Acute Effects of Static Self-Stretching Exercises and Foam Roller Self-Massaging on the Trunk Range of Motions and Strength of the Trunk Extensors
Abstract
:1. Introduction
2. Materials and Methods
2.1. Subjects
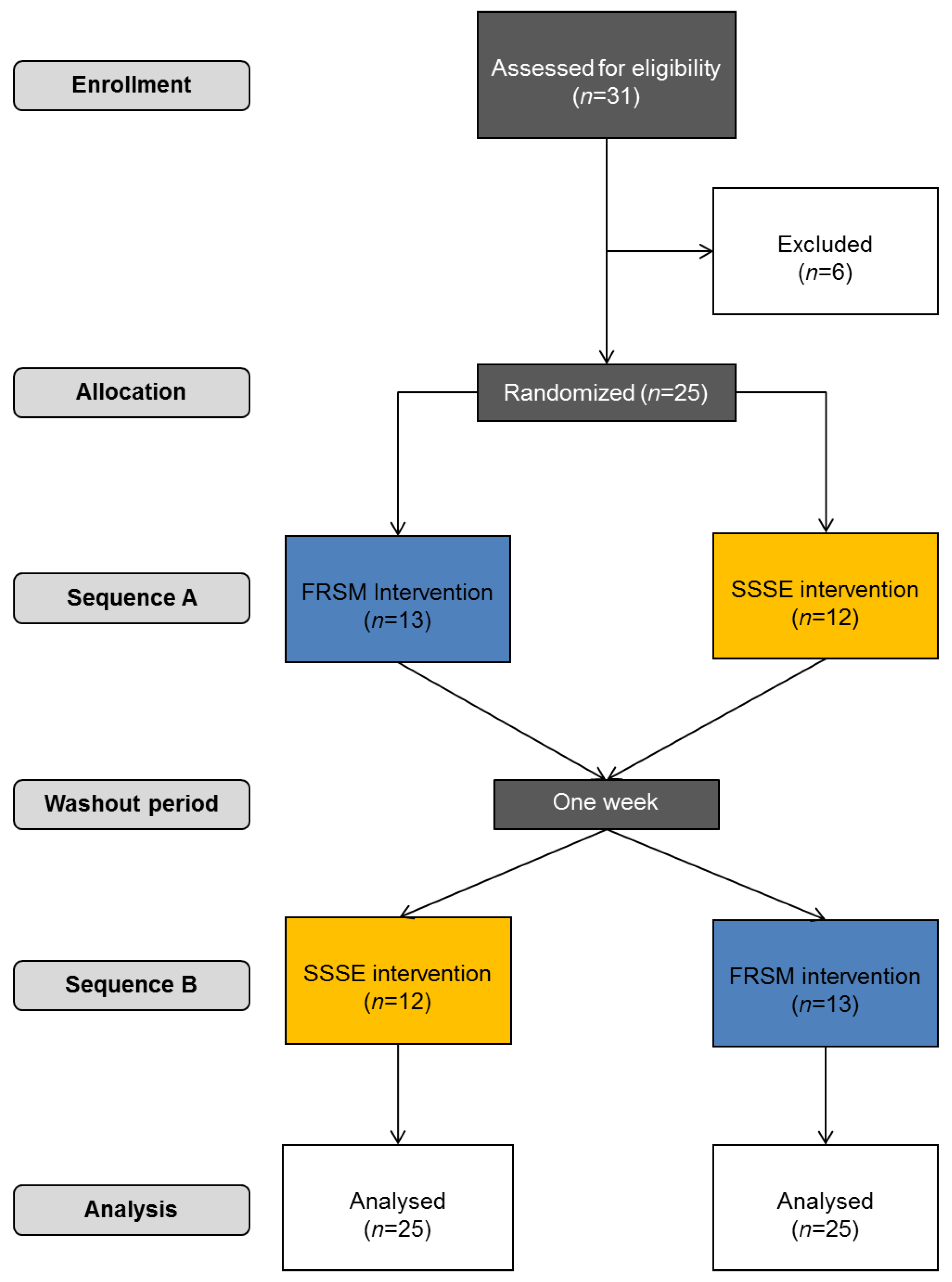
2.2. Study Procedure
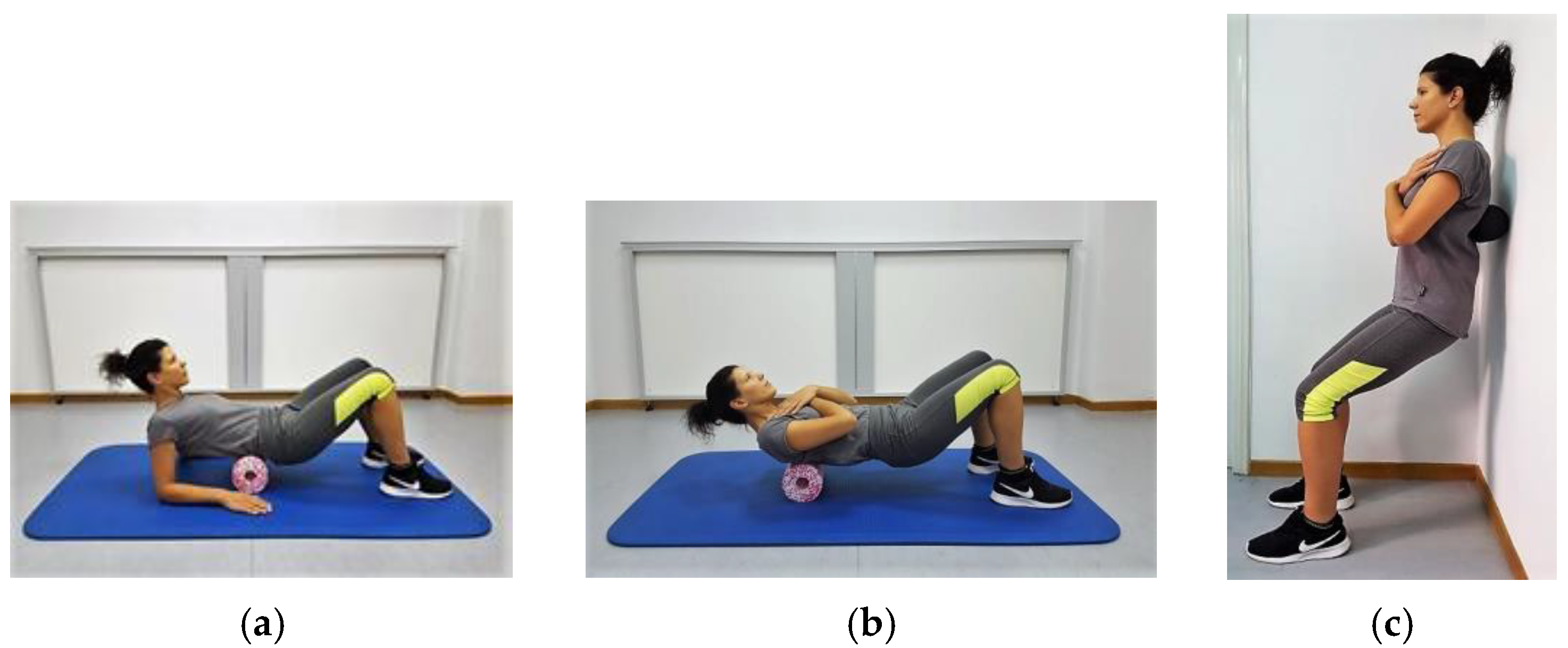
2.2.1. Foam Roller Self-Massaging Protocol
2.2.2. Static Self-Stretching Exercise Protocol
2.3. Outcome Measures
2.3.1. Range of Motion Measurements
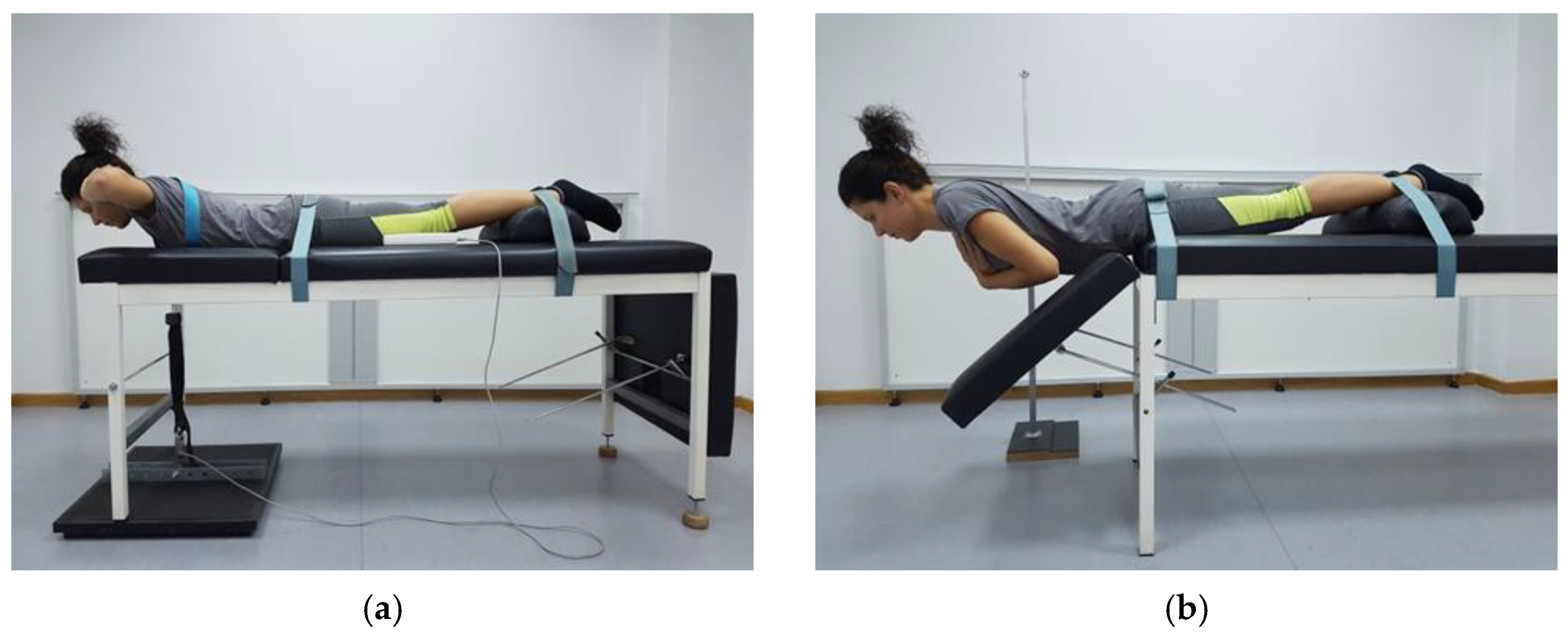
2.3.2. Muscle Strength and Endurance Measurements
2.3.3. Reliability of the Outcome Measures
2.4. Trainees’ Satisfaction towards Intervention
2.5. Statistical Analysis
3. Results
3.1. Range of Trunk Movements
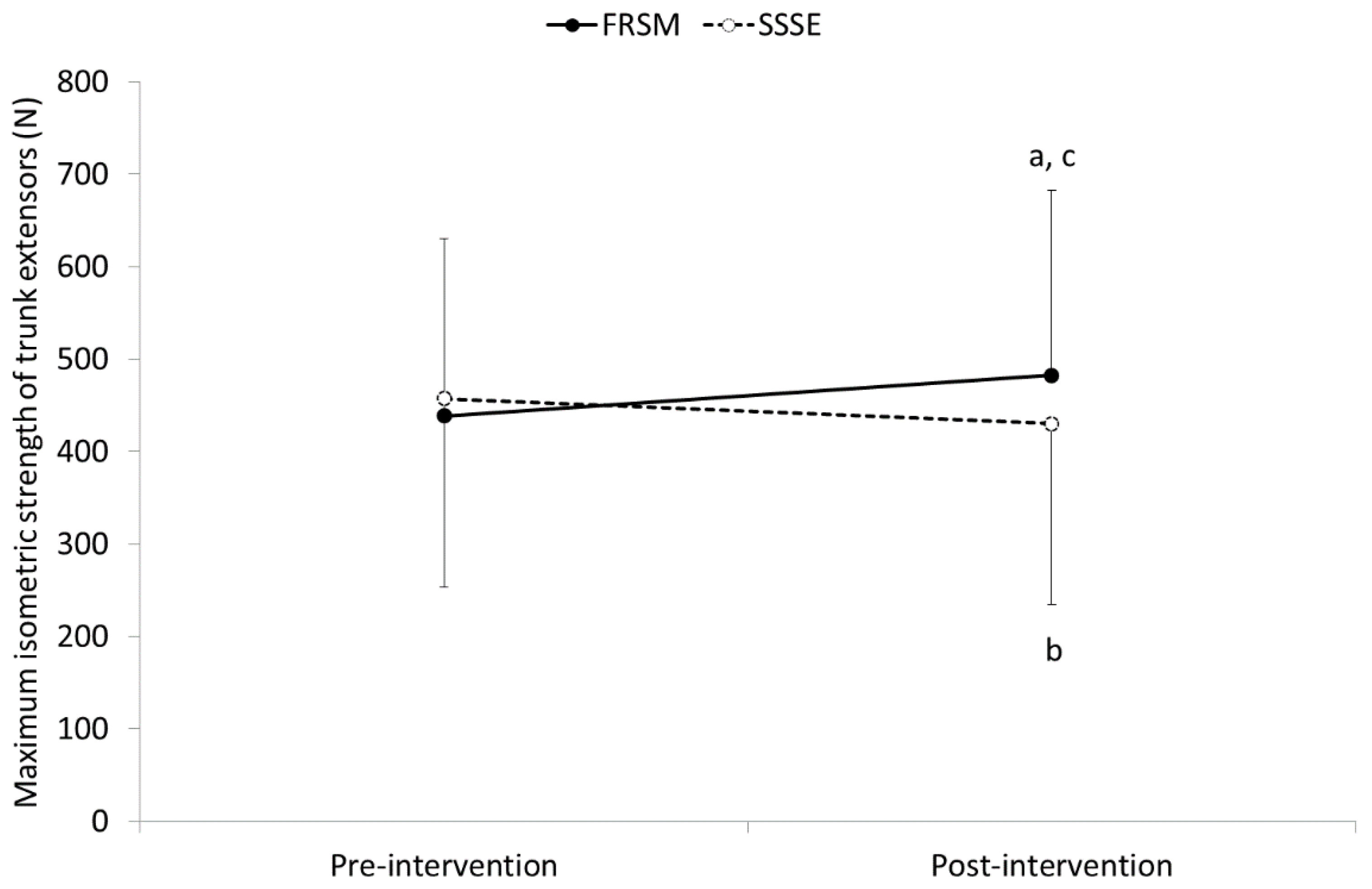
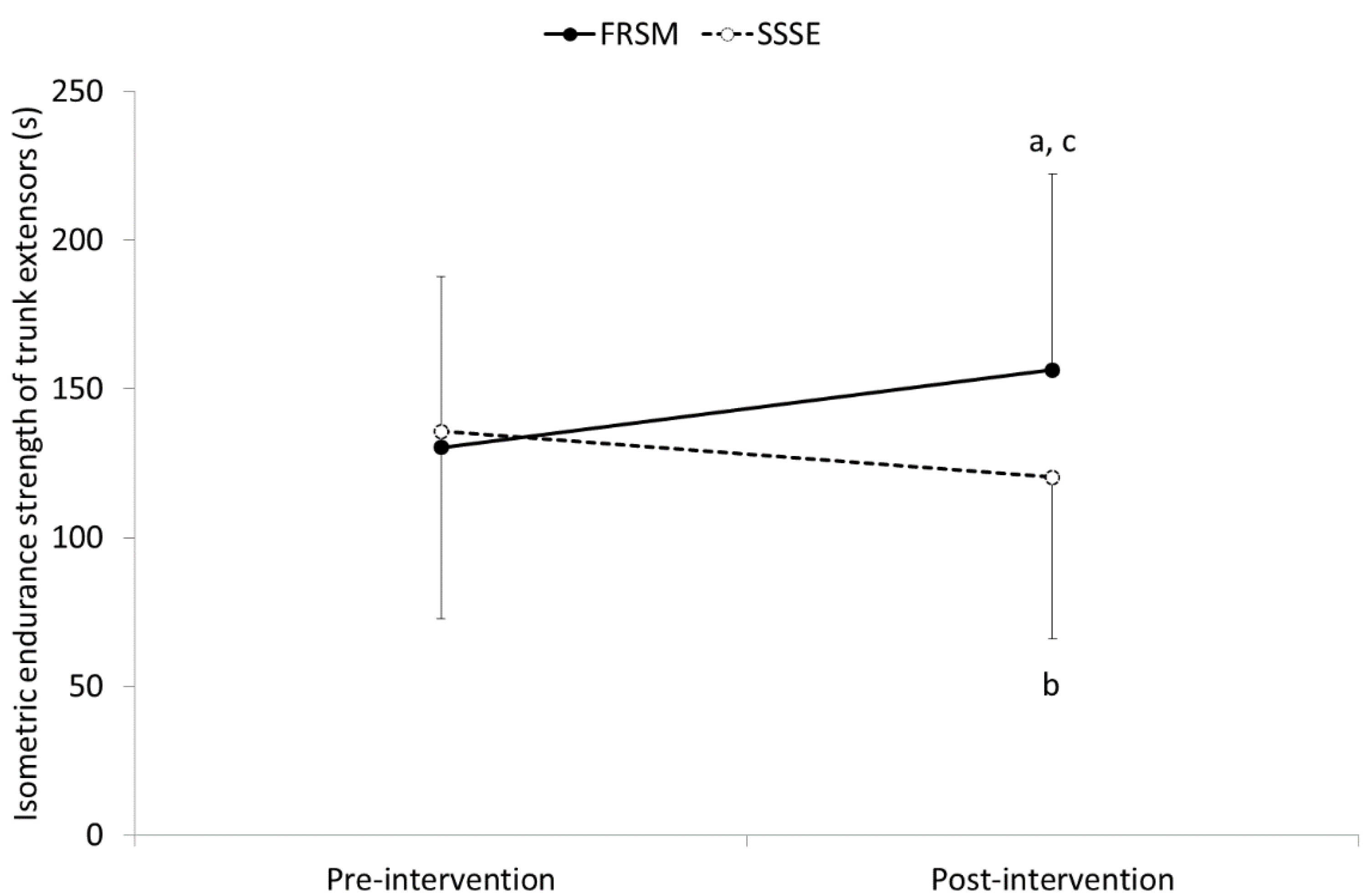
3.2. Isometric Maximum Strength and Endurance of Trunk Extensors
3.3. Trainees’ Satisfaction towards Intervention
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Behm, D.G.; Blazevich, A.J.; Kay, A.D.; McHugh, M. Acute Effects of Muscle Stretching on Physical Performance, Range of Motion, and Injury Incidence in Healthy Active Individuals: A Systematic Review. Appl. Physiol. Nutr. Metab. 2015, 41, 1–11. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Behm, D.G.; Chaouachi, A. A Review of the Acute Effects of Static and Dynamic Stretching on Performance. Eur. J. Appl. Physiol. 2011, 111, 2633–2651. [Google Scholar] [CrossRef]
- Witvrouw, E.; Mahieu, N.; Danneels, L.; McNair, P. Stretching and Injury Prevention: An Obscure Relationship. Sports Med. 2004, 34, 443–449. [Google Scholar] [CrossRef] [PubMed]
- Small, K.; Mc Naughton, L.; Matthews, M. A Systematic Review into the Efficacy of Static Stretching as Part of a Warm-up for the Prevention of Exercise-Related Injury. Res. Sports Med. 2008, 16, 213–231. [Google Scholar] [CrossRef] [PubMed]
- Sands, W.A.; McNeal, J.R.; Murray, S.R.; Ramsey, M.W.; Sato, K.; Mizuguchi, S.; Stone, M.H. Stretching and Its Effects on Recovery: A Review. Strength Cond. J. 2013, 35, 30–36. [Google Scholar] [CrossRef] [Green Version]
- McHugh, M.P.; Cosgrave, C.H. To Stretch or Not to Stretch: The Role of Stretching in Injury Prevention and Performance. Scand. J. Med. Sci. Sports 2010, 20, 169–181. [Google Scholar] [CrossRef]
- Beardsley, C.; Škarabot, J. Effects of Self-Myofascial Release: A Systematic Review. J. Bodyw. Mov. Ther. 2015, 19, 747–758. [Google Scholar] [CrossRef]
- Behm, D.G.; Wilke, J. Do Self-Myofascial Release Devices Release Myofascia? Rolling Mechanisms: A Narrative Review. Sports Med. 2019, 49, 1173–1181. [Google Scholar] [CrossRef]
- Zügel, M.; Maganaris, C.N.; Wilke, J.; Jurkat-Rott, K.; Klingler, W.; Wearing, S.C.; Findley, T.; Barbe, M.F.; Steinacker, J.M.; Vleeming, A.; et al. Fascial Tissue Research in Sports Medicine: From Molecules to Tissue Adaptation, Injury and Diagnostics: Consensus Statement. Br. J. Sports Med. 2018, 52, 1497. [Google Scholar] [CrossRef] [Green Version]
- Hedley, G. Notes on Visceral Adhesions as Fascial Pathology. J. Bodyw. Mov. Ther. 2010, 14, 255–261. [Google Scholar] [CrossRef]
- Sullivan, K.M.; Silvey, D.B.J.; Button, D.C.; Behm, D.G. Roller-Massager Application to the Hamstrings Increases Sit-and-Reach Range of Motion within Five to Ten Seconds without Performance Impairments. Int. J. Sports Phys. Ther. 2013, 8, 228–236. [Google Scholar]
- MacDonald, G.Z.; Penney, M.D.H.; Mullaley, M.E.; Cuconato, A.L.; Drake, C.D.J.; Behm, D.G.; Button, D.C. An Acute Bout of Self-Myofascial Release Increases Range of Motion without a Subsequent Decrease in Muscle Activation or Force. J. Strength Cond. Res. 2013, 27, 812–821. [Google Scholar] [CrossRef] [Green Version]
- Mikesky, A.E.; Bahamonde, R.E.; Stanton, K.; Alvey, T.; Fitton, T. Acute Effects of the Stick on Strength, Power, and Flexibility. J. Strength Cond. Res. 2002, 16, 446–450. [Google Scholar] [CrossRef] [PubMed]
- Halperin, I.; Aboodarda, S.J.; Button, D.C.; Andersen, L.L.; Behm, D.G. Roller Massager Improves Range of Motion of Plantar Flexor Muscles without Subsequent Decreases in Force Parameters. Int. J. Sports Phys. Ther. 2014, 9, 92–102. [Google Scholar]
- Macdonald, G.Z.; Button, D.C.; Drinkwater, E.J.; Behm, D.G. Foam Rolling as a Recovery Tool after an Intense Bout of Physical Activity. Med. Sci. Sports Exerc. 2014, 46, 131–142. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Peacock, C.A.; Krein, D.D.; Silver, T.A.; Sanders, G.J.; von Carlowitz, K.-P.A. An Acute Bout of Self-Myofascial Release in the Form of Foam Rolling Improves Performance Testing. Int. J. Exerc. Sci. 2014, 7, 202–211. [Google Scholar]
- Healey, K.C.; Hatfield, D.L.; Blanpied, P.; Dorfman, L.R.; Riebe, D. The Effects of Myofascial Release with Foam Rolling on Performance. J. Strength Cond. Res. 2014, 28, 61–68. [Google Scholar] [CrossRef] [Green Version]
- Su, H.; Chang, N.J.; Wu, W.L.; Guo, L.Y.; Chu, I.H. Acute Effects of Foam Rolling, Static Stretching, and Dynamic Stretching during Warm-Ups on Muscular Flexibility and Strength in Young Adults. J. Sport Rehabil. 2017, 26, 469–477. [Google Scholar] [CrossRef]
- Lee, C.L.; Chu, I.H.; Lyu, B.J.; Chang, W.D.; Chang, N.J. Comparison of Vibration Rolling, Nonvibration Rolling, and Static Stretching as a Warm-up Exercise on Flexibility, Joint Proprioception, Muscle Strength, and Balance in Young Adults. J. Sports Sci. 2018, 36, 2575–2582. [Google Scholar] [CrossRef]
- Zakas, A.; Balaska, P.; Grammatikopoulou, M.G.; Zakas, N.; Vergou, A. Acute Effects of Stretching Duration on the Range of Motion of Elderly Women. J. Bodyw. Mov. Ther. 2005, 9, 270–276. [Google Scholar] [CrossRef]
- Zakas, A.; Doganis, G.; Zakas, N.; Vergou, A. Acute Effects of Active Warm-up and Stretching on the Flexibility of Elderly Women. J. Sports Med. Phys. Fit. 2006, 46, 617–622. [Google Scholar]
- Zakas, A.; Vergou, A.; Grammatikopoulou, M.G.; Zakas, N.; Sentelidis, T.; Vamvakoudis, S. The Effect of Stretching during Warming-up on the Flexibility of Junior Handball Players. J. Sports Med. Phys. Fit. 2003, 43, 145–149. [Google Scholar]
- Griefahn, A.; Oehlmann, J.; Zalpour, C.; von Piekartz, H. Do Exercises with the Foam Roller Have a Short-Term Impact on the Thoracolumbar Fascia?—A Randomized Controlled Trial. J. Bodyw. Mov. Ther. 2017, 21, 186–193. [Google Scholar] [CrossRef] [PubMed]
- Doğan, M.; Koçak, M.; Onursal Kılınç, Ö.; Ayvat, F.; Sütçü, G.; Ayvat, E.; Kılınç, M.; Ünver, Ö.; Aksu Yıldırım, S. Functional Range of Motion in the Upper Extremity and Trunk Joints: Nine Functional Everyday Tasks with Inertial Sensors. Gait Posture 2019, 70, 141–147. [Google Scholar] [CrossRef]
- Gates, D.H.; Walters, L.S.; Cowley, J.; Wilken, J.M.; Resnik, L. Range of Motion Requirements for Upper-Limb Activities of Daily Living. Am. J. Occup. Ther. 2016, 70, 7001350010p1–7001350010p10. [Google Scholar] [CrossRef] [Green Version]
- Zazulak, B.T.; Ponce, P.L.; Straub, S.J.; Medvecky, M.J.; Avedisian, L.; Hewett, T.E. Gender Comparison of Hip Muscle Activity during Single-Leg Landing. J. Orthop. Sports Phys. Ther. 2005, 35, 292–299. [Google Scholar] [CrossRef] [Green Version]
- Janda, V. Muscle Function Testing; Elsevier: Amsteradm, The Netherlands, 1983; ISBN 9780407002012. [Google Scholar]
- Bunnell, W.P. An Objective Criterion for Scoliosis Screening. J. Bone Jt. Surg. Am. Vol. 1984, 66, 1381–1387. [Google Scholar] [CrossRef]
- Sabharwal, S.; Kumar, A. Methods for Assessing Leg Length Discrepancy. Clin. Orthop. Relat. Res. 2008, 466, 2910–2922. [Google Scholar] [CrossRef] [Green Version]
- Wilke, J.; Müller, A.-L.; Giesche, F.; Power, G.; Ahmedi, H.; Behm, D.G. Acute Effects of Foam Rolling on Range of Motion in Healthy Adults: A Systematic Review with Multilevel Meta-Analysis. Sports Med. 2020, 50, 387–402. [Google Scholar] [CrossRef]
- Hughes, G.A.; Ramer, L.M. Duration of Myofascial Rolling for Optimal Recovery, Range of Motion, and Performance: A Systematic Review of the Literature. Int. J. Sports Phys. Ther. 2019, 14, 845–859. [Google Scholar] [CrossRef]
- Behm, D.G.; Kibele, A. Effects of Differing Intensities of Static Stretching on Jump Performance. Eur. J. Appl. Physiol. 2007, 101, 587–594. [Google Scholar] [CrossRef] [PubMed]
- Hamersma, D.T.; Hofste, A.; Rijken, N.H.M.; Roe of Rohé, M.; Oosterveld, F.G.J.; Soer, R. Reliability and Validity of the Microgate Gyko for Measuring Range of Motion of the Low Back. Musculoskelet. Sci. Pract. 2020, 45, 102091. [Google Scholar] [CrossRef]
- Dvořák, J.; Vajda, E.G.; Grob, D.; Panjabi, M.M. Normal Motion of the Lumbar Spine as Related to Age and Gender. Eur. Spine J. 1995, 4, 18–23. [Google Scholar] [CrossRef]
- Johnson, K.D.; Grindstaff, T.L. Thoracic Rotation Measurement Techniques: Clinical Commentary. North Am. J. Sports Phys. Ther. NAJSPT 2010, 5, 252–256. [Google Scholar]
- da Silva, R.A.; Arsenault, A.B.; Gravel, D.; Larivière, C.; de Oliveira, E. Back Muscle Strength and Fatigue in Healthy and Chronic Low Back Pain Subjects: A Comparative Study of 3 Assessment Protocols. Arch. Phys. Med. Rehabil. 2005, 86, 722–729. [Google Scholar] [CrossRef]
- Biering-Sorensen, F. Physical Measurements as Risk Indicators for Low-Back Trouble over a One-Year Period. Spine 1984, 9, 106–119. [Google Scholar] [CrossRef] [PubMed]
- Haley, S.M.; Fragala-Pinkham, M.A. Interpreting Change Scores of Tests and Measures Used in Physical Therapy. Phys. Ther. 2006, 86, 735–743. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ayala, F.; Sainz de Baranda, P.; de Ste Croix, M.; Santonja, F. Reproducibility and Criterion-Related Validity of the Sit and Reach Test and Toe Touch Test for Estimating Hamstring Flexibility in Recreationally Active Young Adults. Phys. Ther. Sport 2012, 13, 219–226. [Google Scholar] [CrossRef]
- Alqhtani, R.S.; Jones, M.D.; Theobald, P.S.; Williams, J.M. Reliability of an Accelerometer-Based System for Quantifying Multiregional Spinal Range of Motion. J. Manip. Physiol. Ther. 2015, 38, 275–281. [Google Scholar] [CrossRef]
- Yang, S.; Wu, W.; Zhang, C.; Wang, D.; Chen, C.; Tang, Y.; Li, K.; Xu, J.; Luo, F. Reliability and Validity of Three Isometric Back Extensor Strength Assessments with Different Test Postures. J. Int. Med Res. 2020, 48, 030006051988526. [Google Scholar] [CrossRef] [Green Version]
- Latimer, J.; Maher, C.G.; Refshauge, K.; Colaco, I. The Reliability and Validity of the Biering–Sorensen Test in Asymptomatic Subjects and Subjects Reporting Current or Previous Nonspecific Low Back Pain. Spine 1999, 24, 2085. [Google Scholar] [CrossRef]
- Hardy, C.J.; Rejeski, W.J. Not What, but How One Feels: The Measurement of Affect during Exercise. J. Sport Exerc. Psychol. 2016, 11, 304–317. [Google Scholar] [CrossRef]
- Cohen, J. A Power Primer. Psychol. Bull. 1992, 112, 155–159. [Google Scholar] [CrossRef] [PubMed]
- Wiewelhove, T.; Döweling, A.; Schneider, C.; Hottenrott, L.; Meyer, T.; Kellmann, M.; Pfeiffer, M.; Ferrauti, A. A Meta-Analysis of the Effects of Foam Rolling on Performance and Recovery. Front. Physiol. 2019, 10. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wong, K.-K.; Chai, H.-M.; Chen, Y.-J.; Wang, C.-L.; Shau, Y.-W.; Wang, S.-F. Mechanical Deformation of Posterior Thoracolumbar Fascia after Myofascial Release in Healthy Men: A Study of Dynamic Ultrasound Imaging. Musculoskelet. Sci. Pract. 2017, 27, 124–130. [Google Scholar] [CrossRef] [PubMed]
- Schleip, R.; Müller, D.G. Training Principles for Fascial Connective Tissues: Scientific Foundation and Suggested Practical Applications. J. Bodyw. Mov. Ther. 2013, 17, 103–115. [Google Scholar] [CrossRef] [PubMed]
- Magnusson, S.P.; Simonsen, E.B.; Aagaard, P.; Soørensen, H.; Kjær, M. A Mechanism for Altered Flexibility in Human Skeletal Muscle. J. Physiol. 1996, 497, 291–298. [Google Scholar] [CrossRef]
- Morse, C.I.; Degens, H.; Seynnes, O.R.; Maganaris, C.N.; Jones, D.A. The Acute Effect of Stretching on the Passive Stiffness of the Human Gastrocnemius Muscle Tendon Unit. J. Physiol. 2008, 586, 97–106. [Google Scholar] [CrossRef]
- Schleip, R.; Duerselen, L.; Vleeming, A.; Naylor, I.L.; Lehmann-Horn, F.; Zorn, A.; Jaeger, H.; Klingler, W. Strain Hardening of Fascia: Static Stretching of Dense Fibrous Connective Tissues Can Induce a Temporary Stiffness Increase Accompanied by Enhanced Matrix Hydration. J. Bodyw. Mov. Ther. 2012, 16. [Google Scholar] [CrossRef]
- Nakamura, M.; Onuma, R.; Kiyono, R.; Yasaka, K.; Sato, S.; Yahata, K.; Fukaya, T.; Konrad, A. The Acute and Prolonged Effects of Different Durations of Foam Rolling on Range of Motion, Muscle Stiffness, and Muscle Strength. J. Sports Sci. Med. 2021, 62–68. [Google Scholar] [CrossRef]
- Lakie, M.; Robson, L.G. Thixotropic Changes in Human Muscle Stiffness and the Effects of Fatigue. Q. J. Exp. Physiol. 1988, 73, 487–500. [Google Scholar] [CrossRef]
- Ge, H.Y.; Arendt-Nielsen, L. Latent Myofascial Trigger Points. Curr. Pain Headache Rep. 2011, 15, 386–392. [Google Scholar] [CrossRef]
- Lucas, K.R.; Rich, P.A.; Polus, B.I. How Common Are Latent Myofascial Trigger Points in the Scapular Positioning Muscles? J. Musculoskelet. Pain 2008, 16, 279–286. [Google Scholar] [CrossRef]
- Powers, C.M.; Beneck, G.J.; Kulig, K.; Landel, R.F.; Fredericson, M. Effects of a Single Session of Posterior-to-Anterior Spinal Mobilization and Press-up Exercise on Pain Response and Lumbar Spine Extension in People with Nonspecific Low Back Pain. Phys. Ther. 2008, 88, 485–493. [Google Scholar] [CrossRef] [Green Version]
- Shum, G.L.; Tsung, B.Y.; Lee, R.Y. The Immediate Effect of Posteroanterior Mobilization on Reducing Back Pain and the Stiffness of the Lumbar Spine. Arch. Phys. Med. Rehabil. 2013, 94, 673–679. [Google Scholar] [CrossRef]
- Mawston, G.A.; Boocock, M.G. Lumbar Posture Biomechanics and Its Influence on the Functional Anatomy of the Erector Spinae and Multifidus. Phys. Ther. Rev. 2015, 20, 178–186. [Google Scholar] [CrossRef]
- Balle, S.S.; Magnusson, S.P.; McHugh, M.P. Effects of Contract-Relax vs Static Stretching on Stretch-Induced Strength Loss and Length-Tension Relationship. Scand. J. Med. Sci. Sports 2015, 25, 764–769. [Google Scholar] [CrossRef] [PubMed]
- Herda, T.J.; Cramer, J.T.; Ryan, E.D.; Mchugh, M.P.; Stout, J.R. Acute Effects of Static versus Dynamic Stretching on Isometric Peak Torque, Electromyography, and Mechanomyography of the Biceps Femoris Muscle. J. Strength Cond. Res. 2008, 22, 809–817. [Google Scholar] [CrossRef] [PubMed]
- Mannion, A.F.; Dumas, G.A.; Cooper, R.G.; Espinosa, F.J.; Faris, M.W.; Stevenson, J.M. Muscle Fibre Size and Type Distribution in Thoracic and Lumbar Regions of Erector Spinae in Healthy Subjects without Low Back Pain: Normal Values and Sex Differences. J. Anat. 1997, 190, 505–513. [Google Scholar] [CrossRef] [PubMed]
- Sirca, A.; Kostevc, V. The Fibre Type Composition of Thoracic and Lumbar Paravertebral Muscles in Man. J. Anat. 1985, 141, 131–137. [Google Scholar]
- Hotfiel, T.; Swoboda, B.; Krinner, S.; Grim, C.; Engelhardt, M.; Uder, M.; Heiss, R.U. Acute Effects of Lateral Thigh Foam Rolling on Arterial Tissue Perfusion Determined by Spectral Doppler and Power Doppler Ultrasound. J. Strength Cond. Res. 2017, 31, 893–900. [Google Scholar] [CrossRef]
- Okamoto, T.; Masuhara, M.; Ikuta, K. Acute Effects of Self-Myofascial Release Using a Foam Roller on Arterial Function. J. Strength Cond. Res. 2014, 28, 69–73. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jørgensen, K. Human Trunk Extensor Muscles Physiology and Ergonomics. Acta Physiol. Scandinavica. Suppl. 1997, 637, 1–58. [Google Scholar]
- Schleip, R.; Klingler, W. Active Contractile Properties of Fascia. Clin. Anat. 2019, 32, 891–895. [Google Scholar] [CrossRef]
- Cholewicki, J.; McGill, S. Mechanical Stability of the in Vivo Lumbar Spine: Implications for Injury and Chronic Low Back Pain. Clin. Biomech. 1996, 11, 1–15. [Google Scholar] [CrossRef]
- Krauspe, R.; Schmidt, M.; Schaible, H.G. Sensory Innervation of the Anterior Cruciate Ligament. An Electrophysiological Study of the Response Properties of Single Identified Mechanoreceptors in the Cat. J. Bone Jt. Surg. Am. Vol. 1992, 74, 390–397. [Google Scholar] [CrossRef]
- Sjölander, P.; Johansson, H.; Djupsjöbacka, M. Spinal and Supraspinal Effects of Activity in Ligament Afferents. J. Electromyogr. Kinesiol. 2002, 12, 167–176. [Google Scholar] [CrossRef]
- Cipriani, D.J.; Terry, M.E.; Haines, M.A.; Tabibnia, A.P.; Lyssanova, O. Effect of Stretch Frequency and Sex on the Rate of Gain and Rate of Loss in Muscle Flexibility During a Hamstring-Stretching Program. J. Strength Cond. Res. 2012, 26, 2119–2129. [Google Scholar] [CrossRef] [Green Version]
- Cheatham, S.; Stull, K. Comparison of Three Different Density Type Foam Rollers on Knee Range of Motion and Pressure Pain Threshold: A Randomized Controlled Trial. Int. J. Sports Phys. Ther. 2018, 13, 474–482. [Google Scholar] [CrossRef]
- Cheatham, S.W.; Stull, K.R. Roller Massage: Comparison of Three Different Surface Type Pattern Foam Rollers on Passive Knee Range of Motion and Pain Perception. J. Bodyw. Mov. Ther. 2019, 23, 555–560. [Google Scholar] [CrossRef] [PubMed]

| Outcome Measure | ICC | SEM | MDC |
|---|---|---|---|
| T-HF (cm) [39] | 0.92 | 0.3 | 1.4 |
| TSFR (°) [40] | 0.92 | 0.8 | 2.2 |
| TSFL (°) [40] | 0.98 | 0.6 | 1.7 |
| TRR (°) [40] | 0.96 | 3.2 | 8.9 |
| TRL (°) [40] | 0.99 | 2.1 | 5.8 |
| TESmax (N) [41] | 0.93 | 13.0 | 36.0 |
| TESend (s) [42] | 0.86 | 15.2 | 42.1 |
| Foam Roller Self-Massaging | Static Self-Stretching Exercises | |||||||
|---|---|---|---|---|---|---|---|---|
| Pre-FRSM | Post-FRSM | Diff | Cohen’s d | Pre-SSSEs | Post-SSSEs | Diff | Cohen’s d | |
| T-HF (cm) | 36.9 ± 8.2 | 40.6 ± 8.3 b | 3.7 ± 3.3 | 0.45 | 35.8 ± 9.0 | 39.6 ± 8.1 b | 3.8 ± 3.6 | 0.44 |
| TSFR (°) | 50.2 ± 9.9 | 54.1 ± 10.4 b | 3.9 ± 4.4 | 0.39 | 50.9 ± 9.8 | 53.0 ± 8.8 a | 2.1 ± 4.3 c | 0.22 |
| TSFL (°) | 51.6 ± 9.7 | 55.5 ± 10.7 b | 3.9 ± 4.5 | 0.38 | 51.5 ± 8.4 | 55.6 ± 10.7 b | 4.0 ± 4.1 | 0.42 |
| TRR (°) | 55.9 ± 8.6 | 60.6 ± 9.3 b | 4.8 ± 5.0 | 0.53 | 57.2 ± 7.5 | 60.8 ± 8.3 b | 3.6 ± 4.5 | 0.46 |
| TRL (°) | 56.3 ± 9.1 | 63.0 ± 8.2 b | 6.4 ± 4.1 | 0.74 | 58.5 ± 8.1 | 61.3 ± 8.4 a | 2.8 ± 5.1 d | 0.34 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fonta, M.; Tsepis, E.; Fousekis, K.; Mandalidis, D. Acute Effects of Static Self-Stretching Exercises and Foam Roller Self-Massaging on the Trunk Range of Motions and Strength of the Trunk Extensors. Sports 2021, 9, 159. https://doi.org/10.3390/sports9120159
Fonta M, Tsepis E, Fousekis K, Mandalidis D. Acute Effects of Static Self-Stretching Exercises and Foam Roller Self-Massaging on the Trunk Range of Motions and Strength of the Trunk Extensors. Sports. 2021; 9(12):159. https://doi.org/10.3390/sports9120159
Chicago/Turabian StyleFonta, Maria, Elias Tsepis, Konstantinos Fousekis, and Dimitris Mandalidis. 2021. "Acute Effects of Static Self-Stretching Exercises and Foam Roller Self-Massaging on the Trunk Range of Motions and Strength of the Trunk Extensors" Sports 9, no. 12: 159. https://doi.org/10.3390/sports9120159
APA StyleFonta, M., Tsepis, E., Fousekis, K., & Mandalidis, D. (2021). Acute Effects of Static Self-Stretching Exercises and Foam Roller Self-Massaging on the Trunk Range of Motions and Strength of the Trunk Extensors. Sports, 9(12), 159. https://doi.org/10.3390/sports9120159







