikova, T.; Jenkov, V.; Kotsev, S.; Georgiev, D.; Batselova, H. Mental health issues related to some COVID-19 aspects: Online-based bulgarian survey. Arch. Immunol. 2020, 1, 26–29. [Google Scholar] [CrossRef]
- Impact of the COVID-19 Pandemic on the Preschool and School Education—SWOT Analysis of the Effects of Distance Learning. UNICEF-Bulgaria. 2019. Available online: https://www.unicef.org/bulgaria/en/media/11006/file (accessed on 12 July 2023).
- Inchley, J.; Currie, D.; Cosma, A.; Samdal, O. (Eds.) Health Behaviour in School-Aged Children (HBSC) Study Protocol: Background, Methodology and Mandatory Items for the 2017/18 Survey; CAHRU: St. Andrews, UK, 2018. [Google Scholar]
- Andueza, A.; Del Arco-Osuna, M.Á.; Fornés, B.; González-Crespo, R.; Martín-Álvarez, J.M. Using the statistical machine learning models ARIMA and SARIMA to measure the impact of Covid-19 on official provincial sales of cigarettes in Spain. Int. J. Interact. Multimed. Artif. Intell. 2023, 1, 73–87. [Google Scholar] [CrossRef]
- Makransky, G.; Schnohr, C.W.; Torsheim, T.; Currie, C. Equating the HBSC family affluence scale across survey years: A method to account for item parameter drift using the Rasch model. Qual. Life Res. 2014, 23, 2899–2907. [Google Scholar] [CrossRef]
- Torsheim, T.; Cavallo, F.; Levin, K.A.; Schnohr, C.; Mazur, J.; Niclasen, B.; Currie, C. Psychometric validation of the revised family affluence scale: A latent variable approach. Child Indic. Res. 2016, 9, 771–784. [Google Scholar] [CrossRef] [PubMed]
- Mossman, S.A.; Luft, M.J.; Schroeder, H.K.; Varney, S.T.; Fleck, D.E.; Barzman, D.H.; Gilman, R.; DelBello, M.P.; Strawn, J.R. The Generalized Anxiety Disorder 7-item Scale in Adolescents with Generalized Anxiety Disorder: Signal detection and validation. Ann. Clin. Psychiatry 2017, 29, 227–234A. [Google Scholar]
- Spitzer, R.L.; Kroenke, K.; Williams, J.B.; Löwe, B. A Brief measure for assessing Generalized Anxiety Disorder: The GAD-7. Arch. Intern. Med. 2006, 10, 1092–1097. [Google Scholar] [CrossRef]
- Madsen, K.R.; Damsgaard, M.T.; Rubin, M.; Jervelund, S.S.; Lasgaard, M.; Walsh, S.; Stevens, G.; Holstein, B. Loneliness and ethnic composition of the school class: A nationally random sample of adolescents. J. Youth. Adolesc. 2016, 7, 1350–1365. [Google Scholar] [CrossRef] [PubMed]
- Zimet, G.D.; Dahlem, N.W.; Zimet, S.G.; Farley, G.K. The multidimensional scale of perceived social support. J. Pers. Assess. 1988, 52, 30–41. [Google Scholar] [CrossRef]
- ESPAD Group. ESPAD Report 2019: Results from the European School Survey Project on Alcohol and Other Drugs; EMCDDA Joint Publications, Publications Office of the European Union: Luxembourg, 2020; Available online: https://www.emcdda.europa.eu/publications/joint-publications/espad-report-2019_en (accessed on 12 July 2023).
- Dimitrova, E.; Kotzeva, T.; Alexandrova-Karamanova, A. Psychosocial school environment and health risk behaviours of adolescents in Bulgaria: Results from multilevel analysis. Int. J. Public Health 2020, 8, 1331–1344. [Google Scholar] [CrossRef]
- Gohari, M.R.; Varatharajan, T.; MacKillop, J.; Leatherdale, S.T. Examining the Impact of the COVID-19 Pandemic on youth alcohol consumption: Longitudinal changes from pre-to intra-pandemic drinking in the COMPASS Study. J. Adolesc. Health 2022, 6, 665–672. [Google Scholar] [CrossRef]
- Parks, M.J.; Fleischer, N.L.; Patrick, M.E. Increased nicotine vaping due to the COVID-19 pandemic among US young adults: Associations with nicotine dependence, vaping frequency, and reasons for use. Prev Med. 2022, 159, 107059. [Google Scholar] [CrossRef]
- Keyzers, A.; Lee, S.K.; Dworkin, J. Peer pressure and substance use in emerging adulthood: A latent profile analysis. Subst. Use Misuse 2020, 10, 1716–1723. [Google Scholar] [CrossRef] [PubMed]
- Un/Equal Childhood: Deep Dive in Child Poverty and Social Exclusion in Bulgaria. UNICEF-Bulgaria Report. 2022. Available online: https://www.unicef.org/bulgaria/media/12976/file/UnequalChildhoodDeepDiveAnalysisEN.pdf (accessed on 12 July 2023).
- Naito, T.; Tomata, Y.; Otsuka, T.; Tsuno, K.; Tabuchi, T. Did children in single-parent households have a higher probability of emotional instability during the COVID-19 pandemic? A nationwide cross-sectional study in Japan. J. Environ. Res. Public Health 2022, 7, 4239. [Google Scholar] [CrossRef] [PubMed]
- Sinko, L.; He, Y.; Kishton, R.; Ortiz, R.; Jacobs, L.; Fingerman, M. The stay at home order is causing things to get heated up: Family conflict dynamics during COVID-19 from the perspectives of youth calling a national child abuse hotline. J. Fam. Violence 2022, 5, 837–846. [Google Scholar] [CrossRef] [PubMed]
- Dimitrova, E.; Kotzeva, T. Socio-economic inequalities and risk behaviors among school-aged children in Bulgaria: Results of the HBSC. Sociol. Probl. 2019, 1, 102–124. [Google Scholar]
- Kotzeva, T.; Dimitrova, E. Risky Behaviours: Tracking Youth Health and Well-Being in Bulgaria 2006–2018. In Wohlbefinden und Gesundheit im Jugendalter. Theoretische Perspektiven, Empirische Befunde und Praxisansätze; Heinen, A., Samuel, R., Vögele, C., Willems, H., Eds.; Springer-VSL: Wiesbaden, Germany, 2022; pp. 665–688. Available online: https://link.springer.com/chapter/10.1007/978-3-658-35744-3_30 (accessed on 12 July 2023).
- Piko, B.; Fitzpatrick, K. Socioeconomic status, psychosocial health and health behaviours among Hungarian adolescents. Eur. J. Public Health 2007, 4, 353–360. [Google Scholar] [CrossRef] [PubMed]
- Jeriček Klanšček, H.; Furman, L. Socioeconomic deprivation and inequalities in mental well-being during the COVID-19 pandemic among adolescents. Int. J. Environ. Res. Public Health 2023, 20, 6233. [Google Scholar] [CrossRef] [PubMed]
- Kim, B.; Kim, D.H.; Jang, S.Y.; Shin, J.; Lee, S.G.; Kim, T.H. Family economic hardship and adolescent mental health during the COVID-19 pandemic. Front. Public Health 2022, 10, 904985. [Google Scholar] [CrossRef]
- Shapiro, O.; Gannot, R.N.; Green, G.; Zigdon, A.; Zwilling, M.; Giladi, A.; Ben-Meir, L.; Adilson, M.; Barak, S.; Harel-Fisch, Y.; et al. Risk behaviours, family support, and emotional health among adolescents during the COVID-19 pandemic in Israel. Int. J. Environ. Res. Public Health 2022, 19, 3850. [Google Scholar] [CrossRef]
- Kapetanovic, S.; Ander, B.; Gurdal, S.; Gurdal, S.; Sorbring, E. Adolescent smoking, alcohol use, inebriation, and use of narcotics during the Covid-19 pandemic. BMC Psychol. 2022, 10, 44. [Google Scholar] [CrossRef]
- Dimitrova, E.; Kotzeva, T. Adolescent risk behaviours and family settings in Bulgaria: An evidence-based approach to effective family support policies. J. Mother Child 2022, 3, 139–150. [Google Scholar]
- Sharma, P.; Kamath, C.; Kurani, S.; Pazdernik, V.; Kremers, H.M.; St Sauver, J.; Croarkin, P.; Geske, J.; Prasad, K.; Patten, C.; et al. Pravesh Sharma and others, Longitudinal correlates of increased alcohol use among adolescents and young adults during the COVID-19 pandemic. Alcohol Alcohol. 2022, 6, 648–655. [Google Scholar] [CrossRef]
- Paunova-Markova, E.; Alexandrova-Karamanova, A.; Yordanova, T.; Mineva, K. Impact of the Covid-19 Pandemic on adolescent mental health and well-being. Cent. Eur. J. Paediatr. 2023, 1, 54–64. [Google Scholar] [CrossRef]
- Alexandrova-Karamanova, A.; Kotzeva, T.; Paunova-Markova, E.; Mineva, K.; Dimitrova, E.; Yordanova, T. COVID-19 exposure and COVID-19 disease in the family: Effects on adolescent mental health. Bulg. J. Psychol. 2023, 1, 267–284. [Google Scholar]
- Herchenroeder, L.; Post, S.M.; Stock, M.L.; Yeung, E.W. Loneliness and alcohol-related problems among college students who report binge drinking behaviour: The moderating role of food and alcohol disturbance. Int. J. Environ. Res. Public Health 2022, 21, 13954. [Google Scholar] [CrossRef]
- Qin, J.; Ding, Y.; Gao, J.; Wu, Y.; Lv, H.; Wu, J. Effects of COVID-19 on mental health and anxiety of adolescents aged 13–16 years: A comparative analysis of longitudinal data from China. Front. Psychiatry 2021, 12, 695556. [Google Scholar] [CrossRef] [PubMed]
- Vallentin-Holbech, L.; Ewing, S.W.F.; Thomsen, K.R. Hazardous alcohol use among Danish adolescents during the second wave of COVID-19: Link between alcohol use and social life. Nord. Stud. Alcohol Drugs 2023, 2, 127–145. [Google Scholar] [CrossRef]
- Racine, N.; McArthur, B.A.; Cooke, J.E.; Eirich, R.; Zhu, J.; Madigan, S. Global Prevalence of depressive and anxiety symptoms in children and adolescents during COVID-19: A meta-analysis. JAMA Pediatr. 2021, 11, 1142–1150. [Google Scholar] [CrossRef]
- Cho, J.; Bello, M.S.; Christie, N.C.; Monterosso, J.R.; Leventhal, A.M. Adolescent emotional disorder symptoms and transdiagnostic vulnerabilities as predictors of young adult substance use during the COVID-19 pandemic: Mediation by substance-related coping behaviors. Cogn. Behav. Ther. 2021, 4, 276–294. [Google Scholar] [CrossRef]
- Çelik, M.Y.; Fatma Karasu, F.; Çopur, E.Ö.; Sungur, M. The relationship of coronavirus disease 2019 fear and anxiety with smoking and caffeinated beverage consumption in young people. J. Educ. Res. Nurs. 2023, 2, 178–185. [Google Scholar] [CrossRef]
- Almeida, A.; Galiano, A.; Golpe, A.A.; Martín-Álvarez, J.M. The usefulness of marketing strategies in a regulated market: Evidence from the Spanish tobacco market. EM Econ. Manag. 2021, 2, 171–188. [Google Scholar] [CrossRef]
- Golpe, A.A.; Martín-Álvarez, J.M.; Galiano, A.; Asensio, E. Effect of IQOS introduction on Philip Morris International cigarette sales in Spain: A Logarithmic Mean Divisa Index decomposition approach. Gac. Sanit. 2022, 4, 293–300. [Google Scholar] [CrossRef] [PubMed]
- European School Survey Project on Alcohol and Other Drugs (ESPAD).Online Database. Available online: https://data.espad.org/search-questions/?field-text=alcohol (accessed on 12 July 2023).
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).